Drug Detail:Rituxan (Rituximab [ ri-tux-i-mab ])
Drug Class: Antirheumatics CD20 monoclonal antibodies
Highlights of Prescribing Information
RITUXAN® (rituximab) injection, for intravenous use
Initial U.S. Approval: 1997
WARNING: FATAL INFUSION-RELATED REACTIONS, SEVERE MUCOCUTANEOUS REACTIONS, HEPATITIS B VIRUS REACTIVATION and PROGRESSIVE MULTIFOCAL LEUKOENCEPHALOPATHY
See full prescribing information for complete boxed warning.
- Fatal infusion-related reactions within 24 hours of RITUXAN infusion; approximately 80% of fatal reactions occurred with first infusion. Monitor patients and discontinue RITUXAN infusion for severe reactions (5.1).
- Severe mucocutaneous reactions, some with fatal outcomes (5.2).
- Hepatitis B virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure, and death (5.3).
- Progressive multifocal leukoencephalopathy (PML) resulting in death (5.4).
Recent Major Changes
| Indications and Usage (1.1) | 12/2021 |
| Dosage and Administration, Important Dosing Information (2.1) | 12/2021 |
| Dosage and Administration, NHL (2.2.) | 12/2021 |
| Dosage and Administration, Premedication and Prophylactic Medication (2.8) | 12/2021 |
| Dosage and Administration, Administration and Storage (2.9) | 6/2021 |
| Warnings and Precautions, Infusion-Related Reactions (5.1) | 12/2021 |
Indications and Usage for Rituxan
RITUXAN is a CD20-directed cytolytic antibody indicated for the treatment of:
- Adult patients with Non-Hodgkin's Lymphoma (NHL) (1.1).
- Relapsed or refractory, low grade or follicular, CD20-positive B-cell NHL as a single agent.
- Previously untreated follicular, CD20-positive, B-cell NHL in combination with first line chemotherapy and, in patients achieving a complete or partial response to a rituximab product in combination with chemotherapy, as single-agent maintenance therapy.
- Non-progressing (including stable disease), low-grade, CD20-positive, B-cell NHL as a single agent after first-line cyclophosphamide, vincristine, and prednisone (CVP) chemotherapy.
- Previously untreated diffuse large B-cell, CD20-positive NHL in combination with (cyclophosphamide, doxorubicin, vincristine, and prednisone) (CHOP) or other anthracycline-based chemotherapy regimens.
- Pediatric patients aged 6 months and older with mature B-cell NHL and mature B-cell acute leukemia (B-AL) (1.1)
- Previously untreated, advanced stage, CD20-positive, diffuse large B-cell lymphoma (DLBCL), Burkitt lymphoma (BL), Burkitt-like lymphoma (BLL) or mature B-cell acute leukemia (B-AL) in combination with chemotherapy.
- Adult patients with Chronic Lymphocytic Leukemia (CLL) (1.2).
- Previously untreated and previously treated CD20-positive CLL in combination with fludarabine and cyclophosphamide (FC).
- Rheumatoid Arthritis (RA) in combination with methotrexate in adult patients with moderately-to severely-active RA who have inadequate response to one or more TNF antagonist therapies (1.3).
- Granulomatosis with Polyangiitis (GPA) (Wegener's Granulomatosis) and Microscopic Polyangiitis (MPA) in adult and pediatric patients 2 years of age and older in combination with glucocorticoids (1.4).
- Moderate to severe Pemphigus Vulgaris (PV) in adult patients (1.5).
Rituxan Dosage and Administration
- Administer only as an intravenous infusion (2.1).
- Do not administer as an intravenous push or bolus (2.1).
- RITUXAN should only be administered by a healthcare professional with appropriate medical support to manage severe infusion-related reactions that can be fatal if they occur. (2.1).
- The dose for adult and pediatric B-cell NHL is 375 mg/m2 (2.2).
- The dose for CLL is 375 mg/m2 in the first cycle and 500 mg/m2 in cycles 2–6, in combination with FC, administered every 28 days (2.3).
- The dose as a component of Zevalin® (ibritumomab tiuxetan) Therapeutic Regimen is 250 mg/m2 (2.4).
- The dose for RA in combination with methotrexate is two-1,000 mg intravenous infusions separated by 2 weeks (one course) every 24 weeks or based on clinical evaluation, but not sooner than every 16 weeks. Methylprednisolone 100 mg intravenous or equivalent glucocorticoid is recommended 30 minutes prior to each infusion (2.5).
- The induction dose for adult patients with active GPA and MPA in combination with glucocorticoids is 375 mg/m2 once weekly for 4 weeks. The follow up dose for adult patients with GPA and MPA who have achieved disease control with induction treatment, in combination with glucocorticoids is two 500 mg intravenous infusions separated by two weeks, followed by a 500 mg intravenous infusion every 6 months thereafter based on clinical evaluation (2.6).
- The induction dose for pediatric patients with GPA and MPA in combination with glucocorticoids is 375 mg/m2 once weekly for 4 weeks. The follow up dose for pediatric patients with GPA and MPA who have achieved disease control with induction treatment, in combination with glucocorticoids is two 250 mg/m2 intravenous infusions separated by two weeks, followed by a 250 mg/m2 intravenous infusion every 6 months thereafter based on clinical evaluation (2.6).
- The dose for PV is two-1,000 mg intravenous infusions separated by 2 weeks in combination with a tapering course of glucocorticoids, then a 500 mg intravenous infusion at Month 12 and every 6 months thereafter or based on clinical evaluation. Dose upon relapse is a 1,000 mg intravenous infusion with considerations to resume or increase the glucocorticoid dose based on clinical evaluation. Subsequent infusions may be no sooner than 16 weeks after the previous infusion (2.7). Methylprednisolone 100 mg intravenous or equivalent glucocorticoid is recommended 30 minutes prior to each infusion (2.8).
Dosage Forms and Strengths
- Injection: 100 mg/10 mL (10 mg/mL) and 500 mg/50 mL (10 mg/mL) solution in single-dose vials (3)
Contraindications
None (4)
Warnings and Precautions
- Tumor lysis syndrome: Administer aggressive intravenous hydration, anti-hyperuricemic agents, monitor renal function (5.5).
- Infections: Withhold RITUXAN and institute appropriate anti-infective therapy (5.6).
- Cardiac adverse reactions: Discontinue infusions in case of serious or life-threatening events (5.7).
- Renal toxicity: Discontinue in patients with rising serum creatinine or oliguria (5.8).
- Bowel obstruction and perforation: Consider and evaluate for abdominal pain, vomiting, or related symptoms (5.9).
- Immunizations: Live virus vaccinations prior to or during RITUXAN treatment not recommended (5.10).
- Embryo-Fetal toxicity: Can cause fetal harm. Advise females of reproductive potential of the potential risk to a fetus and use of effective contraception (5.11).
Adverse Reactions/Side Effects
Most common adverse reactions in clinical trials were:
- NHL (greater than or equal to 25%): infusion-related reactions, fever, lymphopenia, chills, infection, and asthenia (6.1).
- Pediatric B-NHL/B-AL with chemotherapy (Grade 3 or higher greater than 15%): febrile neutropenia, stomatitis, enteritis, sepsis, alanine aminotransferase increased and hypokalemia (6.1).
- CLL (greater than or equal to 25%): infusion-related reactions and neutropenia (6.1).
- RA (greater than or equal to 10%): upper respiratory tract infection, nasopharyngitis, urinary tract infection, and bronchitis (other important adverse reactions include infusion-related reactions, serious infections, and cardiovascular events) (6.1).
- GPA and MPA (greater than or equal to 15 %): infections, nausea, diarrhea, headache, muscle spasms, anemia, peripheral edema, infusion-related reactions (6.1).
- PV (greater than or equal to 15%): infusion-related reactions, depression, upper respiratory tract infection/ nasopharyngitis, headache (other important adverse reactions include infections) (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Genentech at 1-888-835-2555 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
Renal toxicity when used in combination with cisplatin (5.8).
Use In Specific Populations
- Lactation: Advise not to breastfeed (8.2).
- Geriatric Use: In CLL patients older than 70 years of age, exploratory analyses suggest no benefit with the addition of RITUXAN to FC (8.5).
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 12/2021
Full Prescribing Information
WARNING: FATAL INFUSION-RELATED REACTIONS, SEVERE MUCOCUTANEOUS REACTIONS, HEPATITIS B VIRUS REACTIVATION and PROGRESSIVE MULTIFOCAL LEUKOENCEPHALOPATHY
1. Indications and Usage for Rituxan
1.1 Non–Hodgkin's Lymphoma (NHL)
RITUXAN is indicated for the treatment of adult patients with:
- Relapsed or refractory, low-grade or follicular, CD20-positive, B-cell NHL as a single agent.
- Previously untreated follicular, CD20-positive, B-cell NHL in combination with first line chemotherapy and, in patients achieving a complete or partial response to a rituximab product in combination with chemotherapy, as single-agent maintenance therapy.
- Non-progressing (including stable disease), low-grade, CD20-positive, B-cell NHL as a single agent after first-line cyclophosphamide, vincristine, and prednisone (CVP) chemotherapy.
- Previously untreated diffuse large B-cell, CD20-positive NHL in combination with cyclophosphamide, doxorubicin, vincristine, prednisone (CHOP) or other anthracycline-based chemotherapy regimens.
RITUXAN is indicated for the treatment of pediatric patients aged 6 months and older with:
- Previously untreated, advanced stage, CD20-positive diffuse large B-cell lymphoma (DLBCL), Burkitt lymphoma (BL), Burkitt-like lymphoma (BLL) or mature B-cell acute leukemia (B-AL) in combination with chemotherapy.
1.2 Chronic Lymphocytic Leukemia (CLL)
RITUXAN, in combination with fludarabine and cyclophosphamide (FC), is indicated for the treatment of adult patients with previously untreated and previously treated CD20-positive CLL.
1.3 Rheumatoid Arthritis (RA)
RITUXAN, in combination with methotrexate, is indicated for the treatment of adult patients with moderately- to severely-active rheumatoid arthritis who have had an inadequate response to one or more TNF antagonist therapies.
1.4 Granulomatosis with Polyangiitis (GPA) (Wegener's Granulomatosis) and Microscopic Polyangiitis (MPA)
RITUXAN, in combination with glucocorticoids, is indicated for the treatment of adult and pediatric patients 2 years of age and older with Granulomatosis with Polyangiitis (GPA) (Wegener's Granulomatosis) and Microscopic Polyangiitis (MPA).
2. Rituxan Dosage and Administration
2.1 Important Dosing Information
Administer only as an Intravenous Infusion [see Dosage and Administration (2.8)]. Do not administer as an intravenous push or bolus.
RITUXAN should only be administered by a healthcare professional with appropriate medical support to manage severe infusion-related reactions that can be fatal if they occur [see Warnings and Precautions (5.1)].
Premedicate before each infusion [see Dosage and Administration (2.8)].
2.2 Recommended Dose for Non-Hodgkin's Lymphoma (NHL)
The recommended dose is 375 mg/m2 as an intravenous infusion according to the following schedules:
-
Relapsed or Refractory, Low-Grade or Follicular, CD20-Positive, B-Cell NHL
Administer once weekly for 4 or 8 doses. -
Retreatment for Relapsed or Refractory, Low-Grade or Follicular, CD20-Positive, B-Cell NHL
Administer once weekly for 4 doses. -
Previously Untreated, Follicular, CD20-Positive, B-Cell NHL
Administer on Day 1 of each cycle of chemotherapy for up to 8 doses. In patients with complete or partial response, initiate RITUXAN maintenance eight weeks following completion of a rituximab product in combination with chemotherapy. Administer RITUXAN as a single-agent every 8 weeks for 12 doses. -
Non-progressing, Low-Grade, CD20-Positive, B-Cell NHL, after first-line CVP chemotherapy
Following completion of 6–8 cycles of CVP chemotherapy, administer once weekly for 4 doses at 6-month intervals to a maximum of 16 doses. -
Diffuse Large B-Cell NHL
Administer on Day 1 of each cycle of chemotherapy for up to 8 infusions. -
Pediatric patients aged 6 months and older with previously untreated mature B-cell NHL/B-AL
RITUXAN is given in combination with systemic Lymphome Malin B (LMB) chemotherapy. In total, six infusions of RITUXAN are given, two doses during each of the induction courses, COPDAM1 and COPDAM2, and one dose during each of the two consolidation courses of CYM/CYVE (for details see Table 1).
| Cycle | Day of treatment | Administration details |
|---|---|---|
| COP = Cyclophosphamide, Oncovin (vincristine), Prednisone; COPDAM = Cyclophosphamide, Oncovin (vincristine), Prednisolone, Adriamycin (doxorubicin), Methotrexate; CYM = CYtarabine (Aracytine, Ara-C), Methotrexate; CYVE = CYtarabine (Aracytine, Ara-C), VEposide (VP16) | ||
| Prephase (COP) | No RITUXAN given | - |
| Induction courses 1 and 2 (COPDAM1 and COPDAM2) | Day -2 1st and 3rd RITUXAN infusions | During the 1st induction course, prednisone is given as part of the chemotherapy course, and should be administered prior to RITUXAN. |
| Day 1 2nd and 4th RITUXAN infusions | RITUXAN will be given 48 hours after the first infusion of RITUXAN. | |
| Consolidation courses 1 and 2 (CYM/CYVE) | Day 1 5th and 6th RITUXAN infusions | - |
2.3 Recommended Dose for Chronic Lymphocytic Leukemia (CLL)
The recommended dose is 375 mg/m2 the day prior to the initiation of FC chemotherapy, then 500 mg/m2 on Day 1 of cycles 2–6 (every 28 days).
2.4 Recommended Dose as a Component of Zevalin® for treatment of NHL
- When used as part of the Zevalin therapeutic regimen, infuse 250 mg/m2 in accordance with the Zevalin package insert. Refer to the Zevalin package insert for full prescribing information regarding the Zevalin therapeutic regimen.
2.5 Recommended Dose for Rheumatoid Arthritis (RA)
- Administer RITUXAN as two-1,000 mg intravenous infusions separated by 2 weeks.
- Glucocorticoids administered as methylprednisolone 100 mg intravenous or its equivalent 30 minutes prior to each infusion are recommended to reduce the incidence and severity of infusion-related reactions.
- Subsequent courses should be administered every 24 weeks or based on clinical evaluation, but not sooner than every 16 weeks.
- RITUXAN is given in combination with methotrexate.
2.6 Recommended Dose for Granulomatosis with Polyangiitis (GPA) (Wegener's Granulomatosis) and Microscopic Polyangiitis (MPA)
2.7 Recommended Dose for Pemphigus Vulgaris (PV)
- Administer RITUXAN as two-1,000 mg intravenous infusions separated by 2 weeks in combination with a tapering course of glucocorticoids.
-
Maintenance treatment
Administer RITUXAN as a 500 mg intravenous infusion at Month 12 and every 6 months thereafter or based on clinical evaluation. -
Treatment of relapse
Administer RITUXAN as a 1,000 mg intravenous infusion on relapse, and consider resuming or increasing the glucocorticoid dose based on clinical evaluation.
Subsequent infusions of RITUXAN may be administered no sooner than 16 weeks following the previous infusion.
2.8 Recommended Dose for Premedication and Prophylactic Medications
Premedicate with acetaminophen and an antihistamine before each infusion of RITUXAN. For adult patients administered RITUXAN according to the 90-minute infusion rate, the glucocorticoid component of their chemotherapy regimen should be administered prior to infusion [see Clinical Studies (14.4)].
For pediatric patients with mature B-cell NHL/B-AL, premedication with acetaminophen and H1 antihistamine (diphenhydramine or equivalent) should be administered 30 to 60 minutes before the start of each RITUXAN intravenous infusion.
For RA, GPA and MPA, and PV patients, methylprednisolone 100 mg intravenously or its equivalent is recommended 30 minutes prior to each infusion.
Provide prophylaxis treatment for Pneumocystis jirovecii pneumonia (PCP) and herpes virus infections for patients with CLL during treatment and for up to 12 months following treatment as appropriate [see Warnings and Precautions (5.6)].
PCP prophylaxis is also recommended for patients with GPA and MPA during treatment and for at least 6 months following the last RITUXAN infusion.
PCP prophylaxis should be considered for patients with PV during and following RITUXAN treatment.
3. Dosage Forms and Strengths
Injection: RITUXAN is a colorless, clear solution for intravenous infusion:
- 100 mg/10 mL (10 mg/mL) in a single-dose vial
- 500 mg/50 mL (10 mg/mL) in a single-dose vial
5. Warnings and Precautions
5.1 Infusion-Related Reactions
RITUXAN can cause severe, including fatal, infusion-related reactions. Severe reactions typically occurred during the first infusion with time to onset of 30–120 minutes. RITUXAN-induced infusion-related reactions and sequelae include urticaria, hypotension, angioedema, hypoxia, bronchospasm, pulmonary infiltrates, acute respiratory distress syndrome, myocardial infarction, ventricular fibrillation, cardiogenic shock, anaphylactoid events, or death.
Premedicate patients with an antihistamine and acetaminophen prior to dosing. For RA, GPA and MPA, and PV patients, methylprednisolone 100 mg intravenously or its equivalent is recommended 30 minutes prior to each infusion. For pediatric patients with mature B-cell NHL/B-AL, administer prednisone as part of chemotherapy regimen prior to RITUXAN during induction and as needed for subsequent cycles [see Dosage and Administration (2.2 and 2.8)]. Institute medical management (e.g., glucocorticoids, epinephrine, bronchodilators, or oxygen) for infusion-related reactions as needed. Depending on the severity of the infusion-related reaction and the required interventions, temporarily or permanently discontinue RITUXAN. Resume infusion at a minimum 50% reduction in rate after symptoms have resolved. Closely monitor the following patients: those with pre-existing cardiac or pulmonary conditions, those who experienced prior cardiopulmonary adverse reactions, and those with high numbers of circulating malignant cells (greater than or equal to 25,000/mm3) [see Warnings and Precautions (5.7), Adverse Reactions (6.1)].
5.2 Severe Mucocutaneous Reactions
Mucocutaneous reactions, some with fatal outcome, can occur in patients treated with RITUXAN. These reactions include paraneoplastic pemphigus, Stevens-Johnson syndrome, lichenoid dermatitis, vesiculobullous dermatitis, and toxic epidermal necrolysis. The onset of these reactions has been variable and includes reports with onset on the first day of RITUXAN exposure. Discontinue RITUXAN in patients who experience a severe mucocutaneous reaction. The safety of re-administration of RITUXAN to patients with severe mucocutaneous reactions has not been determined.
5.3 Hepatitis B Virus (HBV) Reactivation
Hepatitis B virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure and death, can occur in patients treated with drugs classified as CD20-directed cytolytic antibodies, including RITUXAN. Cases have been reported in patients who are hepatitis B surface antigen (HBsAg) positive and also in patients who are HBsAg negative but are hepatitis B core antibody (anti-HBc) positive. Reactivation also has occurred in patients who appear to have resolved hepatitis B infection (i.e., HBsAg negative, anti-HBc positive and hepatitis B surface antibody [anti-HBs] positive).
HBV reactivation is defined as an abrupt increase in HBV replication manifesting as a rapid increase in serum HBV DNA levels or detection of HBsAg in a person who was previously HBsAg negative and anti-HBc positive. Reactivation of HBV replication is often followed by hepatitis, i.e., increase in transaminase levels. In severe cases increase in bilirubin levels, liver failure, and death can occur.
Screen all patients for HBV infection by measuring HBsAg and anti-HBc before initiating treatment with RITUXAN. For patients who show evidence of prior hepatitis B infection (HBsAg positive [regardless of antibody status] or HBsAg negative but anti-HBc positive), consult with physicians with expertise in managing hepatitis B regarding monitoring and consideration for HBV antiviral therapy before and/or during RITUXAN treatment.
Monitor patients with evidence of current or prior HBV infection for clinical and laboratory signs of hepatitis or HBV reactivation during and for several months following RITUXAN therapy. HBV reactivation has been reported up to 24 months following completion of RITUXAN therapy.
In patients who develop reactivation of HBV while on RITUXAN, immediately discontinue RITUXAN and any concomitant chemotherapy, and institute appropriate treatment. Insufficient data exist regarding the safety of resuming RITUXAN treatment in patients who develop HBV reactivation. Resumption of RITUXAN treatment in patients whose HBV reactivation resolves should be discussed with physicians with expertise in managing HBV.
5.4 Progressive Multifocal Leukoencephalopathy (PML)
JC virus infection resulting in PML and death can occur in RITUXAN-treated patients with hematologic malignancies or with autoimmune diseases. The majority of patients with hematologic malignancies diagnosed with PML received RITUXAN in combination with chemotherapy or as part of a hematopoietic stem cell transplant. The patients with autoimmune diseases had prior or concurrent immunosuppressive therapy. Most cases of PML were diagnosed within 12 months of their last infusion of RITUXAN.
Consider the diagnosis of PML in any patient presenting with new-onset neurologic manifestations. Evaluation of PML includes, but is not limited to, consultation with a neurologist, brain MRI, and lumbar puncture.
Discontinue RITUXAN and consider discontinuation or reduction of any concomitant chemotherapy or immunosuppressive therapy in patients who develop PML.
5.5 Tumor Lysis Syndrome (TLS)
Acute renal failure, hyperkalemia, hypocalcemia, hyperuricemia, or hyperphosphatemia from tumor lysis, sometimes fatal, can occur within 12–24 hours after the first infusion of RITUXAN in patients with NHL. A high number of circulating malignant cells ( greater than or equal to 25,000/mm3) or high tumor burden, confers a greater risk of TLS.
Administer aggressive intravenous hydration and anti-hyperuricemic therapy in patients at high risk for TLS. Correct electrolyte abnormalities, monitor renal function and fluid balance, and administer supportive care, including dialysis as indicated. [see Warnings and Precautions (5.8)].
5.6 Infections
Serious, including fatal, bacterial, fungal, and new or reactivated viral infections can occur during and following the completion of RITUXAN-based therapy. Infections have been reported in some patients with prolonged hypogammaglobulinemia (defined as hypogammaglobulinemia greater than 11 months after rituximab exposure). New or reactivated viral infections included cytomegalovirus, herpes simplex virus, parvovirus B19, varicella zoster virus, West Nile virus, and hepatitis B and C. Discontinue RITUXAN for serious infections and institute appropriate anti-infective therapy [see Adverse Reactions (6.1, 6.3)]. RITUXAN is not recommended for use in patients with severe, active infections.
5.7 Cardiovascular Adverse Reactions
Cardiac adverse reactions, including ventricular fibrillation, myocardial infarction, and cardiogenic shock may occur in patients receiving RITUXAN. Discontinue infusions for serious or life-threatening cardiac arrhythmias. Perform cardiac monitoring during and after all infusions of RITUXAN for patients who develop clinically significant arrhythmias, or who have a history of arrhythmia or angina [see Adverse Reactions (6.1)].
5.8 Renal Toxicity
Severe, including fatal, renal toxicity can occur after RITUXAN administration in patients with NHL. Renal toxicity has occurred in patients who experience tumor lysis syndrome and in patients with NHL administered concomitant cisplatin therapy during clinical trials. The combination of cisplatin and RITUXAN is not an approved treatment regimen. Monitor closely for signs of renal failure and discontinue RITUXAN in patients with a rising serum creatinine or oliguria [see Warnings and Precautions (5.5)].
5.9 Bowel Obstruction and Perforation
Abdominal pain, bowel obstruction and perforation, in some cases leading to death, can occur in patients receiving RITUXAN in combination with chemotherapy. In postmarketing reports, the mean time to documented gastrointestinal perforation was 6 (range 1–77) days in patients with NHL. Evaluate if symptoms of obstruction such as abdominal pain or repeated vomiting occur.
5.10 Immunization
The safety of immunization with live viral vaccines following RITUXAN therapy has not been studied and vaccination with live virus vaccines is not recommended before or during treatment.
For patients treated with RITUXAN, physicians should review the patient's vaccination status and patients should, if possible, be brought up-to-date with all immunizations in agreement with current immunization guidelines prior to initiating RITUXAN and administer non live vaccines at least 4 weeks prior to a course of RITUXAN.
The effect of RITUXAN on immune responses was assessed in a randomized, controlled study in patients with RA treated with RITUXAN and methotrexate (MTX) compared to patients treated with MTX alone.
A response to pneumococcal vaccination (a T-cell independent antigen) as measured by an increase in antibody titers to at least 6 of 12 serotypes was lower in patients treated with RITUXAN plus MTX as compared to patients treated with MTX alone (19% vs. 61%). A lower proportion of patients in the RITUXAN plus MTX group developed detectable levels of anti-keyhole limpet hemocyanin antibodies (a novel protein antigen) after vaccination compared to patients on MTX alone (47% vs. 93%).
A positive response to tetanus toxoid vaccine (a T-cell dependent antigen with existing immunity) was similar in patients treated with RITUXAN plus MTX compared to patients on MTX alone (39% vs. 42%). The proportion of patients maintaining a positive Candida skin test (to evaluate delayed type hypersensitivity) was also similar (77% of patients on RITUXAN plus MTX vs. 70% of patients on MTX alone).
Most patients in the RITUXAN-treated group had B-cell counts below the lower limit of normal at the time of immunization. The clinical implications of these findings are not known.
5.11 Embryo-Fetal Toxicity
Based on human data, RITUXAN can cause fetal harm due to B-cell lymphocytopenia in infants exposed to rituximab in-utero. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception while receiving RITUXAN and for 12 months after the last dose [see Use in Specific Populations (8.1, 8.3)].
5.12 Concomitant Use with Other Biologic Agents and DMARDS other than Methotrexate in RA, GPA and MPA, PV
Limited data are available on the safety of the use of biologic agents or disease modifying antirheumatic drugs (DMARDs) other than methotrexate in RA patients exhibiting peripheral B-cell depletion following treatment with rituximab. Observe patients closely for signs of infection if biologic agents and/or DMARDs are used concomitantly. Use of concomitant immunosuppressants other than corticosteroids has not been studied in GPA or MPA or PV patients exhibiting peripheral B-cell depletion following treatment with RITUXAN.
5.13 Use in RA Patients Who Have Not Had Prior Inadequate Response to Tumor Necrosis Factor (TNF) Antagonists
While the efficacy of RITUXAN was supported in four controlled trials in patients with RA with prior inadequate responses to non-biologic DMARDs, and in a controlled trial in MTX-naïve patients, a favorable risk-benefit relationship has not been established in these populations. The use of RITUXAN in patients with RA who have not had prior inadequate response to one or more TNF antagonists is not recommended [see Clinical Studies (14.6)].
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are discussed in greater detail in other sections of the labeling:
- Infusion-related reactions [see Warnings and Precautions (5.1)]
- Severe mucocutaneous reactions [see Warnings and Precautions (5.2)]
- Hepatitis B reactivation with fulminant hepatitis [see Warnings and Precautions (5.3)]
- Progressive multifocal leukoencephalopathy [see Warnings and Precautions (5.4)]
- Tumor lysis syndrome [see Warnings and Precautions (5.5)]
- Infections [see Warnings and Precautions (5.6)]
- Cardiovascular adverse reactions [see Warnings and Precautions (5.7)]
- Renal toxicity [see Warnings and Precautions (5.8)]
- Bowel obstruction and perforation [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
B-Cell Malignancies
The data described below reflect exposure to RITUXAN in 3092 patients, with exposures ranging from a single infusion up to 2 years. RITUXAN was studied in both single-arm and controlled trials (n=356 and n=2427). The population included 1180 patients with low grade or follicular lymphoma, 927 patients with DLBCL, 676 patients with CLL, and 309 pediatric patients with mature B-cell NHL/B-AL. Most NHL patients received RITUXAN as an infusion of 375 mg/m2 per infusion, given as a single agent weekly for up to 8 doses, in combination with chemotherapy for up to 8 doses, or following chemotherapy for up to 16 doses. Pediatric patients received 6 total doses of RITUXAN or a non-U.S. licensed rituximab in combination with chemotherapy. CLL patients received RITUXAN 375 mg/m2 as an initial infusion followed by 500 mg/m2 for up to 5 doses, in combination with fludarabine and cyclophosphamide. Seventy-one percent of CLL patients received 6 cycles and 90% received at least 3 cycles of RITUXAN-based therapy.
The most common adverse reactions of RITUXAN (incidence greater than or equal to 25%) observed in clinical trials of patients with NHL were infusion-related reactions, fever, lymphopenia, chills, infection, and asthenia.
The most common adverse reactions of RITUXAN (incidence greater than or equal to 25%) observed in clinical trials of patients with CLL were: infusion-related reactions and neutropenia.
Relapsed or Refractory, Low-Grade NHL
Adverse reactions presented in Table 2 occurred in 356 patients with relapsed or refractory, low-grade or follicular, CD20-positive, B-cell NHL treated in single-arm studies of RITUXAN administered as a single agent [see Clinical Studies (14.1)]. Most patients received RITUXAN 375 mg/m2 weekly for 4 doses.
| All Grades (%) | Grade 3 and 4 (%) | |
|---|---|---|
|
||
| Any Adverse Reactions | 99 | 57 |
| Body as a Whole | 86 | 10 |
| Fever | 53 | 1 |
| Chills | 33 | 3 |
| Infection | 31 | 4 |
| Asthenia | 26 | 1 |
| Headache | 19 | 1 |
| Abdominal Pain | 14 | 1 |
| Pain | 12 | 1 |
| Back Pain | 10 | 1 |
| Throat Irritation | 9 | 0 |
| Flushing | 5 | 0 |
| Heme and Lymphatic System | 67 | 48 |
| Lymphopenia | 48 | 40 |
| Leukopenia | 14 | 4 |
| Neutropenia | 14 | 6 |
| Thrombocytopenia | 12 | 2 |
| Anemia | 8 | 3 |
| Skin and Appendages | 44 | 2 |
| Night Sweats | 15 | 1 |
| Rash | 15 | 1 |
| Pruritus | 14 | 1 |
| Urticaria | 8 | 1 |
| Respiratory System | 38 | 4 |
| Increased Cough | 13 | 1 |
| Rhinitis | 12 | 1 |
| Bronchospasm | 8 | 1 |
| Dyspnea | 7 | 1 |
| Sinusitis | 6 | 0 |
| Metabolic and Nutritional Disorders | 38 | 3 |
| Angioedema | 11 | 1 |
| Hyperglycemia | 9 | 1 |
| Peripheral Edema | 8 | 0 |
| LDH Increase | 7 | 0 |
| Digestive System | 37 | 2 |
| Nausea | 23 | 1 |
| Diarrhea | 10 | 1 |
| Vomiting | 10 | 1 |
| Nervous System | 32 | 1 |
| Dizziness | 10 | 1 |
| Anxiety | 5 | 1 |
| Musculoskeletal System | 26 | 3 |
| Myalgia | 10 | 1 |
| Arthralgia | 10 | 1 |
| Cardiovascular System | 25 | 3 |
| Hypotension | 10 | 1 |
| Hypertension | 6 | 1 |
In these single-arm RITUXAN studies, bronchiolitis obliterans occurred during and up to 6 months after RITUXAN infusion.
Pediatric Patients with DLBCL/BL/BLL/B-AL
The safety of RITUXAN administered in combination with LMB chemotherapy in pediatric patients was evaluated in NHL Study 11 [see Clinical Studies (14.2)], which included 309 patients treated with RITUXAN or non-U.S. licensed rituximab with chemotherapy and 164 patients treated with chemotherapy alone. Pediatric patients randomized to the LMB chemotherapy arm with RITUXAN or non-U.S.-licensed rituximab, or enrolled in the single arm part of the study, were administered RITUXAN or non-U.S. licensed rituximab intravenous at a dose of 375 mg/m2 BSA and received a total of six infusions of RITUXAN (two during each of the two induction courses and one during each of the two consolidation courses of the LMB scheme).
In NHL Study 11, serious adverse reactions occurred in 55% of patients who received RITUXAN or non-US licensed rituximab with LMB chemotherapy. Serious adverse reactions in more than or equal to 5% included febrile neutropenia (15%), stomatitis (11%), sepsis (8%), and device-related infections (5%). Fatal adverse reactions occurred in 3% of patients, most often due to sepsis (2%), and included one case of second primary malignancy. Permanent discontinuation of RITUXAN or non- U.S. licensed rituximab occurred in 2% of patients. Adverse reactions which resulted in permanent discontinuation of RITUXAN or non-U.S. licensed rituximab included infection, anaphylaxis, hypotension, and leukoencephalopathy. Detailed safety data collection in this study was primarily limited to Grade 3 and 4 adverse reactions and serious adverse reactions.
Table 3 shows Grade 3 and higher adverse reactions (greater than or equal to 10%) in the RITUXAN or non-U.S.-licensed rituximab with chemotherapy or chemotherapy alone arms in patients with untreated mature B-cell NHL/B-AL.
The most common (greater than or equal to 15%) Grade 3 and higher adverse reactions were febrile neutropenia, stomatitis, enteritis, sepsis, alanine aminotransferase increased, and hypokalemia.
| Adverse Reaction | RITUXAN + Chemotherapy N=162 (%) | Chemotherapy N=153 (%) |
|---|---|---|
|
||
| Blood and lymphatic system disorders | ||
| Febrile Neutropenia | 93 | 91 |
| Gastrointestinal disorders | ||
| Stomatitis | 80 | 75 |
| Enteritis | 24 | 16 |
| Investigations | ||
| Alanine aminotransferase increased | 19 | 14 |
| Aspartate aminotransferase increased | 11 | 7 |
| Infections and infestations | ||
| Sepsis | 18* | 13* |
| Device Related infection | 13 | 12 |
| Lung Infection | 12 | 9 |
| Enterocolitis infections | 9 | 12 |
| Metabolism and nutrition disorders | ||
| Hypokalemia | 16 | 13 |
| Decreased appetite | 11 | 5 |
Rheumatoid Arthritis
The data presented below reflect the experience in 2578 RA patients treated with RITUXAN in controlled and long-term studies1 with a total exposure of 5014 patient-years.
Among all exposed patients, adverse reactions reported in greater than 10% of patients include infusion-related reactions, upper respiratory tract infection, nasopharyngitis, urinary tract infection, and bronchitis.
In placebo-controlled studies, patients received 2 × 500 mg or 2 × 1,000 mg intravenous infusions of RITUXAN or placebo, in combination with methotrexate, during a 24-week period. From these studies, 938 patients treated with RITUXAN (2 × 1,000 mg) or placebo have been pooled (see Table 4). Adverse reactions reported in greater than or equal to 5% of patients were hypertension, nausea, upper respiratory tract infection, arthralgia, pyrexia and pruritus (see Table 4). The rates and types of adverse reactions in patients who received RITUXAN 2 × 500 mg were similar to those observed in patients who received RITUXAN 2 × 1,000 mg.
| Adverse Reactions | Placebo + MTX N=398 n (%) | RITUXAN + MTX N=540 n (%) |
|---|---|---|
|
||
| Hypertension | 21 (5) | 43 (8) |
| Nausea | 19 (5) | 41 (8) |
| Upper Respiratory Tract Infection | 23 (6) | 37 (7) |
| Arthralgia | 14 (4) | 31 (6) |
| Pyrexia | 8 (2) | 27 (5) |
| Pruritus | 5 (1) | 26 (5) |
| Chills | 9 (2) | 16 (3) |
| Dyspepsia | 3 ( < 1) | 16 (3) |
| Rhinitis | 6 (2) | 14 (3) |
| Paresthesia | 3 ( < 1) | 12 (2) |
| Urticaria | 3 ( < 1) | 12 (2) |
| Abdominal Pain Upper | 4 (1) | 11 (2) |
| Throat Irritation | 0 (0) | 11 (2) |
| Anxiety | 5 (1) | 9 (2) |
| Migraine | 2 ( < 1) | 9 (2) |
| Asthenia | 1 ( < 1) | 9 (2) |
- 1
- Pooled studies: NCT00074438, NCT00422383, NCT00468546, NCT00299130, NCT00282308, NCT00266227, NCT02693210, NCT02093026 and NCT02097745.
Granulomatosis with Polyangiitis (GPA) (Wegener's Granulomatosis) and Microscopic Polyangiitis (MPA)
Induction Treatment of Adult Patients with Active GPA/MPA (GPA/MPA Study 1)
The data presented below from GPA/MPA Study 1 (NCT00104299) reflect the experience in 197 adult patients with active GPA and MPA treated with RITUXAN or cyclophosphamide in a single controlled study, which was conducted in two phases: a 6 month randomized, double-blind, double-dummy, active-controlled remission induction phase and an additional 12 month remission maintenance phase [see Clinical Studies (14.7)]. In the 6-month remission induction phase, 197 patients with GPA and MPA were randomized to either RITUXAN 375 mg/ m2 once weekly for 4 weeks plus glucocorticoids, or oral cyclophosphamide 2 mg/kg daily (adjusted for renal function, white blood cell count, and other factors) plus glucocorticoids to induce remission. Once remission was achieved or at the end of the 6 month remission induction period, the cyclophosphamide group received azathioprine to maintain remission. The RITUXAN group did not receive additional therapy to maintain remission. The primary analysis was at the end of the 6 month remission induction period and the safety results for this period are described below.
Adverse reactions presented below in Table 5 were adverse events which occurred at a rate of greater than or equal to 10% in the RITUXAN group. This table reflects experience in 99 GPA and MPA patients treated with RITUXAN, with a total of 47.6 patient-years of observation and 98 GPA and MPA patients treated with cyclophosphamide, with a total of 47.0 patient-years of observation. Infection was the most common category of adverse events reported (47-62%) and is discussed below.
| Adverse Reaction | RITUXAN N=99 n (%) | Cyclophosphamide N=98 n (%) |
|---|---|---|
|
||
| Nausea | 18 (18%) | 20 (20%) |
| Diarrhea | 17 (17%) | 12 (12%) |
| Headache | 17 (17%) | 19 (19%) |
| Muscle spasms | 17 (17%) | 15 (15%) |
| Anemia | 16 (16%) | 20 (20%) |
| Peripheral edema | 16 (16%) | 6 (6%) |
| Insomnia | 14 (14%) | 12 (12%) |
| Arthralgia | 13 (13%) | 9 (9%) |
| Cough | 13 (13%) | 11 (11%) |
| Fatigue | 13 (13%) | 21 (21%) |
| Increased ALT | 13 (13%) | 15 (15%) |
| Hypertension | 12 (12%) | 5 (5%) |
| Epistaxis | 11 (11%) | 6 (6%) |
| Dyspnea | 10 (10%) | 11 (11%) |
| Leukopenia | 10 (10%) | 26 (27%) |
| Rash | 10 (10%) | 17 (17%) |
Pemphigus Vulgaris (PV)
PV Study 1
PV Study 1 (NCT00784589), a randomized, controlled, multicenter open-label study, evaluated the efficacy and safety of non-U.S.-licensed rituximab in combination with short-term prednisone compared to prednisone monotherapy in 90 patients (74 Pemphigus Vulgaris [PV] patients and 16 Pemphigus Foliaceus [PF] patients) [see Clinical Studies (14.8)]. Safety results for the PV patient population during the 24-month treatment period are described below.
The safety profile of the non-U.S.-licensed rituximab in patients with PV was consistent with that observed in patients with RITUXAN-treated RA and GPA and MPA [see Adverse Reactions (6.1)].
Adverse reactions from PV Study 1 are presented below in Table 6 and were adverse events which occurred at a rate greater than or equal to 5% among PV patients treated with non-U.S.-licensed rituximab and with at least 2% absolute difference in incidence between the group treated with non-U.S.-licensed rituximab and the prednisone monotherapy group up to Month 24. No patients in the group treated with non-U.S.-licensed rituximab withdrew due to adverse reactions. The clinical study did not include sufficient number of patients to allow for direct comparison of adverse reaction rates between treatment groups.
| Adverse Reaction | Non-U.S.-licensed rituximab + short-term prednisone N=38 n (%) | Prednisone N=36 n (%) |
|---|---|---|
| N/A = not applicable | ||
|
||
| Infusion-related reactions* | 22 (58%) | N/A |
| Depression | 7 (18%) | 4 (11%) |
| Herpes simplex | 5 (13%) | 1 (3%) |
| Alopecia | 5 (13%) | 0 (0%) |
| Fatigue | 3 (8%) | 2 (6%) |
| Abdominal pain upper | 2 (5%) | 1 (3%) |
| Conjunctivitis | 2 (5%) | 0 (0%) |
| Dizziness | 2 (5%) | 0 (0%) |
| Headache | 2 (5%) | 1 (3%) |
| Herpes zoster | 2 (5%) | 1 (3%) |
| Irritability | 2 (5%) | 0 (0%) |
| Musculoskeletal pain | 2 (5%) | 0 (0%) |
| Pruritus | 2 (5%) | 0 (0%) |
| Pyrexia | 2 (5%) | 0 (0%) |
| Skin disorder | 2 (5%) | 0 (0%) |
| Skin papilloma | 2 (5%) | 0 (0%) |
| Tachycardia | 2 (5%) | 0 (0%) |
| Urticaria | 2 (5%) | 0 (0%) |
PV Study 2
In PV Study 2 (NCT02383589), a randomized, double-blind, double-dummy, active-comparator, multicenter study evaluating the efficacy and safety of RITUXAN compared to mycophenolate mofetil (MMF) in patients with moderate-to-severe PV requiring oral corticosteroids, 67 PV patients received treatment with RITUXAN (initial 1,000 mg IV on Study Day 1 and a second 1,000 mg IV on Study Day 15 repeated at Weeks 24 and 26) for up to 52 weeks [see Clinical Studies (14.8)].
In PV Study 2, ADR defined as adverse events occurring in greater than or equal to 5% of patients in the RITUXAN arms and assessed as related are shown in Table 7.
| Adverse Reactions | RITUXAN (N=67) |
|---|---|
|
|
| Infusion-related reactions | 15 (22%)* |
| Upper respiratory tract infection/ Nasopharyngitis | 11 (16%) |
| Headache | 10 (15%) |
| Asthenia/Fatigue | 9 (13%) |
| Oral candidiasis | 6 (9%) |
| Arthralgia | 6 (9%) |
| Back pain | 6 (9%) |
| Urinary tract infection | 5 (8%) |
| Dizziness | 4 (6%) |
6.2 Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other rituximab products may be misleading.
Using an ELISA assay, anti-rituximab antibody was detected in 4 of 356 (1.1%) patients with low-grade or follicular NHL receiving single-agent RITUXAN. Three of the four patients had an objective clinical response.
A total of 273/2578 (11%) patients with RA tested positive for anti-rituximab antibodies at any time after receiving RITUXAN. Anti-rituximab antibody positivity was not associated with increased rates of infusion-related reactions or other adverse events. Upon further treatment, the proportions of patients with infusion-related reactions were similar between anti-rituximab antibody positive and negative patients, and most reactions were mild to moderate. Four anti-rituximab antibody positive patients had serious infusion-related reactions, and the temporal relationship between anti-rituximab antibody positivity and infusion-related reaction was variable.
A total of 23/99 (23%) RITUXAN-treated adult patients with GPA and MPA developed anti-rituximab antibodies by 18 months in GPA/MPA Study 1. The clinical relevance of anti-rituximab antibody formation in RITUXAN-treated adult patients is unclear. In GPA/MPA Study 4, a total of 4/21 (19%) RITUXAN-treated pediatric patients with GPA and MPA developed anti-rituximab antibodies during the overall study period (assessed at Month 18).
Using a new ELISA assay, a total of 19/34 (56%) patients with PV, who were treated with non-U.S.-licensed rituximab, tested positive for anti-rituximab antibodies by 18 months in PV Study 1. In PV Study 2, a total of 20/63 (32%) RITUXAN- treated PV patients tested positive for ADA by week 52 (19 patients had treatment-inducted ADA and 1 patient had treatment-enhanced ADA). The clinical relevance of anti-rituximab antibody formation in RITUXAN-treated PV patients is unclear.
6.3 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of RITUXAN. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Hematologic: prolonged pancytopenia, marrow hypoplasia, Grade 3-4 prolonged or late-onset neutropenia, hyperviscosity syndrome in Waldenstrom's macroglobulinemia, prolonged hypogammaglobulinemia [see Warnings and Precautions (5.6)].
- Cardiac: fatal cardiac failure.
- Immune/Autoimmune Events: uveitis, optic neuritis, systemic vasculitis, pleuritis, lupus-like syndrome, serum sickness, polyarticular arthritis, and vasculitis with rash.
- Infection: viral infections, including progressive multifocal leukoencephalopathy (PML), increase in fatal infections in HIV-associated lymphoma, and a reported increased incidence of Grade 3 and 4 infections [see Warnings and Precautions (5.6)].
- Neoplasia: disease progression of Kaposi's sarcoma.
- Skin: severe mucocutaneous reactions, pyoderma gangrenosum (including genital presentation).
- Gastrointestinal: bowel obstruction and perforation.
- Pulmonary: fatal bronchiolitis obliterans and fatal interstitial lung disease.
- Nervous system: Posterior Reversible Encephalopathy Syndrome (PRES) / Reversible Posterior Leukoencephalopathy Syndrome (RPLS).
7. Drug Interactions
Formal drug interaction studies have not been performed with RITUXAN. In patients with CLL, RITUXAN did not alter systemic exposure to fludarabine or cyclophosphamide. In clinical trials of patients with RA, concomitant administration of methotrexate or cyclophosphamide did not alter the pharmacokinetics of rituximab.
8. Use In Specific Populations
8.2 Lactation
There are limited data on the presence of rituximab in human milk and the effect on the breastfed child, and there are no data on the effect on milk production. Rituximab is detected in the milk of lactating cynomolgus monkeys, and maternal IgG is present in human breast milk. Rituximab has also been reported to be excreted at low concentrations in human breast milk. Given that the clinical significance of this finding for children is not known, advise women not to breastfeed during treatment with RITUXAN and for 6 months after the last dose due to the potential of serious adverse reactions in breastfed children.
8.3 Females and Males of Reproductive Potential
RITUXAN can cause fetal harm when administered to a pregnant woman [see Use in Specific Populations (8.1)].
11. Rituxan Description
Rituximab is a genetically engineered chimeric murine/human monoclonal IgG1 kappa antibody directed against the CD20 antigen. Rituximab has an approximate molecular weight of 145 kD.
Rituximab is produced by mammalian cell (Chinese Hamster Ovary) suspension culture in a nutrient medium that may contain the antibiotic gentamicin. Gentamicin is not detectable in the final product.
RITUXAN (rituximab) injection is a sterile, preservative-free, clear, colorless solution for intravenous infusion. RITUXAN is supplied at a concentration of 10 mg/mL in either 100 mg/10 mL or 500 mg/50 mL single-dose vials. Each mL of solution contains 10 mg rituximab, polysorbate 80 (0.7 mg), sodium chloride (9 mg), sodium citrate dihydrate (7.35 mg), and Water for Injection, USP. The pH is 6.5.
12. Rituxan - Clinical Pharmacology
12.1 Mechanism of Action
Rituximab is a monoclonal antibody that targets the CD20 antigen expressed on the surface of pre-B and mature B-lymphocytes. Upon binding to CD20, rituximab mediates B-cell lysis. Possible mechanisms of cell lysis include complement dependent cytotoxicity (CDC) and antibody dependent cell mediated cytotoxicity (ADCC). B cells are believed to play a role in the pathogenesis of rheumatoid arthritis (RA) and associated chronic synovitis. In this setting, B cells may be acting at multiple sites in the autoimmune/inflammatory process, including through production of rheumatoid factor (RF) and other autoantibodies, antigen presentation, T-cell activation, and/or proinflammatory cytokine production.
12.3 Pharmacokinetics
Granulomatosis with Polyangiitis (GPA) (Wegener's Granulomatosis) and Microscopic Polyangiitis
The PK parameters in adult and pediatric patients 6 years to 17 years of age with GPA/MPA receiving 375 mg/m2 intravenous RITUXAN or non-U.S.-licensed rituximab once weekly for four doses are summarized in Table 8.
| Parameter | Statistic | Study | |
|---|---|---|---|
| Pediatric GPA/MPA (GPA/MPA Study 4) | Adult GPA/MPA (GPA/MPA Study 1) |
||
| N | Number of Patients | 25 | 97 |
| Terminal Half-life (days) | Median (Range) | 22 (11 to 42) | 25 (11 to 52) |
| AUC0-180d
(µg/mL*day) | Median (Range) | 9787 (4838 to 20446) | 10302 (3653 to 21874) |
| Clearance (L/day) | Median (Range) | 0.222 (0.0996 to 0.381) | 0.279 (0.113 to 0.653) |
| Volume of Distribution (L) | Median (Range) | 2.28 (1.43 to 3.17) | 3.12 (2.42 to 3.91) |
Based on a population PK analysis in pediatric patients with GPA and MPA, the PK parameters of rituximab were similar to those in adults with GPA and MPA, once taking into account the BSA effect on clearance and volume of distribution parameters. The population PK analysis in adults with GPA and MPA showed that male patients and patients with higher BSA or positive anti-rituximab antibody levels have higher clearance. However, further dose adjustment based on gender or anti-rituximab antibody status is not necessary.
Pemphigus Vulgaris
The PK parameters in adult PV patients receiving 1,000 mg IV infusion of RITUXAN at Days 1, 15, 168, and 182 are summarized in Table 9.
| Parameter | Infusion Cycle | |
|---|---|---|
| 1st cycle of 1,000 mg Day 1 and Day 15 N=67 | 2nd cycle of 1,000 mg Day 168 and Day 182 N=67 |
|
| Terminal Half-life (days) | ||
| Median | 21.1 | 26.2 |
| (Range) | (9.3 to 36.2) | (16.4 to 42.8) |
| Clearance (L/day) | ||
| Median | 0.30 | 0.24 |
| (Range) | (0.16 to 1.51) | (0.13 to 0.45) |
| Central Volume of Distribution (L) | ||
| Median | 3.49 (2.48 to 5.22) | 3.49 (2.48 to 5.22) |
| (Range) | ||
Following the first cycle of rituximab administration, the PK parameters of rituximab in patients with PV were similar to those in patients with RA and in patients with GPA/MPA. Following the 2nd cycle of rituximab administration, rituximab clearance decreased by 22% assuming Pemphigus Disease Area Index (PDAI) activity score of 0 at the start of both cycles, while the central volume of distribution remained unchanged. The presence of anti-rituximab antibodies was associated with a higher clearance resulting in lower rituximab concentrations.
Specific Populations
The clearance and volume of distribution of rituximab increased with increasing body surface area (BSA).
No formal studies were conducted to examine the effects of either renal or hepatic impairment on the pharmacokinetics of rituximab.
Pediatric patients
The pharmacokinetics of rituximab have been studied in pediatric patients 6 years of age and older with active GPA and MPA (GPA/MPA Study 4). The effect of body surface area on the pharmacokinetics of rituximab was assessed in a population pharmacokinetic analysis which included 6 patients 6 years to less than 12 years of age and 19 patients 12 years to 17 years of age with GPA and MPA. BSA was a significant covariate on rituximab pharmacokinetics. The median AUC0-180d in patients 2 years to 5 years of age (BSA of 0.5 m2) was estimated to be 10100 (µg/mL*day) and is comparable to that in adults. For follow up treatment of pediatric patients with GPA/MPA, the 250 mg/m2 dose is estimated to provide pediatric GPA and MPA patients with exposure comparable to that observed in adults [see Use in Special Populations (8.4) and Clinical Studies (14.7)].
In the clinical trial studying pediatric patients with DLBCL/BL/BLL/B-AL (NHL Study 11), the PK of rituximab was studied in a subset of 35 patients aged 3 years and older. The PK was comparable between the two age groups (greater than or equal to 3 to less than 12 years vs. greater than or equal to 12 to less than 18 years) (Table 10). After two RITUXAN IV infusions of 375 mg/m2 in each of the two induction cycles (cycle 1 and 2) followed by one RITUXAN IV infusion of 375 mg/m2 in each of the consolidation cycles (cycle 3 and 4), the maximum concentration was highest after the fourth infusion (cycle 2). With this dosing regimen, trough concentrations were sustained. The PK characteristics of RITUXAN IV in pediatric patients aged 3 years and older with DLBCL/BL/BLL/B-AL were similar to what has been observed in adult NHL patients. No PK data are available in the greater than or equal to 6 months to less than 3 years age group [see Use in Special Populations (8.4) and Clinical Studies (14.2)].
| Age group | Greater than or equal to 3 to less than 12 years | Greater than or equal to 12 to less than 18 years |
|---|---|---|
| Results are presented as median (min – max); Cmax is at Cycle 2 after 4th infusion; Ctrough is at pre-dose Cycle 4; AUC 0-inf and T1/2 are at Cycle 4. | ||
| Cmax (µg/mL) | 374 (292, 446) | 297 (242, 394) |
| Ctrough (µg/mL) | 61.4 (34.9, 126) | 39.5 (19.2, 93.2) |
| AUC0-inf (µg*day/mL) | 5040 (3380, 10400) | 5040 (2740, 6970) |
| T1/2 (days) | 25.7 (18.0, 31.0) | 26.3 (16.9, 31.9) |
14. Clinical Studies
14.1 Relapsed or Refractory, Low-Grade or Follicular, CD20-Positive, B-Cell NHL
The safety and effectiveness of RITUXAN in relapsed, refractory CD20+ NHL were demonstrated in 3 single-arm studies enrolling 296 patients.
Bulky Disease
In pooled data from studies 1 and 3, 39 patients with bulky (single lesion > 10 cm in diameter) and relapsed or refractory, low-grade NHL received RITUXAN 375 mg/m2 weekly for 4 doses. Results are summarized in Table 11.
| Study 1 Weekly × 4 N=166 | Study 2 Weekly × 8 N=37 | Study 1 and Study 3 Bulky disease, Weekly × 4 N=39* | Study 3 Retreatment, Weekly × 4 N=60 |
|
|---|---|---|---|---|
|
||||
| Overall Response Rate | 48% | 57% | 36% | 38% |
| Complete Response Rate | 6% | 14% | 3% | 10% |
| Median Duration of Response†, ‡, § | 11.2 | 13.4 | 6.9 | 15.0 |
| (Months) [Range] | [1.9 to 42.1+] | [2.5 to 36.5+] | [2.8 to 25.0+] | [3.0 to 25.1+] |
14.2 Previously Untreated, Low-Grade or Follicular, CD20-Positive, B-Cell NHL
The safety and effectiveness of RITUXAN in previously untreated, low-grade or follicular, CD20+ NHL were demonstrated in 3 randomized, controlled trials enrolling 1,662 patients.
NHL Study 4
A total of 322 patients with previously untreated follicular NHL were randomized (1:1) to receive up to eight 3-week cycles of CVP chemotherapy alone (CVP) or in combination with RITUXAN 375 mg/m2 on Day 1 of each cycle (R-CVP) in an open-label, multicenter study. The main outcome measure of the study was progression-free survival (PFS) defined as the time from randomization to the first of progression, relapse, or death.
Twenty-six percent of the study population was >60 years of age, 99% had Stage III or IV disease, and 50% had an International Prognostic Index (IPI) score greater than or equal to 2. The results for PFS as determined by a blinded, independent assessment of progression are presented in Table 12. The point estimates may be influenced by the presence of informative censoring. The PFS results based on investigator assessment of progression were similar to those obtained by the independent review assessment.
| Study Arm | ||
|---|---|---|
| R-CVP N=162 | CVP N=160 |
|
|
||
| Median PFS (years)* | 2.4 | 1.4 |
| Hazard ratio (95% CI)† | 0.44 (0.29, 0.65) | |
NHL Study 5
An open-label, multicenter, randomized (1:1) study was conducted in 1,018 patients with previously untreated follicular NHL who achieved a response (CR or PR) to RITUXAN in combination with chemotherapy. Patients were randomized to RITUXAN as single-agent maintenance therapy, 375 mg/m2 every 8 weeks for up to 12 doses or to observation. RITUXAN was initiated at 8 weeks following completion of chemotherapy. The main outcome measure of the study was progression-free survival (PFS), defined as the time from randomization in the maintenance/observation phase to progression, relapse, or death, as determined by independent review.
Of the randomized patients, 40% were greater than or equal to 60 years of age, 70% had Stage IV disease, 96% had ECOG performance status (PS) 0–1, and 42% had FLIPI scores of 3–5. Prior to randomization to maintenance therapy, patients had received R-CHOP (75%), R-CVP (22%), or R-FCM (3%); 71% had a complete or unconfirmed complete response and 28% had a partial response.
PFS was longer in patients randomized to RITUXAN as single agent maintenance therapy (HR: 0.54, 95% CI: 0.42, 0.70). The PFS results based on investigator assessment of progression were similar to those obtained by the independent review assessment.
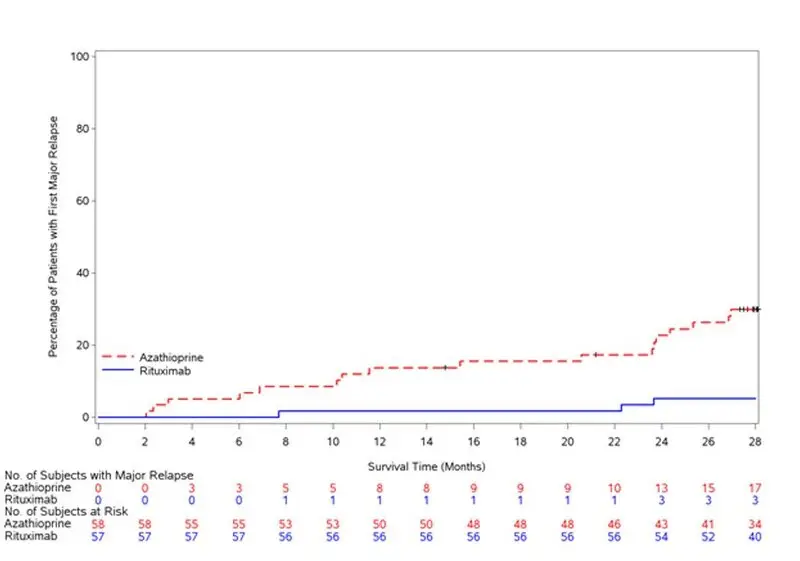
| Figure 1 |
|---|
| Kaplan-Meier Plot of IRC Assessed PFS in NHL Study 5 |
 |
NHL Study 11
RITUXAN in combination with chemotherapy was evaluated in Inter-B-NHL Ritux 2010 (NCT01516580), a multicenter, open-label, randomized trial of patients with previously untreated, advanced stage, CD20-positive DLBCL/BL/BLL/B-AL aged 6 months and older. Advanced stage is defined as Stage III with elevated lactose dehydrogenase (LDH) level [LDH greater than twice the institutional upper limit of the adult normal values] or stage IV B-cell NHL or B-AL. LMB therapy was administered based on the clinical group classification of group B (stage III with high LDH and non-central nervous system (CNS) (Stage IV), group C1 (B-AL, CNS positive and cerebrospinal fluid (CSF) negative) and C3 (CSF positive).
Patients were randomized to Lymphome Malin B (LMB) chemotherapy (corticosteroids, vincristine, cyclophosphamide, high-dose methotrexate, cytarabine, doxorubicin, etoposide and triple drug [methotrexate/cytarabine/ corticosteroid] intrathecal therapy) alone or in combination with RITUXAN or non-U.S. licensed rituximab, administered as six infusions of RITUXAN IV at a dose of 375 mg/m2 BSA (two doses during each of the two induction courses and one during each of the two consolidation courses) as per the LMB scheme [see Dosage and Administration (2.2)].
The trial was planned to enroll 600 patients with 1:1 randomization. The randomization was stopped early for efficacy after 362 patients had been enrolled (181 in each arm) according to the first planned interim analysis result. A total of 328 randomized patients, aged 6 months and older, were included in the efficacy analyses, of which one patient under 3 years of age received intravenous RITUXAN or non-U.S.-licensed rituximab in combination with LMB chemotherapy. Demographic and disease characteristics of the randomized trial population are displayed in Table 13:
| RITUXAN + LMB Chemotherapy N = 164 | LMB Chemotherapy N = 164 |
|
|---|---|---|
| BSA= Body Surface Area, B-AL=B-Cell Acute Leukemia, DLBCL= Diffuse Large B-cell Lymphoma, NHL= Non-Hodgkin's Lymphoma , CNS= Central Nervous System | ||
| Male | 82% | 84% |
| Female | 18% | 17% |
| Age (years) | ||
| Median (range) | 8 (2, 17) | 7 (1, 17) |
| Age group | ||
| 6 months to less than 3 years | 0.6% | 4% |
| 3 to less than 12 years | 71% | 71% |
| 12 to less than 18 years | 29% | 25% |
| BSA (m2) | ||
| Median (range) | 1.0 (0.6, 2.3) | 0.97 (0.5, 2.7) |
| Therapeutic group | ||
| Group B high-risk | 49% | 51% |
| Group C1 | 40% | 40% |
| Group C3 | 11% | 10% |
| Disease Type | ||
| B-AL | 37% | 34% |
| Burkitt or Burkitt-like NHL | 55% | 56% |
| DLBCL | 8% | 8% |
| Bone marrow involvement | 45% | 45% |
| CNS involvement | 27% | 27% |
Efficacy was established based on event-free survival (EFS), where an event was defined as occurrence of progressive disease, relapse, second malignancy, death from any cause, or non-response as evidenced by detection of viable cells in residue after the second CYVE course, whichever occurs first.
Efficacy analyses were performed in 328 randomized patients with a median follow-up of 3.1 years. The results are described in Table 14.
| Analysis | LMB (N = 164) | R-LMB (N=164) |
|---|---|---|
| CI = confidence interval; EFS = event-free survival; HR = hazard ratio; ITT = intent-to-treat | ||
|
||
| EFS* | 28 events | 10 events |
| Two-sided unstratified log-rank test p-value 0.0012† | ||
| Adjusted Cox HR‡ 0.32 (90% CI: 0.17, 0.58) | ||
As of data cutoff date of 31 December 2017, there were 20 and 8 deaths reported in LMB arm and R-LMB arm, respectively, with an estimated overall survival (OS) HR of 0.36 (95% CI, 0.16 - 0.81). No formal statistical test was conducted for overall survival and therefore the OS result is considered descriptive.
14.3 Diffuse Large B-Cell NHL (DLBCL)
The safety and effectiveness of RITUXAN were evaluated in three randomized, active-controlled, open-label, multicenter studies with a collective enrollment of 1854 patients. Patients with previously untreated diffuse large B-cell NHL received RITUXAN in combination with cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP) or other anthracycline-based chemotherapy regimens.
NHL Study 9
A total of 823 patients with DLBCL, aged 18–60 years, were randomized in a 1:1 ratio to receive an anthracycline-containing chemotherapy regimen alone or in combination with RITUXAN. The main outcome measure of the study was time to treatment failure, defined as time from randomization to the earliest of progressive disease, failure to achieve a complete response, relapse, or death. Among all enrolled patients, 28% had Stage III–IV disease, 100% had IPI scores of less than or equal to 1, 99% had ECOG performance status of < 2, 29% had elevated LDH levels, 49% had bulky disease, and 34% had extranodal involvement. Efficacy results are presented in Table 15.
| Study 7 (n = 632) | Study 8 (n = 399) | Study 9 (n = 823) |
||||||
|---|---|---|---|---|---|---|---|---|
| R-CHOP | CHOP | R-CHOP | CHOP | R-Chemo | Chemo | |||
| Main outcome | Progression-free survival (years) | Event-free survival (years) | Time to treatment failure (years) |
|||||
|
||||||||
| Median of main outcome measure | 3.1 | 1.6 | 2.9 | 1.1 | NE* | NE* | ||
| Hazard ratio† | 0.69‡ | 0.60‡ | 0.45‡ | |||||
| Overall survival at 2 years§ | 74% | 63% | 69% | 58% | 95% | 86% | ||
| Hazard ratio† | 0.72‡ | 0.68‡ | 0.40‡ | |||||
In NHL Study 8, overall survival estimates at 5 years were 58% vs. 46% for R-CHOP and CHOP, respectively.
14.4 Ninety-Minute Infusions in Previously Untreated Follicular NHL and DLBCL
In NHL Study 10, a total of 363 patients with previously untreated follicular NHL (n=113) or DLBCL (n=250) were evaluated in a prospective, open-label, multi-center, single-arm trial for the safety of 90-minute rituximab infusions. Patients with follicular NHL received rituximab 375 mg/m2 plus CVP chemotherapy. Patients with DLBCL received rituximab 375 mg/m2 plus CHOP chemotherapy. Patients with clinically significant cardiovascular disease were excluded from the study. Patients were eligible for a 90-minute infusion at Cycle 2 if they did not experience a Grade 3-4 infusion-related adverse event with Cycle 1 and had a circulating lymphocyte count less than or equal to 5,000/mm3 before Cycle 2. All patients were pre-medicated with acetaminophen and an antihistamine and received the glucocorticoid component of their chemotherapy prior to RITUXAN infusion. The main outcome measure was the development of Grade 3-4 infusion-related reactions on the day of, or day after, the 90-minute infusion at Cycle 2 [see Adverse Reactions (6.1)].
Eligible patients received their Cycle 2 rituximab infusion over 90 minutes as follows: 20% of the total dose given in the first 30 minutes and the remaining 80% of the total dose given over the next 60 minutes [see Dosage and Administration (2.1)]. Patients who tolerated the 90-minute rituximab infusion at Cycle 2 continued to receive subsequent rituximab infusions at the 90-minute infusion rate for the remainder of the treatment regimen (through Cycle 6 or Cycle 8).
The incidence of Grade 3-4 infusion-related reactions at Cycle 2 was 1.1% (95% CI [0.3%, 2.8%]) among all patients, 3.5% (95% CI [1.0%, 8.8%]) for those patients treated with R-CVP, and 0.0% (95% CI [0.0%, 1.5%]) for those patients treated with R-CHOP. For Cycles 2-8, the incidence of Grade 3-4 infusion-related reactions was 2.8% (95% CI [1.3%, 5.0%]). No acute fatal infusion-related reactions were observed.
14.5 Chronic Lymphocytic Leukemia (CLL)
The safety and effectiveness of RITUXAN were evaluated in two randomized (1:1) multicenter open-label studies comparing FC alone or in combination with RITUXAN for up to 6 cycles in patients with previously untreated CLL [CLL Study 1 (n=817)] or previously treated CLL [CLL Study 2 (n=552)]. Patients received fludarabine 25 mg/m2/day and cyclophosphamide 250 mg/m2/day on days 1, 2 and 3 of each cycle, with or without RITUXAN. In both studies, seventy-one percent of CLL patients received 6 cycles and 90% received at least 3 cycles of RITUXAN-based therapy.
In CLL Study 1, 30% of patients were 65 years or older, 31% were Binet stage C, 45% had B symptoms, more than 99% had ECOG performance status (PS) 0–1, 74% were male, and 100% were White. In CLL Study 2, 44% of patients were 65 years or older, 28% had B symptoms, 82% received a prior alkylating drug, 18% received prior fludarabine, 100% had ECOG PS 0–1, 67% were male and 98% were White.
The main outcome measure in both studies was progression-free survival (PFS), defined as the time from randomization to progression, relapse, or death, as determined by investigators (CLL Study 1) or an independent review committee (CLL Study 2). The investigator assessed results in CLL Study 2 were supportive of those obtained by the independent review committee. Efficacy results are presented in Table 16.
| Study 1*
(Previously untreated) | Study 2*
(Previously treated) |
|||
|---|---|---|---|---|
| R-FC N = 408 | FC N = 409 | R-FC N = 276 | FC N = 276 |
|
|
||||
| Median PFS (months) | 39.8 | 31.5 | 26.7 | 21.7 |
| Hazard ratio (95% CI) | 0.56 (0.43, 0.71) | 0.76 (0.6, 0.96) | ||
| P value (Log-Rank test) | < 0.01 | 0.02 | ||
| Response rate (95% CI) | 86% (82, 89) | 73% (68, 77) | 54% (48, 60) | 45% (37, 51) |
Across both studies, 243 of 676 RITUXAN-treated patients (36%) were 65 years of age or older and 100 RITUXAN-treated patients (15%) were 70 years of age or older. The results of exploratory subset analyses in elderly patients are presented in Table 17.
| Study 1 | Study 2 | |||
|---|---|---|---|---|
| Age subgroup | Number of Patients | Hazard Ratio for PFS (95% CI) | Number of Patients | Hazard Ratio for PFS (95% CI) |
|
||||
| Age less than 65 yrs | 572 | 0.52 (0.39, 0.70) | 313 | 0.61 (0.45, 0.84) |
| Age greater than or equal to 65 yrs | 245 | 0.62 (0.39, 0.99) | 233 | 0.99 (0.70, 1.40) |
| Age less than 70 yrs | 736 | 0.51 (0.39, 0.67) | 438 | 0.67 (0.51, 0.87) |
| Age greater than or equal to 70 yrs | 81 | 1.17 (0.51, 2.66) | 108 | 1.22 (0.73, 2.04) |
14.6 Rheumatoid Arthritis (RA)
Reducing the Signs and Symptoms: Initial and Re-Treatment Courses
The efficacy and safety of RITUXAN were evaluated in two randomized, double-blind, placebo-controlled studies of adult patients with moderately to severely active RA who had a prior inadequate response to at least one TNF inhibitor. Patients were 18 years of age or older, diagnosed with active RA according to American College of Rheumatology (ACR) criteria, and had at least 8 swollen and 8 tender joints.
In RA Study 1 (NCT00468546), patients were randomized to receive either RITUXAN 2 × 1,000 mg + MTX or placebo + MTX for 24 weeks. Further courses of RITUXAN 2 × 1,000 mg + MTX were administered in an open label extension study at a frequency determined by clinical evaluation, but no sooner than 16 weeks after the preceding course of RITUXAN. In addition to the intravenous premedication, glucocorticoids were administered orally on a tapering schedule from baseline through Day 14. The proportions of patients achieving ACR 20, 50, and 70 responses at Week 24 of the placebo-controlled period are shown in Table 18.
In RA Study 2 (NCT00266227), all patients received the first course of RITUXAN 2 × 1,000 mg + MTX. Patients who experienced ongoing disease activity were randomized to receive a second course of either RITUXAN 2 × 1,000 mg + MTX or placebo + MTX, the majority between Weeks 24–28. The proportions of patients achieving ACR 20, 50, and 70 responses at Week 24, before the re-treatment course, and at Week 48, after retreatment, are shown in Table 18.
| Inadequate Response to TNF Antagonists | ||||||||
|---|---|---|---|---|---|---|---|---|
| Study 1 24 Week Placebo-Controlled (Week 24) | Study 2 Placebo-Controlled Retreatment (Week 24 and Week 48) |
|||||||
| Response | Placebo + MTX n = 201 | RITUXAN + MTX n = 298 | Treatment Difference (RITUXAN – Placebo)* (95% CI) | Response | Placebo + MTX Retreatment n = 157 | RITUXAN + MTX Retreatment n = 318 | Treatment Difference (RITUXAN – Placebo)†,‡,* (95% CI) |
|
|
||||||||
| ACR20 | ACR20 | |||||||
| Week 24 | 18% | 51% | 33% (26%, 41%) | Week 24 | 48% | 45% | NA | |
| Week 48 | 45% | 54% | 11% (2%, 20%) |
|||||
| ACR50 | ACR50 | |||||||
| Week 24 | 5% | 27% | 21% (15%, 27%) | Week 24 | 27% | 21% | NA | |
| Week 48 | 26% | 29% | 4% (-4%, 13%) |
|||||
| ACR70 | ACR70 | |||||||
| Week 24 | 1% | 12% | 11% (7%, 15%) | Week 24 | 11% | 8% | NA | |
| Week 48 | 13% | 14% | 1% (-5%, 8%) |
|||||
Improvement was also noted for all components of ACR response following treatment with RITUXAN, as shown in Table 19.
| Inadequate Response to TNF Antagonists | ||||
|---|---|---|---|---|
| Parameter (median) | Placebo + MTX (n = 201) | RITUXAN + MTX (n = 298) |
||
| Baseline | Wk 24 | Baseline | Wk 24 | |
|
||||
| Tender Joint Count | 31.0 | 27.0 | 33.0 | 13.0 |
| Swollen Joint Count | 20.0 | 19.0 | 21.0 | 9.5 |
| Physician Global Assessment* | 71.0 | 69.0 | 71.0 | 36.0 |
| Patient Global Assessment* | 73.0 | 68.0 | 71.0 | 41.0 |
| Pain* | 68.0 | 68.0 | 67.0 | 38.5 |
| Disability Index (HAQ)† | 2.0 | 1.9 | 1.9 | 1.5 |
| CRP (mg/dL) | 2.4 | 2.5 | 2.6 | 0.9 |
The time course of ACR 20 response for RA Study 1 is shown in Figure 2. Although both treatment groups received a brief course of intravenous and oral glucocorticoids, resulting in similar benefits at Week 4, higher ACR 20 responses were observed for the RITUXAN group by Week 8. A similar proportion of patients achieved these responses through Week 24 after a single course of treatment (2 infusions) with RITUXAN. Similar patterns were demonstrated for ACR 50 and 70 responses.
| Figure 2 |
|---|
|
| Percent of Patients Achieving ACR 20 Response by Visit*
RA Study 1 (Inadequate Response to TNF Antagonists) |
 |
Radiographic Response
In RA Study 1, structural joint damage was assessed radiographically and expressed as changes in Genant-modified Total Sharp Score (TSS) and its components, the erosion score (ES) and the joint space narrowing (JSN) score. RITUXAN + MTX slowed the progression of structural damage compared to placebo + MTX after 1 year as shown in Table 20.
| Inadequate Response to TNF Antagonists | ||||
|---|---|---|---|---|
| Parameter | RITUXAN 2 × 1,000 mg + MTX* | Placebo + MTX† | Treatment Difference (Placebo – RITUXAN) | 95% CI |
|
||||
| Change during First Year | ||||
| TSS | 0.66 | 1.77 | 1.11 | (0.47, 1.75) |
| ES | 0.44 | 1.19 | 0.75 | (0.32, 1.19) |
| JSN Score | 0.22 | 0.58 | 0.36 | (0.10, 0.62) |
| Change during Second Year‡ | ||||
| TSS | 0.48 | 1.04 | — | — |
| ES | 0.28 | 0.62 | — | — |
| JSN Score | 0.20 | 0.42 | — | — |
In RA Study 1 and its open-label extension, 70% of patients initially randomized to RITUXAN + MTX and 72% of patients initially randomized to placebo + MTX were evaluated radiographically at Year 2. As shown in Table 20, progression of structural damage in RITUXAN + MTX patients was further reduced in the second year of treatment.
Following 2 years of treatment with RITUXAN + MTX, 57% of patients had no progression of structural damage. During the first year, 60% of RITUXAN + MTX treated patients had no progression, defined as a change in TSS of zero or less compared to baseline, compared to 46% of placebo + MTX treated patients. In their second year of treatment with RITUXAN + MTX, more patients had no progression than in the first year (68% vs. 60%), and 87% of the RITUXAN + MTX treated patients who had no progression in the first year also had no progression in the second year.
Physical Function Response
RA Study 4 (NCT00299130) is a randomized, double-blind, placebo-controlled study in adult RA patients with moderately to severely active disease with inadequate response to MTX. Patients were randomized to receive an initial course of RITUXAN 500 mg, RITUXAN 1,000 mg, or placebo in addition to background MTX.
Physical function was assessed at Weeks 24 and 48 using the Health Assessment Questionnaire Disability Index (HAQ-DI). From baseline to Week 24, a greater proportion of RITUXAN-treated patients had an improvement in HAQ-DI of at least 0.22 (a minimal clinically important difference) and a greater mean HAQ-DI improvement compared to placebo, as shown in Table 21. HAQ-DI results for the RITUXAN 500 mg treatment group were similar to the RITUXAN 1,000 mg treatment group; however radiographic responses were not assessed (see Dosing Precaution in the Radiographic Responses section above). These improvements were maintained at 48 weeks.
| Placebo + MTX n = 172 | RITUXAN 2 × 1,000 mg + MTX n = 170 | Treatment Difference (RITUXAN – Placebo)* (95% CI) |
|
|---|---|---|---|
|
|||
| Mean Improvement from Baseline | 0.19 | 0.42 | 0.23 (0.11, 0.34) |
| Percent of patients with "Improved" score (Change from Baseline greater than or equal to MCID)† | 48% | 58% | 11% (0%, 21%) |
14.7 Granulomatosis with Polyangiitis (GPA) (Wegener's Granulomatosis) and Microscopic Polyangiitis (MPA)
Induction Treatment of Adult Patients with Active Disease (GPA/MPA Study 1)
A total of 197 patients with active, severe GPA and MPA (two forms of ANCA Associated Vasculitides) were treated in a randomized, double-blind, active-controlled, multicenter, non-inferiority study, conducted in two phases – a 6 month remission induction phase and a 12 month remission maintenance phase. Patients were 15 years of age or older, diagnosed with GPA (75% of patients) or MPA (24% of patients) according to the Chapel Hill Consensus conference criteria (1% of the patients had unknown vasculitis type). All patients had active disease, with a Birmingham Vasculitis Activity Score for Granulomatosis with Polyangiitis (BVAS/GPA) greater than or equal to 3, and their disease was severe, with at least one major item on the BVAS/GPA. Ninety-six (49%) of patients had new disease and 101 (51%) of patients had relapsing disease.
Patients in both arms received 1,000 mg of pulse intravenous methylprednisolone per day for 1 to 3 days within 14 days prior to initial infusion. Patients were randomized in a 1:1 ratio to receive either RITUXAN 375 mg/m2 once weekly for 4 weeks or oral cyclophosphamide 2 mg/kg daily for 3 to 6 months in the remission induction phase. Patients were pre-medicated with antihistamine and acetaminophen prior to RITUXAN infusion. Following intravenous corticosteroid administration, all patients received oral prednisone (1 mg/kg/day, not exceeding 80 mg/day) with pre-specified tapering. Once remission was achieved or at the end of the 6 month remission induction period, the cyclophosphamide group received azathioprine to maintain remission. The RITUXAN group did not receive additional therapy to maintain remission. The main outcome measure for both GPA and MPA patients was achievement of complete remission at 6 months defined as a BVAS/GPA of 0, and off glucocorticoid therapy. The pre-specified non-inferiority margin was a treatment difference of 20%. As shown in Table 22, the study demonstrated non-inferiority of RITUXAN to cyclophosphamide for complete remission at 6 months.
| RITUXAN (n = 99) | Cyclophosphamide (n = 98) | Treatment Difference (RITUXAN – Cyclophosphamide) |
|
|---|---|---|---|
|
|||
| Rate | 64% | 53% | 11% |
| 95.1%* CI | (54%, 73%) | (43%, 63%) | (-3%, 24%) † |
Follow up Treatment of Adult Patients with GPA/MPA who have achieved disease control with other Immunosuppressant (GPA/MPA Study 2)
A total of 115 patients (86 with GPA, 24 with MPA, and 5 with renal-limited ANCA-associated vasculitis) in disease remission were randomized to receive azathioprine (58 patients) or non-U.S.-licensed rituximab (57 patients) in this open-label, prospective, multi-center, randomized, active-controlled study. Eligible patients were 21 years and older and had either newly diagnosed (80%) or relapsing disease (20%). A majority of the patients were ANCA-positive. Remission of active disease was achieved using a combination of glucocorticoids and cyclophosphamide. Within a maximum of 1 month after the last cyclophosphamide dose, eligible patients (based on BVAS of 0), were randomized in a 1:1 ratio to receive either non-U.S.-licensed rituximab or azathioprine.
The non-U.S.-licensed rituximab was administered as two 500 mg intravenous infusions separated by two weeks (on Day 1 and Day 15) followed by a 500 mg intravenous infusion every 6 months for 18 months. Azathioprine was administered orally at a dose of 2 mg/kg/day for 12 months, then 1.5 mg/kg/day for 6 months, and finally 1 mg/kg/day for 4 months; treatment was discontinued after 22 months. Prednisone treatment was tapered and then kept at a low dose (approximately 5 mg per day) for at least 18 months after randomization. Prednisone dose tapering and the decision to stop prednisone treatment after month 18 were left at the investigator's discretion.
Planned follow-up was until month 28 (10 or 6 months, respectively, after the last non-U.S.-licensed rituximab infusion or azathioprine dose). The primary endpoint was the occurrence of major relapse (defined by the reappearance of clinical and/or laboratory signs of vasculitis activity that could lead to organ failure or damage, or could be life threatening) through month 28.
By month 28, major relapse occurred in 3 patients (5%) in the non-U.S.-licensed rituximab group and 17 patients (29%) in the azathioprine group.
The observed cumulative incidence rate of first major relapse during the 28 months was lower in patients on non-U.S.-licensed rituximab relative to azathioprine (Figure 3).
| Figure 3 Cumulative Incidence Over Time of First Major Relapse in Patients with GPA/MPA |
|---|
| Patients were censored at the last follow-up dates if they had no event |
|
|
Treatment of Pediatric Patients (GPA/MPA Study 4)
The study design consisted of an initial 6-month remission induction phase, and a minimum 12-month follow-up phase up to a maximum of 54 months (4.5 years) in pediatric patients 2 years to 17 years of age with GPA and MPA. Patients were to receive a minimum of 3 doses of intravenous methylprednisolone (30 mg/kg/day, not exceeding 1g/day) prior to the first RITUXAN or non-U.S.-licensed rituximab intravenous infusion. If clinically indicated, additional daily doses (up to three), of intravenous methylprednisolone could be given. The remission induction regimen consisted of four once weekly intravenous infusions of RITUXAN or non-U.S.-licensed rituximab at a dose of 375 mg/m2 BSA, on study days 1, 8, 15 and 22 in combination with oral prednisolone or prednisone at 1 mg/kg/day (max 60 mg/day) tapered to 0.2 mg/kg/day minimum (max 10 mg/day) by Month 6. After the remission induction phase, patients could receive subsequent RITUXAN or non-U.S.-licensed rituximab intravenous infusions on or after Month 6 to maintain remission and control disease activity.
The primary objectives of this study were to evaluate safety and PK parameters in pediatric GPA and MPA patients (2 years to 17 years of age). The efficacy objectives of the study were exploratory and principally assessed using the Pediatric Vasculitis Activity Score (PVAS).
A total of 25 pediatric patients 6 years to 17 years of age with active GPA and MPA were treated with RITUXAN or non-U.S.-licensed rituximab in a multicenter, open-label, single-arm, uncontrolled study (NCT01750697). The median age of patients in the study was 14 years and the majority of patients (20/25 [80%]) were female. A total of 19 patients (76%) had GPA and 6 patients (24%) had MPA at baseline. Eighteen patients (72%) had newly diagnosed disease upon study entry (13 patients with GPA and 5 patients with MPA) and 7 patients had relapsing disease (6 patients with GPA and 1 patient with MPA).
All 25 patients completed all four once weekly intravenous infusions for the 6-month remission induction phase. A total of 24 out of 25 patients completed at least 18 months from Day 1 (baseline).
The exploratory efficacy using the PVAS is described in Table 23.
| Time to Follow Up Since Day 1 | |||
|---|---|---|---|
| Month 6 n=25 | Month 12 n = 25 | Month 18 n = 25 |
|
| *PVAS remission is defined by a PVAS of 0 and achieved glucocorticoid taper to 0.2 mg/kg/day (or 10 mg/day, whichever is lower), or a PVAS of 0 on two consecutive readings greater than or equal to 4 weeks apart irrespective of glucocorticoid dose | |||
|
|||
| Response rate | 56% | 92% | 100% |
| 95% CI* | (34.9%, 75.6%) | (74.0%, 99.0%) | (86.3%, 100.0%) |
14.8 Pemphigus Vulgaris (PV)
PV Study 1 (NCT00784589)
Non-U.S.-licensed rituximab in combination with short-term prednisone was compared to prednisone monotherapy as first-line treatment in 90 newly diagnosed adult patients with moderate to severe pemphigus (74 Pemphigus Vulgaris [PV] and 16 Pemphigus Foliaceus [PF]) in this randomized, open-label, controlled, multicenter study (PV Study 1). Patients were between 19 and 79 years of age and had not received prior therapies for pemphigus. In the PV population, 5 (13%) patients in the group treated with non-U.S.-licensed rituximab and 3 (8%) patients in the prednisone group had moderate disease and 33 (87%) patients in the group treated with non-U.S.-licensed rituximab and 33 (92%) patients in the prednisone group had severe disease according to disease severity defined by Harman's criteria.
Patients were stratified by baseline disease severity (moderate or severe) and randomized 1:1 to receive either the non-U.S.-licensed rituximab and short-term prednisone or long-term prednisone monotherapy. Patients were pre-medicated with antihistamine, acetaminophen and methylprednisolone prior to infusion of the non-U.S.-licensed rituximab. Patients randomized to the group treated with non-U.S.-licensed rituximab received an initial intravenous infusion of 1,000 mg non-U.S.-licensed rituximab on Study Day 1 in combination with a short-term regimen of 0.5 mg/kg/day oral prednisone tapered off over 3 months if they had moderate disease or 1 mg/kg/day oral prednisone tapered off over 6 months if they had severe disease. All patients received a second intravenous infusion of 1,000 mg non-U.S.-licensed rituximab on Study Day 15. Maintenance infusions of 500 mg non-U.S.-licensed rituximab were administered at Months 12 and 18. Patients randomized to the prednisone monotherapy group received an initial 1 mg/kg/day oral prednisone tapered off over 12 months if they had moderate disease or 1.5 mg/kg/day oral prednisone tapered off over 18 months if they had severe disease. Patients in the group treated with non-U.S.-licensed rituximab who relapsed could receive an additional infusion of 1,000 mg non-U.S.-licensed rituximab in combination with reintroduced or escalated prednisone dose. Maintenance and relapse infusions were administered no sooner than 16 weeks following the previous infusion.
The primary endpoint for the study was complete remission (complete epithelialization and absence of new and/or established lesions) at Month 24 without the use of prednisone therapy for 2 months or more (CRoff for greater than or equal to 2 months).
The results of the trial are presented in Table 24.
| Non-U.S.-licensed rituximab + short-term prednisone N=46 | Prednisone N=44 |
|
|---|---|---|
| Number of responders (response rate [%]) | 41 (89%) | 15 (34%) |
| PV patients | 34/38 (90%) | 10/36 (28%) |
| PF patients | 7/8 (88%) | 5/8 (63%) |
PV Study 2 (NCT02383589)
In a randomized, double-blind, double-dummy, active-comparator, multicenter study, the efficacy and safety of RITUXAN compared to mycophenolate mofetil (MMF) were evaluated in patients with moderate-to-severe PV receiving 60-120 mg/day oral prednisone or equivalent (1.0-1.5 mg/kg/day) at study entry and tapered to reach a dose of 60 or 80 mg/day by Day 1. Patients had a confirmed diagnosis of PV within the previous 24 months and evidence of moderate-to-severe disease defined as a total Pemphigus Disease Area Index (PDAI) activity score of greater than or equal to 15. The study consisted of a screening period of up to 28 days, a 52-week double-blind treatment period, and a 48-week safety follow up period.
One hundred and thirty-five patients were randomized to treatment with RITUXAN 1,000 mg administered on Day 1, Day 15, Week 24 and Week 26 or oral MMF 2 g/day (starting at 1 g/day on Day 1 and titrated to achieve a goal of 2 g/day by Week 2) for 52 weeks in combination with an initial dose of 60 or 80 mg oral prednisone with the aim of tapering to 0 mg/day by Week 24. Randomization was stratified by duration of PV (within the 1 year prior to screening or greater than 1 year) and geographical region. A dual-assessor approach was used during the study for efficacy and safety evaluations to prevent potential unblinding.
One hundred and twenty-five patients (excluding exploratory data from ten telemedicine patients) were analyzed for efficacy (Modified Intent-to-Treat Population). The primary efficacy endpoint for this study was the proportion of subjects achieving sustained complete remission defined as achieving healing of lesions with no new active lesions (i.e., PDAI activity score of 0) while on 0 mg/day prednisone or equivalent, and maintaining this response for at least 16 consecutive weeks, during the 52-week treatment period.
Secondary endpoints included cumulative oral corticosteroid dose and the total number of disease flares.
The results of the trial are presented in Table 25.
| RITUXAN (N=62) | MMF (N=63) | Difference (95% CI) | |
|---|---|---|---|
| MMF = Mycophenolate mofetil. CI = Confidence Interval. | |||
| Number of responders (response rate [%]) | 25 (40.3%) | 6 (9.5%) | 30.80% (14.70%, 45.15%) |
16. How is Rituxan supplied
RITUXAN (rituximab) injection is a sterile, preservative-free, clear, colorless solution for intravenous infusion supplied as follows:
| Carton contents | NDC number |
|---|---|
| One 100 mg/10 mL (10 mg/mL) single-dose vial | NDC 50242-051-21 |
| Ten 100 mg/10 mL (10 mg/mL) single-dose vials | NDC 50242-051-10 |
| One 500 mg/50 mL (10 mg/mL) single-dose vial | NDC 50242-053-06 |
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised: 12/2021 | ||
| MEDICATION GUIDE
RITUXAN® (ri tuk san) (rituximab) injection |
|||
| What is the most important information I should know about RITUXAN?
RITUXAN can cause serious side effects that can lead to death including:
|
|||
|
| ||
|
|||
|
| ||
| See "What are the possible side effects of RITUXAN?" for more information about side effects. | |||
| What is RITUXAN?
RITUXAN is a prescription medicine used to treat:
|
|||
Before you or your child receive RITUXAN, tell your healthcare provider about all of your or your child's medical conditions, including if you or your child:
|
|||
|
| ||
|
|||
How will I receive RITUXAN?
|
|||
| What are the possible side effect of RITUXAN? RITUXAN can cause serious side effects, including:
|
|||
|
| ||
The most common side effects of RITUXAN include:
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 |
|||
| General information about the safe and effective use of RITUXAN.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. You can ask your pharmacist or healthcare provider for information about RITUXAN that is written for healthcare providers. |
|||
| What are the ingredients in RITUXAN?
Active ingredient: rituximab Inactive ingredients: polysorbate 80, sodium chloride, sodium citrate dihydrate, and water for injection, USP. Manufactured by: Genentech, Inc., A Member of the Roche Group, 1 DNA Way, South San Francisco, CA 94080-4990 Jointly Marketed by Biogen and Genentech USA, Inc. U.S. License Number: 1048 RITUXAN® is a registered trademark of Biogen. ©2021 Biogen and Genentech, Inc. For more information, go to www.RITUXAN.com or call 1-877-474-8892. |
|||
| RITUXAN
rituximab injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| RITUXAN
rituximab injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Genentech, Inc. (080129000) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Genentech, Inc. | 080129000 | ANALYSIS(50242-051, 50242-053) , MANUFACTURE(50242-051, 50242-053) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Genentech, Inc. | 004074162 | ANALYSIS(50242-051, 50242-053) , API MANUFACTURE(50242-051, 50242-053) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Genentech, Inc. | 146373191 | ANALYSIS(50242-051, 50242-053) , API MANUFACTURE(50242-051, 50242-053) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Genentech, Inc. | 833220176 | MANUFACTURE(50242-051, 50242-053) , PACK(50242-051, 50242-053) , LABEL(50242-051, 50242-053) , ANALYSIS(50242-051, 50242-053) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Roche Singapore Technical Operations Pte. Ltd. | 937189173 | ANALYSIS(50242-051, 50242-053) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Roche Diagnostics GmbH | 323105205 | ANALYSIS(50242-051, 50242-053) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Roche Diagnostics GmbH | 315028860 | ANALYSIS(50242-051, 50242-053) , MANUFACTURE(50242-051, 50242-053) , API MANUFACTURE(50242-051, 50242-053) | |