Drug Detail:Targiniq er (Naloxone and oxycodone extended release tablets)
Drug Class: Narcotic analgesic combinations
Highlights of Prescribing Information
TARGINIQ ER (oxycodone hydrochloride and naloxone hydrochloride extended-release tablets), for oral use, CII
Initial U.S. Approval: 2014
WARNING: ADDICTION, ABUSE, AND MISUSE; LIFE-THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL INGESTION; NEONATAL OPIOID WITHDRAWAL SYNDROME; CYTOCHROME P450 3A4 INTERACTION; and RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES AND OTHER CNS DEPRESSANTS
See full prescribing information for complete boxed warning.
- TARGINIQ ER exposes users to risks of addiction, abuse and misuse, which can lead to overdose and death. Assess patient’s risk before prescribing and monitor regularly for these behaviors and conditions. (5.1)
- Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely, especially upon initiation or following a dose increase. Instruct patients to swallow TARGINIQ ER tablets whole to avoid exposure to a potentially fatal dose of oxycodone. (5.2)
- Accidental ingestion of TARGINIQ ER, especially by children, can result in a fatal overdose of oxycodone. (5.2)
- Prolonged use of TARGINIQ ER during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated. If prolonged opioid use is required in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. (5.3)
- Concomitant use with CYP3A4 inhibitors (or discontinuation of CYP3A4 inducers) can result in a fatal overdose of oxycodone. (5.4)
- Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing for use in patients for whom alternative treatment options are inadequate; limit dosages and durations to the minimum required; and follow patients for signs and symptoms of respiratory depression and sedation. (5.5, 7)
Recent Major Changes
Indications and Usage for Targiniq ER
TARGINIQ ER is a combination product consisting of oxycodone, an opioid agonist, and naloxone, an opioid antagonist, indicated for the management of pain severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate. (1)
Limitations of Use
- Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, and because of the greater risks of overdose and death with extended-release opioid formulations, reserve TARGINIQ ER for use in patients for whom alternative treatment options (e.g., non-opioid analgesics or immediate-release opioids) are ineffective, not tolerated, or would be otherwise inadequate to provide sufficient management of pain. (1)
- TARGINIQ ER is not indicated as an as-needed (prn) analgesic. (1)
- Total daily dose should not exceed 80 mg/40 mg (40 mg/20 mg q12h) because higher doses may be associated with symptoms of opioid withdrawal. (1)
Targiniq ER Dosage and Administration
- To be prescribed only by healthcare providers knowledgeable in use of potent opioids for management of chronic pain. (2.1)
- A single dose of TARGINIQ ER greater than 40 mg/20 mg or a total daily dose greater than 80 mg/40 mg are only for use in patients in whom tolerance to an opioid of comparable potency has been established.
- Patients considered opioid tolerant are those taking, for one week or longer, at least 60 mg oral morphine per day, 25 mcg transdermal fentanyl per hour, 30 mg oral oxycodone per day, 8 mg oral hydromorphone per day, 25 mg oral oxymorphone per day, 60 mg oral hydrocodone per day, or an equianalgesic dose of another opioid. (2.1)
- Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals. (2.1)
- Individualize dosing based on the severity of pain, patient response, prior analgesic experience, and risk factors for addiction, abuse, and misuse. (2.1)
- Instruct patients to swallow tablets intact and not to cut, break, chew, crush, or dissolve tablets (risk of potentially fatal overdose). (2.1, 5.1)
- For opioid-naïve and opioid non-tolerant patients, initiate with 10 mg/5 mg tablets orally every 12 hours. (2.1)
- Mild Hepatic Impairment: Reduce the starting dose of TARGINIQ ER to 1/3 to 1/2 the usual starting dose in patients with mild hepatic impairment. (8.7)
- Renal Impairment: Reduce the initial dose to 1/2 the usual dose when administering TARGINIQ ER to patients with renal impairment. (8.8)
- Do not abruptly discontinue TARGINIQ ER in a physically dependent patient. (2.5)
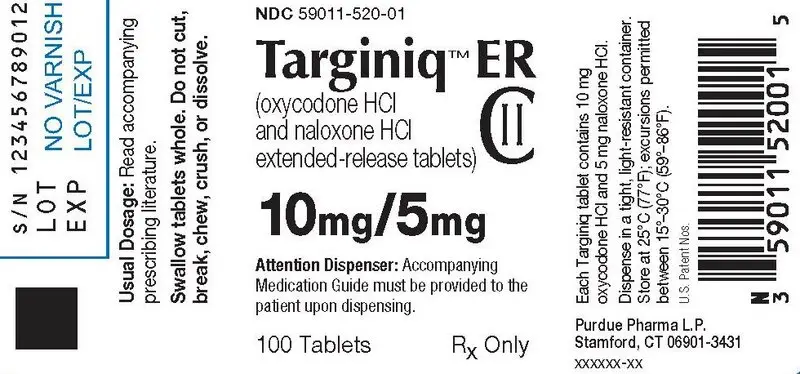
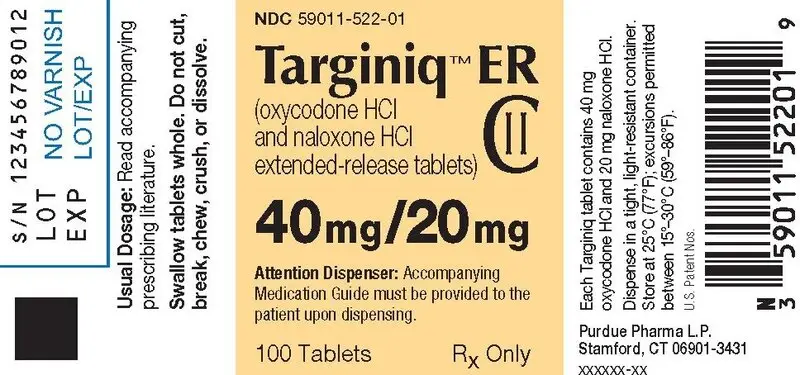
Dosage Forms and Strengths
- Extended-release tablets: 10 mg/5 mg, 20 mg/10 mg, and 40 mg/20 mg (3)
Contraindications
- Significant respiratory depression (4)
- Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment (4)
- Known or suspected gastrointestinal obstruction, including paralytic ileus (4)
- Hypersensitivity to oxycodone or naloxone (4)
- Moderate to severe hepatic impairment (4)
Warnings and Precautions
- Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients: Monitor closely, particularly during initiation and titration. (5.6)
- Adrenal Insufficiency: If diagnosed, treat with physiologic replacement of corticosteroids, and wean patient off of the opioid. (5.7)
- Severe Hypotension: Monitor during dose initiation and titration. Avoid use in patients with circulatory shock. (5.8)
- Risks of Use in Patients with Increased Intracranial Pressure, Head Injury, Brain Tumors, or Impaired Consciousness: Monitor for sedation and respiratory depression. Avoid use of TARGINIQ ER in patients with impaired consciousness or coma. (5.9)
- Withdrawal: Symptoms consistent with opioid withdrawal occurred in some patients in the clinical trials. Monitor patients for symptoms of withdrawal during treatment with TARGINIQ ER. (5.12)
Adverse Reactions/Side Effects
Most common adverse reactions (incidence ≥ 5%) were nausea and vomiting. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Purdue Pharma L.P. at 1-888-726-7535 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- CNS Depressants: Concomitant use may cause hypotension, profound sedation, respiratory depression, coma, and death. If co-administration is require decision to begin TARGINIQ ER is made, start with 1/3 to ½ the recommended starting dosage, consider a dosage of the concommitant CNS depressant, and monitor closely. (2.3, 5.5, 7)
- Serotonergic Drugs: Concomitant use may result in serotonin syndrome. Discontinue TARGINIQ ER if serotonin syndrome is suspected. (7)
- Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics: Avoid use with TARGINIQ ER because they may reduce analgesic effect of TARGINIQ ER or precipitate withdrawal symptoms. (5.12, 7)
- Monoamine Oxidase Inhibitors (MAOIs): Can potentiate the effects of morphine. Avoid concomitant use in patients receiving MAOIs or within 14 days of stopping treatment with an MAOI. (7)
Use In Specific Populations
- Pregnancy: May cause fetal harm. (8.1)
- Lactation: Not recommended. (8.2)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 12/2016
Full Prescribing Information
WARNING: ADDICTION, ABUSE, AND MISUSE; LIFE-THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL INGESTION; NEONATAL OPIOID WITHDRAWAL SYNDROME; CYTOCHROME P450 3A4 INTERACTION; and RISKS FROM CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS
- Reserve concomitant prescribing of TARGINIQ ER Injection and benzodiazepines or other CNS depressants for use in patients for whom alternative treatment options are inadequate.
-
Limit dosages and durations to
the minimum required.
Follow patients for signs and symptoms of respiratory depression and sedation.
1. Indications and Usage for Targiniq ER
- Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, and because of the greater risks of overdose and death with extended-release opioid formulations [see Warnings and Precautions (5.1)], reserve TARGINIQ ER for use in patients for whom alternative treatment options (e.g., non-opioid analgesics or immediate-release opioids) are ineffective, not tolerated, or would be otherwise inadequate to provide sufficient management of pain.
- TARGINIQ ER is not indicated as an as-needed (prn) analgesic.
- The maximum total daily dose of TARGINIQ ER should not exceed 80 mg/40 mg (40 mg/20 mg q12h) because higher doses may be associated with symptoms of opioid withdrawal or decreased analgesia [see Warnings and Precautions 5.12].
2. Targiniq ER Dosage and Administration
2.1 Important Dosing and Administration Instructions
- Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals [see Warnings and Precautions (5.1)].Initiate the dosing regimen for each patient individually, taking into account the patient's severity of pain, patient response, prior analgesic treatment experience, and risk factors for addiction, abuse, and misuse [see Warnings and Precautions (5.1)].
- Monitor patients closely for respiratory depression, especially within the first 24-72 hours of initiating therapy with TARGINIQ ER and following dosage increases with TARGINIQ and adjust the dosage accordingly [see Warnings and Precautions (5.2)].
2.2 Initial Dosage
Consider the following when using the information in Table 1 and Table 2:
- These are not tables of equianalgesic doses. The conversion factors in Table 1 are only for the conversion from one of the listed oral opioid analgesics to the Equivalent Daily Oral Morphine Dose.
- The conversion factors in Table 2 are only for conversion from the calculated Equivalent Daily Oral Morphine Dose to TARGINIQ ER.
- The tables cannot be used to convert from TARGINIQ ER to another opioid. Doing so will result in an overestimation of the dose of the new opioid and may result in a fatal overdose.
Convert patients from their previous opioid to TARGINIQ ER as follows:
- Using Table 1, calculate the Equivalent Daily Oral Morphine Dose by multiplying the current total daily dose of each opioid by the appropriate Conversion Factor.
- Using Table 2, determine the starting dose of TARGINIQ ER by reading across from the appropriate Equivalent Daily Dose of Oral Morphine range, rounding down, if necessary.
| Current Oral Opioid | Conversion Factor |
| Morphine | 1 |
| Codeine | 0.3 |
| Hydrocodone | 1.8 |
| Hydromorphone | 8 |
| Methadone† | 3 |
| Oxycodone | 2 |
| Oxymorphone | 4 |
| Tramadol* | - |
| Tapentadol | 0.3 |
| † See note on conversion of methadone
to TARGINIQ ER below * patients on tramadol should be initiated on the lowest available TARGINIQ ER dose, 10 mg/5 mg every 12 hours |
|
| Equivalent Daily Oral Morphine Dose | Recommended TARGINIQ ER Starting Dose |
| 20 to <70 mg | 10 mg/5 mg every 12 hours (ie. 20 mg oxycodone daily) |
| 70 to <110 mg | 20 mg/10 mg every 12 hours (ie. 40 mg oxycodone daily) |
| 110 to <150 mg | 30 mg/15 mg every 12 hours (ie. 60 mg oxycodone daily) |
| 150 to 160 mg | 40 mg/20 mg every 12 hours (ie. 80 mg oxycodone daily) |
Example conversion from a single opioid to TARGINIQ ER:
Step 2: Based on Table 2, the starting dose is TARGINIQ ER 10 mg/5 mg every 12 hours.
- For patients on a regimen of more than one opioid, use Table 1 to calculate the Equivalent Daily Oral Morphine dose for each opioid and sum the totals, then use Table 2 to obtain the starting dose of TARGINIQ ER.
- Round down, if necessary, to the appropriate TARGINIQ ER tablet strengths available.
- Monitor patients for signs and symptoms of opioid withdrawal or for signs of over-sedation/toxicity after converting patients to TARGINIQ ER.
- Titrate appropriately to a stable and tolerated dose.
2.7 Discontinuation of TARGINIQ ER
| * 30 mg/15 mg dose was achieved by administering a 20 mg/10 mg + a 10 mg/5 mg tablet | |||||||||||
| Patient’s Dose of TARGINIQ ER | Taper Dose (mg/mg) | ||||||||||
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | Day 8 | Day 9 | Day 10 | ||
| 10 mg/5 mg q12h | AM | 10/5 | 10/5 | - | - | - | - | - | - | - | - |
| PM | - | - | - | - | - | - | - | - | - | - | |
| 20 mg/10 mg q12h | AM | 20/10 | 20/10 | 10/5 | 10/5 | 10/5 | 10/5 | - | - | - | - |
| PM | 10/5 | 10/5 | 10/5 | 10/5 | - | - | - | - | - | - | |
| 30 mg/15 mg q12h* | AM | 20/10 | 20/10 | 20/10 | 20/10 | 10/5 | 10/5 | 10/5 | 10/5 | - | - |
| PM | 20/10 | 20/10 | 10/5 | 10/5 | 10/5 | 10/5 | - | - | - | - | |
| 40 mg/20 mg q12h | AM | 30/15 | 30/15 | 20/10 | 20/10 | 20/10 | 20/10 | 10/5 | 10/5 | 10/5 | 10/5 |
| PM | 30/15 | 30/15 | 20/10 | 20/10 | 10/5 | 10/5 | 10/5 | 10/5 | - | - | |
3. Dosage Forms and Strengths
Extended-release tablets: 10 mg/5 mg, 20 mg/10 mg, and 40 mg/20.
- 10 mg/5 mg film-coated extended-release tablets (capsule shaped, white film-coated tablets debossed with “ONX” on one side and “10” on the other)
- 20 mg/10 mg film-coated extended-release tablets (capsule shaped, pink film-coated tablets debossed with “ONX” on one side and “20” on the other)
- 40 mg/20 mg film-coated extended-release tablets (capsule shaped, yellow film-coated tablets debossed with “ONX” on one side and “40” on the other)
4. Contraindications
TARGINIQ ER is contraindicated in patients with:
- Significant respiratory depression [see Warnings and Precautions (5.2)]
- Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment [see Warnings and Precautions (5.6)]
- Known or suspected gastrointestinal obstruction, including paralytic ileus [see Warnings and Precautions (5.10)]
- Hypersensitivity (e.g., anaphylaxis) to oxycodone or naloxone [see Adverse Reactions (6.2)]
- Moderate to severe hepatic impairment [see Clinical Pharmacology (12.2)]
5. Warnings and Precautions
5.6 Risk of Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients
5.9 Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury or Impaired Consciousness
6. Adverse Reactions/Side Effects
The following serious adverse reactions are described elsewhere in the labeling:
- Addiction, Abuse, and Misuse [see Warnings and Precautions (5.1)]
- Life-Threatening Respiratory Depression [see Warnings and Precautions (5.2)]
- Neonatal Opioid Withdrawal Syndrome [see Warnings and Precautions (5.3)]
- Interactions with Benzodiazepine or Other CNS Depressants [see Warnings and Precautions (5.4)]
- Adrenal Insufficiency [see Warnings and Precautions (5.7)]
- Severe Hypotension [see Warnings and Precautions (5.8)]
- Gastrointestinal Adverse Reactions [see Warnings and Precautions (5.10)]
- Seizures [see Warnings and Precautions (5.11]
- Withdrawal [see Warnings and Precautions (5.12)]
6.1 Clinical Trial Experience
| *Percentages in the table are based on adverse reaction reports of Drug Withdrawal Syndrome in the key efficacy and safety study. In addition to the adverse reaction reports, an independent Adjudication Committee identified additional subjects with possible drug withdrawal syndrome, resulting in a total (adverse reactions plus adjudicated cases) of 2% of subjects in the Open-Label Period, and in the Double-Blind Period 4% of subjects treated with TARGINIQ ER and 2% treated with placebo. | |||||
| Open-Label Period | Double-Blind Period | ||||
| TARGINIQ
ER (N=1095) (%) | Placebo
(N=302) (%) | TARGINIQ
ER (N=298) (%) |
|||
| MedDRA System Organ Class | |||||
| Preferred Term | |||||
| Nausea | 7 | 5 | 8 | ||
| Headache | 4 | 3 | 3 | ||
| Constipation | 3 | 1 | 3 | ||
| Abdominal pain | 3 | 2 | 3 | ||
| Vomiting | 2 | 2 | 5 | ||
| Pruritus | 2 | 1 | 2 | ||
| Anxiety | 1 | 0 | 3 | ||
| *Drug withdrawal syndrome | 1 | 2 | 3 | ||
| Insomnia | 1 | 1 | 2 | ||
| Back pain | 0 | 1 | 3 | ||
6.2 Postmarketing Experience
Gastrointestinal Disorders: abdominal pain, constipation, diarrhea, nausea, and vomiting
Injury, Poisoning, and Procedural Complications: inadequate analgesia
Nervous System Disorders: dizziness, headache, tremor, and somnolence
Psychiatric Disorders: restlessness, confusional state, and anxiety
Respiratory, Thoracic, and Mediastinal Disorders: dyspnea
Skin and Subcutaneous Tissue Disorders: hyperhidrosis and pruritus
Anaphylaxis: Anaphylaxis has been reported with ingredients contained in TARGINIQ ER.
7. Drug Interactions
Table 5 includes clinically significant drug interactions with TARGINIQ ER
| Inhibitors of CYP3A4 and CYP2D6 | |
| Clinical Impact: | The concomitant use of TARGINIQ
ER and CYP3A4 inhibitors can increase the plasma concentration of
oxycodone, resulting in increased or prolonged opioid effects. These
effects could be more pronounced with concomitant use of TARGINIQ
ER and CYP2D6 and CYP3A4 inhibitors, particularly when an inhibitor
is added after a stable dose of TARGINIQ ER is achieved [see
Warnings and Precautions (5.4)]. After stopping a CYP3A4 inhibitor, as the effects of the inhibitor decline, the oxycodone plasma concentration will decrease [see Clinical Pharmacology (12.3)], resulting in decreased opioid efficacy or a withdrawal syndrome in patients who had developed physical dependence to oxycodone. |
| Intervention: | If concomitant use is necessary,
consider dosage reduction of TARGINIQ ER until stable drug effects
are achieved. Monitor patients for respiratory depression and sedation
at frequent intervals. If a CYP3A4 inhibitor is discontinued, consider increasing the TARGINIQ ER dosage until stable drug effects are achieved. Monitor for signs of opioid withdrawal. |
| Examples: | Macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g. ketoconazole), protease inhibitors (e.g., ritonavir) |
| CYP3A4 Inducers | |
| Clinical Impact: | The concomitant use of TARGINIQ
ER and CYP3A4 inducers can decrease the plasma concentration of oxycodone [see Clinical Pharmacology (12.3)], resulting in decreased efficacy or onset of a withdrawal
syndrome in patients who have developed physical dependence to oxycodone [see Warnings and Precautions (5.4)]. After stopping a CYP3A4 inducer, as the effects of the inducer decline, the oxycodone plasma concentration will increase [see Clinical Pharmacology (12.3)], which could increase or prolong both the therapeutic effects and adverse reactions, and may cause serious respiratory depression. |
| Intervention: | If concomitant use is necessary, consider increasing the TARGINIQ ER dosage until stable drug effects are achieved. Monitor for signs of opioid withdrawal. If a CYP3A4 inducer is discontinued, consider TARGINIQ ER dosage reduction and monitor for signs of respiratory depression. |
| Examples: | Rifampin, carbamazepine, phenytoin |
| Benzodiazepines and Other Central Nervous System (CNS) Depressants | |
| Clinical Impact: | Due to additive pharmacologic effect, the concomitant use of benzodiazepines or other CNS depressants, including alcohol, can increase the risk of hypotension, respiratory depression, profound sedation, coma, and death. |
| Intervention: | Reserve concomitant prescribing of these drugs for use in patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients closely for signs of respiratory depression and sedation [see Dosage and Administration (2.4), Warnings and Precautions(5.4)]. |
| Examples: | Benzodiazepines and other sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, , antipsychotics, other opioids, alcohol. |
| Serotonergic Drugs | |
| Clinical Impact: | The concomitant use of opioids with other drugs that affect the serotonergic neurotransmitter system has resulted in serotonin syndrome. |
| Intervention: | If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation and dose adjustment. Discontinue TARGINIQ ER if serotonin syndrome is suspected. |
| Examples: | Selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5-HT3 receptor antagonists, drugs that affect the serotonin neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), monoamine oxidase (MAO) inhibitors (those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue). |
| Monoamine Oxidase Inhibitors (MAOIs) | |
| Clinical Impact: | MAOI interactions with opioids may manifest as serotonin syndrome or opioid toxicity (e.g., respiratory depression, coma) [see Warnings and Precautions (5.2)]. |
| Intervention: | The use of TARGINIQ ER is not recommended for patients taking MAOIs or within 14 days of stopping such treatment. |
| Examples: | phenelzine, tranylcypromine, linezolid |
| Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics | |
| Clinical Impact: | May reduce the analgesic effect of TARGINIQ ER and/or precipitate withdrawal symptoms. |
| Intervention: | Avoid concomitant use. |
| Examples: | butorphanol, nalbuphine, pentazocine, buprenorphine |
| Muscle Relaxants | |
| Clinical Impact: | Oxycodone may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression. |
| Intervention: | Monitor patients for signs of respiratory depression that may be greater than otherwise expected and decrease the dosage of TARGINIQ ER and/or the muscle relaxant as necessary. |
| Diuretics | |
| Clinical Impact: | Opioids can reduce the efficacy of diuretics by inducing the release of antidiuretic hormone. |
| Intervention: | Monitor patients for signs of diminished diuresis and/or effects on blood pressure and increase the dosage of the diuretic as needed. |
| Anticholinergic Drugs | |
| Clinical Impact: | The concomitant use of anticholinergic drugs may increase risk of urinary retention and/or severe constipation, which may lead to paralytic ileus. |
| Intervention: | Monitor patients for signs of urinary retention or reduced gastric motility when TARGINIQ ER is used concomitantly with anticholinergic drugs. |
8. Use In Specific Populations
9. Drug Abuse and Dependence
9.2 Abuse
Clinical Abuse Potential Studies
Study in Non-Dependent, Opioid Abusers (Intranasal (IN) Administration)
| VAS: visual analog scale | ||||
| SE: standard error | ||||
| * Drug Liking Question text: “At this moment, my liking for this drug is”; scale: 0 = maximum disliking, 50 = neither liking nor disliking (neutral response), 100 = maximum liking. | ||||
| **Take Drug Again Question text: “I would take this drug again”; scale: 0 = definitely not, 100 = definitely so. | ||||
| VAS | TARGINIQ ER 40 mg/20 mg (finely crushed) | Oxycodone HCl 40 mg (powdered) | Placebo (lactose powder) |
|
| Drug Liking* | Mean (SE) | 59.1 (2.8) | 94.8 (2.2) | 53.2 (2.1) |
| Median (Range) | 51 (50-100) | 100 (61-100) | 51 (50-100) | |
| Take Drug Again** | Mean (SE) | 42.6 (6.4) | 93.6 (2.3) | 30.7 (6.1) |
| Median (Range) | 50.0 (0-100) | 100 (62-100) | 50 (0-100) | |
| VAS: visual analog scale | ||||
| SE: standard error | ||||
| * Drug Liking Question text: “At this moment, my liking for this drug is”; scale: 0 = maximum disliking, 50 = neither liking nor disliking (neutral response), 100 = maximum liking. | ||||
| **Take Drug Again Question text: “I would take this drug again”; scale: 0 = definitely not, 100 = definitely so; Values obtained at 8 hours post dose. | ||||
| VAS | Oxycodone HCl/ Naloxone HCl 0.07/0.35 mg/kg | Oxycodone HCl 0.07 mg/kg | Placebo saline (0.9% NaCl) |
|
| Drug Liking* | Mean (SE) | 56.5 (2.8) | 96.4 (2.3) | 48.7 (2.3) |
| Median (Range) | 51 (50-100) | 100 (50-100) | 51.0 (0-53) | |
| Take Drug Again** | Mean (SE) | 37.0 (6.2) | 82.0 (6.0) | 34.5 (5.1)) |
| Median (Range) | 50.0 (0-100) | 99.0 (0-100) | 50.0 (0-55) | |
| VAS: visual analog scale | |||||
| SE: standard error | |||||
| * Drug Liking Question text: “At this moment, my liking for this drug is”; scale: 0 = maximum disliking, 50 = neither liking nor disliking (neutral response), 100 = maximum liking. | |||||
| **Take Drug Again Question text: “I would take this drug again”; scale: 0 = definitely not, 100 = definitely so; Values obtained at 12 hours post dose. | |||||
| ***Getting High Question Text: “I am feeling high”; scale: 0 = definitely not, 100 = definitely so. | |||||
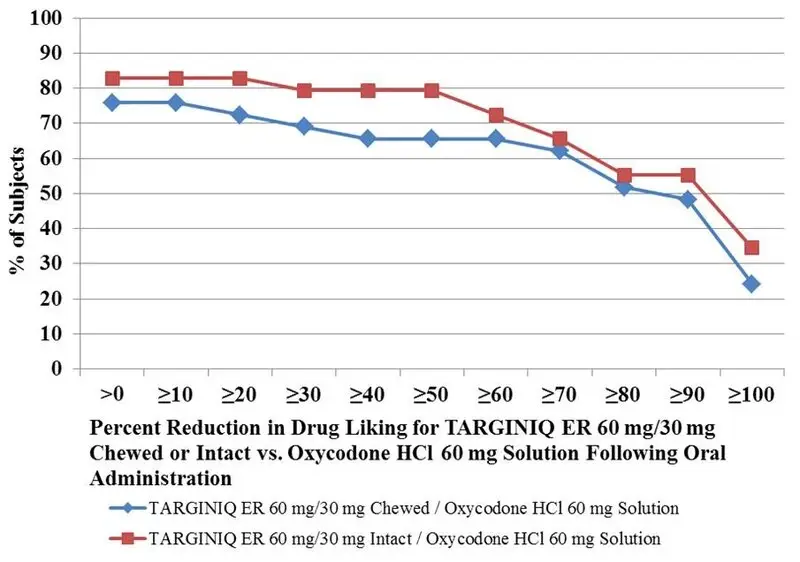
| VAS | TARGINIQ ER 60 mg/30 mg intact | TARGINIQ ER 60 mg/30 mg chewed | Oxycodone HCl solution 60 mg | Placebo chewed and intact tablet, solution |
|
| Drug Liking* | Mean (SE) | 54.7 (2.0) | 54.6 (3.2) | 77.9 (3.8) | 54.4 (2.1) |
| Median (Range) | 51.0 (50-99) | 51.0 (0-100) | 78.0 (50-100) | 51.0 (50-100) | |
| Take Drug Again** | Mean (SE) | 38.5 (5.7) | 32.6 (5.9) | 61.4 (5.9) | 41.5 (5.0) |
| Median (Range) | 50.0 (0-100) | 50.0 (0-100) | 50.0 (0-100) | 50.0 (0-100) | |
| Getting High*** | Mean (SE) | 20.6 (5.1) | 27.7 (6.5) | 77.9 (5.0) | 20.6 (5.0) |
| Median (Range) | 1.0 (0-73) | 1.0 (0-100) | 86.0 (0-100) | 1.0 (0-82) | |
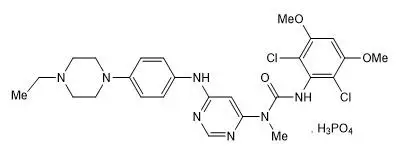
11. Targiniq ER Description
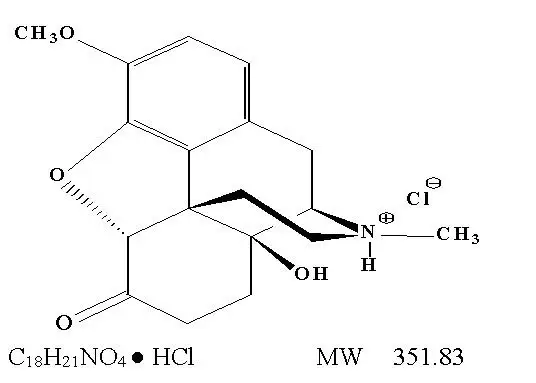
The chemical name is 4, 5α-epoxy-14-hydroxy-3-methoxy-17-methylmorphinan-6-one hydrochloride.
The structural formula for naloxone hydrochloride is as follows:
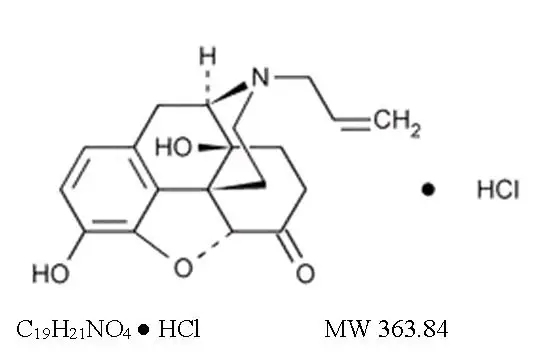
The chemical name is (-)-17-Allyl-4,5α -epoxy-3,14-dihydroxy-morphinan-6-one hydrochloride.
12. Targiniq ER - Clinical Pharmacology
12.2 Pharmacodynamics
Effects on the Central Nervous System
Effects on the Gastrointestinal Tract and Other Smooth Muscle
Effects on the Cardiovascular System
Effects on the Endocrine System
Concentration –Efficacy Relationships
12.3 Pharmacokinetics
| † for single-dose, AUC = AUC0-inf; for multiple-dose, AUC = AUCtau | |||||
| †† median (range) | |||||
| Data obtained from healthy subjects receiving naltrexone. | |||||
| Regimen | TARGINIQ ER Dose (mg/mg) | AUC (ng•hr/mL)† | Cmax
(ng/mL) | Tmax
(hour) †† | Trough Conc. (ng/mL) |
| Single Dose | 10/5 | 130 [25.6] | 12.1 [2.67] | 3 [1, 6] | NA |
| 20/10 | 247 [62.7] | 22.2 [4.19] | 3 [1, 6] | NA | |
| 40/20 | 506 [128] | 40.9 [9.52] | 3.5 [1, 6] | NA | |
| Multiple Dose | 10/5 q12h | 129 [33.4] | 15.0 [3.25] | 1.75 [1, 5] | 5.69 [1.78] |
| 40/20 q12h | 507 [100] | 57.0 [10.0] | 2 [0.5, 5] | 24.7 [5.68] | |
| † for single-dose, AUC = AUC0-inf; for multiple-dose, AUC = AUCtau | |||||
| †† median (range) | |||||
| Data obtained from healthy subjects receiving naltrexone. | |||||
| Regimen | TARGINIQ ER Dose (mg/mg) | AUC (ng•hr/mL)† | Cmax
(ng/mL) | Tmax
(hour) †† | Trough Conc. (ng/mL) |
| Single Dose | 10/5 | 0.136 [0.141] | 0.0306 [0.0236] | 5 [1, 12] | NA |
| 20/10 | 0.657 [0.585] | 0.0839 [0.0812] | 1.5 [0.5, 12] | NA | |
| 40/20 | 0.833 [0.526] | 0.0845 [0.0834] | 2 [1, 16] | NA | |
| Multiple Dose | 10/5 q12h | 0.416 [0.367] | 0.0725 [0.0885] | 3.75 [0.5, 8] | 0.0154 [0.00882] |
| 40/20 q12h | 1.55 [1.02] | 0.217 [0.173] | 5 [0.5, 12] | 0.0711 [0.0410] | |
Pharmacokinetic properties of TARGINIQ ER were not affected by sex.
13. Nonclinical Toxicology
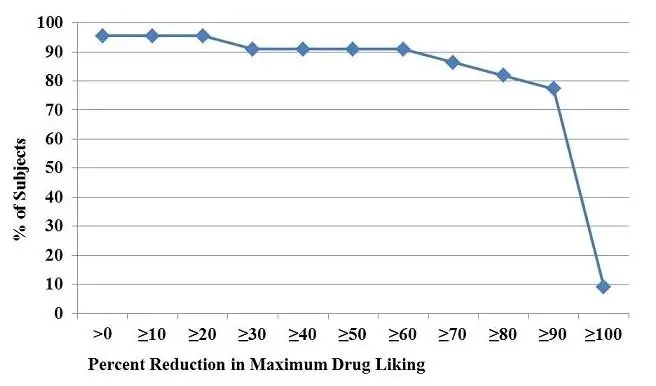
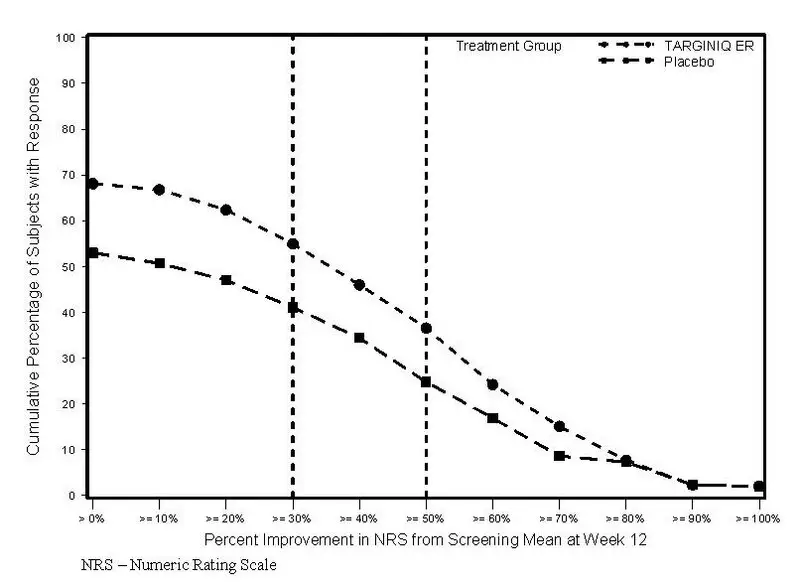
14. Clinical Studies
Figure 4. Plot of Distribution of Responders Based on Pain Intensity at Week 12
16. How is Targiniq ER supplied
Dispense in tight, light-resistant container, with a child-resistant closing.
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Life-Threatening Respiratory Depression
Interaction with Benzodiazepines and Other CNS Depressants
Important Administration Instructions
Instruct patients how to properly take TARGINIQ ER, including the following:
- TARGINIQ ER is designed to work properly only if swallowed intact. Taking cut, broken, chewed, crushed, or dissolved TARGINIQ ER tablets can result in a fatal overdose or other serious side effects (e.g., withdrawal symptoms) [see Dosage and Administration (2.1)].
- Do not discontinue TARGINIQ ER without first discussing the need for a tapering regimen with the prescriber [see Dosage and Administration (2.7)].
Driving or Operating Heavy Machinery
Disposal of Unused TARGINIQ ER
Advise patients to flush the unused tablets down the toilet when TARGINIQ ER is no longer needed.
| Medication
Guide TARGINIQ™ ER (tar-gih-NEEK E-R) (oxycodone hydrochloride and naloxone hydrochloride extended-release tablets), CII |
|
TARGINIQ ER
is:
|
|
Important
information about TARGINIQ ER:
|
|
Do not take
TARGINIQ ER if you have:
|
|
| Before taking TARGINIQ ER, tell your healthcare provider if you have a history of: | |
|
|
Tell your healthcare
provider if you are:
|
|
When taking
TARGINIQ ER:
|
|
While taking
TARGINIQ ER DO NOT:
|
|
The possible
side effects of TARGINIQ ER are:
These are not all the possible side effects of TARGINIQ ER. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. For more information go to dailymed.nlm.nih.gov. Manufactured by: Purdue Pharma L.P., Stamford, CT 06901-3431, www.purduepharma.com or call 1-888-726-7535 |
|
This Medication Guide
has been approved by the U.S. Food and Drug Administration.
Issue: 12/2016
| TARGINIQ
ER
oxycodone hydrochloride/naloxone hydrochloride tablet, film coated, extended release |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| TARGINIQ
ER
oxycodone hydrochloride/naloxone hydrochloride tablet, film coated, extended release |
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
| TARGINIQ
ER
oxycodone hydrochloride/naloxone hydrochloride tablet, film coated, extended release |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| Labeler - Purdue Pharma LP (932323652) |
| Registrant - Purdue Pharma LP (932323652) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Purdue Pharmaceuticals L.P. | 132080875 | MANUFACTURE(59011-521, 59011-522, 59011-520) | |