Drug Detail:Temodar (Temozolomide)
Drug Class: Alkylating agents
Highlights of Prescribing Information
TEMODAR® (temozolomide) capsules, for oral use
TEMODAR® (temozolomide) for injection, for intravenous use
Initial U.S. Approval: 1999
Indications and Usage for Temodar
TEMODAR is an alkylating drug indicated for the treatment of adult patients with:
- Newly diagnosed glioblastoma concomitantly with radiotherapy and then as maintenance treatment. (1.1)
- Refractory anaplastic astrocytoma who have experienced disease progression on a drug regimen containing nitrosourea and procarbazine. (1.2)
Temodar Dosage and Administration
- Administer either orally or intravenously.
-
Newly Diagnosed Glioblastoma:
- 75 mg/m2 once daily for 42 days concomitant with focal radiotherapy followed by initial maintenance dose of 150 mg/m2 once daily for Days 1 to 5 of each 28-day cycle for 6 cycles. May increase maintenance dose to 200 mg/m2 for cycles 2 to 6 based on toxicity. (2.1)
- Provide Pneumocystis pneumonia (PCP) prophylaxis during concomitant phase and continue in patients who develop lymphopenia until resolution to Grade 1 or less. (2.1)
- Refractory Anaplastic Astrocytoma: Initial dose of 150 mg/m2 once daily on Days 1 to 5 of each 28-day cycle. (2.2)
Dosage Forms and Strengths
- Capsules: 5 mg, 20 mg, 100 mg, 140 mg, 180 mg, and 250 mg. (3)
- For injection: 100 mg as a lyophilized powder in single-dose vial for reconstitution. (3)
Contraindications
- History of hypersensitivity to temozolomide or any other ingredients in TEMODAR and dacarbazine.
Warnings and Precautions
- Myelosuppression: Monitor absolute neutrophil count (ANC) and platelet count prior to each cycle and during treatment. Geriatric patients and women have a higher risk of developing myelosuppression. (5.1)
- Myelodysplastic Syndrome and Secondary Malignancies, including myeloid leukemia, have been observed. (5.2)
- Pneumocystis Pneumonia (PCP): Closely monitor all patients, particularly those receiving steroids, for the development of lymphopenia and PCP. (5.3)
- Hepatotoxicity: Fatal and severe hepatotoxicity have been reported. Perform liver tests at baseline, midway through the first cycle, prior to each subsequent cycle, and approximately 2 to 4 weeks after the last dose of TEMODAR. (5.4)
- Embryo-Fetal Toxicity: Can cause fetal harm. Advise females of reproductive potential of the potential risk to a fetus and to use effective contraception. Advise male patients with pregnant partners or female partners of reproductive potential to use condoms. (5.5, 8.1, 8.3)
Adverse Reactions/Side Effects
- The most common adverse reactions (≥20% incidence) are: alopecia, fatigue, nausea, vomiting, headache, constipation, anorexia, and convulsions. (6.1)
- The most common Grade 3 to 4 hematologic laboratory abnormalities (≥10% incidence) in patients with anaplastic astrocytoma are: decreased lymphocytes, decreased platelets, decreased neutrophils, and decreased leukocytes. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Merck Sharp & Dohme LLC at 1-877-888-4231 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch .
Use In Specific Populations
- Lactation: Advise not to breastfeed. (8.2)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 11/2022
Related/similar drugs
Avastin, bevacizumab, temozolomide, Mvasi, procarbazine, Zirabev, MatulaneFull Prescribing Information
1. Indications and Usage for Temodar
2. Temodar Dosage and Administration
2.1 Recommended Dosage and Dosage Modifications for Newly Diagnosed Glioblastoma
Administer TEMODAR either orally or intravenously once daily for 42 consecutive days during the concomitant phase with focal radiotherapy and then once daily on Days 1 to 5 of each 28-day cycle for 6 cycles during the maintenance phase.
Provide Pneumocystis pneumonia (PCP) prophylaxis during the concomitant phase and continue in patients who develop lymphocytopenia until resolution to Grade 1 or less [see Warnings and Precautions (5.3)].
Concomitant Phase
The recommended dosage of TEMODAR is 75 mg/m2 either orally or intravenously once daily for 42 days (up to 49 days) concomitant with focal radiotherapy (60 Gy administered in 30 fractions). Focal radiotherapy includes the tumor bed or resection site with a 2- to 3-cm margin.
Obtain a complete blood count weekly. No dose reductions are recommended during the concomitant phase. The recommended dosage modifications during the concomitant phase are provided in Table 1.
| Adverse Reaction | Interruption | Discontinuation |
|---|---|---|
| Absolute Neutrophil Count | Withhold TEMODAR if ANC is greater than or equal to 0.5 × 109/L and less than 1.5 × 109/L. | Discontinue TEMODAR if platelet count is less than 0.5 × 109/L. |
| Resume TEMODAR when ANC is greater than or equal to 1.5 × 109/L. | ||
| Platelet Count | Withhold TEMODAR if platelet count is greater than or equal to 10 × 109/L and less than 100 × 109/L. | Discontinue TEMODAR if platelet count is less than 10 × 109/L. |
| Resume TEMODAR when platelet count is greater than or equal to 100 × 109/L. | ||
| Non-hematological Adverse Reaction (except for alopecia, nausea, vomiting) | Withhold TEMODAR if Grade 2 adverse reaction occurs. | Discontinue TEMODAR if Grade 3 or 4 adverse reaction occurs. |
| Resume TEMODAR when resolution to Grade 1 or less. |
Maintenance Phase:
Beginning 4 weeks after Concomitant Phase completion, administer TEMODAR either orally or intravenously once daily on Days 1 to 5 of each 28-day cycle for 6 cycles. The recommended dosage of TEMODAR is as follows:
- Cycle 1: 150 mg/m2 per day
- Cycles 2 to 6: May increase to 200 mg/m2 per day if the following conditions are met before starting cycle 2. If the dose was not escalated at the onset of Cycle 2, do not increase the dose for Cycles 3 to 6.
- Nonhematologic toxicity is Grade 2 or less (except for alopecia, nausea, and vomiting)
- ANC is greater than or equal to 1.5 × 109/L, and
- Platelet count is greater than or equal to 100 × 109/L.
Obtain a complete blood count on Day 22 and then weekly until the ANC is above 1.5 × 109/L and the platelet count is above 100 × 109/L. Do not start the next cycle until the ANC and platelet count exceed these levels.
The recommended dosage modifications during the maintenance phase are provided in Table 2. If TEMODAR is withheld, reduce the dose for the next cycle by 50 mg/m2 per day. Permanently discontinue TEMODAR in patients who are unable to tolerate a dose of 100 mg/m2 per day.
| Toxicity | Interruption and Dose Reduction | Discontinuation |
|---|---|---|
| Absolute Neutrophil Count | Withhold TEMODAR if ANC less than 1 × 109/L. | Unable to tolerate a dose of 100 mg/m2 per day. |
| When ANC is above 1.5 × 109/L, resume TEMODAR at reduced dose for the next cycle. | ||
| Platelet Count | Withhold TEMODAR if platelet less than 50 × 109/L. | Unable to tolerate a dose of 100 mg/m2 per day. |
| When platelet count is above 100 × 109/L, resume TEMODAR at reduced dose for the next cycle. | ||
| Nonhematological Adverse Reaction (except for alopecia, nausea, vomiting) | Withhold TEMODAR if Grade 3 adverse reaction. | Recurrent Grade 3 after dose reduction. |
| When resolved to Grade 1 or less, resume TEMODAR at reduced dose for the next cycle. | Grade 4 Unable to tolerate a dose of 100 mg/m2 per day. |
2.2 Recommended Dosage and Dosage Modifications for Refractory Anaplastic Astrocytoma
The recommended initial dosage of TEMODAR is 150 mg/m2 once daily on Days 1 to 5 of each 28-day cycle. Increase the TEMODAR dose to 200 mg/m2 per day if the following conditions are met at the nadir and on Day 1 of the next cycle:
- ANC is greater than or equal to 1.5 × 109/L, and
- Platelet count is greater than or equal to 100 × 109/L.
Continue TEMODAR until disease progression or unacceptable toxicity. In the clinical trial, treatment could be continued for a maximum of 2 years, but the optimum duration of therapy is not known.
Obtain a complete blood count on Day 22 and then weekly until the ANC is above 1.5 × 109/L and the platelet count is above 100 × 109/L. Do not start the next cycle until the ANC and platelet count exceed these levels.
If the ANC is less than 1 × 109/L or the platelet count is less than 50 × 109/L during any cycle, reduce the TEMODAR dose for the next cycle by 50 mg/m2 per day. Permanently discontinue TEMODAR in patients who are unable to tolerate a dose of 100 mg/m2 per day.
3. Dosage Forms and Strengths
- Capsules:
- –
- 5 mg: opaque white bodies with green caps. The capsule body is imprinted with two stripes, the dosage strength, and the Schering-Plough logo. The cap is imprinted with "TEMODAR."
- –
- 20 mg: opaque white bodies with yellow caps. The capsule body is imprinted with two stripes, the dosage strength, and the Schering-Plough logo. The cap is imprinted with "TEMODAR."
- –
- 100 mg: opaque white bodies with pink caps. The capsule body is imprinted with two stripes, the dosage strength, and the Schering-Plough logo. The cap is imprinted with "TEMODAR."
- –
- 140 mg: opaque white bodies with blue caps. The capsule body is imprinted with two stripes, the dosage strength, and the Schering-Plough logo. The cap is imprinted with "TEMODAR."
- –
- 180 mg: opaque white bodies with orange caps. The capsule body is imprinted with two stripes, the dosage strength, and the Schering-Plough logo. The cap is imprinted with "TEMODAR."
- –
- 250 mg: opaque white bodies with white caps. The capsule body is imprinted with two stripes, the dosage strength, and the Schering-Plough logo. The cap is imprinted with "TEMODAR."
- For injection: 100 mg white to light tan/light pink lyophilized powder for reconstitution in a single-dose vial.
4. Contraindications
TEMODAR is contraindicated in patients with a history of hypersensitivity reactions to:
- temozolomide or any other ingredients in TEMODAR; and
- dacarbazine, since both temozolomide and dacarbazine are metabolized to the same active metabolite 5-(3-methyltriazen-1-yl)-imidazole-4-carboxamide.
Reactions to TEMODAR have included anaphylaxis [see Adverse Reactions (6.2)].
5. Warnings and Precautions
5.1 Myelosuppression
Myelosuppression, including pancytopenia, leukopenia and anemia, some with fatal outcomes, have occurred with TEMODAR [see Adverse Reactions (6.1, 6.2)]. Geriatric patients and women have been shown in clinical trials to have a higher risk of developing myelosuppression.
Prior to dosing, patients must have an ANC of 1.5 × 109/L or greater and a platelet count of 100 × 109/L or greater.
For the concomitant phase with radiotherapy, obtain a complete blood count prior to initiation of treatment and weekly during treatment [see Dosage and Administration (2.1)].
For the 28-day treatment cycles, obtain a complete blood count prior to treatment on Day 1 and on Day 22 of each cycle. Perform complete blood counts weekly until recovery if the ANC falls below 1.5 × 109/L and the platelet count falls below 100 × 109/L [see Dosage and Administration (2.1, 2.2)].
5.2 Myelodysplastic Syndrome and Secondary Malignancies
Cases of myelodysplastic syndrome and secondary malignancies, including myeloid leukemia, have been observed following TEMODAR administration.
5.3 Pneumocystis Pneumonia
Pneumocystis pneumonia (PCP) can occur in patients receiving TEMODAR. The risk of PCP is increased in patients receiving steroids or with longer treatment regimens.
For patients with newly diagnosed glioblastoma, provide PCP prophylaxis for all patients during the concomitant phase. Continue in patients who experience lymphopenia until resolution to Grade 1 or less [see Dosage and Administration (2.1)].
Monitor all patients receiving TEMODAR for the development of lymphopenia and PCP.
5.4 Hepatotoxicity
Fatal and severe hepatotoxicity have been reported in patients receiving TEMODAR. Perform liver tests at baseline, midway through the first cycle, prior to each subsequent cycle, and approximately two to four weeks after the last dose of TEMODAR.
5.5 Embryo-Fetal Toxicity
Based on findings from animal studies and its mechanism of action, TEMODAR can cause fetal harm when administered to a pregnant woman. Adverse developmental outcomes have been reported in both pregnant patients and pregnant partners of male patients. Oral administration of temozolomide to rats and rabbits during the period of organogenesis resulted in embryolethality and polymalformations at doses less than the maximum human dose based on body surface area.
Advise pregnant women of the potential risk to the fetus. Advise females of reproductive potential to use effective contraception during treatment with TEMODAR and for at least 6 months after the final dose. Because of potential risk of genotoxic effects on sperm, advise male patients with female partners of reproductive potential to use condoms during treatment with TEMODAR and for at least 3 months after the final dose. Advise male patients not to donate semen during treatment with TEMODAR and for at least 3 months after the final dose [see Use in Specific Populations (8.1, 8.3)].
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Myelosuppression [see Warnings and Precautions (5.1)].
- Myelodysplastic Syndrome and Secondary Malignancies [see Warnings and Precautions (5.2)].
- Pneumocystis Pneumonia [see Warnings and Precautions (5.3)].
- Hepatotoxicity [see Warnings and Precautions (5.4)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Newly Diagnosed Glioblastoma
The safety of TEMODAR was evaluated in Study MK-7365-051 [see Clinical Studies (14.1)].
Forty-nine percent (49%) of patients treated with TEMODAR reported one or more severe or life-threatening reactions, most commonly fatigue (13%), convulsions (6%), headache (5%), and thrombocytopenia (5%).
The most common adverse reactions (≥20%) across the cumulative TEMODAR experience were alopecia, fatigue, nausea, and vomiting. Table 3 summarizes the adverse reactions in Newly Diagnosed Glioblastoma Trial. Overall, the pattern of reactions during the maintenance phase was consistent with the known safety profile of TEMODAR.
| Adverse Reactions | Concomitant Phase | Maintenance Phase | ||||
|---|---|---|---|---|---|---|
| Radiation Therapy and TEMODAR N=288* | Radiation Therapy Alone N=285 | TEMODAR N=224 |
||||
| All Grades (%) | Grade ≥3 (%) | All Grades (%) | Grades ≥3 (%) | All Grades (%) | Grade ≥3 (%) |
|
| NOS = not otherwise specified. Note: Grade 5 (fatal) adverse reactions are included in the Grade ≥3 column. |
||||||
|
||||||
| Skin and Subcutaneous Tissue | ||||||
| Alopecia | 69 | 63 | 55 | |||
| Rash | 19 | 1 | 15 | 13 | 1 | |
| Dry Skin | 2 | 2 | 5 | <1 | ||
| Pruritus | 4 | 1 | 5 | |||
| Erythema | 5 | 5 | 1 | |||
| General | ||||||
| Fatigue | 54 | 7 | 49 | 5 | 61 | 9 |
| Anorexia | 19 | 1 | 9 | <1 | 27 | 1 |
| Headache | 19 | 2 | 17 | 4 | 23 | 4 |
| Weakness | 3 | 2 | 3 | 1 | 7 | 2 |
| Dizziness | 4 | 1 | 4 | 5 | ||
| Gastrointestinal System | ||||||
| Nausea | 36 | 1 | 16 | <1 | 49 | 1 |
| Vomiting | 20 | <1 | 6 | <1 | 29 | 2 |
| Constipation | 18 | 1 | 6 | 22 | ||
| Diarrhea | 6 | 3 | 10 | 1 | ||
| Stomatitis | 7 | 5 | <1 | 9 | 1 | |
| Abdominal Pain | 2 | <1 | 1 | 5 | <1 | |
| Eye | ||||||
| Vision Blurred | 9 | 1 | 9 | 1 | 8 | |
| Injury | ||||||
| Radiation Injury NOS | 7 | 4 | <1 | 2 | ||
| Central and Peripheral Nervous System | ||||||
| Convulsions | 6 | 3 | 7 | 3 | 11 | 3 |
| Memory Impairment | 3 | <1 | 4 | <1 | 7 | 1 |
| Confusion | 4 | 1 | 4 | 2 | 5 | 2 |
| Special Senses Other | ||||||
| Taste Perversion | 6 | 2 | 5 | |||
| Respiratory System | ||||||
| Coughing | 5 | 1 | 1 | 8 | <1 | |
| Dyspnea | 4 | 2 | 3 | 1 | 5 | <1 |
| Psychiatric | ||||||
| Insomnia | 5 | 3 | <1 | 4 | ||
| Immune System | ||||||
| Allergic Reaction | 5 | 2 | <1 | 3 | ||
| Platelet, Bleeding and Clotting | ||||||
| Thrombocytopenia | 4 | 3 | 1 | 8 | 4 | |
| Musculoskeletal System | ||||||
| Arthralgia | 2 | <1 | 1 | 6 | ||
When laboratory abnormalities and adverse reactions were combined, Grade 3 or Grade 4 neutrophil abnormalities including neutropenic reactions were observed in 8% of patients, and Grade 3 or Grade 4 platelet abnormalities including thrombocytopenic reactions were observed in 14% of patients.
Refractory Anaplastic Astrocytoma
The safety of TEMODAR was evaluated in Study MK-7365-006 [see Clinical Studies (14.2)].
Myelosuppression (thrombocytopenia and neutropenia) was the dose-limiting adverse reaction. It usually occurred within the first few cycles of therapy and was not cumulative. Myelosuppression occurred late in the treatment cycle and returned to normal, on average, within 14 days of nadir counts. The median nadirs occurred at 26 days for platelets (range: 21 to 40 days) and 28 days for neutrophils (range: 1 to 44 days). Only 14% (22/158) of patients had a neutrophil nadir and 20% (32/158) of patients had a platelet nadir, which may have delayed the start of the next cycle. Less than 10% of patients required hospitalization, blood transfusion, or discontinuation of therapy due to myelosuppression.
The most common adverse reactions (≥20%) were nausea, vomiting, headache, fatigue, constipation, and convulsions.
Tables 4 and 5 summarize the adverse reactions and hematological laboratory abnormalities in Refractory Anaplastic Astrocytoma Trial.
| Adverse Reactions | TEMODAR N=158 |
|
|---|---|---|
| All Reactions (%) | Grades 3-4 (%) |
|
|
||
| Gastrointestinal System | ||
| Nausea | 53 | 10 |
| Vomiting | 42 | 6 |
| Constipation | 33 | 1 |
| Diarrhea | 16 | 2 |
| Abdominal pain | 9 | 1 |
| Anorexia | 9 | 1 |
| General | ||
| Headache | 41 | 6 |
| Fatigue | 34 | 4 |
| Asthenia | 13 | 6 |
| Fever | 13 | 2 |
| Back pain | 8 | 3 |
| Central and Peripheral Nervous System | ||
| Convulsions | 23 | 5 |
| Hemiparesis | 18 | 6 |
| Dizziness | 12 | 1 |
| Coordination abnormal | 11 | 1 |
| Amnesia | 10 | 4 |
| Insomnia | 10 | |
| Paresthesia | 9 | 1 |
| Somnolence | 9 | 3 |
| Paresis | 8 | 3 |
| Urinary incontinence | 8 | 2 |
| Ataxia | 8 | 2 |
| Dysphasia | 7 | 1 |
| Convulsions local | 6 | |
| Gait abnormal | 6 | 1 |
| Confusion | 5 | |
| Cardiovascular | ||
| Edema peripheral | 11 | 1 |
| Resistance Mechanism | ||
| Infection viral | 11 | |
| Endocrine | ||
| Adrenal hypercorticism | 8 | |
| Respiratory System | ||
| Upper respiratory tract infection | 8 | |
| Pharyngitis | 8 | |
| Sinusitis | 6 | |
| Coughing | 5 | |
| Skin and Appendages | ||
| Rash | 8 | |
| Pruritus | 8 | 1 |
| Urinary System | ||
| Urinary tract infection | 8 | |
| Micturition increased frequency | 6 | |
| Psychiatric | ||
| Anxiety | 7 | 1 |
| Depression | 6 | |
| Reproductive Disorders | ||
| Breast pain, female | 6 | |
| Metabolic | ||
| Weight increase | 5 | |
| Musculoskeletal System | ||
| Myalgia | 5 | |
| Vision | ||
| Diplopia | 5 | |
| Vision abnormal* | 5 | |
| TEMODAR*,† | |
|---|---|
|
|
| Decreased lymphocytes | 55% |
| Decreased platelets | 19% |
| Decreased neutrophils | 14% |
| Decreased leukocytes | 11% |
| Decreased hemoglobin | 4% |
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of TEMODAR. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to the drug exposure.
Dermatologic: Toxic epidermal necrolysis and Stevens-Johnson syndrome
Immune System: Hypersensitivity reactions, including anaphylaxis. Erythema multiforme, which resolved after discontinuation of TEMODAR and, in some cases, recurred upon rechallenge.
Hematopoietic: Prolonged pancytopenia, which may result in aplastic anemia and fatal outcomes.
Hepatobiliary: Fatal and severe hepatotoxicity, elevation of liver enzymes, hyperbilirubinemia, cholestasis, and hepatitis.
Infections: Serious opportunistic infections, including some cases with fatal outcomes, with bacterial, viral (primary and reactivated), fungal, and protozoan organisms.
Pulmonary: Interstitial pneumonitis, pneumonitis, alveolitis, and pulmonary fibrosis.
Endocrine: Diabetes insipidus
8. Use In Specific Populations
8.2 Lactation
There are no data on the presence of TEMODAR or its metabolites in human milk, the effects on a breastfed child, or the effects on milk production. Because of the potential for serious adverse reactions, including myelosuppression from temozolomide in the breastfed children, advise women not to breastfeed during treatment with TEMODAR and for at least 1 week after the final dose.
8.4 Pediatric Use
Safety and effectiveness of TEMODAR have not been established in pediatric patients. Safety and effectiveness of TEMODAR capsules were assessed, but not established, in 2 open-label studies in pediatric patients aged 3 to 18 years. In one study, 29 patients with recurrent brain stem glioma and 34 patients with recurrent high-grade astrocytoma were enrolled. In a second study conducted by the Children's Oncology Group (COG), 122 patients were enrolled, including patients with medulloblastoma/PNET (29), high grade astrocytoma (23), low grade astrocytoma (22), brain stem glioma (16), ependymoma (14), other CNS tumors (9), and non-CNS tumors (9). The adverse reaction profile in pediatric patients was similar to adults.
8.5 Geriatric Use
In the Newly Diagnosed Glioblastoma trial, Study MK-7365-051, 15% of patients were 65 years and older. This study did not include sufficient numbers of patients aged 65 years and older to determine differences in effectiveness from younger patients. No overall differences in safety were observed between patients ≥65 years and younger patients.
In the Refractory Anaplastic Astrocytoma trial, Study MK-7365-0006, 4% of patients were 70 years and older. This study did not include sufficient numbers of patients aged 70 years and older to determine differences in effectiveness from younger patients. Patients 70 years and older had a higher incidence of Grade 4 neutropenia (25%) and Grade 4 thrombocytopenia (20%) in the first cycle of therapy than patients less than 70 years of age [see Warnings and Precautions (5.1), Adverse Reactions (6.1)].
8.6 Renal Impairment
No dosage adjustment is recommended for patients with creatinine clearance (CLcr) of 36 to 130 mL/min/m2 [see Clinical Pharmacology (12.3)]. The recommended dose of TEMODAR has not been established for patients with severe renal impairment (CLcr <36 mL/min/m2) or for patients with end-stage renal disease on dialysis.
10. Overdosage
Dose-limiting toxicity was myelosuppression and was reported with any dose but is expected to be more severe at higher doses. An overdose of 2000 mg per day for 5 days was taken by one patient and the adverse reactions reported were pancytopenia, pyrexia, multi-organ failure, and death. There are reports of patients who have taken more than 5 days of treatment (up to 64 days), with adverse reactions reported including myelosuppression, which in some cases was severe and prolonged, and infections and resulted in death. In the event of an overdose, monitor complete blood count and provide supportive measures as necessary.
11. Temodar Description
Temozolomide is an alkylating drug. The chemical name of temozolomide is 3,4-dihydro-3-methyl-4-oxoimidazo[5,1-d]-as-tetrazine-8-carboxamide. The structural formula of temozolomide is:

The material is a white to light tan/light pink powder with a molecular formula of C6H6N6O2 and a molecular weight of 194.15. The molecule is stable at acidic pH (<5) and labile at pH >7; hence TEMODAR can be administered orally and intravenously. The prodrug, temozolomide, is rapidly hydrolyzed to the active 5-(3-methyltriazen-1-yl) imidazole-4-carboxamide (MTIC) at neutral and alkaline pH values, with hydrolysis taking place even faster at alkaline pH.
12. Temodar - Clinical Pharmacology
12.1 Mechanism of Action
Temozolomide is not directly active but undergoes rapid nonenzymatic conversion at physiologic pH to the reactive compound 5-(3-methyltriazen-1-yl)-imidazole-4-carboxamide (MTIC). The cytotoxicity of MTIC is thought to be primarily due to alkylation of DNA. Alkylation (methylation) occurs mainly at the O6 and N7 positions of guanine.
12.3 Pharmacokinetics
Following a single oral dose of 150 mg/m2, the mean Cmax value for temozolomide was 7.5 mcg/mL and for MTIC was 282 ng/mL. The mean AUC value for temozolomide was 23.4 mcg∙hr/mL and for MTIC was 864 ng∙hr/mL.
Following a single 90-minute intravenous infusion of 150 mg/m2, the mean Cmax value for temozolomide was 7.3 mcg/mL and for MTIC was 276 ng/mL. The mean AUC value for temozolomide was 24.6 mcg∙hr/mL and for MTIC was 891 ng∙hr/mL.
Temozolomide exhibits linear kinetics over the therapeutic dosing range of 75 mg/m2/day to 250 mg/m2/day.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Temozolomide is carcinogenic in rats at doses less than the maximum recommended human dose. Temozolomide induced mammary carcinomas in both males and females at doses 0.13 to 0.63 times the maximum human dose (25-125 mg/m2) when administered orally on 5 consecutive days every 28 days for 6 cycles. Temozolomide also induced fibrosarcomas of the heart, eye, seminal vesicles, salivary glands, abdominal cavity, uterus, and prostate, carcinomas of the seminal vesicles, schwannomas of the heart, optic nerve, and harderian gland, and adenomas of the skin, lung, pituitary, and thyroid at doses 0.5 times the maximum daily dose. Mammary tumors were also induced following 3 cycles of temozolomide at the maximum recommended daily dose.
Temozolomide is a mutagen and a clastogen. In a reverse bacterial mutagenesis assay (Ames assay), temozolomide increased revertant frequency in the absence and presence of metabolic activation. Temozolomide was clastogenic in human lymphocytes in the presence and absence of metabolic activation.
Temozolomide impairs male fertility. Temozolomide caused syncytial cells/immature sperm formation at doses of 50 and 125 mg/m2 (0.25 and 0.63 times the human dose of 200 mg/m2) in rats and dogs, respectively, and testicular atrophy in dogs at 125 mg/m2.
13.2 Animal Toxicology and/or Pharmacology
Toxicology studies in rats and dogs identified a low incidence of hemorrhage, degeneration, and necrosis of the retina at temozolomide doses equal to or greater than 125 mg/m2 (0.63 times the human dose of 200 mg/m2). These changes were most commonly seen at doses where mortality was observed.
14. Clinical Studies
14.1 Newly Diagnosed Glioblastoma
The efficacy of TEMODAR was evaluated in Study MK-7365-051, a randomized (1:1), multicenter, open-label trial. Eligible patients were required to have newly diagnosed glioblastoma. Patients were randomized to receive either radiation therapy alone or concomitant TEMODAR 75 mg/m2 once daily starting the first day of radiation therapy and continuing until the last day of radiation therapy for 42 days (with a maximum of 49 days), followed by TEMODAR 150 mg/m2 or 200 mg/m2 once daily on Days 1 to 5 of each 28-day cycle, starting 4 weeks after the end of radiation therapy and continuing for 6 cycles. In both arms, focal radiation therapy was delivered as 60 Gy/30 fractions and included radiation to the tumor bed or resection site with a 2- to 3-cm margin. PCP prophylaxis was required during the concomitant phase regardless of lymphocyte count and continued until recovery of lymphocyte count to Grade 1 or less. The major efficacy outcome measure was overall survival.
A total of 573 patients were randomized, 287 to TEMODAR and radiation therapy and 286 to radiation therapy alone. At the time of disease progression, TEMODAR was administered as salvage therapy in 161 patients of the 282 (57%) in the radiation therapy alone arm and 62 patients of the 277 (22%) in the TEMODAR and radiation therapy arm.
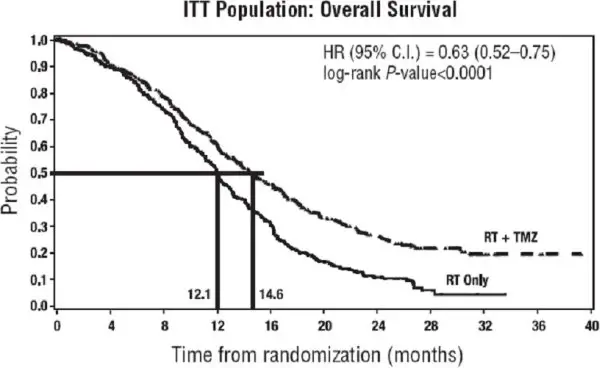
The addition of concomitant and maintenance TEMODAR to radiation therapy for the treatment of patients with newly diagnosed glioblastoma showed a statistically significant improvement in overall survival compared to radiotherapy alone (Figure 1). The hazard ratio (HR) for overall survival was 0.63 (95% CI: 0.52, 0.75) with a log-rank P<0.0001 in favor of the TEMODAR arm. The median survival was increased by 2.5 months in the TEMODAR arm.
 |
14.2 Refractory Anaplastic Astrocytoma
The efficacy of TEMODAR was evaluated in Study MK-7365-006, a single-arm, multicenter trial. Eligible patients had anaplastic astrocytoma at first relapse and a baseline Karnofsky performance status (KPS) of 70 or greater. Patients had previously received radiation therapy and may also have previously received a nitrosourea with or without other chemotherapy. Fifty-four patients had disease progression on prior therapy with both a nitrosourea and procarbazine and their malignancy was considered refractory to chemotherapy (refractory anaplastic astrocytoma population). TEMODAR capsules were given on Days 1 to 5 of each 28-day cycle at a starting dose of 150 mg/m2/day. If ANC was ≥1.5 × 109/L and platelet count was ≥100 × 109/L at the nadir and on Day 1 of the next cycle, the TEMODAR dose was increased to 200 mg/m2/day. The major efficacy outcome measure was progression-free survival at 6 months and the additional efficacy outcome measures were overall survival and overall response rate.
In the refractory anaplastic astrocytoma population (n=54), the median age was 42 years (range: 19 to 76); 65% were male; and 72% had a KPS of >80. Sixty-three percent of patients had surgery other than a biopsy at the time of initial diagnosis. Of those patients undergoing resection, 73% underwent a subtotal resection and 27% underwent a gross total resection. Eighteen percent of patients had surgery at the time of first relapse. The median time from initial diagnosis to first relapse was 13.8 months (range: 4.2 months to 6.3 years).
In the refractory anaplastic astrocytoma population, the overall response rate (CR+PR) was 22% (12 of 54 patients) and the complete response rate was 9% (5 of 54 patients). The median duration of all responses was 50 weeks (range: 16 to 114 weeks) and the median duration of complete responses was 64 weeks (range: 52 to 114 weeks). In this population, progression-free survival at 6 months was 45% (95% CI: 31%, 58%) and progression-free survival at 12 months was 29% (95% CI: 16%, 42%). Median progression-free survival was 4.4 months. Overall survival at 6 months was 74% (95% CI: 62%, 86%) and 12-month overall survival was 65% (95% CI: 52%, 78%). Median overall survival was 15.9 months.
16. How is Temodar supplied
TEMODAR is a cytotoxic drug. Follow applicable special handling and disposal procedures.1
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
| Patient Information | ||
|---|---|---|
| TEMODAR® (tem-o-dar) (temozolomide) capsules | TEMODAR® (tem-o-dar) (temozolomide) for injection |
|
| This Patient Information has been approved by the U.S. Food and Drug Administration. | Revised: November 2022 | |
| What is the most important information I should know about TEMODAR? | ||
| TEMODAR may cause birth defects. | ||
| Females and female partners of male patients who take TEMODAR: | ||
|
||
| Males taking TEMODAR and have a female partner who is pregnant or who can become pregnant: | ||
|
||
| See the section "What are the possible side effects of TEMODAR?" for more information about side effects. | ||
| What is TEMODAR? | ||
| TEMODAR is a prescription medicine used to treat adults with certain brain cancer tumors. | ||
| It is not known if TEMODAR is safe and effective in children. | ||
| Who should not take TEMODAR? | ||
| Do not take TEMODAR if you: | ||
|
||
| What should I tell my doctor before taking TEMODAR? | ||
| Tell your doctor about all of your medical conditions, including if you: | ||
|
||
| Tell your doctor about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements. Especially tell your doctor if you take a medicine that contains valproic acid. | ||
| Know the medicines you take. Keep a list of them and show it to your doctor and pharmacist when you get a new medicine. | ||
| How should I take TEMODAR? | ||
| TEMODAR may be taken 2 different ways: | ||
|
||
| Your doctor will decide the best way for you to take TEMODAR. Take TEMODAR exactly as prescribed by your doctor. | ||
| There are 2 common dosing schedules for taking TEMODAR depending on the type of brain cancer tumor that you have. | ||
|
||
| TEMODAR capsules: | ||
|
||
| TEMODAR for injection: | ||
|
||
| What are the possible side effects of TEMODAR? | ||
| TEMODAR can cause serious side effects, including: | ||
|
||
| Common side effects of TEMODAR include: | ||
|
|
|
| Additional side effects seen with TEMODAR for injection: | ||
|
||
| TEMODAR can affect fertility in males and may affect your ability to father a child. Talk with your doctor if fertility is a concern for you. | ||
| Tell your doctor about any side effect that bothers you or that does not go away. | ||
| These are not all the possible side effects with TEMODAR. For more information, ask your doctor or pharmacist. | ||
| Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. | ||
| How should I store TEMODAR capsules? | ||
|
||
| General information about the safe and effective use of TEMODAR. | ||
| Medicines are sometimes prescribed for purposes other than those listed in the Patient Information leaflet. Do not use TEMODAR for a condition for which it was not prescribed. Do not give TEMODAR to other people, even if they have the same symptoms that you have. It may harm them. | ||
| This leaflet summarizes the most important information about TEMODAR. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about TEMODAR that is written for health professionals. | ||
| For more information, go to www.TEMODAR.com or call 1-877-888-4231. | ||
| What are the ingredients in TEMODAR? | ||
| TEMODAR capsules: | ||
| Active ingredient: temozolomide. | ||
| Inactive ingredients: lactose anhydrous, colloidal silicon dioxide, sodium starch glycolate, tartaric acid, stearic acid. | ||
| The body of the capsules is made of gelatin and is opaque white. The cap is also made of gelatin, and the colors vary based on the dosage strength. The capsule body and cap are imprinted with pharmaceutical branding ink, which contains shellac, dehydrated alcohol, isopropyl alcohol, butyl alcohol, propylene glycol, purified water, strong ammonia, potassium hydroxide, and ferric oxide. | ||
| TEMODAR 5 mg: The green cap contains gelatin, titanium dioxide, iron oxide yellow, sodium lauryl sulfate, and FD&C Blue #2. | ||
| TEMODAR 20 mg: The yellow cap contains gelatin, sodium lauryl sulfate, and iron oxide yellow. | ||
| TEMODAR 100 mg: The pink cap contains gelatin, titanium dioxide, sodium lauryl sulfate, and iron oxide red. | ||
| TEMODAR 140 mg: The blue cap contains gelatin, sodium lauryl sulfate, and FD&C Blue #2. | ||
| TEMODAR 180 mg: The orange cap contains gelatin, iron oxide red, iron oxide yellow, titanium dioxide, and sodium lauryl sulfate. | ||
| TEMODAR 250 mg: The white cap contains gelatin, titanium dioxide, and sodium lauryl sulfate. | ||
| TEMODAR for injection: | ||
| Active ingredient: temozolomide. | ||
| Inactive ingredients: mannitol, L-threonine, polysorbate 80, sodium citrate dihydrate, and hydrochloric acid. | ||
| Distributed by: Merck Sharp & Dohme LLC Rahway, NJ 07065, USA |
||
| For patent information: www.msd.com/research/patent | ||
| The trademarks depicted herein are owned by their respective companies. | ||
| Copyright © 1999-2022 Merck & Co., Inc., Rahway, NJ, USA, and its affiliates.
All rights reserved. |
||
| Revised: 11/2022 | ||
| usppi-mk7365-mtl-2211r012 | ||
TEMODAR® (temozolomide) for injection
PHARMACIST:
Dispense enclosed Patient Package Insert to each patient.
PHARMACIST INFORMATION SHEET
What is TEMODAR? [See Full Prescribing Information, Indications and Usage (1).]
TEMODAR® (temozolomide) is an alkylating drug for the treatment of adult patients with newly diagnosed glioblastoma multiforme and refractory anaplastic astrocytoma.
How is TEMODAR dosed? [See Full Prescribing Information, Recommended Dosage and Dosage Modifications for Newly Diagnosed Glioblastoma (2.1), Recommended Dosage and Dosage Modifications for Refractory Anaplastic Astrocytoma (2.2).]
The physician calculates the daily dose of TEMODAR for a given patient based on the patient’s body surface area (BSA). The recommended dose for TEMODAR as an intravenous infusion over 90 minutes is the same as the dose for the oral capsule formulation. Adjust the dose for subsequent cycles according to nadir neutrophil and platelet counts in the previous cycle and at the time of initiating the next cycle.
Dosing for Patients with Refractory Anaplastic Astrocytoma [See Full Prescribing Information, Recommended Dosage and Dosage Modifications for Refractory Anaplastic Astrocytoma (2.2).]
The initial dose is 150 mg/m2 intravenously once daily for 5 consecutive days per 28-day treatment cycle. Increase the TEMODAR dose to 200 mg/m2/day for 5 consecutive days per 28-day treatment cycle if both the nadir and day of dosing (Day 29, Day 1 of next cycle) absolute neutrophil counts (ANC) are greater than or equal to 1.5 x 109/L (1500/µL) and both the nadir and Day 29, Day 1 of next cycle platelet counts are greater than or equal to 100 x 109/L (100,000/µL). During treatment, obtain a complete blood count on Day 22 (21 days after the first dose), and weekly until the ANC is above 1.5 x 109/L (1500/µL) and the platelet count exceeds 100 x 109/L (100,000/µL). Do not start the next cycle of TEMODAR until the ANC and platelet count exceed these levels. If the ANC falls to less than 1.0 x 109/L (1000/µL) or the platelet count is less than 50 x 109/L (50,000/µL) during any cycle, reduce the dose for the next cycle by 50 mg/m2. Permanently discontinue TEMODAR in patients who are unable to tolerate a dose of 100 mg/m2 per day.
Patients should continue to receive TEMODAR until their physician determines that their disease has progressed, or until unacceptable side effects or toxicities occur. In the clinical trial, treatment could be continued for a maximum of 2 years, but the optimum duration of therapy is not known. Physicians may alter the treatment regimen for a given patient.
Dosing for Patients with Newly Diagnosed Glioblastoma Multiforme [See Full Prescribing Information, Recommended Dosage and Dosage Modifications for Newly Diagnosed Glioblastoma (2.1).]
Concomitant Phase Treatment Schedule
Administer TEMODAR at 75 mg/m2 daily for 42 days concomitant with focal radiotherapy (60 Gy administered in 30 fractions), followed by maintenance TEMODAR for 6 cycles. No dose reductions are recommended; however, dose interruptions may occur based on patient tolerance. Continue the TEMODAR dose throughout the 42-day concomitant period up to 49 days if all of the following conditions are met: absolute neutrophil count greater than or equal to 1.5 x 109/L, platelet count greater than or equal to 100 x 109/L, and nonhematological adverse reactions less than or equal to Grade 1 (except for alopecia, nausea, and vomiting). During treatment, obtain a complete blood count weekly. Interrupt or discontinue temozolomide dosing during the concomitant phase according to the hematological and nonhematological toxicity criteria [see Table 1 in the Full Prescribing Information, Recommended Dosage and Dosage Modifications for Newly Diagnosed Glioblastoma (2.1)]. Pneumocystis pneumonia (PCP) prophylaxis is required during the concomitant administration of TEMODAR and radiotherapy, and should be continued in patients who develop lymphocytopenia until resolution to Grade 1 or less.
Maintenance Phase Treatment Schedule
Four weeks after completing the TEMODAR and radiotherapy phase, administer TEMODAR for an additional 6 cycles of maintenance treatment. Dosage in Cycle 1 (maintenance) is 150 mg/m2 once daily for 5 days followed by 23 days without treatment. At the start of Cycle 2, escalate the dose to 200 mg/m2, if the nonhematologic adverse reactions for Cycle 1 are Grade less than or equal to 2 (except for alopecia, nausea, and vomiting), absolute neutrophil count (ANC) is greater than or equal to 1.5 x 109/L, and the platelet count is greater than or equal to 100 x 109/L. If the dose was not escalated at Cycle 2, do not escalate the dose in subsequent cycles. Maintain the dose at 200 mg/m2 per day for the first 5 days of each subsequent cycle except if toxicity occurs.
During treatment, obtain a complete blood count on Day 22 (21 days after the first dose) and weekly until the ANC is above 1.5 x 109/L (1500/µL) and the platelet count exceeds 100 x 109/L (100,000/µL). Do not start the next cycle of TEMODAR until the ANC and platelet count exceed these levels. Base dose reductions during the next cycle on the lowest blood counts and worst nonhematologic adverse reactions during the previous cycle. Apply dose reductions or discontinuations during the maintenance phase [see Table 2 in the Full Prescribing Information, Recommended Dosage and Dosage Modifications for Newly Diagnosed Glioblastoma (2.1)].
How is TEMODAR for injection prepared? [See Full Prescribing Information, Preparation and Administration, TEMODAR for injection (2.3).]
Take care in the handling and preparation of TEMODAR. Do not open vials. If vials are accidentally opened or damaged, take rigorous precautions with the contents to avoid inhalation or contact with the skin or mucous membranes. In case of powder contact, wash hands. Use gloves and safety glasses to avoid exposure in case of breakage of the vial. Consider implementing procedures for proper handling and disposal of anticancer drugs {see “OSHA Hazardous Drugs” reference below}. Several guidelines on this subject have been published.
- Store TEMODAR for injection vials refrigerated at 2°- 8°C (36°- 46°F).
- Bring the vial to room temperature prior to reconstitution with Sterile Water for Injection.
- Using aseptic technique, reconstitute each vial with 41 mL Sterile Water for Injection. The resulting solution will contain 2.5 mg/mL temozolomide.
- Gently swirl vial. Do not shake.
- Visually inspect reconstituted solution, and discard if particulate matter or discoloration is observed.
- Do not further dilute the reconstituted solution.
- Store reconstituted solution at room temperature for up to 14 hours, including infusion time.
- Using aseptic technique, withdraw up to 40 mL from each vial to make up the total dose and transfer into an empty 250 mL infusion bag. Discard any unused portion.
- Attach the pump tubing to the bag, purge the tubing, and then cap.
How is TEMODAR for injection administered? [See Full Prescribing Information, Preparation and Administration, TEMODAR for injection (2.3).]
Administer TEMODAR for injection as an intravenous infusion over 90 minutes. Administer TEMODAR for injection only by intravenous infusion. Flush the lines before and after each TEMODAR infusion.
TEMODAR for injection may be administered in the same intravenous line with 0.9% Sodium Chloride injection only.
Because no data are available on the compatibility of TEMODAR for injection with other intravenous substances or additives, other medications should not be infused simultaneously through the same intravenous line.
What should the patient avoid during treatment with TEMODAR? [See Full Prescribing Information, Use in Specific Populations, Pregnancy (8.1), Lactation (8.2), Females and Males of Reproductive Potential (8.3).]
There are no dietary restrictions for patients taking TEMODAR. TEMODAR may affect testicular function and may cause birth defects. Advise male patients to exercise adequate birth control measures. Advise female patients to avoid becoming pregnant while receiving this drug. Advise pregnant women of the potential risk to the fetus. Advise females of reproductive potential to use effective contraception during treatment and for at least 6 months after the last dose. Advise males of reproductive potential to use condoms during treatment and for at least 3 months after the last dose. Advise male patients not to donate semen during treatment with TEMODAR and for at least 3 months after the final dose. It is not known whether TEMODAR is excreted into breast milk. Because of the potential for serious adverse reactions in breastfed children, advise women not to breastfeed while taking TEMODAR and for at least 1 week after the last dose.
What are the side effects of TEMODAR? [See Full Prescribing Information, Adverse Reactions (6).]
Alopecia, fatigue, nausea, and vomiting are the most common side effects associated with TEMODAR. Noncumulative myelosuppression is the dose-limiting toxicity. Patients should be evaluated periodically by their physician to monitor blood counts.
Other commonly reported side effects reported by patients taking TEMODAR are headache, constipation, anorexia, convulsions, bruising, petechia, and hematoma, as well as pain, irritation, itching, warmth, swelling, and erythema at the site of infusion.
How is TEMODAR supplied? [See Full Prescribing Information, How Supplied/Storage and Handling (16).]
TEMODAR for injection is supplied in single-dose glass vials containing 100 mg temozolomide (NDC 0085-1381-01). TEMODAR is also available as capsules in 5-mg, 20-mg, 100-mg, 140-mg, 180-mg, and 250-mg strengths.
References:
“OSHA Hazardous Drugs.” OSHA. http://www.osha.gov/SLTC/hazardousdrugs/index.
TEMODAR® (temozolomide) capsules
PHARMACIST:
Dispense enclosed Patient Package Insert to each patient.
PHARMACIST INFORMATION SHEET
What is TEMODAR? [See Full Prescribing Information, Indications and Usage (1).]
TEMODAR® (temozolomide) is an oral alkylating agent for the treatment of newly diagnosed glioblastoma multiforme and refractory anaplastic astrocytoma.
How is TEMODAR dosed? [See Full Prescribing Information, Recommended Dosage and Dosage Modifications for Newly Diagnosed Glioblastoma (2.1), Recommended Dosage and Dosage Modifications for Refractory Anaplastic Astrocytoma (2.2).]
The physician calculates the daily dose of TEMODAR capsules for a given patient based on the patient’s body surface area (BSA). Round off the resulting dose to the nearest 5 mg. An example of the dosing may be as follows: the initial daily dose of TEMODAR in milligrams is the BSA multiplied by mg/m2/day (e.g., a patient with a BSA of 1.84 is 1.84 x 75 mg = 138, or 140 mg/day). Adjust the dose for subsequent cycles according to nadir neutrophil and platelet counts in the previous cycle and at the time of initiating the next cycle.
How might the dose of TEMODAR be modified for Refractory Anaplastic Astrocytoma? [See Full Prescribing Information, Recommended Dosage and Dosage Modifications for Refractory Anaplastic Astrocytoma (2.2).]
The initial dose is 150 mg/m2 orally once daily for 5 consecutive days per 28-day treatment cycle. Increase the TEMODAR dose to 200 mg/m2/day for 5 consecutive days per 28-day treatment cycle if both the nadir and day of dosing (Day 29, Day 1 of next cycle) absolute neutrophil counts (ANC) are greater than or equal to 1.5 x 109/L (1500/µL) and both the nadir and Day 29, Day 1 of next cycle platelet counts are greater than or equal to 100 x 109/L (100,000/µL). During treatment, obtain a complete blood count on Day 22 (21 days after the first dose), and weekly until the ANC is above 1.5 x 109/L (1500/µL) and the platelet count exceeds 100 x 109/L (100,000/µL). Do not start the next cycle of TEMODAR until the ANC and platelet count exceed these levels. If the ANC falls to less than 1.0 x 109/L (1000/µL) or the platelet count is less than 50 x 109/L (50,000/µL) during any cycle, reduce the dose for the next cycle by 50 mg/m2. Permanently discontinue TEMODAR in patients who are unable to tolerate a dose of 100 mg/m2 per day.
Patients should continue taking TEMODAR until their physician determines that their disease has progressed or until unacceptable side effects or toxicities occur. In the clinical trial, treatment could be continued for a maximum of 2 years, but the optimum duration of therapy is not known. Physicians may alter the treatment regimen for a given patient.
Dosing for Patients with Newly Diagnosed Glioblastoma Multiforme [See Full Prescribing Information, Recommended Dosage and Dosage Modifications for Newly Diagnosed Glioblastoma (2.1).]
Concomitant Phase Treatment Schedule
Administer TEMODAR orally at 75 mg/m2 daily for 42 days concomitant with focal radiotherapy (60 Gy administered in 30 fractions), followed by maintenance TEMODAR for 6 cycles. No dose reductions are recommended; however, dose interruptions may occur based on patient tolerance. Continue the TEMODAR dose throughout the 42-day concomitant period up to 49 days if all of the following conditions are met: absolute neutrophil count greater than or equal to 1.5 x 109/L, platelet count greater than or equal to 100 x109/L, and nonhematological adverse reactions less than or equal to Grade 1 (except for alopecia, nausea and vomiting). During treatment, obtain a complete blood count weekly. Interrupt or discontinue temozolomide dosing during the concomitant phase according to the hematological and nonhematological toxicity criteria [see Table 1 in the Full Prescribing Information, Recommended Dosage and Dosage Modifications for Newly Diagnosed Glioblastoma (2.1)]. Pneumocystis pneumonia (PCP) prophylaxis is required during the concomitant administration of TEMODAR and radiotherapy, and should be continued in patients who develop lymphocytopenia until resolution to Grade 1 or less.
Maintenance Phase Treatment Schedule
Four weeks after completing the TEMODAR and radiotherapy phase, administer TEMODAR for an additional 6 cycles of maintenance treatment. Dosage in Cycle 1 (maintenance) is 150 mg/m2 once daily for 5 days followed by 23 days without treatment. At the start of Cycle 2, escalate the dose to 200 mg/m2, if the nonhematologic adverse reactions for Cycle 1 are Grade less than or equal to 2 (except for alopecia, nausea and vomiting), absolute neutrophil count (ANC) is greater than or equal to 1.5 x 109/L, and the platelet count is greater than or equal to 100 x 109/L. If the dose was not escalated at Cycle 2, do not escalate the dose in subsequent cycles. Maintain the dose at 200 mg/m2 per day for the first 5 days of each subsequent cycle except if toxicity occurs.
During treatment, obtain a complete blood count on Day 22 (21 days after the first dose) and weekly until the ANC is above 1.5 x 109/L (1500/µL) and the platelet count exceeds 100 x 109/L (100,000/µL). Do not start the next cycle of TEMODAR until the ANC and platelet count exceed these levels. Base dose reductions during the next cycle on the lowest blood counts and worst nonhematologic adverse reactions during the previous cycle. Apply dose reductions or discontinuations during the maintenance phase [see Table 2 in the Full Prescribing Information, Recommended Dosage and Dosage Modifications for Newly Diagnosed Glioblastoma (2.1)].
How is TEMODAR taken? [See Full Prescribing Information, Preparation and Administration, TEMODAR capsules (2.3).]
Advise patients to take each day’s dose with a full glass of water, preferably on an empty stomach or at bedtime. Taking the medication on an empty stomach or at bedtime may help ease nausea. If patients are also taking anti-nausea or other medications to relieve the side effects associated with TEMODAR, advise them to take these medications prior to and/or following administration of TEMODAR capsules. Advise patients that TEMODAR capsules should be swallowed whole and NEVER CHEWED. Advise patients that they SHOULD NOT open or split the capsules. If capsules are accidentally opened or damaged, advise patients to take rigorous precautions with the capsule contents to avoid inhalation or contact with the skin or mucous membranes. In case of powder contact, advise the patients to wash their hands. Advise patients to keep this medication away from children.
What should the patient avoid during treatment with TEMODAR? [See Full Prescribing Information, Use in Specific Populations, Pregnancy (8.1), Lactation (8.2), Females and Males of Reproductive Potential (8.3).]
There are no dietary restrictions for patients taking TEMODAR. TEMODAR may affect testicular function and may cause birth defects. Advise male patients to exercise adequate birth control measures. Advise female patients to avoid becoming pregnant while receiving this drug. Advise pregnant women of the potential risk to the fetus. Advise females of reproductive potential to use effective contraception during treatment and for at least 6 months after the last dose. Advise males of reproductive potential to use condoms during treatment and for at least 3 months after the last dose. Advise male patients not to donate semen during treatment with TEMODAR and for at least 3 months after the final dose. It is not known whether TEMODAR is excreted into breast milk. Because of the potential for serious adverse reactions in breastfed children, advise women not to breastfeed while taking TEMODAR and for at least 1 week after the last dose.
What are the side effects of TEMODAR? [See Full Prescribing Information, Adverse Reactions (6).]
Alopecia, fatigue, nausea, and vomiting are the most common side effects associated with TEMODAR. Noncumulative myelosuppression is the dose-limiting toxicity. Patients should be evaluated periodically by their physician to monitor blood counts.
Other commonly reported side effects reported by patients taking TEMODAR are headache, constipation, anorexia, and convulsions.
How is TEMODAR supplied? [See Full Prescribing Information, How Supplied/Storage and Handling (16).]
TEMODAR capsules are available in 5-mg, 20-mg, 100-mg, 140-mg, 180-mg, and 250-mg strengths. The capsules contain a white capsule body with a color cap, and the colors vary based on the dosage strength.
| TEMODAR Capsule Strength | Color |
|---|---|
| 5 mg | Green Cap |
| 20 mg | Yellow Cap |
| 100 mg | Pink Cap |
| 140 mg | Blue Cap |
| 180 mg | Orange Cap |
| 250 mg | White Cap |
The 5-mg, 20-mg, 100-mg, 140-mg, and 180-mg capsule strengths are available in 5-count and 14-count packages. The 250-mg capsule strength is available in a 5-count package.
TEMODAR is also available for injection in single-dose glass vials containing 100mg temozolomide.
How is TEMODAR dispensed?
Dispense each strength of TEMODAR in a separate vial or in its original package (one strength per one container). Follow the instructions below:
Based on the dose prescribed, determine the number of each strength of TEMODAR capsules needed for the full 42- or 5-day cycle as prescribed by the physician. For example, in a 5-day cycle, 275 mg/day would be dispensed as five 250-mg capsules, five 20-mg capsules and five 5-mg capsules. Label each container with the appropriate number of capsules to be taken each day. Dispense to the patient, making sure each container lists the strength (mg) per capsule and that he or she understands to take the appropriate number of capsules of TEMODAR from each package or vial to equal the total daily dose prescribed by the physician.
How can TEMODAR be ordered?
TEMODAR can be ordered from your wholesaler. It is important to understand if TEMODAR is being used as part of a 42-day regimen or as part of a 5-day course. Remember to order enough TEMODAR for the appropriate cycle.
For example:
- a 5-day course of 360 mg/day would require the following to be ordered: two 5-count packages of 180-mg capsules.
- a 42-day course of 140 mg/day would require the following to be ordered: three 14-count packages of 140-mg capsules.
| TEMODAR Product | NDC Number |
|---|---|
| Sachets: | |
| 5-mg capsules (5 count) | 0085-3004-03 |
| 5-mg capsules (14 count) | 0085-3004-04 |
| 20-mg capsules (5 count) | 0085-1519-03 |
| 20-mg capsules (14 count) | 0085-1519-04 |
| 100-mg capsules (5 count) | 0085-1366-03 |
| 100-mg capsules (14 count) | 0085-1366-04 |
| 140-mg capsules (5 count) | 0085-1425-03 |
| 140-mg capsules (14 count) | 0085-1425-04 |
| 180-mg capsules (5 count) | 0085-1430-03 |
| 180-mg capsules (14 count) | 0085-1430-04 |
| 250-mg capsules (5 count) | 0085-1417-02 |
References:
“OSHA Hazardous Drugs.” OSHA. http://www.osha.gov/SLTC/hazardousdrugs/index.
| TEMODAR
temozolomide capsule |
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
| TEMODAR
temozolomide capsule |
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
| TEMODAR
temozolomide capsule |
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
| TEMODAR
temozolomide capsule |
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
| TEMODAR
temozolomide capsule |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| TEMODAR
temozolomide capsule |
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||
| TEMODAR
temozolomide injection, powder, lyophilized, for solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Merck Sharp & Dohme LLC (118446553) |











