Drug Detail:Thymoglobulin (rabbit) (Anti-thymocyte globulin (rabbit) [ an-tee-thye-moe-syt-glob-ue-lin ])
Drug Class: Selective immunosuppressants
Highlights of Prescribing Information
THYMOGLOBULIN (anti-thymocyte globulin [rabbit]) for injection, for intravenous use
Initial U.S. Approval: 1998
WARNING: IMMUNOSUPPRESSION
THYMOGLOBULIN should only be used by physicians experienced in immunosuppressive therapy in transplantation. (5.1)
Indications and Usage for Thymoglobulin
- THYMOGLOBULIN is an immunoglobulin G indicated for the prophylaxis and treatment of acute rejection in patients receiving a kidney transplant. (1)
- Use in conjunction with concomitant immunosuppression. (1)
Thymoglobulin Dosage and Administration
- The first dose should be infused over at least 6 hours; doses on subsequent days should be infused over at least 4 hours. (2.2)
- Premedication with corticosteroids, acetaminophen, and/or an antihistamine prior to each infusion is recommended. (2.2)
- The THYMOGLOBULIN dose should be reduced by one-half if the white blood cell (WBC) count is between 2,000 and 3,000 cells/mm3 or if the platelet count is between 50,000 and 75,000 cells/mm3. Stopping THYMOGLOBULIN treatment should be considered if the WBC count falls below 2,000 cells/mm3 or if the platelet count falls below 50,000 cells/mm3. (2.3)
| Indication | Dose |
|---|---|
| Prophylaxis of acute rejection | 1.5 mg/kg of body weight administered daily for 4 to 7 days |
| Treatment of acute rejection | 1.5 mg/kg of body weight administered daily for 7 to 14 days |
For complete dosing instructions, see full prescribing information. (2)
Dosage Forms and Strengths
- Single-dose 10 mL vial containing 25 mg of anti-thymocyte globulin (rabbit) lyophilized, sterile powder. (3)
Contraindications
Allergy or anaphylactic reaction to rabbit proteins or to any product excipients, or active acute or chronic infections which contraindicate any additional immunosuppression (4)
Warnings and Precautions
- THYMOGLOBULIN should only be used by physicians experienced in immunosuppressant therapy in transplantation. (5.1)
- Immune-mediated reactions: THYMOGLOBULIN infusion could result in an anaphylactic reaction. (5.2)
- Infusion-associated reactions: Close compliance with the recommended infusion time may reduce the incidence and severity of infusion-associated reactions. (5.3)
- Hematologic effects: low counts of platelets and white blood cells have been identified and are reversible following dose adjustments. Monitor total white blood cell and platelet counts. (5.4)
- Infection: Infections and reactivation of infections have been reported. Monitor patients and administer anti-infective prophylaxis. (5.5)
- Malignancy: Incidence of malignancies may increase. (5.6)
- Immunization with attenuated live vaccines is not recommended for patients who have recently received THYMOGLOBULIN. (5.7)
- THYMOGLOBULIN may interfere with rabbit antibody–based immunoassays and with cross-match or panel-reactive antibody cytotoxicity assays. (5.8)
Adverse Reactions/Side Effects
The most common adverse reactions and laboratory abnormalities (incidence >5% higher than comparator) are urinary tract infection, abdominal pain, hypertension, nausea, shortness of breath, fever, headache, anxiety, chills, increased potassium levels in the blood, low counts of platelets and white blood cells. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Genzyme Corporation at 1-800-633-1610 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 3/2023
Full Prescribing Information
WARNING: IMMUNOSUPPRESSION
THYMOGLOBULIN should only be used by physicians experienced in immunosuppressive therapy in transplantation [see Warnings and Precautions (5.1)].
1. Indications and Usage for Thymoglobulin
THYMOGLOBULIN is indicated for the prophylaxis and treatment of acute rejection in patients receiving a kidney transplant. THYMOGLOBULIN is to be used in conjunction with concomitant immunosuppression.
2. Thymoglobulin Dosage and Administration
THYMOGLOBULIN is intended for intravenous use only.
2.2 Recommended Dosing Regimen
Administer the first dose of THYMOGLOBULIN over a minimum of 6 hours; administer doses on subsequent days over at least 4 hours [see Warnings and Precautions (5.3)].
Premedication with corticosteroids, acetaminophen, and/or an antihistamine 1 hour prior to each infusion of THYMOGLOBULIN is recommended and may reduce the incidence and intensity of infusion-associated reactions [see Warnings and Precautions (5.2, 5.3) and Adverse Reactions (6.1)].
2.3 Dose Modifications
Monitor patients for adverse reactions during and after infusion. Monitor total white blood cell and platelet counts during and after THYMOGLOBULIN therapy.
Reduce the THYMOGLOBULIN dose by one-half if the white blood cell (WBC) count is between 2,000 and 3,000 cells/mm3 or if the platelet count is between 50,000 and 75,000 cells/mm3. Consider stopping THYMOGLOBULIN treatment if the WBC count falls below 2,000 cells/mm3 or if the platelet count falls below 50,000 cells/mm3.
2.4 Recommended Concomitant Medication
THYMOGLOBULIN is used with concomitant immunosuppressants.
Administer prophylactic antifungal and antibacterial therapy if clinically indicated [see Warnings and Precautions (5.5)].
Antiviral prophylactic therapy is recommended for patients who are seropositive for cytomegalovirus (CMV) at the time of transplant and for CMV-seronegative patients scheduled to receive a kidney from a CMV-seropositive donor [see Warnings and Precautions (5.5)].
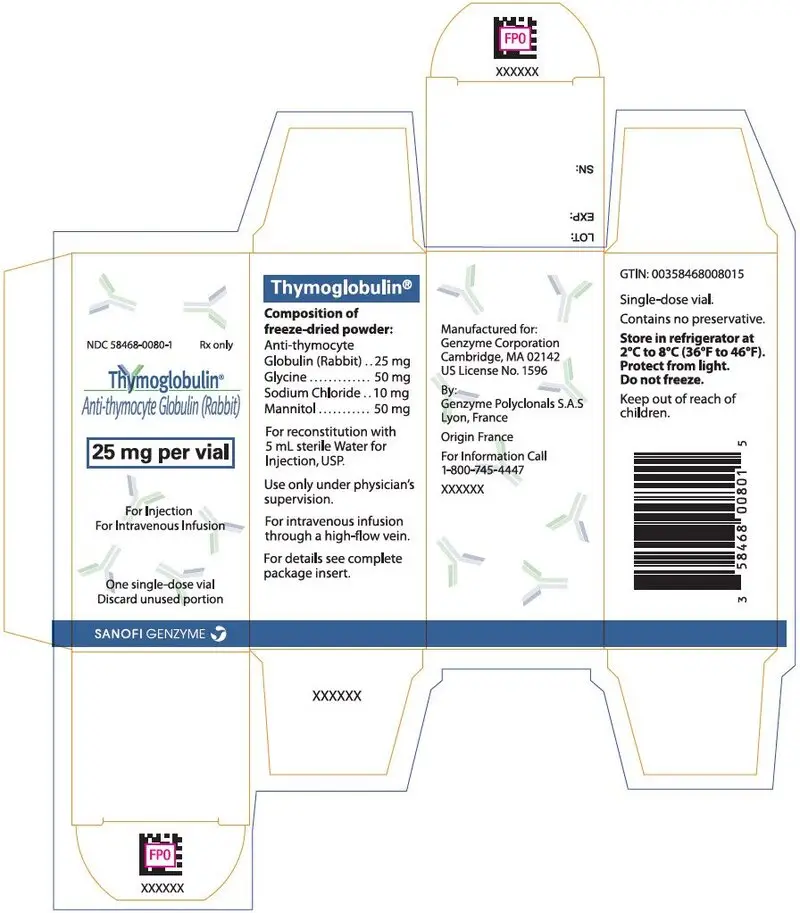
3. Dosage Forms and Strengths
THYMOGLOBULIN for injection: 25 mg anti-thymocyte globulin (rabbit) as a sterile lyophilized powder, in single-dose 10 mL vials for reconstitution.
4. Contraindications
THYMOGLOBULIN is contraindicated in patients with history of allergy or anaphylactic reaction to rabbit proteins or to any product excipients, or who have active acute or chronic infections that contraindicate any additional immunosuppression [see Warnings and Precautions (5.2, 5.5) and Adverse Reactions (6.2)].
5. Warnings and Precautions
5.1 Management of Immunosuppression
To prevent over-immunosuppression, physicians may wish to decrease the dose of the maintenance immunosuppression regimen during the period of THYMOGLOBULIN use.
Dosing for THYMOGLOBULIN is different from dosing for other anti-thymocyte globulin (ATG) products, because protein composition and concentrations vary depending on the source of ATG. The prescribing physician must ensure that the dose prescribed is appropriate for the ATG product being administered.
5.2 Immune-Mediated Reactions
Serious immune-mediated reactions, including anaphylaxis or severe cytokine release syndrome (CRS), have been reported with the use of THYMOGLOBULIN [see Warnings and Precautions (5.3)].
Fatal anaphylaxis has been reported. If an anaphylactic reaction occurs, terminate the infusion immediately. Provide emergency treatment, such as 0.3 mL to 0.5 mL aqueous epinephrine (1:1000 dilution) subcutaneously and other resuscitative measures including oxygen, intravenous fluids, antihistamines, corticosteroids, pressor amines, and airway management, as clinically indicated.
5.3 Infusion-Associated Reactions
Cases consistent with cytokine release syndrome (CRS) have been reported with rapid infusion rates. CRS is attributed to the release of cytokines by activated monocytes and lymphocytes. Severe acute CRS can cause serious cardiorespiratory events and/or death [see Adverse Reactions (6.2)]. Close compliance with the recommended dosage and infusion time may reduce the incidence and severity of infusion-associated reactions (IARs). Slowing the infusion rate may minimize many of these IARs.
Reactions at the infusion site may include pain, swelling, and redness of the skin.
5.4 Hematologic Effects
Low counts of platelets and white blood cells (including low counts of lymphocytes and neutrophils) have been identified and are reversible following dose adjustments. Total white blood cell and platelet counts should be monitored [see Dosage and Administration (2.3)].
5.5 Infection
THYMOGLOBULIN is routinely used in combination with other immunosuppressive agents. Infections (bacterial, fungal, viral and protozoal), reactivation of infection (particularly cytomegalovirus [CMV]) and sepsis have been reported after THYMOGLOBULIN administration in combination with multiple immunosuppressive agents. These infections can be fatal.
Monitor patients carefully and administer appropriate anti-infective treatment when indicated [see Dosage and Administration (2.4)].
5.6 Malignancy
Use of immunosuppressive agents, including THYMOGLOBULIN, may increase the incidence of malignancies, including lymphoma or lymphoproliferative disorders. These events have been associated with fatal outcome [see Adverse Reactions (6.2)].
6. Adverse Reactions/Side Effects
The most common adverse reactions and laboratory abnormalities (incidence >5% higher than comparator) are urinary tract infection, abdominal pain, hypertension, nausea, shortness of breath, fever, headache, anxiety, chills, increased potassium levels in the blood, and low counts of platelets and white blood cells.
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of THYMOGLOBULIN. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
7. Drug Interactions
No drug interaction studies have been performed.
THYMOGLOBULIN can stimulate the production of antibodies that cross-react with rabbit immune globulins [see Clinical Pharmacology (12.3)].
8. Use In Specific Populations
8.4 Pediatric Use
The safety and effectiveness of THYMOGLOBULIN in pediatric patients have not been established in controlled trials. However, based on limited European studies and U.S. compassionate use, the dose, efficacy, and adverse reaction profile are not thought to be different than for adults.
10. Overdosage
THYMOGLOBULIN overdosage may result in leukopenia (including lymphopenia and neutropenia) and/ or thrombocytopenia, which can be managed with dose reduction [see Dosage and Administration (2.1, 2.3)].
11. Thymoglobulin Description
THYMOGLOBULIN® (anti-thymocyte globulin [rabbit]) is a purified, pasteurized, immunoglobulin G, obtained by immunization of rabbits with human thymocytes. This immunosuppressive product contains cytotoxic antibodies directed against antigens expressed on human T-lymphocytes.
THYMOGLOBULIN is a sterile, lyophilized powder for intravenous administration after reconstitution with sterile Water for Injection, USP (SWFI). Each single-dose 10 mL vial contains 25 mg of anti-thymocyte globulin (rabbit), 50 mg glycine, 10 mg sodium chloride, and 50 mg mannitol.
After reconstitution with 5 mL SWFI, each vial of reconstituted product contains approximately 5 mg/mL of THYMOGLOBULIN, of which >90% is rabbit gamma immune globulin (IgG). The reconstituted solution has a pH of 6.5 to 7.2.
Human red blood cells are used in the manufacturing process to deplete cross-reactive antibodies to non–T-cell antigens. The manufacturing process is validated to remove or inactivate potential exogenous viruses. All human red blood cells are from U.S.-registered or FDA-licensed blood banks. A virus removal step (nanofiltration, using a 20 nm filter) and a viral inactivation step (pasteurization, i.e., heat treatment of active ingredient at 60°C/10 hr) are performed for each lot. Each THYMOGLOBULIN lot is released following potency testing (lymphocytotoxicity and E-rosette inhibition assays), and cross-reactive antibody testing (hemagglutination, platelet agglutination, antiglomerular basement membrane antibody, and fibroblast toxicity assays on every lot).
12. Thymoglobulin - Clinical Pharmacology
12.1 Mechanism of Action
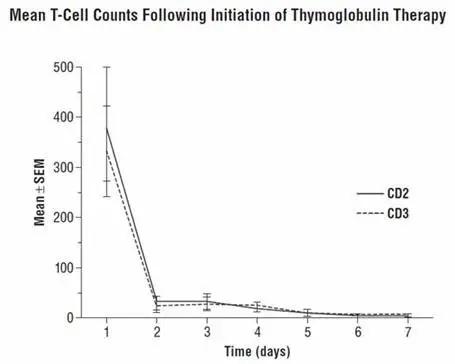
The mechanism of action by which polyclonal antilymphocyte preparations suppress immune responses is not fully understood. Possible mechanisms by which THYMOGLOBULIN may induce immunosuppression in vivo include: T-cell clearance from the circulation and modulation of T-cell activation, homing, and cytotoxic activities. THYMOGLOBULIN includes antibodies against T-cell markers such as CD2, CD3, CD4, CD8, CD11a, CD18, CD25, CD44, CD45, HLA-DR, HLA Class I heavy chains, and ß2 micro-globulin. In vitro, THYMOGLOBULIN (concentrations >0.1 mg/mL) mediates T-cell suppressive effects via inhibition of proliferative responses to several mitogens. In patients, T-cell depletion is usually observed within a day after initiating THYMOGLOBULIN therapy.
THYMOGLOBULIN has not been shown to be effective for treating antibody-mediated (humoral) rejections.
12.3 Pharmacokinetics
After an intravenous dose of 1.25 to 1.5 mg/kg/day (over 4 hours for 7–11 days) 4–8 hours post infusion, THYMOGLOBULIN levels were on average 21.5 mcg/mL (10–40 mcg/mL) with a half-life of 2–3 days after the first dose, and 87 mcg/mL (23–170 mcg/mL) after the last dose.
During the THYMOGLOBULIN Phase 3 randomized trial for the treatment of acute rejection, of the 108 of 163 patients evaluated, anti-rabbit antibodies developed in 68% of the THYMOGLOBULIN-treated patients, and anti-horse antibodies developed in 78% of the Active Comparator-treated patients. No controlled studies have been conducted to study the effect of anti-rabbit antibodies on repeat use of THYMOGLOBULIN. However, to ensure that T-cell depletion is achieved upon retreatment with THYMOGLOBULIN, monitoring the lymphocyte count is recommended. T-cell counts based on data collected from a limited number of patients (n=12) in this study, are presented in the chart below. These data were collected using flow cytometry (FACSCAN, Becton-Dickinson).
14. Clinical Studies
14.2 Treatment of Acute Rejection in Patients Receiving a Kidney Transplant
A controlled, double-blind, multicenter, randomized clinical trial comparing THYMOGLOBULIN and Active Comparator was conducted at 28 US transplant centers in renal transplant patients (n=163) with biopsy-proven Banff Grade II (moderate), Grade III (severe), or steroid-resistant Grade I (mild) acute graft rejection. This clinical trial met the non-inferiority criteria for THYMOGLOBULIN relative to Active Comparator in reversing acute rejection episodes with a 20% non-inferiority margin. The overall weighted estimate of the treatment difference (THYMOGLOBULIN – Active Comparator success rate) was 11% with a lower 95% confidence bound of 0.07%. Therefore, THYMOGLOBULIN was not inferior to Active Comparator in reversing acute rejection episodes.
In the study, patients were randomized to receive 7 to 14 days of THYMOGLOBULIN (1.5 mg/kg/day) or Active Comparator (15 mg/kg/day). For the entire study, the two treatment groups were comparable with respect to donor and recipient characteristics. In Table 9, successful treatment is presented as those patients whose serum creatinine levels (14 days from the diagnosis of rejection) returned to baseline and whose graft was functioning on Day 30 after the end of therapy.
| Success/n | Total | |
|---|---|---|
| Thymoglobulin | Active Comparator* | |
|
||
| Rejection Severity: | ||
| Mild | 9/10 (90%) | 5/8 (63%) |
| Moderate | 44/58 (76%) | 41/58 (71%) |
| Severe | 11/14 (72%) | 8/14 (57%) |
| Overall | 64/82 (78%) | 54/80 (68%) |
| Weighted estimate of difference (Thymoglobulin – Active Comparator*) | 11% | |
| Lower one-sided 95% confidence bound | 0.07% | |
| p Value† | 0.061 | |
There were no statistically significant differences between the two treatments with respect to (1) serum creatinine levels 30 days after treatment relative to baseline, (2) improvement rate in post-treatment histology, (3) one-year post-rejection Kaplan-Meier patient survival (THYMOGLOBULIN 93%, n=82 and Active Comparator 96%, n=80), (4) Day 30 post-rejection graft survival and (5) one-year post-rejection graft survival (THYMOGLOBULIN 83%, n=82; Active Comparator 75%, n=80).
16. How is Thymoglobulin supplied
16.1 How Supplied
THYMOGLOBULIN is supplied as a single-dose clear glass 10 mL vial containing 25 mg of lyophilized (solid) THYMOGLOBULIN. Each carton contains one THYMOGLOBULIN vial (NDC 58468-0080-1).
16.2 Storage and Handling
- Store in refrigerator at 2°C to 8°C (36°F to 46°F).
- Protect from light.
- Do not freeze.
- Do not use after the expiration date indicated on the label.
- Reconstituted THYMOGLOBULIN is physically and chemically stable for up to 24 hours at room temperature; however, room temperature storage is not recommended. As THYMOGLOBULIN contains no preservatives, reconstituted product should be used immediately.
- Infusion solutions of THYMOGLOBULIN must be used immediately.
- Any unused drug remaining after infusion must be discarded.
| THYMOGLOBULIN
anti-thymocyte globulin (rabbit) injection, powder, lyophilized, for solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Genzyme Corporation (025322157) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Genzyme Polyclonals S.A.S. | 500026062 | API MANUFACTURE(58468-0080) , MANUFACTURE(58468-0080) , ANALYSIS(58468-0080) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Genzyme Ireland Limited | 985127419 | MANUFACTURE(58468-0080) , ANALYSIS(58468-0080) , STERILIZE(58468-0080) , LABEL(58468-0080) , PACK(58468-0080) | |