Drug Detail:Tibsovo (Ivosidenib [ eye-voe-sid-e-nib ])
Drug Class: Miscellaneous antineoplastics
Highlights of Prescribing Information
TIBSOVO® (ivosidenib tablets), for oral use
Initial U.S. Approval: 2018
WARNING: DIFFERENTIATION SYNDROME IN AML
See full prescribing information for complete boxed warning.
Patients treated with TIBSOVO have experienced symptoms of differentiation syndrome, which can be fatal. If differentiation syndrome is suspected, initiate corticosteroid therapy and hemodynamic monitoring until symptom resolution (5.1, 6.1).
Recent Major Changes
| Indications and Usage (1.1) | 5/2022 |
| Indications and Usage (1.3) | 8/2021 |
| Dosage and Administration (2.2) | 5/2022 |
Indications and Usage for Tibsovo
TIBSOVO is an isocitrate dehydrogenase-1 (IDH1) inhibitor indicated for patients with a susceptible IDH1 mutation as detected by an FDA-approved test with:
Newly Diagnosed Acute Myeloid Leukemia (AML)
- In combination with azacitidine or as monotherapy for the treatment of newly diagnosed AML in adults 75 years or older, or who have comorbidities that preclude use of intensive induction chemotherapy (1.1).
Relapsed or refractory AML
- For the treatment of adult patients with relapsed or refractory AML (1.2).
Locally Advanced or Metastatic Cholangiocarcinoma
- For the treatment of adult patients with locally advanced or metastatic cholangiocarcinoma who have been previously treated (1.3).
Tibsovo Dosage and Administration
500 mg orally once daily with or without food until disease progression or unacceptable toxicity (2.2). Avoid a high-fat meal.
Dosage Forms and Strengths
Tablets: 250 mg (3).
Contraindications
None (4).
Warnings and Precautions
- QTc Interval Prolongation: Monitor electrocardiograms and electrolytes. If QTc interval prolongation occurs, dose reduce or withhold, then resume dose or permanently discontinue TIBSOVO (2.3, 5.2).
- Guillain-Barré Syndrome: Monitor patients for signs and symptoms of new motor and/or sensory findings. Permanently discontinue TIBSOVO in patients who are diagnosed with Guillain-Barré syndrome (2.3, 5.3).
Adverse Reactions/Side Effects
The most common adverse reactions including laboratory abnormalities (≥25%) in patients with AML are leukocytes decreased, diarrhea, hemoglobin decreased, platelets decreased, glucose increased, fatigue, alkaline phosphatase increased, edema, potassium decreased, nausea, vomiting, phosphate decreased, decreased appetite, sodium decreased, leukocytosis, magnesium decreased, aspartate aminotransferase increased, arthralgia, dyspnea, uric acid increased, abdominal pain, creatinine increased, mucositis, rash, electrocardiogram QT prolonged, differentiation syndrome, calcium decreased, neutrophils decreased, and myalgia (6.1).
The most common adverse reactions (≥15%) in patients with cholangiocarcinoma are fatigue, nausea, abdominal pain, diarrhea, cough, decreased appetite, ascites, vomiting, anemia, and rash (6.1).
The most common laboratory abnormalities (≥10%) in patients with cholangiocarcinoma are hemoglobin decreased, aspartate aminotransferase increased, and bilirubin increased (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact Servier Pharmaceuticals at 1-800-807-6124 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Strong or Moderate CYP3A4 Inhibitors: Reduce TIBSOVO dose with strong CYP3A4 inhibitors. Monitor patients for increased risk of QTc interval prolongation (2.4, 5.2, 7.1, 12.3).
- Strong CYP3A4 Inducers: Avoid concomitant use with TIBSOVO (7.1, 12.3).
- Sensitive CYP3A4 substrates: Avoid concomitant use with TIBSOVO (7.2, 12.3).
- QTc Prolonging Drugs: Avoid concomitant use with TIBSOVO. If co-administration is unavoidable, monitor patients for increased risk of QTc interval prolongation (5.2, 7.1).
Use In Specific Populations
Lactation: Advise women not to breastfeed (8.2).
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 5/2022
Related/similar drugs
venetoclax, Venclexta, azacitidine, durvalumab, vincristine, cytarabine, ImfinziFull Prescribing Information
WARNING: DIFFERENTIATION SYNDROME IN AML
Patients treated with TIBSOVO have experienced symptoms of differentiation syndrome, which can be fatal. Symptoms may include fever, dyspnea, hypoxia, pulmonary infiltrates, pleural or pericardial effusions, rapid weight gain or peripheral edema, hypotension, and hepatic, renal, or multi-organ dysfunction. If differentiation syndrome is suspected, initiate corticosteroid therapy and hemodynamic monitoring until symptom resolution [see Warnings and Precautions (5.1) and Adverse Reactions (6.1)].
1. Indications and Usage for Tibsovo
1.1 Newly Diagnosed Acute Myeloid Leukemia
TIBSOVO is indicated in combination with azacitidine or as monotherapy for the treatment of newly diagnosed acute myeloid leukemia (AML) with a susceptible isocitrate dehydrogenase-1 (IDH1) mutation as detected by an FDA-approved test in adults 75 years or older, or who have comorbidities that preclude use of intensive induction chemotherapy [see Dosage and Administration (2.1), Clinical Pharmacology (12.1) and Clinical Studies (14.1)].
1.2 Relapsed or Refractory Acute Myeloid Leukemia
TIBSOVO is indicated for the treatment of adult patients with relapsed or refractory acute myeloid leukemia (AML) with a susceptible isocitrate dehydrogenase-1 (IDH1) mutation as detected by an FDA-approved test [see Dosage and Administration (2.1), Clinical Pharmacology (12.1) and Clinical Studies (14.2)].
1.3 Locally Advanced or Metastatic Cholangiocarcinoma
TIBSOVO is indicated for the treatment of adult patients with previously treated, locally advanced or metastatic cholangiocarcinoma with an isocitrate dehydrogenase-1 (IDH1) mutation as detected by an FDA-approved test [see Dosage and Administration (2.1), Clinical Pharmacology (12.1), and Clinical Studies (14.3)].
2. Tibsovo Dosage and Administration
2.3 Monitoring and Dosage Modifications for Toxicities
Obtain an electrocardiogram (ECG) prior to treatment initiation. Monitor ECGs at least once weekly for the first 3 weeks of therapy and then at least once monthly for the duration of therapy. Manage any abnormalities promptly [see Adverse Reactions (6.1)].
Interrupt dosing or reduce dose for toxicities. See Table 1 for dose modification guidelines.
| Adverse Reactions | Recommended Action |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| AML monotherapy:
|
2.4 Dosage Modification for Use with Strong CYP3A4 Inhibitors
If a strong CYP3A4 inhibitor must be coadministered, reduce the TIBSOVO dose to 250 mg once daily. If the strong inhibitor is discontinued, increase the TIBSOVO dose (after at least 5 half-lives of the strong CYP3A4 inhibitor) to the recommended dose of 500 mg once daily.
3. Dosage Forms and Strengths
Tablets: 250 mg as a blue oval-shaped film-coated tablet debossed "IVO" on one side and "250" on the other side.
5. Warnings and Precautions
5.1 Differentiation Syndrome in AML
In the combination study AG120-C-009, 15% (11/71) patients with newly diagnosed AML treated with TIBSOVO plus azacitidine experienced differentiation syndrome [see Adverse Reactions (6.1)]. Differentiation syndrome is associated with rapid proliferation and differentiation of myeloid cells and may be life-threatening or fatal. Symptoms of differentiation syndrome in patients treated with TIBSOVO included noninfectious leukocytosis, peripheral edema, pyrexia, dyspnea, pleural effusion, hypotension, hypoxia, pulmonary edema, pneumonitis, pericardial effusion, rash, fluid overload, tumor lysis syndrome and creatinine increased. Of the 11 patients with newly diagnosed AML who experienced differentiation syndrome with TIBSOVO plus azacitidine 8 (73%) recovered. Differentiation syndrome occurred as early as 3 days after start of therapy and during the first month on treatment.
In the monotherapy clinical trial AG120-C-001, 25% (7/28) of patients with newly diagnosed AML and 19% (34/179) of patients with relapsed or refractory AML treated with TIBSOVO experienced differentiation syndrome [see Adverse Reactions (6.1)]. Of the 7 patients with newly diagnosed AML who experienced differentiation syndrome, 6 (86%) patients recovered. Of the 34 patients with relapsed or refractory AML who experienced differentiation syndrome, 27 (79%) patients recovered after treatment or after dose interruption of TIBSOVO. Differentiation syndrome occurred as early as 1 day and up to 3 months after TIBSOVO initiation and has been observed with or without concomitant leukocytosis.
If differentiation syndrome is suspected, initiate dexamethasone 10 mg IV every 12 hours (or an equivalent dose of an alternative oral or IV corticosteroid) and hemodynamic monitoring until improvement [see Dosage and Administration (2.3)]. If concomitant noninfectious leukocytosis is observed, initiate treatment with hydroxyurea or leukapheresis, as clinically indicated. Taper corticosteroids and hydroxyurea after resolution of symptoms and administer corticosteroids for a minimum of 3 days. Symptoms of differentiation syndrome may recur with premature discontinuation of corticosteroid and/or hydroxyurea treatment. If severe signs and/or symptoms persist for more than 48 hours after initiation of corticosteroids, interrupt TIBSOVO until signs and symptoms are no longer severe [see Dosage and Administration (2.3)].
5.2 QTc Interval Prolongation
Patients treated with TIBSOVO can develop QT (QTc) prolongation [see Clinical Pharmacology (12.2)] and ventricular arrhythmias.
Of the 71 patients with newly diagnosed AML treated with TIBSOVO in combination with azacitidine in the clinical trial (Study AG120-C-009), 10 (14%) were found to have a heart-rate corrected QT interval (using Fridericia's method) (QTcF) greater than 500 msec and 15 out of 69 (22%) had an increase from baseline QTcF greater than 60 msec [see Adverse Reactions (6.1)]. The clinical trial excluded patients with a QTcF ≥ 470 msec or other factors that increased the risk of QT prolongation or arrhythmic events (e.g. NYHA Class III or IV congestive heart failure, hypokalemia, family history of long QT interval syndrome).
Of the 258 patients with hematological malignancies treated with TIBSOVO monotherapy in the clinical trial (AG120-C-001), 9% were found to have a QTc interval greater than 500 msec and 14% of patients had an increase from baseline QTc greater than 60 msec [see Adverse Reactions (6.1)]. One patient developed ventricular fibrillation attributed to TIBSOVO. The clinical trial excluded patients with baseline QTc of ≥ 450 msec (unless the QTc ≥ 450 msec was due to a pre-existing bundle branch block) or with a history of long QT syndrome or uncontrolled or significant cardiovascular disease.
Of the 123 patients with cholangiocarcinoma treated with TIBSOVO in the clinical trial (Study AG120-C-005), 2% were found to have a QTc interval greater than 500 msec. and 5% of patients had an increase from baseline QTc greater than 60 msec [see Adverse Reactions (6.1)]. The clinical trial excluded patients with a heart-rate corrected QT interval (using Fridericia's formula) (QTcF) ≥ 450 msec or other factors that increased the risk of QT prolongation or arrhythmic events (e.g., heart failure, hypokalemia, family history of long QT interval syndrome).
Concomitant use of TIBSOVO with drugs known to prolong the QTc interval (e.g., anti-arrhythmic medicines, fluoroquinolones, triazole anti-fungals, 5-HT3 receptor antagonists) and CYP3A4 inhibitors may increase the risk of QTc interval prolongation [see Drug Interactions (7.1), Clinical Pharmacology (12.2)]. Conduct monitoring of electrocardiograms (ECGs) and electrolytes [see Dosage and Administration (2.3)].
In patients with congenital long QTc syndrome, congestive heart failure, electrolyte abnormalities, or those who are taking medications known to prolong the QTc interval, more frequent monitoring may be necessary.
Interrupt TIBSOVO if QTc increases to greater than 480 msec and less than 500 msec. Interrupt and reduce TIBSOVO if QTc increases to greater than 500 msec. Permanently discontinue TIBSOVO in patients who develop QTc interval prolongation with signs or symptoms of life-threatening arrhythmia [See Dosage and Administration (2.3)].
5.3 Guillain-Barré Syndrome
Guillain-Barré syndrome can develop in patients treated with TIBSOVO. Guillain-Barré syndrome occurred in <1% (2/258) of patients treated with TIBSOVO in study AG120-C-001 [see Adverse Reactions (6.1)].
Monitor patients taking TIBSOVO for onset of new signs or symptoms of motor and/or sensory neuropathy such as unilateral or bilateral weakness, sensory alterations, paresthesias, or difficulty breathing. Permanently discontinue TIBSOVO in patients who are diagnosed with Guillain-Barré syndrome [see Dosage and Administration (2.3)].
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Differentiation Syndrome in AML [see Warnings and Precautions (5.1)]
- QTc Interval Prolongation [see Warnings and Precautions (5.2)]
- Guillain-Barré Syndrome [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Newly Diagnosed AML
TIBSOVO in Combination with Azacitidine
The safety of TIBSOVO was evaluated in AML patients treated in combination with azacitidine, in Study AG120-C-009 [see Clinical Studies (14.1)]. Patients received at least one dose of either TIBSOVO 500 mg daily (N=71) or placebo (N=73). Among patients who received TIBSOVO in combination with azacitidine, the median duration of exposure to TIBSOVO was 6 months (range 0 to 33 months). Thirty-four patients (48%) were exposed to TIBSOVO for at least 6 months and 22 patients (31%) were exposed for at least 1 year.
Common (≥ 5%) serious adverse reactions in patients who received TIBSOVO in combination with azacitidine included differentiation syndrome (8%).
Fatal adverse reactions occurred in 4% of patients who received TIBSOVO in combination with azacitidine, due to differentiation syndrome (3%) and one case of cerebral ischemia.
Adverse reactions leading to discontinuation of TIBSOVO in ≥2% of patients were differentiation syndrome (3%) and pulmonary embolism (3%).
The most common (>5%) adverse reactions leading to dose interruption of TIBSOVO were neutropenia (25%), electrocardiogram QT prolonged (7%), and thrombocytopenia (7%).
Adverse reactions leading to dose reduction of TIBSOVO included electrocardiogram QT prolonged (8%), neutropenia (8%), and thrombocytopenia (1%).
The most common adverse reactions and laboratory abnormalities observed in Study AG120-C-009 are shown in Tables 2 and 3.
| TIBSOVO + Azacitidine N=71 | Placebo + Azacitidine N=73 |
|||
|---|---|---|---|---|
| Body System Adverse Reaction | All Grades n (%) | Grade ≥3 n (%) | All Grades n (%) | Grade ≥3 n (%) |
|
||||
| Gastrointestinal disorders | ||||
| Nausea | 30 (42) | 2 (3) | 28 (38) | 3 (4) |
| Vomiting* | 29 (41) | 0 | 20 (27) | 1 (1) |
| Investigations | ||||
| Electrocardiogram QT prolonged | 14 (20) | 7 (10) | 5 (7) | 2 (3) |
| Psychiatric Disorders | ||||
| Insomnia | 13 (18) | 1 (1) | 9 (12) | 0 |
| Blood system and lymphatic system disorders | ||||
| Differentiation Syndrome† | 11 (15) | 7 (10) | 6 (8) | 6 (8) |
| Leukocytosis‡ | 9 (13) | 0 | 1 (1) | 0 |
| Vascular disorders | ||||
| Hematoma§ | 11 (15) | 0 | 3 (4) | 0 |
| Hypertension¶ | 9 (13) | 3 (4) | 6 (8) | 4 (5) |
| Musculoskeletal and connective tissue disorders | ||||
| Arthralgia# | 21 (30) | 3 (4) | 6 (8) | 1 (1) |
| Respiratory, thoracic and mediastinal disorders | ||||
| DyspneaÞ | 14 (20) | 2 (3) | 11 (15) | 4 (5) |
| Nervous system disorders | ||||
| Headache | 8 (11) | 0 | 2 (3) | 0 |
| TIBSOVO + Azacitidine N=71 | Placebo + Azacitidine N=73 |
|||
|---|---|---|---|---|
| Parameter | All Grades n (%) | Grade ≥ 3 n (%) | All Grades n (%) | Grade ≥ 3 n (%) |
|
||||
| Hematology Parameters | ||||
| Leukocytes decreased | 46 (65) | 39 (55) | 47 (64) | 42 (58) |
| Platelets decreased | 41 (58) | 30 (42) | 52 (71) | 42 (58) |
| Hemoglobin decreased | 40 (56) | 33 (46) | 48 (66) | 42 (58) |
| Neutrophils decreased | 18 (25) | 16 (23) | 25 (35) | 23 (32) |
| Lymphocytes increased | 17 (24) | 1 (1) | 7 (10) | 1 (1) |
| Chemistry Parameters | ||||
| Glucose increased | 40 (56) | 9 (13) | 34 (47) | 8 (11) |
| Phosphate decreased | 29 (41) | 7 (10) | 25 (34) | 9 (12) |
| Aspartate Aminotransferase increased | 26 (37) | 0 | 17 (23) | 0 |
| Magnesium decreased | 25 (35) | 0 | 19 (26) | 0 |
| Alkaline Phosphatase increased | 23 (32) | 0 | 21 (29) | 0 |
| Potassium increased | 17 (24) | 2 (3) | 9 (12) | 1 (1) |
TIBSOVO Monotherapy
The safety profile of single-agent TIBSOVO was studied in 28 adults with newly diagnosed AML treated with 500 mg daily [see Clinical Studies (14.1)]. The median duration of exposure to TIBSOVO was 4.3 months (range 0.3 to 40.9 months). Ten patients (36%) were exposed to TIBSOVO for at least 6 months and 6 patients (21%) were exposed for at least 1 year.
Common (≥ 5%) serious adverse reactions included differentiation syndrome (18%), electrocardiogram QT prolonged (7%), and fatigue (7%). There was one case of posterior reversible encephalopathy syndrome (PRES).
Common (≥ 10%) adverse reactions leading to dose interruption included electrocardiogram QT prolonged (14%) and differentiation syndrome (11%). Two (7%) patients required a dose reduction due to electrocardiogram QT prolonged. One patient each required permanent discontinuation due to diarrhea and PRES.
The most common adverse reactions reported in the trial are shown in Table 4.
| TIBSOVO (500 mg daily) N=28 |
||
|---|---|---|
| Body System Adverse Reaction | All Grades n (%) | Grade ≥ 3 n (%) |
|
||
| Gastrointestinal disorders | ||
| Diarrhea | 17 (61) | 2 (7) |
| Nausea | 10 (36) | 2 (7) |
| Abdominal pain* | 8 (29) | 1 (4) |
| Constipation | 6 (21) | 1 (4) |
| Vomiting | 6 (21) | 1 (4) |
| Mucositis† | 6 (21) | 0 |
| Dyspepsia | 3 (11) | 0 |
| General disorders and administration site conditions | ||
| Fatigue‡ | 14 (50) | 4 (14) |
| Edema§ | 12 (43) | 0 |
| Metabolism and nutrition disorders | ||
| Decreased appetite | 11 (39) | 1 (4) |
| Blood system and lymphatic system disorders | ||
| Leukocytosis¶ | 10 (36) | 2 (7) |
| Differentiation Syndrome# | 7 (25) | 3 (11) |
| Musculoskeletal and connective tissue disorders | ||
| ArthralgiaÞ | 9 (32) | 1 (4) |
| Myalgiaß | 7 (25) | 1 (4) |
| Respiratory, thoracic, and mediastinal disorders | ||
| Dyspneaà | 8 (29) | 1 (4) |
| Coughè | 4 (14) | 0 |
| Investigations | ||
| Electrocardiogram QT prolonged | 6 (21) | 3 (11) |
| Weight decreased | 3 (11) | 0 |
| Nervous system disorders | ||
| Dizziness | 6 (21) | 0 |
| Neuropathyð | 4 (14) | 0 |
| Headache | 3 (11) | 0 |
| Skin and subcutaneous tissue disorders | ||
| Pruritis | 4 (14) | 1 (4) |
| Rashø | 4 (14) | 1 (4) |
Changes in selected post-baseline laboratory values that were observed in patients with newly diagnosed AML are shown in Table 5.
| TIBSOVO (500 mg daily) N=28 |
||
|---|---|---|
| Parameter | All Grades n (%) | Grade ≥ 3 n (%) |
|
||
| Hemoglobin decreased | 15 (54) | 12 (43) |
| Alkaline phosphatase increased | 13 (46) | 0 |
| Potassium decreased | 12 (43) | 3 (11) |
| Sodium decreased | 11 (39) | 1 (4) |
| Uric acid increased | 8 (29) | 1 (4) |
| Aspartate aminotransferase increased | 8 (29) | 1 (4) |
| Creatinine increased | 8 (29) | 0 |
| Magnesium decreased | 7 (25) | 0 |
| Calcium decreased | 7 (25) | 1 (4) |
| Phosphate decreased | 6 (21) | 2 (7) |
| Alanine aminotransferase increased | 4 (14) | 1 (4) |
Relapsed or Refractory AML
The safety profile of single-agent TIBSOVO was studied in 179 adults with relapsed or refractory AML treated with 500 mg daily [see Clinical Studies (14.2)]. The median duration of exposure to TIBSOVO was 3.9 months (range 0.1 to 39.5 months). Sixty-five patients (36%) were exposed to TIBSOVO for at least 6 months and 16 patients (9%) were exposed for at least 1 year.
Serious adverse reactions (≥ 5%) were differentiation syndrome (10%), leukocytosis (10%), and electrocardiogram QT prolonged (7%). There was one case of progressive multifocal leukoencephalopathy (PML).
The most common adverse reactions leading to dose interruption were electrocardiogram QT prolonged (7%), differentiation syndrome (3%), leukocytosis (3%) and dyspnea (3%). Five out of 179 patients (3%) required a dose reduction due to an adverse reaction. Adverse reactions leading to a dose reduction included electrocardiogram QT prolonged (1%), diarrhea (1%), nausea (1%), decreased hemoglobin (1%), and increased transaminases (1%). Adverse reactions leading to permanent discontinuation included Guillain-Barré syndrome (1%), rash (1%), stomatitis (1%), and creatinine increased (1%).
The most common adverse reactions reported in the trial are shown in Table 6.
| TIBSOVO (500 mg daily) N=179 |
||
|---|---|---|
| Body System Adverse Reaction | All Grades n (%) | Grade ≥ 3 n (%) |
|
||
| General disorders and administration site conditions | ||
| Fatigue* | 69 (39) | 6 (3) |
| Edema† | 57 (32) | 2 (1) |
| Pyrexia | 41 (23) | 2 (1) |
| Chest pain‡ | 29 (16) | 5 (3) |
| Blood system and lymphatic system disorders | ||
| Leukocytosis§ | 68 (38) | 15 (8) |
| Differentiation Syndrome¶ | 34 (19) | 23 (13) |
| Musculoskeletal and connective tissue disorders | ||
| Arthralgia# | 64 (36) | 8 (4) |
| MyalgiaÞ | 33 (18) | 1 (1) |
| Gastrointestinal disorders | ||
| Diarrhea | 60 (34) | 4 (2) |
| Nausea | 56 (31) | 1 (1) |
| Mucositisß | 51 (28) | 6 (3) |
| Constipation | 35 (20) | 1 (1) |
| Vomitingà | 32 (18) | 2 (1) |
| Abdominal painè | 29 (16) | 2 (1) |
| Respiratory, thoracic, and mediastinal disorders | ||
| Dyspneað | 59 (33) | 16 (9) |
| Coughø | 40 (22) | 1 (<1) |
| Pleural effusion | 23 (13) | 5 (3) |
| Investigations | ||
| Electrocardiogram QT prolonged | 46 (26) | 18 (10) |
| Skin and subcutaneous tissue disorders | ||
| Rashý | 46 (26) | 4 (2) |
| Metabolism and nutrition disorders | ||
| Decreased appetite | 33 (18) | 3 (2) |
| Tumor lysis syndrome | 14 (8) | 11 (6) |
| Nervous system disorders | ||
| Headache | 28 (16) | 0 |
| Neuropathy£ | 21 (12) | 2 (1) |
| Vascular disorders | ||
| Hypotension¥ | 22 (12) | 7 (4) |
Changes in selected post-baseline laboratory values that were observed in patients with relapsed or refractory AML are shown in Table 7.
| TIBSOVO (500 mg daily) N=179 |
||
|---|---|---|
| Parameter | All Grades n (%) | Grade ≥ 3 n (%) |
|
||
| Hemoglobin decreased | 108 (60) | 83 (46) |
| Sodium decreased | 69 (39) | 8 (4) |
| Magnesium decreased | 68 (38) | 0 |
| Uric acid increased | 57 (32) | 11 (6) |
| Potassium decreased | 55 (31) | 11 (6) |
| Alkaline phosphatase increased | 49 (27) | 1 (1) |
| Aspartate aminotransferase increased | 49 (27) | 1 (1) |
| Phosphate decreased | 45 (25) | 15 (8) |
| Creatinine increased | 42 (23) | 2 (1) |
| Alanine aminotransferase increased | 26 (15) | 2 (1) |
| Bilirubin increased | 28 (16) | 1 (1) |
Locally Advanced or Metastatic Cholangiocarcinoma
The safety of TIBSOVO was studied in patients with previously treated, locally advanced or metastatic cholangiocarcinoma in Study AG120-C-005 [see Clinical Studies (14.3)]. Patients received at least one dose of either TIBSOVO 500 mg daily (N=123) or placebo (N=59). The median duration of treatment was 2.8 months (range 0.1 to 34.4 months) with TIBSOVO.
Serious adverse reactions occurred in 34% of patients receiving TIBSOVO. Serious adverse reactions in ≥2% of patients in the TIBSOVO arm were pneumonia, ascites, hyperbilirubinemia, and jaundice cholestatic.
Fatal adverse reactions occurred in 4.9% of patients receiving TIBSOVO, including sepsis (1.6%) and pneumonia, intestinal obstruction, pulmonary embolism, and hepatic encephalopathy (each 0.8%)
TIBSOVO was permanently discontinued in 7% of patients. The most common adverse reactions leading to permanent discontinuation was acute kidney injury (1.6%).
Dose interruptions due to adverse reactions occurred in 29% of patients treated with TIBSOVO. The most common (>2%) adverse reactions leading to dose interruption were hyperbilirubinemia, alanine aminotransferase increased, aspartate aminotransferase increased, ascites, and fatigue.
Dose reductions of TIBSOVO due to an adverse reaction occurred in 4.1% of patients. Adverse reactions leading to dose reduction were electrocardiogram QT prolonged (3.3%) and neuropathy peripheral (0.8%).
The most common adverse reactions (≥15%) were fatigue, nausea, abdominal pain, diarrhea, cough, decreased appetite, ascites, vomiting, anemia, and rash.
Adverse reactions and laboratory abnormalities observed in Study AG120-C-005 are shown in Tables 8 and 9.
| TIBSOVO (500 mg daily) N=123 | Placebo N=59 |
|||
|---|---|---|---|---|
| Body System Adverse Reaction | All Grades n (%) | Grade ≥ 3 n (%) | All Grades n (%) | Grade ≥ 3 n (%) |
|
||||
| General disorders and administration site conditions | ||||
| Fatigue* | 53 (43) | 4 (3) | 18 (31) | 3 (5) |
| Gastrointestinal disorders | ||||
| Nausea | 51 (41) | 3 (2) | 17 (29) | 1 (2) |
| Diarrhea | 43 (35) | 0 | 10 (17) | 0 |
| Abdominal pain† | 43 (35) | 3 (2) | 13 (22) | 2 (3) |
| Ascites | 28 (23) | 11 (9) | 9 (15) | 4 (7) |
| Vomiting‡ | 28 (23) | 3 (2) | 12 (20) | 0 |
| Respiratory, thoracic, and mediastinal disorders | ||||
| Cough§ | 33 (27) | 0 | 5 (9) | 0 |
| Metabolism and nutrition disorders | ||||
| Decreased appetite | 30 (24) | 2 (2) | 11 (19) | 0 |
| Blood and lymphatic system disorders | ||||
| Anemia | 22 (18) | 8 (7) | 3 (5) | 0 |
| Skin and subcutaneous tissue disorders | ||||
| Rash¶ | 19 (15) | 1 (1) | 4 (7) | 0 |
| Nervous system disorders | ||||
| Headache | 16 (13) | 0 | 4 (7) | 0 |
| Neuropathy peripheral# | 13 (11) | 0 | 0 | 0 |
| Investigations | ||||
| Electrocardiogram QT prolonged | 12 (10) | 2 (2) | 2 (3) | 0 |
| TIBSOVO (500 mg daily) N=123 | Placebo N=59 |
|||
|---|---|---|---|---|
| Parameter | All Grades n (%) | Grade ≥ 3 n (%) | All Grades n (%) | Grade ≥ 3 n (%) |
|
||||
| AST increased | 41 (34) | 5 (4) | 14 (24) | 1 (2) |
| Bilirubin increased | 36 (30) | 15 (13) | 11 (19) | 2 (3) |
| Hemoglobin decreased | 48 (40) | 8 (7) | 14 (25) | 0 |
7. Drug Interactions
7.1 Effect of Other Drugs on Ivosidenib
| Strong or Moderate CYP3A4 Inhibitors | |
| Clinical Impact |
|
| Prevention or Management |
|
| Strong CYP3A4 Inducers | |
| Clinical Impact |
|
| Prevention or Management |
|
| QTc Prolonging Drugs | |
| Clinical Impact |
|
| Prevention or Management |
|
7.2 Effect of Ivosidenib on Other Drugs
Ivosidenib induces CYP3A4 and may induce CYP2C9. Co-administration will decrease concentrations of drugs that are sensitive CYP3A4 substrates and may decrease concentrations of drugs that are sensitive CYP2C9 substrates [see Clinical Pharmacology (12.3)]. Use alternative therapies that are not sensitive substrates of CYP3A4 and CYP2C9 during TIBSOVO treatment. If co-administration of TIBSOVO with sensitive CYP3A4 substrates or CYP2C9 substrates is unavoidable, monitor patients for loss of therapeutic effect of these drugs.
Do not administer TIBSOVO with anti-fungal agents that are substrates of CYP3A4 due to expected loss of antifungal efficacy.
Co-administration of TIBSOVO may decrease the concentrations of hormonal contraceptives, consider alternative methods of contraception in patients receiving TIBSOVO.
8. Use In Specific Populations
8.4 Pediatric Use
The safety and effectiveness of TIBSOVO in pediatric patients have not been established.
8.5 Geriatric Use
Of the 72 patients with newly diagnosed AML treated with TIBSOVO in combination with azacitidine, 94% were 65 years of age or older, and 54% were 75 years or older. Of the 34 patients with newly diagnosed AML treated with TIBSOVO monotherapy, 97% were 65 years of age or older, and 56% were 75 years or older. Of the 179 patients with relapsed or refractory AML treated with TIBSOVO monotherapy, 63% were 65 years of age or older and 22% were 75 years or older. Of the 124 patients with cholangiocarcinoma treated with TIBSOVO in Study AG120-C-005, 37% were 65 years of age or older and 11% were 75 years or older.
No overall differences in effectiveness or safety were observed between patients who were 65 years and older compared to younger patients.
8.6 Renal Impairment
No modification of the starting dose is recommended for patients with mild or moderate renal impairment (eGFR ≥ 30 mL/min/1.73m2, MDRD). The pharmacokinetics and safety of ivosidenib in patients with severe renal impairment (eGFR < 30 mL/min/1.73m2, MDRD) or renal impairment requiring dialysis are unknown [see Clinical Pharmacology (12.3)]. For patients with pre-existing severe renal impairment or who are requiring dialysis, consider the risks and potential benefits before initiating treatment with TIBSOVO.
8.7 Hepatic Impairment
No modification of the starting dose is recommended for patients with mild or moderate (Child-Pugh A or B) hepatic impairment [see Clinical Pharmacology (12.3)]. The pharmacokinetics and safety of ivosidenib in patients with severe hepatic impairment (Child-Pugh C) are unknown. For patients with pre-existing severe hepatic impairment, consider the risks and potential benefits before initiating treatment with TIBSOVO.
11. Tibsovo Description
TIBSOVO (ivosidenib) is an inhibitor of isocitrate dehydrogenase 1 (IDH1) enzyme. The chemical name is (2S)-N-{(1S)-1-(2-chlorophenyl)-2-[(3,3-difluorocyclobutyl)-amino]-2-oxoethyl}-1-(4-cyanopyridin-2-yl)-N-(5-fluoropyridin-3-yl)-5-oxopyrrolidine-2-carboxamide. The chemical structure is:
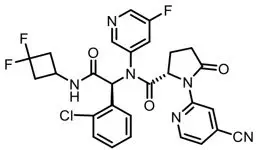
The molecular formula is C28H22ClF3N6O3 and the molecular weight is 583.0 g/mol. Ivosidenib is practically insoluble in aqueous solutions between pH 1.2 and 7.4.
TIBSOVO (ivosidenib) is available as a film-coated 250 mg tablet for oral administration. Each tablet contains the following inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hypromellose acetate succinate, magnesium stearate, microcrystalline cellulose, and sodium lauryl sulfate. The tablet coating includes FD&C blue #2, hypromellose, lactose monohydrate, titanium dioxide, and triacetin.
12. Tibsovo - Clinical Pharmacology
12.1 Mechanism of Action
Ivosidenib is a small molecule inhibitor that targets the mutant isocitrate dehydrogenase 1 (IDH1) enzyme. In patients with AML, susceptible IDH1 mutations are defined as those leading to increased levels of 2-hydroxyglutarate (2-HG) in the leukemia cells and where efficacy is predicted by 1) clinically meaningful remissions with the recommended dose of ivosidenib and/or 2) inhibition of mutant IDH1 enzymatic activity at concentrations of ivosidenib sustainable at the recommended dosage according to validated methods. The most common of such mutations in patients with AML are R132H and R132C substitutions.
Ivosidenib was shown to inhibit selected IDH1 R132 mutants at much lower concentrations than wild-type IDH1 in vitro. Inhibition of the mutant IDH1 enzyme by ivosidenib led to decreased 2-HG levels and induced myeloid differentiation in vitro and in vivo in mouse xenograft models of IDH1-mutated AML. In blood samples from patients with AML with mutated IDH1, ivosidenib decreased 2-HG levels ex-vivo, reduced blast counts, and increased percentages of mature myeloid cells.
In a patient-derived xenograft intra-hepatic cholangiocarcinoma mouse model with IDH1 R132C, ivosidenib reduced 2-HG levels.
12.2 Pharmacodynamics
Multiple doses of ivosidenib 500 mg daily were observed to decrease plasma 2-HG concentrations in patients with hematological malignancies and cholangiocarcinoma to levels similar to those observed at baseline in healthy subjects. In bone marrow of patients with hematological malignancies and in tumor biopsy of patients with cholangiocarcinoma, the mean [% coefficient of variation (%CV)] reduction in 2-HG concentrations were 93.1% (11.1%) and 82.2% (32.4%), respectively.
12.3 Pharmacokinetics
The AUC and Cmax of ivosidenib increase in a less than dose-proportional manner from 200 mg to 1,200 mg daily (0.4 to 2.4 times the approved recommended dosage). The following ivosidenib pharmacokinetic parameters (Table 10) were observed following administration of ivosidenib 500 mg as a single dose or daily dose (for steady state), unless otherwise specified. The steady-state pharmacokinetics of ivosidenib 500 mg were comparable between patients with newly diagnosed AML and relapsed or refractory AML and were lower in patients with cholangiocarcinoma.
| Cholangiocarcinoma treated with TIBSOVO | Relapsed or refractory AML treated with TIBSOVO | Newly diagnosed AML treated with a combination of TIBSOVO and azacitidine | |
|---|---|---|---|
|
|||
| PK parameters | |||
| Single dose Cmax (ng/mL)* | 4,060 (45%) | 4,503 (38%) | 4,820 (39%) |
| Steady state Cmax (ng/mL)* | 4,799 (33%) | 6,551 (44%) | 6,145 (34%) |
| Steady state AUC (ng∙hr/mL)* | 86,382 (34%) | 117,348 (50%) | 106,326 (41%) |
| Steady state PK | Within 14 days | ||
| Accumulation | |||
| Cmax | 1.2 | 1.5 | 1.2 |
| AUC | 1.5 | 1.9 | 1.6 |
| Absorption | |||
| Median Tmax (hr) | 2 | 3 | 2 |
| Effect of Food† | |||
| Cmax | 1.98-fold (90% CI: 1.79, 2.19) | ||
| AUC | 1.24-fold (90% CI: 1.16, 1.33) | ||
| Distribution | |||
| In vitro protein binding | 92 to 96% | ||
| Apparent volume of distribution at steady state (L)* | 706 (45%) | 403 (35%) | 504 (22%) |
| Elimination | |||
| Apparent clearance at steady state (L/hr)* | 6.1 (31%) | 5.6 (35%) | 4.6 (35%) |
| Terminal half-life at steady state (hr)* | 129 (102%) | 58 (42%) | 98 (42%) |
| Metabolism | |||
| Plasmac | >92% of total radioactivity as ivosidenib | ||
| Metabolic pathways | |||
| Major | CYP3A4 | ||
| Minor | N-dealkylation and hydrolytic pathways | ||
| Excretion‡ | |||
| Urine | 17% (10% as unchanged ivosidenib) | ||
| Feces | 77% (67% as unchanged ivosidenib) | ||
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies have not been conducted with ivosidenib. Ivosidenib was not mutagenic in an in vitro bacterial reverse mutation (Ames) assay. Ivosidenib was not clastogenic in an in vitro human lymphocyte micronucleus assay, or in an in vivo rat bone marrow micronucleus assay. Fertility studies in animals have not been conducted with ivosidenib. In repeat-dose toxicity studies up to 90 days in duration with twice daily oral administration of ivosidenib in rats, uterine atrophy was reported in females at non-tolerated dose levels.
14. Clinical Studies
14.1 Newly Diagnosed AML
Newly Diagnosed AML in Combination with Azacitidine
The efficacy of TIBSOVO was evaluated in a randomized (1:1), multicenter, double-blind, placebo-controlled clinical trial (Study AG120-C-009, NCT03173248) of 146 adult patients with newly-diagnosed AML with an IDH1 mutation who were 75 years or older, or had comorbidities that precluded the use of intensive induction chemotherapy based on at least one of the following criteria: baseline Eastern Cooperative Oncology Group (ECOG) performance status of 2, severe cardiac or pulmonary disease, hepatic impairment with bilirubin > 1.5 times the upper limit of normal, creatinine clearance < 45 mL/min, or other comorbidity. IDH1 mutations were confirmed centrally using the Abbott RealTime™ IDH1 Assay. Local diagnostic tests were permitted for screening and randomization provided a bone marrow or peripheral blood sample was sent for central confirmation. Gene mutation analysis to document IDH1 mutated disease from a bone marrow or peripheral blood sample was conducted for all patients. Patients were randomized to receive either TIBSOVO 500 mg or matched placebo orally once daily on Days 1-28 in combination with azacitidine 75 mg/m2/day either subcutaneously or intravenously on Days 1-7 or Days 1-5 and 8-9 of each 28-day cycle beginning on Cycle 1 Day 1. Patients were treated for a minimum of 6 cycles unless they experienced disease progression, unacceptable toxicity or undergoing hematopoietic stem cell transplantation. Baseline demographic and disease characteristics are shown in Table 11.
| Demographic and Disease Characteristics | TIBSOVO + azacitidine (500 mg daily) N=72 | Placebo + azacitidine N=74 |
|---|---|---|
| ECOG PS: Eastern Cooperative Oncology Group Performance Status; MPN = Myeloproliferative Neoplasm; MDS = Myelodysplastic syndrome | ||
|
||
| Demographics | ||
| Age (Years) Median (Min, Max) | 76 (58, 84) | 76 (45, 94) |
| Age Categories, n (%) | ||
| <65 years | 4 (6) | 4 (5) |
| ≥65 years to <75 years | 29 (40) | 27 (36) |
| ≥75 years | 39 (54) | 43 (58) |
| Sex, n (%) | ||
| Male | 42 (58) | 38 (51) |
| Female | 30 (42) | 36 (49) |
| Race, n (%) | ||
| Asian | 15 (21) | 19 (26) |
| White | 12 (17) | 12 (16) |
| Black or African American | 0 | 2 (3) |
| Other | 1 (1) | 1 (1) |
| Not provided | 44 (61) | 40 (54) |
| Disease Characteristics | ||
| ECOG PS, n (%) | ||
| 0 | 14 (19) | 10 (14) |
| 1 | 32 (44) | 40 (54) |
| 2 | 26 (36) | 24 (32) |
| IDH1 Mutation, n (%)* | ||
| R132C | 45 (63) | 51 (69) |
| R132H | 14 (19) | 12 (16) |
| R132G | 6 (8) | 4 (5) |
| R132L | 3 (4) | 0 |
| R132S | 2 (3) | 6 (8) |
| Wild type | 1 (1) | 0 |
| Missing | 1 (1) | 1 (1) |
| Cytogenetic risk status† n (%) | ||
| Favorable | 3 (4) | 7 (9) |
| Intermediate | 48 (67) | 44 (59) |
| Poor | 16 (22) | 20 (27) |
| Other | 3 (4) | 1 (1) |
| Missing | 2 (3) | 2 (3) |
| Transfusion Dependent at Baseline‡, n (%) | 39 (54) | 40 (54) |
| Type of AML, n (%) | ||
| De novo AML | 54 (75) | 53 (72) |
| Secondary AML | 18 (25) | 21 (28) |
| Therapy-related AML | 2 (3) | 1 (1) |
| MDS related | 10 (14) | 12 (16) |
| MPN related | 4 (6) | 8 (11) |
Efficacy was established on the basis of event-free survival (EFS), overall survival (OS), and rate and duration of complete remission (CR). EFS was defined as the time from randomization until treatment failure, relapse from remission, or death from any cause, whichever occurred first. Treatment failure was defined as failure to achieve CR by 24 weeks. The efficacy results are shown in Table 12 and Figure 1.
| Endpoint | TIBSOVO (500 mg daily) + azacitidine N=72 | Placebo + azacitidine N=74 |
|---|---|---|
| Abbreviations: EFS = Event free survival; CI: confidence interval; OS = Overall survival; CR = Complete remission; CRh = Complete remission with partial hematologic recovery; NE = Not estimable. | ||
| The 2-sided p-value boundaries for EFS, OS, CR, and CR+CRh are 0.0095, 0.0034, 0.0174, and 0.0174, respectively. | ||
|
||
| EFS, events (%) | 47 (65) | 62 (84) |
| Treatment Failure | 43 (60) | 59 (80) |
| Relapse | 3 (4) | 2 (3) |
| Death | 1 (1) | 1 (1) |
| Hazard ratio* (95% CI) | 0.35 (0.17, 0.72) | |
| p-value† | 0.0038 | |
| OS events (%) | 28 (39) | 46 (62) |
| Median OS (95% CI) months | 24.0 (11.3, 34.1) | 7.9 (4.1, 11.3) |
| Hazard ratio* (95% CI) | 0.44 (0.27, 0.73) | |
| p-value† | 0.0010 | |
| CR, n (%) | 34 (47) | 11 (15) |
| 95% CI‡ | (35, 59) | (8, 25) |
| Risk difference§ (95% CI), (%) | 31 (17, 46) | |
| p-value¶ | <0.0001 | |
| Median duration of CR (95% CI), months | NE (13.0, NE) | 11.2 (3.2, NE) |
| CR +CRh, n (%) | 37 (51) | 13 (18) |
| 95% CI‡ | (39, 63) | (10, 28) |
| Risk difference§ (95% CI), (%) | 33 (18, 47) | |
| p-value¶ | <0.0001 | |
| Median duration of CR + CRh (95% CI), months | NE (13.0, NE) | 9.2 (5.8, NE) |
Figure 1: Kaplan-Meier Curve for Overall Survival in AG120-C-009
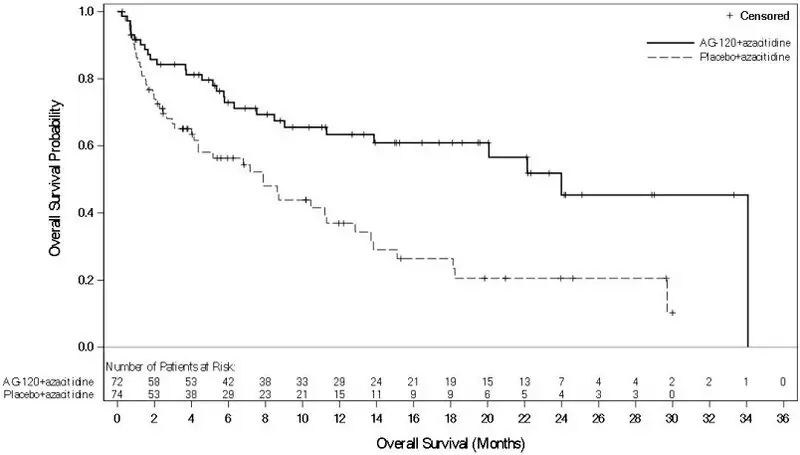
The median time to first CR for TIBSOVO with azacitidine was 4 months (range, 1.7 to 11.9 months).
The median time to first CR + CRh for TIBSOVO with azacitidine was 4 months (range, 1.7 to 11.9 months).
Monotherapy in Newly Diagnosed AML
The efficacy of TIBSOVO was evaluated in an open-label, single-arm, multicenter clinical trial (Study AG120-C-001, NCT02074839) that included 28 adult patients with newly diagnosed AML with an IDH1 mutation. IDH1 mutations were identified by a local or central diagnostic test and confirmed retrospectively using the Abbott RealTime™ IDH1 Assay. The cohort included patients who were age 75 years or older or who had comorbidities that precluded the use of intensive induction chemotherapy based on at least one of the following criteria: baseline ECOG performance status of ≥ 2, severe cardiac or pulmonary disease, hepatic impairment with bilirubin > 1.5 times the upper limit of normal, or creatinine clearance < 45 mL/min. TIBSOVO was given orally at a starting dose of 500 mg daily until disease progression, development of unacceptable toxicity, or undergoing hematopoietic stem cell transplantation. Two (7%) of the 28 patients went on to stem cell transplantation following TIBSOVO treatment.
The baseline demographic and disease characteristics are shown in Table 13.
| Demographic and Disease Characteristics | TIBSOVO (500 mg daily) N=28 |
|
|---|---|---|
| ECOG PS: Eastern Cooperative Oncology Group Performance Status. ELN: European Leukemia Net | ||
|
||
| Demographics | ||
| Age (Years) Median (Min, Max) | 77 (64, 87) | |
| Age Categories, n (%) | ||
| <65 years | 1 (4) | |
| ≥65 years to <75 years | 8 (29) | |
| ≥75 years | 19 (68) | |
| Sex, n (%) | ||
| Male | 15 (54) | |
| Female | 13 (46) | |
| Race, n (%) | ||
| White | 24 (86) | |
| Black or African American | 2 (7) | |
| Asian | 0 | |
| Native Hawaiian/Other Pacific Islander | 0 | |
| Other/Not provided | 2 (7) | |
| Disease Characteristics | ||
| ECOG PS, n (%) | ||
| 0 | 6 (21) | |
| 1 | 16 (57) | |
| 2 | 5 (18) | |
| 3 | 1 (4) | |
| IDH1 Mutation, n (%)* | ||
| R132C | 24 (86) | |
| R132G | 1 (4) | |
| R132H | 2 (7) | |
| R132L | 1 (4) | |
| R132S | 0 | |
| ELN Risk Category, n (%) | ||
| Favorable | 0 | |
| Intermediate | 9 (32) | |
| Adverse | 19 (68) | |
| Transfusion Dependent at Baseline†, n (%) | 17 (61) | |
| Type of AML, n (%) | ||
| De novo AML | 6 (21) | |
| AML-MRC‡ | 19 (68) | |
| Therapy-related AML | 3 (11) | |
| Prior Hypomethylating Agent for Antecedent | ||
| Hematologic Disorder | 13 (46) | |
Efficacy was established on the basis of the rate of complete remission (CR) or complete remission with partial hematologic recovery (CRh), the duration of CR+CRh, and the rate of conversion from transfusion dependence to transfusion independence. The efficacy results are shown in Table 14. The median follow-up was 8.1 months (range, 0.6 to 40.9 months) and median treatment duration was 4.3 months (range, 0.3 to 40.9 months).
| Endpoint | TIBSOVO (500 mg daily) N=28 |
|---|---|
| CI: confidence interval, NE: not estimable | |
|
|
| CR* n (%) | 8 (28.6) |
| 95% CI | (13.2, 48.7) |
| Median DOCR† (months) | NE‡ |
| 95% CI | (4.2, NE) |
| CRh§ n (%) | 4 (14.3) |
| 95% CI | (4.0, 32.7) |
| Observed DOCRh† (months) | 2.8, 4.6, 8.3, 15.7+ |
| CR+CRh n (%) | 12 (42.9) |
| 95% CI | (24.5, 62.8) |
| Median DOCR+CRh† (months) | NE‡ |
| 95% CI | (4.2, NE) |
For patients who achieved a CR or CRh, the median time to CR or CRh was 2.8 months (range, 1.9 to 12.9 months). Of the 12 patients who achieved a best response of CR or CRh, 11 (92%) achieved a first response of CR or CRh within 6 months of initiating TIBSOVO.
Among the 17 patients who were dependent on red blood cell (RBC) and/or platelet transfusions at baseline, 7 (41.2%) became independent of RBC and platelet transfusions during any 56-day post-baseline period. Of the 11 patients who were independent of both RBC and platelet transfusions at baseline, 6 (54.5%) remained transfusion independent during any 56-day post-baseline period.
14.2 Relapsed or Refractory AML
The efficacy of TIBSOVO was evaluated in an open-label, single-arm, multicenter clinical trial (Study AG120-C-001, NCT02074839) of 174 adult patients with relapsed or refractory AML with an IDH1 mutation. IDH1 mutations were identified by a local or central diagnostic test and confirmed retrospectively using the Abbott RealTime™ IDH1 Assay. TIBSOVO was given orally at a starting dose of 500 mg daily until disease progression, development of unacceptable toxicity, or undergoing hematopoietic stem cell transplantation. Twenty-one (12%) of the 174 patients went on to stem cell transplantation following TIBSOVO treatment.
The baseline demographic and disease characteristics are shown in Table 15.
| Demographic and Disease Characteristics | TIBSOVO (500 mg daily) N=174 |
|---|---|
| ECOG PS: Eastern Cooperative Oncology Group Performance Status. | |
|
|
| Demographics | |
| Age (Years) Median (Min, Max) | 67 (18, 87) |
| Age Categories, n (%) | |
| <65 years | 63 (36) |
| ≥65 years to <75 years | 71 (41) |
| ≥75 years | 40 (23) |
| Sex, n (%) | |
| Male | 88 (51) |
| Female | 86 (49) |
| Race, n (%) | |
| White | 108 (62) |
| Black or African American | 10 (6) |
| Asian | 6 (3) |
| Native Hawaiian/Other Pacific Islander | 1 (1) |
| Other/Not provided | 49 (28) |
| Disease Characteristics | |
| ECOG PS, n (%) | |
| 0 | 36 (21) |
| 1 | 97 (56) |
| 2 | 39 (22) |
| 3 | 2 (1) |
| IDH1 Mutation, n (%)* | |
| R132C | 102 (59) |
| R132H | 43 (25) |
| R132G | 12 (7) |
| R132S | 10 (6) |
| R132L | 7 (4) |
| Cytogenetic Risk Status, n (%) | |
| Intermediate | 104 (60) |
| Poor | 47 (27) |
| Missing/Unknown | 23 (13) |
| Relapse Type | |
| Primary refractory | 64 (37) |
| Refractory relapse | 45 (26) |
| Untreated relapse | 65 (37) |
| Relapse Number | |
| 0 | 64 (37) |
| 1 | 83 (48) |
| 2 | 21 (12) |
| ≥3 | 6 (3) |
| Prior Stem Cell Transplantation for AML, n (%) | 40 (23) |
| Transfusion Dependent at Baseline†, n (%) | 110 (63) |
| Median Number of Prior Therapies (Min, Max) | 2 (1, 6) |
| Type of AML, n (%) | |
| De novo AML | 116 (67) |
| Secondary AML | 58 (33) |
Efficacy was established on the basis of the rate of complete remission (CR) plus complete remission with partial hematologic recovery (CRh), the duration of CR+CRh, and the rate of conversion from transfusion dependence to transfusion independence. The efficacy results are shown in Table 16. The median follow-up was 8.3 months (range, 0.2 to 39.5 months) and median treatment duration was 4.1 months (range, 0.1 to 39.5 months).
| Endpoint | TIBSOVO (500 mg daily) N=174 |
|---|---|
| CI: confidence interval | |
|
|
| CR* n (%) | 43 (24.7) |
| 95% CI | (18.5, 31.8) |
| Median DOCR† (months) | 10.1 |
| 95% CI | (6.5, 22.2) |
| CRh‡ n (%) | 14 (8.0) |
| 95% CI | (4.5, 13.1) |
| Median DOCRh† (months) | 3.6 |
| 95% CI | (1, 5.5) |
| CR+CRh§ n (%) | 57 (32.8) |
| 95% CI | (25.8, 40.3) |
| Median DOCR+CRh† (months) | 8.2 |
| 95% CI | (5.6, 12) |
For patients who achieved a CR or CRh, the median time to CR or CRh was 2 months (range, 0.9 to 5.6 months). Of the 57 patients who achieved a best response of CR or CRh, all achieved a first response of CR or CRh within 6 months of initiating TIBSOVO.
Among the 110 patients who were dependent on red blood cell (RBC) and/or platelet transfusions at baseline, 41 (37.3%) became independent of RBC and platelet transfusions during any 56-day post-baseline period. Of the 64 patients who were independent of both RBC and platelet transfusions at baseline, 38 (59.4%) remained transfusion independent during any 56-day post-baseline period.
14.3 Locally Advanced or Metastatic Cholangiocarcinoma
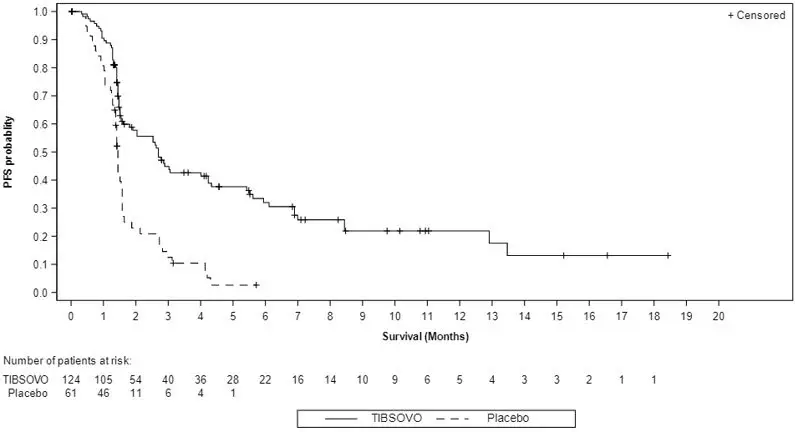
The efficacy of TIBSOVO was evaluated in a randomized (2:1), multicenter, double-blind, placebo-controlled clinical trial (Study AG120-C-005, NCT02989857) of 185 adult patients with locally advanced or metastatic cholangiocarcinoma with an IDH1 mutation whose disease had progressed following at least 1 but not more than 2 prior regimens, including at least one gemcitabine- or 5-FU-containing regimen. Patients were randomized to receive either TIBSOVO 500 mg orally once daily or matched placebo until disease progression or unacceptable toxicity. Randomization was stratified by number of prior therapies (1 or 2). Eligible patients who were randomized to placebo were allowed to cross over to receive TIBSOVO after documented radiographic disease progression. Patients with IDH1 mutations were selected using a central diagnostic next generation sequencing assay. Tumor imaging assessments were performed every 6 weeks for the first 8 assessments and every 8 weeks thereafter.
The major efficacy outcome measure was Progression Free Survival (PFS) as determined by independent review committee (IRC) according to Response Evaluation Criteria in Solid Tumors (RECIST) v1.1.
The median age was 62 years (range: 33 to 83); 63% were female; 57% were White, 12% Asian, 1.1% Black, 0.5% Native Hawaiian/Other Pacific Islander, 0.5% American Indian or Alaska Native, 28% race missing/not reported; and 37% had an ECOG performance status of 0 (37%) or 1 (62%). All patients received at least 1 prior line of systemic therapy and 47% received two prior lines. Most patients had intrahepatic cholangiocarcinoma (91%) at diagnosis and 92% had metastatic disease. Across both arms, 70% patients had an R132C mutation, 15% had an R132L mutation, 12% had an R132G mutation, 1.1% had an R132H mutation, and 1.6% had an R132S mutation.
The efficacy results are shown in Table 17 and Figure 2. The study demonstrated a statistically significant improvement in PFS.
| Endpoint | TIBSOVO (500 mg daily) | Placebo |
|---|---|---|
| IRC: Independent Review Committee; CI: Confidence Interval | ||
|
||
| Progression-Free Survival by IRC Assessment | N=124 | N=61 |
| Events, n (%) | 76 (61) | 50 (82) |
| Progressive Disease | 64 (52) | 44 (72) |
| Death | 12 (10) | 6 (10) |
| Hazard ratio (95% CI)* | 0.37 (0.25, 0.54) | |
| p-value† | <0.0001 | |
| Objective Response Rate, n (%) | 3 (2.4) | 0 |
| Overall Survival‡ | N=126 | N=61 |
| Deaths, n (%) | 100 (79) | 50 (82) |
| Hazard ratio (95% CI)* | 0.79 (0.56, 1.12) | |
| p-value† | 0.093 | |
Figure 2: Kaplan-Meier Plot of Progression-Free Survival per Independent Review Committee - Before Crossover (ITT)
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised: May 2022 | ||
| MEDICATION GUIDE
TIBSOVO® (tib-SOH-voh) (ivosidenib tablets) |
|||
|
What is the most important information I should know about TIBSOVO? |
|||
| TIBSOVO may cause serious side effects, including: | |||
|
|||
|
|
||
| If you develop signs and symptoms of differentiation syndrome, your healthcare provider may treat you with a corticosteroid medicine or a medicine called hydroxyurea and may monitor you in the hospital. | |||
| See "What are the possible side effects of TIBSOVO?" for more information about side effects. | |||
| What is TIBSOVO? | |||
| TIBSOVO is a prescription medicine used to treat: | |||
|
|||
| Your healthcare provider will perform a test to make sure that TIBSOVO is right for you. | |||
| It is not known if TIBSOVO is safe and effective in children. | |||
| Before taking TIBSOVO, tell your healthcare provider about all of your medical conditions, including if you: | |||
|
|||
| Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. | |||
| Especially tell your healthcare provider if you take hormonal contraceptives. TIBSOVO may affect how hormonal contraceptives work and may cause them to not work as well. | |||
| How should I take TIBSOVO? | |||
|
|||
| What are the possible side effects of TIBSOVO? | |||
| TIBSOVO may cause serious side effects, including: | |||
|
|||
|
|
||
| The most common side effects of TIBSOVO when used in combination with azacitidine or alone in adults with AML include: | |||
|
|
||
|
The most common side effects of TIBSOVO in adults with Cholangiocarcinoma include: |
|||
|
|
||
| Your healthcare provider will do blood tests before you start and during treatment with TIBSOVO. Your healthcare provider may decrease, temporarily hold, or permanently stop your treatment with TIBSOVO if you develop certain side effects. | |||
| TIBSOVO may cause fertility problems in females and males, which may affect your ability to have children. Talk to your healthcare provider if you have concerns about fertility. | |||
| These are not all of the possible side effects of TIBSOVO. | |||
| Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. | |||
| How should I store TIBSOVO? | |||
|
|||
| Keep TIBSOVO and all medicines out of the reach of children. | |||
| General information about the safe and effective use of TIBSOVO | |||
| Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not take TIBSOVO for conditions for which it was not prescribed. Do not give TIBSOVO to other people, even if they have the same symptoms you have. It may harm them. You can ask your pharmacist or healthcare provider for information about TIBSOVO that is written for healthcare professionals. | |||
| What are the ingredients in TIBSOVO? | |||
| Active ingredient: ivosidenib | |||
| Inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, hypromellose acetate succinate, magnesium stearate, microcrystalline cellulose, and sodium lauryl sulfate. The tablet coating includes FD&C blue #2, hypromellose, lactose monohydrate, titanium dioxide, and triacetin. | |||
| Manufactured for Servier Pharmaceuticals LLC, Boston, MA 02210 | |||
| Servier and the Servier logo are trademarks of Les Laboratoires Servier. TIBSOVO® is a registered trademark of Servier Pharmaceuticals LLC, a wholly owned, indirect subsidiary of Les Laboratoires Servier. | |||
| © 2021, 2022 Servier Pharmaceuticals LLC | |||
| For more information go to www.TIBSOVO.com or call 1-800-807-6124. | |||
| TIBSOVO
ivosidenib tablet, film coated |
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
| Labeler - Servier Pharmaceutical LLC (116608503) |





