Drug Detail:Troxyca er (Naltrexone hydrochloride and oxycodone hydrochloride)
Drug Class: Narcotic analgesic combinations
Highlights of Prescribing Information
TROXYCA® ER (oxycodone hydrochloride and naltrexone hydrochloride) extended-release capsules, for oral use, CII
Initial U.S. Approval: 2016
WARNING: ADDICTION, ABUSE, AND MISUSE; LIFE-THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL INGESTION; NEONATAL OPIOID WITHDRAWAL SYNDROME; and CYTOCHROME P450 3A4 INTERACTION
See full prescribing information for complete boxed warning.
- TROXYCA ER exposes users to risks of addiction, abuse, and misuse, which can lead to overdose and death. Assess patient's risk before prescribing, and monitor regularly for these behaviors and conditions. (5.1)
- Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely, especially upon initiation or following a dose increase. Instruct patients to swallow TROXYCA ER capsules whole to avoid exposure to a potentially fatal dose of oxycodone. (5.2)
- Accidental ingestion of TROXYCA ER, especially by children, can result in fatal overdose of oxycodone. (5.2)
- Prolonged use of TROXYCA ER during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated. If prolonged opioid use is required in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. (5.3)
- Concomitant use with CYP3A4 inhibitors (or discontinuation of CYP3A4 inducers) can result in fatal overdose of oxycodone from TROXYCA ER. (5.4)
Indications and Usage for Troxyca ER
TROXYCA ER is a combination opioid agonist/opioid antagonist product indicated for the management of pain severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate. (1)
Limitations of Use
- Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, and because of the greater risks of overdose and death with extended-release opioid formulations, reserve TROXYCA ER for use in patients for whom alternative treatment options (e.g., non-opioid analgesics or immediate-release opioids) are ineffective, not tolerated, or would be otherwise inadequate to provide sufficient management of pain. (1)
- TROXYCA ER is not indicated as an as-needed (prn) analgesic. (1)
Troxyca ER Dosage and Administration
- To be prescribed only by healthcare providers knowledgeable in use of potent opioids for management of chronic pain. (2.1)
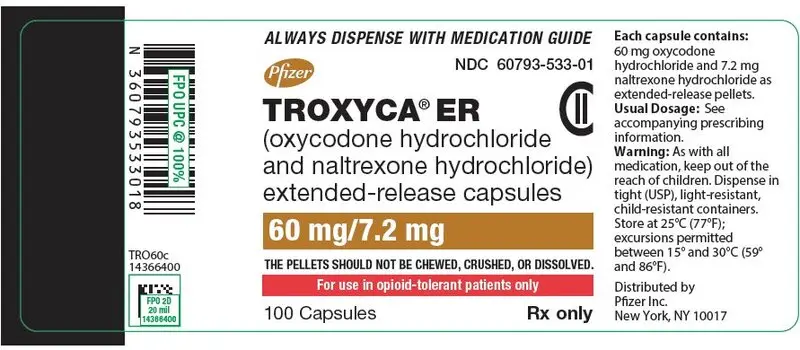
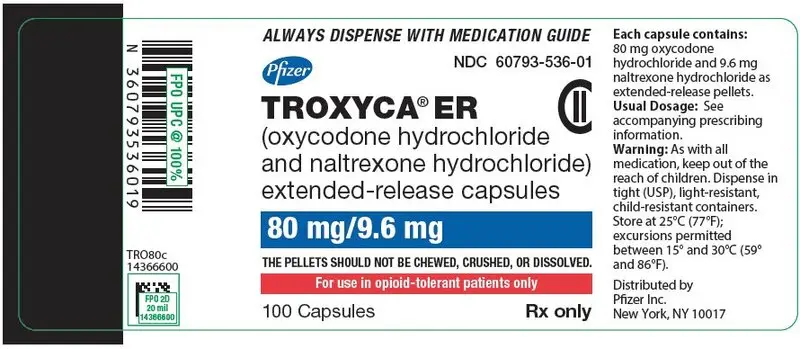
- TROXYCA ER 60 mg/7.2 mg and 80 mg/9.6 mg capsules, single doses of TROXYCA ER greater than 40 mg/4.8 mg, or a total daily dose greater than 80 mg/9.6 mg are only for use in patients in whom tolerance to an opioid of comparable potency has been established. (2.1)
- Patients considered opioid-tolerant are those taking, for one week or longer, at least 60 mg oral morphine per day, 25 mcg transdermal fentanyl per hour, 30 mg oral oxycodone per day, 8 mg oral hydromorphone per day, 25 mg oral oxymorphone per day, 60 mg oral hydrocodone per day, or an equianalgesic dose of another opioid. (2.1)
- Use the lowest effective dose for the shortest duration consistent with individual patient treatment goals. (2.1)
- Individualize dosing based on the severity of pain, patient response, prior analgesic experience, and risk factors for addiction, abuse, and misuse. (2.1)
- Instruct patients to swallow TROXYCA ER capsules intact, or to sprinkle the capsule contents on applesauce and immediately swallow without chewing. (2.1, 2.5)
- Instruct patients not to crush, chew, or dissolve the pellets in the capsule to avoid the risk of release and absorption of a potentially fatal dose of oxycodone and to avoid release of sequestered naltrexone that could precipitate opioid withdrawal. (2.1, 2.5, 5.1)
- For opioid-naïve and opioid non-tolerant patients, initiate with the 10 mg/1.2 mg capsule every 12 hours. (2.1, 2.2)
- Do not abruptly discontinue TROXYCA ER. (2.4, 5.12)
Dosage Forms and Strengths
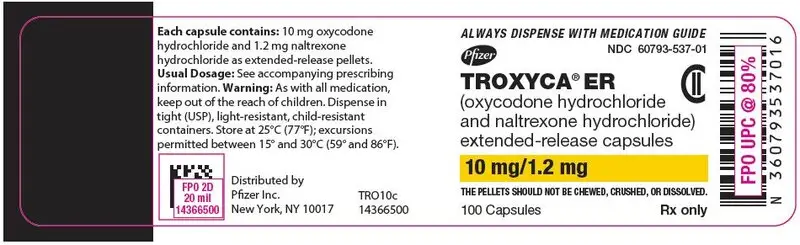
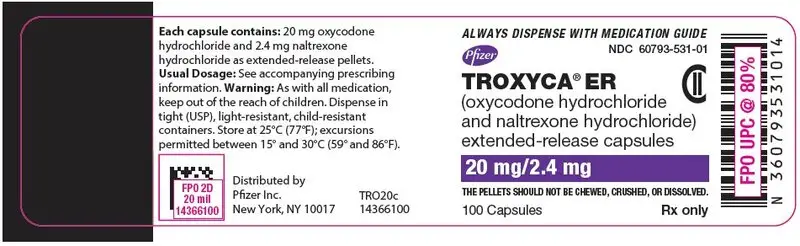
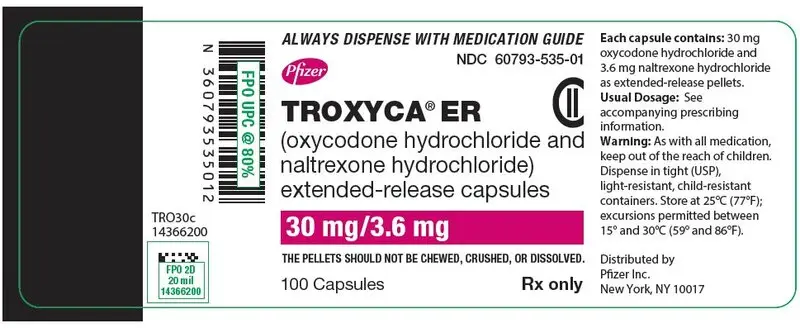
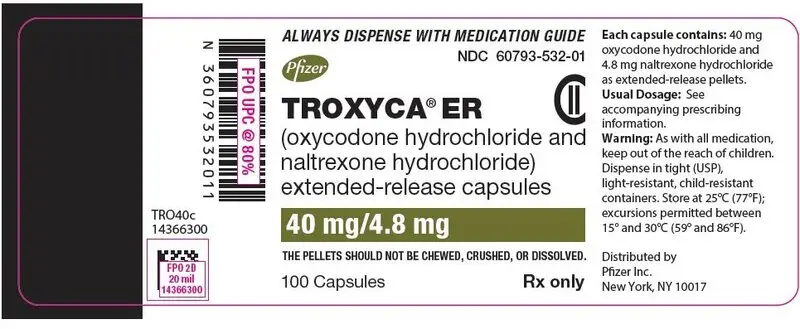
Extended-release capsules (oxycodone hydrochloride/naltrexone hydrochloride): 10 mg/1.2 mg, 20 mg/2.4 mg, 30 mg/3.6 mg, 40 mg/4.8 mg, 60 mg/7.2 mg and 80 mg/9.6 mg. (3)
Contraindications
- Significant respiratory depression (4)
- Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment (4)
- Known or suspected gastrointestinal obstruction, including paralytic ileus (4)
- Hypersensitivity to oxycodone or naltrexone (4)
Warnings and Precautions
- Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients: Monitor closely, particularly during initiation and titration. (5.6)
- Adrenal Insufficiency: If diagnosed, treat with physiologic replacement of corticosteroids, and wean patient off of the opioid. (5.7)
- Severe Hypotension: Monitor during dosage initiation and titration. Avoid use of TROXYCA ER in patients with circulatory shock. (5.8)
- Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness: Monitor for sedation and respiratory depression. Avoid use of TROXYCA ER in patients with impaired consciousness or coma. (5.9)
Adverse Reactions/Side Effects
Most common adverse reactions: nausea, constipation, vomiting, headache, and somnolence. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Pfizer Inc. at 1-800-438-1985 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- CNS Depressants: Concomitant use may cause hypotension, profound sedation, respiratory depression, coma, and death. If coadministration is required, consider dose reduction of one or both drugs because of additive pharmacological effects and monitor closely. (5.5, 7)
- Serotonergic Drugs: Concomitant use may result in serotonin syndrome. Discontinue TROXYCA ER if serotonin syndrome is suspected. (7)
- Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics: Avoid use with TROXYCA ER because they may reduce analgesic effect of TROXYCA ER or precipitate withdrawal symptoms. (7)
- Monoamine Oxidase Inhibitors (MAOIs): Avoid TROXYCA ER in patients taking MAOIs or within 14 days of stopping such treatment. (7)
Use In Specific Populations
- Pregnancy: May cause fetal harm. (5.3, 8.1)
- Lactation: Not recommended. (8.2)
- Geriatric patients: Start at the low end of the dosing range and monitor closely for respiratory depression. (5.6, 8.5)
- Hepatic Impairment: Monitor patients closely for CNS or respiratory depression and for signs of withdrawal. (8.6, 12.3)
- Renal Impairment: Monitor patients closely for CNS or respiratory depression and for signs of withdrawal. (8.7, 12.3)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 8/2016
Related/similar drugs
aspirin, acetaminophen, tramadol, naproxen, oxycodone, TylenolFull Prescribing Information
WARNING: ADDICTION, ABUSE, AND MISUSE; LIFE-THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL INGESTION; NEONATAL OPIOID WITHDRAWAL SYNDROME; and CYTOCHROME P450 3A4 INTERACTION.
Addiction, Abuse, and Misuse
TROXYCA ER exposes patients and other users to the risks of opioid addiction, abuse, and misuse, which can lead to overdose and death. Assess each patient's risk prior to prescribing TROXYCA ER, and monitor all patients regularly for the development of these behaviors and conditions [see Warnings and Precautions (5.1)].
1. Indications and Usage for Troxyca ER
TROXYCA ER is indicated for the management of pain severe enough to require daily, around-the-clock, long-term opioid treatment and for which alternative treatment options are inadequate.
2. Troxyca ER Dosage and Administration
2.1 Important Dosage and Administration Instructions
TROXYCA ER should be prescribed only by healthcare professionals who are knowledgeable in the use of potent opioids for the management of chronic pain.
TROXYCA ER 60 mg/7.2 mg and 80 mg/9.6 mg capsules, single doses of TROXYCA ER greater than 40 mg/4.8 mg, or a total daily dose greater than 80 mg/9.6 mg are only for use in patients in whom tolerance to an opioid of comparable potency has been established. Patients who are opioid-tolerant are those receiving, for one week or longer, at least 60 mg oral morphine per day, 25 mcg transdermal fentanyl per hour, 30 mg oral oxycodone per day, 8 mg oral hydromorphone per day, 25 mg oral oxymorphone per day, 60 mg oral hydrocodone per day, or an equianalgesic dose of another opioid.
- Use the lowest effective dosage for the shortest duration consistent with individual patient treatment goals [see Warnings and Precautions (5)].
- Initiate the dosing regimen for each patient individually; taking into account the patient's severity of pain, patient response, prior analgesic treatment experience, and risk factors for addiction, abuse, and misuse [see Warnings and Precautions (5.1)].
- Monitor patients closely for respiratory depression, especially within the first 24–72 hours of initiating therapy and following dosage increases with TROXYCA ER and adjust the dosage accordingly [see Warnings and Precautions (5.2)].
Instruct patients to swallow TROXYCA ER capsules whole [see Patient Counseling Information (17)]. Crushing, chewing, or dissolving the pellets in TROXYCA ER capsules will result in uncontrolled delivery of oxycodone and can lead to overdose or death [see Warnings and Precautions (5.1)].
Instruct patients who are unable to swallow TROXYCA ER capsules to sprinkle the capsule contents on applesauce and immediately swallow without chewing [see Dosage and Administration (2.5)].
Administer TROXYCA ER orally every 12 hours.
2.3 Titration and Maintenance of Therapy
Individually titrate TROXYCA ER to a dosage that provides adequate analgesia and minimizes adverse reactions. Continually reevaluate patients receiving TROXYCA ER to assess the maintenance of pain control and the relative incidence of adverse reactions, as well as monitoring for the development of addiction, abuse, or misuse [see Warnings and Precautions (5.1)]. Frequent communication is important among the prescriber, other members of the healthcare team, the patient, and the caregiver/family during periods of changing analgesic requirements, including initial titration. During chronic therapy, periodically reassess the continued need for opioid analgesics.
Patients who experience breakthrough pain may require a dosage increase of TROXYCA ER, or may need rescue medication with an appropriate dose of an immediate-release analgesic. If the level of pain increases after dose stabilization, attempt to identify the source of increased pain before increasing the TROXYCA ER dosage. Because steady-state plasma concentrations are achieved within 48 hours, the total daily dose of TROXYCA ER may be adjusted by 20 mg/2.4 mg every 2 to 3 days as needed based on efficacy, safety, and tolerability.
If unacceptable opioid-related adverse reactions are observed, consider reducing the dosage. Adjust the dosage to obtain an appropriate balance between management of pain and opioid-related adverse reactions.
There are no well-controlled clinical studies evaluating the safety and efficacy with dosing more frequently than every 12 hours.
2.4 Discontinuation of TROXYCA ER
When a patient no longer requires therapy with TROXYCA ER, taper the dose gradually, by 25% to 50% every 2 to 4 days, while monitoring carefully for signs and symptoms of withdrawal. If the patient develops these signs or symptoms, raise the dose to the previous level and taper more slowly, either by increasing the interval between decreases, decreasing the amount of change in dose, or both. Do not abruptly discontinue TROXYCA ER [see Warnings and Precautions (5.12), Drug Abuse and Dependence (9.3)].
2.5 Administration of TROXYCA ER
Instruct patients to swallow TROXYCA ER capsules intact. The capsules contain pellets that consist of oxycodone HCl and sequestered naltrexone HCl. The pellets in the capsules are not to be manipulated, i.e., crushed, dissolved, or chewed due to the risk of rapid release and absorption of a potentially fatal dose of oxycodone [see Warnings and Precautions (5.1)]. Consuming TROXYCA ER capsules that have been altered by crushing, dissolving, or chewing the pellets can release sufficient naltrexone to precipitate withdrawal in opioid-dependent individuals [see Warnings and Precautions (5.12)].
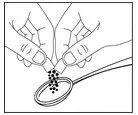
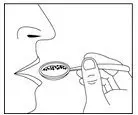
Alternatively, the contents of the TROXYCA ER capsules (pellets) may be sprinkled over applesauce and then swallowed. This method is appropriate only for patients able to reliably swallow the applesauce without chewing. Other foods have not been tested and should not be substituted for applesauce. Instruct the patient to:
- Open the capsule.
- Sprinkle the pellets onto a small amount of applesauce and swallow immediately without chewing.
- Rinse the mouth to ensure all pellets have been swallowed.
- Discard the empty capsule shell after the contents have been sprinkled on applesauce.
Do not administer TROXYCA ER pellets through a nasogastric or gastric tube.
3. Dosage Forms and Strengths
TROXYCA ER is available in 6 strengths as an extended-release hard gelatin capsule filled with common pellets as noted below:
| Strength (oxycodone hydrochloride/naltrexone hydrochloride) | Description |
|---|---|
| 10 mg/1.2 mg | Hard gelatin capsule, silver opaque body with "NTO 10" printed in black ink, yellow opaque cap with "Pfizer" printed in black ink |
| 20 mg/2.4 mg | Hard gelatin capsule, silver opaque body with "NTO 20" printed in black ink, violet opaque cap with "Pfizer" printed in white ink |
| 30 mg/3.6 mg | Hard gelatin capsule, silver opaque body with "NTO 30" printed in black ink, fuchsia opaque cap with "Pfizer" printed in black ink |
| 40 mg/4.8 mg | Hard gelatin capsule, silver opaque body with "NTO 40" printed in black ink, olive green opaque cap with "Pfizer" printed in black ink |
| 60 mg/7.2 mg | Hard gelatin capsule, silver opaque body with "NTO 60" printed in black ink, green opaque cap with "Pfizer" printed in black ink |
| 80 mg/9.6 mg | Hard gelatin capsule, silver opaque body with "NTO 80" printed in black ink, brick red opaque cap with "Pfizer" printed in black ink |
4. Contraindications
TROXYCA ER is contraindicated in patients with:
- Significant respiratory depression [see Warnings and Precautions (5.2)]
- Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment [see Warnings and Precautions (5.6)]
- Known or suspected gastrointestinal obstruction, including paralytic ileus [see Warnings and Precautions (5.10)]
- Hypersensitivity (e.g., anaphylaxis) to oxycodone or naltrexone or any other components of the TROXYCA ER formulation [see Adverse Reactions (6.1)]
5. Warnings and Precautions
5.1 Addiction, Abuse, and Misuse
TROXYCA ER contains oxycodone, a Schedule II controlled substance. As an opioid, TROXYCA ER exposes users to the risks of addiction, abuse, and misuse [see Drug Abuse and Dependence (9)]. As extended-release products such as TROXYCA ER deliver the opioid over an extended period of time, there is a greater risk for overdose and death due to the larger amount of oxycodone present [see Drug Abuse and Dependence (9)].
Although the risk of addiction in any individual is unknown, it can occur in patients appropriately prescribed TROXYCA ER and in those who obtain the drug illicitly. Addiction can occur at recommended dosages and if the drug is misused or abused.
Assess each patient's risk for opioid addiction, abuse, or misuse prior to prescribing TROXYCA ER, and monitor all patients receiving TROXYCA ER for the development of these behaviors or conditions. Risks are increased in patients with a personal or family history of substance abuse (including drug or alcohol addiction or abuse) or mental illness (e.g., major depression). The potential for these risks should not, however, prevent the proper management of pain in any given patient. Patients at increased risk may be prescribed opioids such as TROXYCA ER, but use in such patients necessitates intensive counseling about the risks and proper use of TROXYCA ER along with intensive monitoring for signs of addiction, abuse, and misuse.
Abuse or misuse of TROXYCA ER by cutting, breaking, chewing, crushing, or dissolving the pellets in TROXYCA ER and then swallowing, snorting or injecting will result in the uncontrolled delivery of the oxycodone and can result in overdose and death [see Overdosage (10)]. Misuse or abuse of TROXYCA ER by these methods may also release sufficient naltrexone to precipitate withdrawal in opioid-dependent individuals [see Warnings and Precautions (5.12)].
Opioids are sought by drug abusers and people with addiction disorders and are subject to criminal diversion. Consider these risks when prescribing or dispensing TROXYCA ER. Strategies to reduce these risks include prescribing the drug in the smallest appropriate quantity and advising the patient on the proper disposal of unused drug [see Patient Counseling Information (17)]. Contact the local state professional licensing board or state controlled substances authority for information on how to prevent and detect abuse or diversion of this product.
5.2 Life-Threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression has been reported with the use of opioids, even when used as recommended. Respiratory depression, if not immediately recognized and treated, may lead to respiratory arrest and death. Management of respiratory depression may include close observation, supportive measures, and use of opioid antagonists, depending on the patient's clinical status [see Overdosage (10)]. Carbon dioxide (CO2) retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids.
While serious, life-threatening, or fatal respiratory depression can occur at any time during the use of TROXYCA ER, the risk is greatest during the initiation of therapy or following a dosage increase. Monitor patients closely for respiratory depression, especially within the first 24–72 hours of initiating therapy with and following dosage increases of TROXYCA ER.
To reduce the risk of respiratory depression, proper dosing and titration of TROXYCA ER are essential [see Dosage and Administration (2)]. Overestimating the TROXYCA ER dosage when converting patients from another opioid product can result in fatal overdose with the first dose.
Accidental ingestion of even one dose of TROXYCA ER, especially by children, can result in respiratory depression and death due to an overdose of oxycodone.
5.3 Neonatal Opioid Withdrawal Syndrome
Prolonged use of TROXYCA ER during pregnancy can result in withdrawal in the neonate. Neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. Observe newborns for signs of neonatal opioid withdrawal syndrome and manage accordingly. Advise pregnant women using opioids for a prolonged period of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available [see Use in Specific Populations (8.1), Patient Counseling Information (17)].
5.4 Risks of Concomitant Use or Discontinuation of Cytochrome P450 3A4 Inhibitors and Inducers
Concomitant use of TROXYCA ER with a CYP3A4 inhibitors, such as macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g., ketoconazole), and protease inhibitors (e.g., ritonavir), may increase plasma concentrations of oxycodone and prolong opioid adverse reactions, which may cause potentially fatal respiratory depression [see Warnings and Precautions (5.2)], particularly when an inhibitor is added after a stable dose of TROXYCA ER is achieved. Similarly, discontinuation of a CYP3A4 inducer, such as rifampin, carbamazepine, and phenytoin, in TROXYCA ER-treated patients may increase oxycodone plasma concentrations and prolong opioid adverse reactions. When using TROXYCA ER with CYP3A4 inhibitors or discontinuing CYP3A4 inducers in TROXYCA ER-treated patients, monitor patients closely at frequent intervals and consider dosage reduction of TROXYCA ER until stable drug effects are achieved [see Drug Interactions (7)].
Concomitant use of TROXYCA ER with CYP3A4 inducers or discontinuation of an CYP3A4 inhibitor could decrease oxycodone plasma concentrations, decrease opioid efficacy or, possibly, lead to a withdrawal syndrome in a patient who had developed physical dependence to oxycodone. When using TROXYCA ER with CYP3A4 inducers or discontinuing CYP3A4 inhibitors, monitor patients closely at frequent intervals and consider increasing the opioid dosage if needed to maintain adequate analgesia or if symptoms of opioid withdrawal occur [see Drug Interactions (7)].
5.5 Risks Due to Interactions with Central Nervous System Depressants
Hypotension, profound sedation, respiratory depression, coma, and death may result if TROXYCA ER is used concomitantly with alcohol or other central nervous system (CNS) depressants (e.g., benzodiazepines and other sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, and other opioids).
When considering the use of TROXYCA ER in a patient taking a CNS depressant, assess the duration of use of the CNS depressant and the patient's response, including the degree of tolerance that has developed to CNS depression. Additionally, evaluate the patient's use of alcohol or illicit drugs that cause CNS depression. If the decision to begin TROXYCA ER is made, start with a lower dosage of TROXYCA ER, monitor patients for signs of respiratory depression, sedation, and hypotension, and consider using a lower dose of the concomitant CNS depressant [see Drug Interactions (7)].
5.6 Life-Threatening Respiratory Depression in Patients with Chronic Pulmonary Disease or in Elderly, Cachectic, or Debilitated Patients
The use of TROXYCA ER in patients with acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment is contraindicated.
5.7 Adrenal Insufficiency
Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use. Presentation of adrenal insufficiency may include non-specific symptoms and signs including nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. If adrenal insufficiency is suspected, confirm the diagnosis with diagnostic testing as soon as possible. If adrenal insufficiency is diagnosed, treat with physiologic replacement doses of corticosteroids. Wean the patient off of the opioid to allow adrenal function to recover and continue corticosteroid treatment until adrenal function recovers. Other opioids may be tried as some cases reported use of a different opioid without recurrence of adrenal insufficiency. The information available does not identify any particular opioids as being more likely to be associated with adrenal insufficiency.
5.8 Severe Hypotension
TROXYCA ER may cause severe hypotension including orthostatic hypotension and syncope in ambulatory patients. There is an increased risk in patients whose ability to maintain blood pressure has already been compromised by a reduced blood volume or concurrent administration of certain CNS depressant drugs (e.g., phenothiazines or general anesthetics) [see Drug Interactions (7)]. Monitor these patients for signs of hypotension after initiating or titrating the dosage of TROXYCA ER. In patients with circulatory shock, TROXYCA ER may cause vasodilation that can further reduce cardiac output and blood pressure. Avoid the use of TROXYCA ER in patients with circulatory shock.
5.9 Risks of Use in Patients with Increased Intracranial Pressure, Brain Tumors, Head Injury, or Impaired Consciousness
In patients who may be susceptible to the intracranial effects of CO2 retention (e.g., those with evidence of increased intracranial pressure or brain tumors), TROXYCA ER may reduce respiratory drive, and the resultant CO2 retention can further increase intracranial pressure. Monitor such patients for signs of sedation and respiratory depression, particularly when initiating therapy with TROXYCA ER.
Opioids may also obscure the clinical course in a patient with a head injury. Avoid the use of TROXYCA ER in patients with impaired consciousness or coma.
5.10 Risks of Use in Patients with Gastrointestinal Conditions
TROXYCA ER is contraindicated in patients with gastrointestinal obstruction, including paralytic ileus.
The oxycodone in TROXYCA ER may cause spasm of the sphincter of Oddi. Opioids may cause increases in serum amylase. Monitor patients with biliary tract disease, including acute pancreatitis, for worsening symptoms.
5.11 Increased Risk of Seizures in Patients with Seizure Disorders
The oxycodone in TROXYCA ER may increase the frequency of seizures in patients with seizure disorders and may increase the risk of seizures in other clinical settings associated with seizures. Monitor patients with a history of seizure disorders for worsened seizure control during TROXYCA ER therapy.
5.12 Withdrawal
Avoid the use of mixed agonist/antagonist (e.g., pentazocine, nalbuphine, and butorphanol) or partial agonist (e.g., buprenorphine) analgesics in patients who have received or are receiving a course of therapy with a full opioid agonist analgesic, including TROXYCA ER. In these patients, mixed agonists/antagonist and partial agonist analgesics may reduce the analgesic effect and/or may precipitate withdrawal symptoms.
Consuming TROXYCA ER that has been altered by crushing, chewing, or dissolving the pellets can release sufficient naltrexone to precipitate withdrawal in opioid-dependent individuals. Symptoms of withdrawal usually appear within five minutes of ingestion of naltrexone, can last for up to 48 hours, and can include mental status changes, restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Significant fluid losses from vomiting and diarrhea can require intravenous fluid administration.
When discontinuing TROXYCA ER, gradually taper the dosage [see Dosage and Administration (2.4)]. Do not abruptly discontinue TROXYCA ER [see Drug Abuse and Dependence (9.3)].
5.13 Risks of Driving and Operating Machinery
TROXYCA ER may impair the mental or physical abilities needed to perform potentially hazardous activities such as driving a car or operating machinery. Warn patients not to drive or operate dangerous machinery unless they are tolerant to the effects of TROXYCA ER and know how they will react to the medication [see Patient Counseling Information (17)].
5.14 Laboratory Tests and Monitoring
Naltrexone does not interfere with thin-layer, gas-liquid, or high pressure liquid chromatographic methods which may be used for the separation and detection of morphine, methadone, oxycodone, or quinine in the urine. Naltrexone may or may not interfere with enzymatic methods for the detection of opioids depending on the sensitivity and specificity of the test. Consult the test manufacturer for details.
Not every urine drug test for "opioids" or "opiates" detects oxycodone reliably, especially those designed for in-office use. Further, many laboratories will report urine drug concentrations below a specified "cut-off" value as "negative". Therefore, if urine testing for oxycodone is considered in the clinical management of an individual patient, ensure that the sensitivity and specificity of the assay is appropriate, and consider the limitations of the testing used when interpreting results.
6. Adverse Reactions/Side Effects
The following serious adverse reactions are discussed elsewhere in the labeling:
- Addiction, Abuse, and Misuse [see Warnings and Precautions (5.1)]
- Life-Threatening Respiratory Depression [see Warnings and Precautions (5.2)]
- Neonatal Opioid Withdrawal Syndrome [see Warnings and Precautions (5.3)]
- Interactions with CNS Depressants [see Warnings and Precautions (5.5)]
- Adrenal Insufficiency [see Warnings and Precautions (5.7)]
- Severe Hypotension [see Warnings and Precautions (5.8)]
- Gastrointestinal Adverse Reactions [see Warnings and Precautions (5.10)]
- Seizures [see Warnings and Precautions (5.11)]
- Withdrawal [see Warnings and Precautions (5.12)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared with rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In controlled and uncontrolled studies, the most common adverse reactions were nausea, constipation, vomiting, headache, and somnolence. The most common adverse reactions leading to discontinuation (≥1% in any of the treatment phases) were nausea, constipation, vomiting, somnolence, headache, fatigue, and dizziness.
In a randomized, placebo-controlled, double-blind study in subjects with moderate-to-severe chronic low back pain, 410 subjects received TROXYCA ER. This study utilized an enriched enrollment with a randomized withdrawal design in which subjects were titrated to effect on open-label TROXYCA ER for up to 42 days. Once their pain was controlled, 280 subjects were randomized to and received active treatment with TROXYCA ER (146 subjects) or were tapered off TROXYCA ER using a double-dummy design and treated with placebo (134 subjects) for 12 weeks.
Adverse reactions reported in ≥2% of subjects receiving TROXYCA ER in either the titration phase or maintenance phase of the placebo-controlled study are presented in Table 2.
| System Organ Class | Open-Label Titration Phase TROXYCA ER (N=410) | Double-Blind Maintenance Phase TROXYCA ER (N=146) | Double-Blind Maintenance Phase Placebo (N=134) |
|---|---|---|---|
| Adverse Drug Reaction (ADR) | n (%) | n (%) | n (%) |
| Gastrointestinal disorders | |||
|
|||
| Abdominal pain* | 12 ( 2.9) | 2 ( 1.4) | 8 ( 6.0) |
| Constipation | 61 (14.9) | 5 ( 3.4) | 3 ( 2.2) |
| Diarrhea | 9 ( 2.2) | 8 ( 5.5) | 6 ( 4.5) |
| Dry mouth | 13 ( 3.2) | 0 | 0 |
| Nausea | 84 (20.5) | 21 (14.4) | 5 ( 3.7) |
| Vomiting | 37 ( 9.0) | 9 ( 6.2) | 4 ( 3.0) |
| General disorders and administration site conditions | |||
| Drug withdrawal syndrome† | 4 ( 1.0) | 4 ( 2.7) | 2 (1.5) |
| Fatigue | 13 ( 3.2) | 5 ( 3.4) | 1 ( 0.7) |
| Edema peripheral | 3 ( 0.7) | 3 ( 2.1) | 1 ( 0.7) |
| Musculoskeletal and connective tissue disorders | |||
| Arthralgia | 3 ( 0.7) | 3 ( 2.1) | 1 ( 0.7) |
| Back pain | 5 ( 1.2) | 3 ( 2.1) | 8 ( 6.0) |
| Muscle spasms | 1 ( 0.2) | 4 ( 2.7) | 1 ( 0.7) |
| Nervous system disorders | |||
| Dizziness | 24 ( 5.9) | 6 ( 4.1) | 1 ( 0.7) |
| Headache | 30 ( 7.3) | 2 ( 1.4) | 7 ( 5.2) |
| Hypoesthesia | 0 | 3 ( 2.1) | 0 |
| Somnolence‡ | 37 ( 9.0) | 1 ( 0.7) | 1 ( 0.7) |
| Psychiatric disorders | |||
| Insomnia | 8 ( 2.0) | 1 ( 0.7) | 1 ( 0.7) |
| Respiratory, thoracic and mediastinal disorders | |||
| Oropharyngeal pain | 1 ( 0.2) | 4 ( 2.7) | 1 ( 0.7) |
| Skin and subcutaneous tissue disorders | |||
| Hyperhidrosis§ | 10 ( 2.4) | 4 ( 2.7) | 1 ( 0.7) |
| Pruritus¶ | 27 ( 6.6) | 3 ( 2.1) | 0 |
| Vascular disorders | |||
| Hot flush# | 10 ( 2.4) | 2 ( 1.4) | 3 ( 2.2) |
An additional 395 subjects received at least one dose of TROXYCA ER in an open-label, 12-month safety study of subjects with moderate-to-severe chronic non-cancer pain. In this study, 193 subjects received TROXYCA ER for at least 6 months and 105 subjects received TROXYCA ER for approximately 12 months.
Adverse reactions reported in ≥2% of subjects of the 12-month open-label safety study are presented in Table 3.
| System Organ Class | TROXYCA ER (N=395) |
|---|---|
| Adverse Drug Reaction (ADR) | n (%) |
| Gastrointestinal disorders | |
|
|
| Abdominal pain* | 33 ( 8.4) |
| Constipation | 84 (21.3) |
| Diarrhea | 36 ( 9.1) |
| Dry mouth | 9 ( 2.3) |
| Nausea | 100 (25.3) |
| Vomiting | 55 (13.9) |
| General disorders and administration site conditions | |
| Fatigue | 36 ( 9.1) |
| Edema peripheral | 15 ( 3.8) |
| Musculoskeletal and connective tissue disorders | |
| Arthralgia | 13 ( 3.3) |
| Back pain | 25 ( 6.3) |
| Muscle spasms | 9 ( 2.3) |
| Nervous system disorders | |
| Dizziness | 34 ( 8.6) |
| Headache | 46 (11.6) |
| Somnolence† | 38 ( 9.6) |
| Tremor | 8 ( 2.0) |
| Psychiatric disorders | |
| Depression | 13 ( 3.3) |
| Insomnia | 20 ( 5.1) |
| Restlessness | 9 ( 2.3) |
| Respiratory, thoracic and mediastinal disorders | |
| Cough | 10 ( 2.5) |
| Oropharyngeal pain | 9 ( 2.3) |
| Skin and subcutaneous tissue disorders | |
| Hyperhidrosis‡ | 27 ( 6.8) |
| Pruritus§ | 22 ( 5.6) |
| Vascular disorders | |
| Hot flush¶ | 17 ( 4.3) |
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of oxycodone. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Serotonin syndrome: Cases of serotonin syndrome, a potentially life-threatening condition, have been reported during concomitant use of opioids with serotonergic drugs.
Adrenal insufficiency: Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use.
Anaphylaxis and pharyngeal edema: Anaphylaxis and pharyngeal edema have been reported with ingredients contained in TROXYCA ER.
Androgen deficiency: Cases of androgen deficiency have occurred with chronic use of opioids [see Clinical Pharmacology (12.2)].
Myocardial ischemia and ventricular fibrillation: Myocardial ischemia and ventricular fibrillation have been reported with oxycodone overdose.
7. Drug Interactions
Table 5 includes clinically significant drug interactions with TROXYCA ER.
| Inhibitors of CYP3A4 and CYP2D6 | |
|---|---|
| Clinical Impact: | The concomitant use of TROXYCA ER and CYP3A4 inhibitors can increase the plasma concentration of oxycodone, resulting in increased or prolonged opioid effects. These effects could be more pronounced with concomitant use of TROXYCA ER and CYP2D6 and CYP3A4 inhibitors, particularly when an inhibitor is added after stable dose of TROXYCA ER is achieved [see Warnings and Precautions (5.4)]. After stopping a CYP3A4 inhibitor, as the effects of the inhibitor decline, the oxycodone plasma concentration will decrease [see Clinical Pharmacology (12.3)], resulting in decreased opioid efficacy or a withdrawal syndrome in patients who had developed physical dependence to oxycodone. |
| Intervention: | If concomitant use is necessary, consider dosage reduction of TROXYCA ER until stable drug effects are achieved. Monitor patients for respiratory depression and sedation at frequent intervals. If a CYP3A4 inhibitor is discontinued, consider increasing the TROXYCA ER dosage until stable drug effects are achieved. Monitor for signs of opioid withdrawal. |
| Examples: | Macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g., ketoconazole), protease inhibitors (e.g., ritonavir) |
| CYP3A4 Inducers | |
| Clinical Impact: | The concomitant use of TROXYCA ER and CYP3A4 inducers can decrease the plasma concentration of oxycodone [see Clinical Pharmacology (12.3)], resulting in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence to oxycodone [see Warnings and Precautions (5.4)].
After stopping a CYP3A4 inducer, as the effects of the inducer decline, the oxycodone plasma concentration will increase [see Clinical Pharmacology (12.3)], which could increase or prolong both the therapeutic effects and adverse reactions, and may cause serious respiratory depression. |
| Intervention: | If concomitant use is necessary, consider increasing the TROXYCA ER dosage until stable drug effects are achieved. Monitor for signs of opioid withdrawal. If a CYP3A4 inducer is discontinued, consider TROXYCA ER dosage reduction and monitor for signs of respiratory depression. |
| Examples: | Rifampin, carbamazepine, phenytoin |
| Central Nervous System (CNS) Depressants | |
| Clinical Impact: | Due to additive pharmacologic effects, the concomitant use of CNS depressants can increase the risk of hypotension, respiratory depression, profound sedation, coma, and death. |
| Intervention: | Consider dose reduction of one or both drugs. Monitor patients for signs of respiratory depression, sedation, and hypotension [see Warnings and Precautions (5.2)]. |
| Examples | Alcohol, benzodiazepines, and other sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, other opioids. |
| Serotonergic Drugs | |
| Clinical Impact: | The concomitant use of opioids with other drugs that affect the serotonergic neurotransmitter system has resulted in serotonin syndrome. |
| Intervention: | If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation and dose adjustment. Discontinue TROXYCA ER if serotonin syndrome is suspected. |
| Examples: | Selective serotonin reuptake inhibitors (SSRIs), serotonin and norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), triptans, 5-HT3 receptor antagonists, drugs that effect the serotonin neurotransmitter system (e.g., mirtazapine, trazodone, tramadol), monoamine oxidase (MAO) inhibitors (those intended to treat psychiatric disorders and also others, such as linezolid and intravenous methylene blue). |
| Mixed Agonist/Antagonist and Partial Agonist Opioid Analgesics | |
| Clinical Impact: | May reduce the analgesic effect of TROXYCA ER and/or precipitate withdrawal symptoms. |
| Intervention: | Avoid concomitant use. |
| Examples: | butorphanol, nalbuphine, pentazocine, buprenorphine |
| Muscle Relaxants | |
| Clinical Impact: | Oxycodone may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression. |
| Intervention: | Monitor patients for signs of respiratory depression that may be greater than otherwise expected and decrease the dosage of TROXYCA ER and/or the muscle relaxant, as necessary. |
| Monoamine Oxidase Inhibitors (MAOIs) | |
| Clinical Impact: | The concomitant use of MAOIs can potentiate the effects of oxycodone and can increase the risk of anxiety, confusion, hypotension, respiratory depression, profound sedation, coma, and death. |
| Intervention: | Avoid concomitant use in patients receiving MAOIs or within 14 days of stopping treatment with an MAOI. |
| Diuretics | |
| Clinical Impact: | Opioids can reduce the efficacy of diuretics by inducing the release of antidiuretic hormone. |
| Intervention: | Monitor patients for signs of diminished diuresis and/or effects on blood pressure and increase the dosage of the diuretic as needed. |
| Anticholinergic Drugs | |
| Clinical Impact: | The concomitant use of anticholinergic drugs may increase risk of urinary retention and/or severe constipation, which may lead to paralytic ileus. |
| Intervention: | Monitor patients for signs of urinary retention or reduced gastric motility when TROXYCA ER is used concomitantly with anticholinergic drugs. |
8. Use In Specific Populations
8.4 Pediatric Use
The safety and efficacy of TROXYCA ER in patients less than 18 years of age have not been established.
8.5 Geriatric Use
The pharmacokinetics of TROXYCA ER have not been investigated in elderly patients (≥65 years) although such patients were included in clinical studies. Clinical studies with TROXYCA ER did not include sufficient numbers of subjects aged 65 and older to determine if they respond differently than younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients.
Elderly patients (aged 65 years or older) may have increased sensitivity to oxycodone. In general, use caution when selecting a dosage for an elderly patient, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, concomitant disease, and use of other drug therapy.
Respiratory depression is the chief risk for elderly patients treated with opioids, and has occurred after large initial doses were administered to patients who were not opioid-tolerant or when opioids were co-administered with other agents that depress respiration. Titrate the dosage of TROXYCA ER slowly in geriatric patients [see Warnings and Precautions (5.6)].
This drug is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function.
8.6 Hepatic Impairment
Since oxycodone is extensively metabolized in the liver, its clearance may decrease in patients with hepatic impairment. Naltrexone is sequestered in the TROXYCA ER capsules and is not intended to be released when TROXYCA ER is used as directed. However, measurable naltrexone plasma concentrations have been observed in some patients in clinical trials with TROXYCA ER [see Clinical Pharmacology (12.3)]. An increase in naltrexone AUC in patients with compensated and decompensated liver cirrhosis, compared with subjects with normal liver function, has been reported [see Clinical Pharmacology (12.3)]. These data also suggest that alterations in naltrexone bioavailability are related to liver disease severity.
Dose initiation of TROXYCA ER should follow a conservative approach in patients with hepatic impairment. In patients with hepatic impairment, there is a potential for differential increase in naltrexone exposure compared to oxycodone exposure. Hence, when administering TROXYCA ER to patients with hepatic impairment, monitor patients closely for signs of central nervous system or respiratory depression due to elevated levels of oxycodone and for signs of withdrawal due to elevated levels of naltrexone and adjust the dose based on the clinical response.
8.7 Renal Impairment
Elimination of oxycodone is reported to be impaired in patients with renal impairment.
Although naltrexone is sequestered in the TROXYCA ER formulations, measurable naltrexone plasma concentrations have been observed in some patients in clinical trials with TROXYCA ER [see Clinical Pharmacology (12.3)]. Since naltrexone and its primary metabolite are excreted primarily in urine, their plasma concentrations may be increased in patients with renal impairment.
Dose initiation of TROXYCA ER should follow a conservative approach in patients with renal impairment. In patients with renal impairment, there is a potential for differential increase in naltrexone exposure compared to oxycodone exposure. Hence, when administering TROXYCA ER to patients with renal impairment, monitor patients closely for signs of central nervous system or respiratory depression due to elevated levels of oxycodone and for signs of withdrawal due to elevated levels of naltrexone and adjust the dose based on the clinical response.
8.8 Sex Differences
There are no clinically significant differences in oxycodone pharmacokinetics following oral administration of TROXYCA ER to males or females; therefore, no specific dosage adjustment is recommended for the initiation or maintenance of TROXYCA ER doses based on the sex of the patient [see Clinical Pharmacology (12.3)].
9. Drug Abuse and Dependence
9.2 Abuse
TROXYCA ER contains oxycodone, a substance with a high potential for abuse similar to other opioids including fentanyl, hydrocodone, hydromorphone, methadone, morphine, oxymorphone, and tapentadol. TROXYCA ER can be abused and is subject to misuse, addiction, and criminal diversion [see Warnings and Precautions (5.1)].
The high drug content in extended-release formulations adds to the risk of adverse outcomes from abuse and misuse.
All patients treated with opioids require careful monitoring for signs of abuse and addiction, since use of opioid analgesic products carries the risk of addiction even under appropriate medical use.
Prescription drug abuse is the intentional non-therapeutic use of a prescription drug, even once, for its rewarding psychological or physiological effects.
Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that develop after repeated substance use and includes: a strong desire to take the drug, difficulties in controlling its use, persisting in its use despite harmful consequences, a higher priority given to drug use than to other activities and obligations, increased tolerance, and sometimes a physical withdrawal.
"Drug-seeking" behavior is very common to persons with substance use disorders. Drug-seeking tactics include emergency calls or visits near the end of office hours, refusal to undergo appropriate examination, testing, or referral, repeated "loss" of prescriptions, tampering with prescriptions and reluctance to provide prior medical records or contact information for other healthcare provider(s). "Doctor shopping" (visiting multiple prescribers to obtain additional prescriptions) is common among drug abusers and people suffering from untreated addiction. Preoccupation with achieving adequate pain relief can be appropriate behavior in a patient with poor pain control.
Abuse and addiction are separate and distinct from physical dependence and tolerance. Healthcare providers should be aware that addiction may not be accompanied by concurrent tolerance and symptoms of physical dependence in all persons with substance use disorders. In addition, abuse of opioids can occur in the absence of true addiction.
TROXYCA ER, like other opioids, can be diverted for non-medical use into illicit channels of distribution. Careful record-keeping of prescribing information, including quantity, frequency, and renewal requests, as required by state and federal law, is strongly advised.
Proper assessment of the patient, proper prescribing practices, periodic re-evaluation of therapy, and proper dispensing and storage are appropriate measures that help to limit abuse of opioid drugs.
9.3 Dependence
Both tolerance and physical dependence can develop during chronic opioid therapy. Tolerance is the need for increasing doses of opioids to maintain a defined effect such as analgesia (in the absence of disease progression or other external factors). Tolerance may occur to both the desired and undesired effects of drugs, and may develop at different rates for different effects.
Physical dependence results in withdrawal symptoms after abrupt discontinuation or a significant dosage reduction of a drug. Withdrawal also may be precipitated through the administration of drugs with opioid antagonist activity (e.g., naloxone, nalmefene), mixed agonist/antagonist analgesics (e.g., pentazocine, butorphanol, nalbuphine), or partial agonists (e.g., buprenorphine).
Physical dependence may not occur to a clinically significant degree until after several days to weeks of continued opioid usage.
TROXYCA ER should not be abruptly discontinued [see Dosage and Administration (2.4)]. If TROXYCA ER is abruptly discontinued in a physically-dependent patient, a withdrawal syndrome may occur. Some or all of the following can characterize this syndrome: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other signs and symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, increased blood pressure, respiratory rate, or heart rate.
Infants born to mothers physically dependent on opioids will also be physically dependent and may exhibit respiratory difficulties and withdrawal signs [see Use in Specific Populations (8.1)].
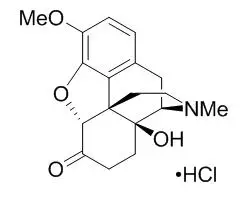
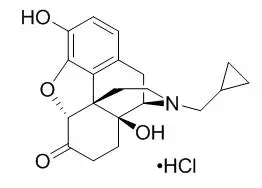
11. Troxyca ER Description
TROXYCA ER extended-release capsules contain pellets of oxycodone HCl with naltrexone HCl at a ratio of 100:12 in each capsule strength for oral administration. The capsule strength describes the amount of oxycodone HCl/naltrexone HCl per capsule. Oxycodone HCl is an opioid agonist and naltrexone HCl is an opioid antagonist at the mu-opioid receptor.
TROXYCA ER extended-release capsules contain the following inactive ingredients common to all strengths: talc, ammonio methacrylate copolymer, sugar spheres, ethylcellulose, hydroxypropyl cellulose, polyethylene glycol, dibutyl sebacate, sodium lauryl sulfate, diethyl phthalate, magnesium stearate, methacrylic acid copolymer, and ascorbic acid. Each TROXYCA ER capsule (as a component of the capsule shell) also contains gelatin, titanium dioxide, E172 Black Iron Oxide, E172 Yellow Iron Oxide, and black ink.
The 10 mg/1.2 mg capsule does not contain additional excipient other than those listed above.
The 20 mg/2.4 mg capsule also contains FD&C Red #3, FD&C Blue #1, white ink.
The 30 mg/3.6 mg capsule also contains FD&C Blue #1, FD&C Red #3.
The 40 mg/4.8 mg capsule also contains FD&C Blue #1, FD&C Yellow #5, FD&C Yellow #6.
The 60 mg/7.2 mg capsule also contains FD&C Blue #1, FD&C Yellow #5, FD&C Yellow #6.
The 80 mg/9.6 mg capsule also contains FD&C Blue #1, FD&C Red #3, FD&C Yellow #6.
12. Troxyca ER - Clinical Pharmacology
12.3 Pharmacokinetics
The analgesic activity of TROXYCA ER is primarily due to the parent drug oxycodone. TROXYCA ER is designed to provide delivery of oxycodone over 12 hours.
Chewing, crushing or dissolving the pellets within the TROXYCA ER capsules impairs the extended-release delivery mechanism and results in the rapid release and absorption of a potentially fatal dose of oxycodone as well as a potentially complete release of sequestered naltrexone.
Oxycodone Pharmacokinetics
Oxycodone is a semi-synthetic narcotic with multiple actions qualitatively similar to those of morphine; the most prominent of these is mediated by the mu-opioid receptor and involves the central nervous system and organs composed of smooth muscle.
Naltrexone Pharmacokinetics
Naltrexone blocks the effects of opioids by competitive binding at mu-opioid receptors. Naltrexone has few, if any intrinsic actions besides its opioid-blocking properties. However, it does produce some pupillary constriction by an unknown mechanism. Naltrexone, administered alone, is not associated with the development of tolerance or dependence, but it will precipitate withdrawal symptoms in subjects physically dependent on opioids.
14. Clinical Studies
The analgesic efficacy of TROXYCA ER has been evaluated in one randomized, double-blind, placebo-controlled clinical trial in patients with moderate-to-severe chronic low back pain. This study utilized an enriched-enrollment, randomized-withdrawal design and was conducted in a population consisting of both opioid-experienced and opioid-naïve subjects. Subjects were titrated to effect with TROXYCA ER in the open-label period, which was followed by a 12-week double-blind treatment period. Total daily doses of the oxycodone in TROXYCA ER ranged from 20 mg to 160 mg administered in two equal doses approximately 12 hours apart. Subjects with controlled pain (defined as pain intensity numerical rating scale [NRS] ≤4) were randomized into the 12-week double-blind treatment period to either continue TROXYCA ER or be switched to placebo. Subjects randomized to placebo were given a blinded taper of TROXYCA ER according to a pre-specified schedule to prevent opioid withdrawal. Rescue medication (up to 3 grams per day of acetaminophen) was allowed throughout the study to treat episodes of breakthrough pain. Immediate-release oxycodone HCl (as a single ingredient product) was also allowed during the first 3 weeks of the open-label period to manage the initial conversion from prior therapy.
A total of 410 subjects entered the open-label titration period and 281 were successfully titrated onto TROXYCA ER and randomized into the double-blind treatment period: 134 to placebo and 147 to TROXYCA ER. Of these, 42.5% of subjects were previously treated with an opioid.
In the open-label titration period, 57% of subjects were female and 43% were male with the majority of subjects being less than 65 years of age (89%) and white (73%). Overall, in the double-blind treatment period, 56% of subjects were female and 44% were male with a median age of 51 years and the majority (73%) of subjects being white. Subject demographics were similar between placebo and TROXYCA ER groups.
A total of 188 (67%) subjects completed the double-blind treatment period, including 107 (73%) TROXYCA ER subjects and 81 (60%) placebo subjects. More subjects in the placebo group discontinued due to lack of efficacy (12%) compared to TROXYCA ER (3%), and more subjects discontinued due to adverse events in the TROXYCA ER group (10%) compared to placebo (7%). Subjects discontinued from the open-label titration period for the following reasons: adverse events (n=57), protocol violations (n=7), lost to follow-up (n=10), did not meet entrance criteria (n=41), no longer willing to participate (n=11), and other (n=3). Subjects discontinued from the double-blind treatment period from the placebo group for the following reasons: insufficient clinical response (n=16), adverse event (n=9), protocol violation (n=8), lost to follow-up (n=3), no longer willing to participate (n=11), and other (n=6) and from the TROXYCA ER group for the following reasons: insufficient clinical response (n=4), adverse event (n=14), protocol violation (n=9), lost to follow-up (n=6), no longer willing to participate (n=6), and other (n=1).
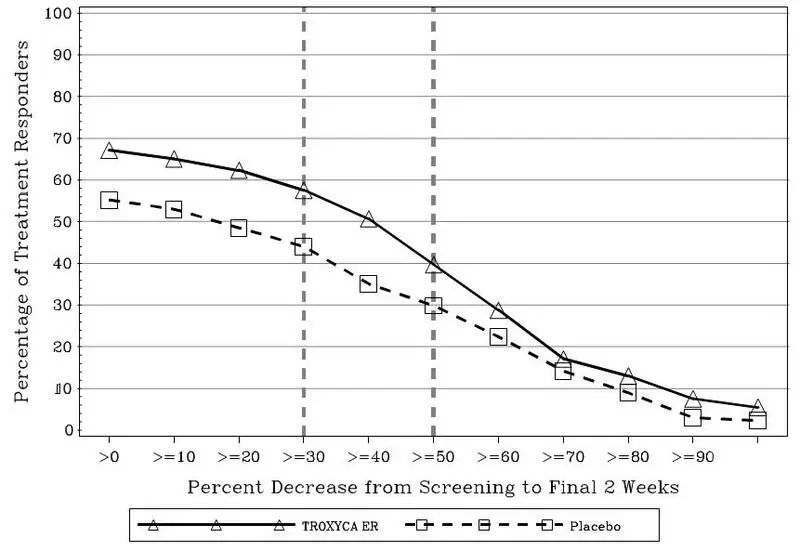
The mean change in the weekly average pain intensity NRS scores from randomization baseline to the average of Weeks 11 and 12 was statistically significantly superior for those treated with TROXYCA ER compared to placebo. The percentage of patients (responders) in each group who demonstrated improvement in their final 2 weeks, as compared with screening is shown in Figure 1. The figure is cumulative, so that patients whose change from screening is, for example, 30%, are also included at every level of improvement below 30%. Patients who did not complete the study were classified as non-responders. A higher percentage of subjects receiving TROXYCA ER, compared to placebo, had a ≥30% decrease in their weekly average NRS-pain intensity scores from Screening to Weeks 11 and 12 of the double-blind treatment period (58% versus 44% for TROXYCA ER and placebo, respectively), while, 40% of subjects receiving TROXYCA ER and 30% of subjects receiving placebo had a 50% decrease.
Figure 1. Percent Reduction Profiles for Weekly Average Daily Pain Scores from Screening to Final 2 Weeks
16. How is Troxyca ER supplied
| Oxycodone HCl / naltrexone HCl | TROXYCA ER 10 mg/1.2 mg | TROXYCA ER 20 mg/2.4 mg | TROXYCA ER 30 mg/3.6 mg | TROXYCA ER 40 mg/4.8 mg | TROXYCA ER 60 mg/7.2 mg | TROXYCA ER 80 mg/9.6 mg |
|---|---|---|---|---|---|---|
| Extended-Release Capsule Description | Two-toned hard gelatin capsule, silver opaque body, yellow opaque cap, black print | Two-toned hard gelatin capsule, silver opaque body, violet opaque cap, black print on body and white print on cap | Two-toned hard gelatin capsule, silver opaque body, fuchsia opaque cap, black print | Two-toned hard gelatin capsule, silver opaque body, olive green opaque cap, black print | Two-toned hard gelatin capsule, silver opaque body, green opaque cap, black print | Two-toned hard gelatin capsule, silver opaque body, brick red opaque cap, black print |
| NDC # | 60793-537-01 | 60793-531-01 | 60793-535-01 | 60793-532-01 | 60793-533-01 | 60793-536-01 |
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide and Instructions for Use).
Instructions For UseTROXYCA® ER (TROKS' ih-ka ee' ahr)(oxycodone hydrochloride and naltrexone hydrochloride) extended-release capsules, CII
- If you cannot swallow TROXYCA ER capsules whole, tell your healthcare provider. If your healthcare provider tells you that you can take TROXYCA ER by sprinkling the capsule contents on applesauce, follow these steps:
TROXYCA ER can be opened and the contents inside the capsule can be sprinkled on applesauce, as follows:
|
|
|
|
|
|
|
- Do not give TROXYCA ER through a nasogastric tube or gastric tube (stomach tube).
| TROXYCA ER
oxycodone hydrochloride and naltrexone hydrochloride capsule, extended release |
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||
| TROXYCA ER
oxycodone hydrochloride and naltrexone hydrochloride capsule, extended release |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| TROXYCA ER
oxycodone hydrochloride and naltrexone hydrochloride capsule, extended release |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| TROXYCA ER
oxycodone hydrochloride and naltrexone hydrochloride capsule, extended release |
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
| TROXYCA ER
oxycodone hydrochloride and naltrexone hydrochloride capsule, extended release |
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
| TROXYCA ER
oxycodone hydrochloride and naltrexone hydrochloride capsule, extended release |
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||
| Labeler - Pfizer Laboratories Div Pfizer Inc (134489525) |