Drug Detail:Tussigon (Homatropine and hydrocodone [ hom-a-troe-peen-and-hye-dro-koe-done ])
Drug Class: Upper respiratory combinations
Highlights of Prescribing Information
TUSSIGON (hydrocodone bitartrate and homatropine methylbromide) tablets, for oral administration, CII
Initial U.S. Approval: 1943
WARNING: ADDICTION, ABUSE, AND MISUSE; LIFE-THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL INGESTION; MEDICATION ERRORS; CYTOCHROME P450 3A4 INTERACTION; CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS; INTERACTION WITH ALCOHOL; NEONATAL OPIOID WITHDRAWAL SYNDROME
See full prescribing information for complete boxed warning.
- TUSSIGON exposes users to risks of addiction, abuse, and misuse, which can lead to overdose and death. Assess patient's risk before prescribing and monitor closely for these behaviors and conditions. (5.1)
- Serious, life-threatening, or fatal respiratory depression may occur. Monitor closely, especially upon initiation or when used in patients at higher risk. (5.2)
- Accidental ingestion of TUSSIGON, especially by children, can result in a fatal overdose of hydrocodone. (5.2)
- Ensure accuracy when prescribing, dispensing, and administering TUSSIGON. Dosing errors can result in accidental overdose and death. (2,1, 5.5)
- Concomitant use with CYP3A4 inhibitors (or discontinuation of CYP3A4 inducers) can result in a fatal overdose of hydrocodone. Avoid the use of TUSSIGON in patients taking CYP3A4 inhibitors or inducers. (5.7, 7.2, 7.3)
- Concomitant use of opioids with benzodiazepines or other central nervous system (CNS) depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Avoid the use of TUSSIGON in patients taking benzodiazepines, other CNS depressants, or alcohol. (5.8, 7.4)
- Instruct patients not to consume alcohol or any products containing alcohol while taking TUSSIGON because co-ingestion can result in fatal plasma hydrocodone levels. (5.8, 7.1)
- TUSSIGON is not recommended for use in pregnant women. Prolonged use of TUSSIGON during pregnancy can result in neonatal opioid withdrawal syndrome, which may be life-threatening if not recognized and treated. If TUSSIGON is used for a prolonged period in a pregnant woman, advise the patient of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available. (5.13, 8.1)
Recent Major Changes
| Boxed Warning | 2/2018 |
| Indications and Usage (1) | 2/2018 |
| Dosage and Administration (2.1, 2.3) | 2/2018 |
| Dosage and Administration, Children under 18 years (2.2) | Removed 6/2018 |
| Contraindications (4) | 2/2018 |
| Warnings and Precautions (5.1, 5.2, 5.4, 5.5, 5.6, 5.7, 5.8, 5.9, 5.11, 5.12, 5.13, 5.14, 5.15) | 2/2018 |
| Warnings and Precautions (5.3) | 4/2018 |
Indications and Usage for Tussigon
TUSSIGON is a combination of hydrocodone, an opioid agonist, and homatropine, a muscarinic antagonist, indicated for the symptomatic relief of cough in patients 18 years of age and older. (1)
Important Limitations of Use (1)
- Not indicated for pediatric patients under 18 years of age.
- Because of the risks of addiction, abuse, and misuse with opioids, even at recommended doses, reserve TUSSIGON for use in adult patients for whom the benefits of cough suppression are expected to outweigh the risks, and in whom an adequate assessment of the etiology of the cough has been made.
Tussigon Dosage and Administration
- Adults 18 years of age and older: One (1) tablet every 4 to 6 hours as needed; not to exceed six (6) tablets in 24 hours. (2.2)
- Do not increase the dose or dosing frequency. (2.1)
- Prescribe for the shortest duration consistent with treatment goals. (2.3)
- Reevaluate patients with unresponsive cough in 5 days or sooner for possible underlying pathology. (2.3)
- Reevaluate patient prior to refilling. (2.3)
Dosage Forms and Strengths
Tablets: Each tablet contains hydrocodone bitartrate 5 mg and homatropine methylbromide 1.5 mg. (3)
Contraindications
- Children younger than 6 years of age. (4)
- Significant respiratory depression. (4)
- Acute or severe bronchial asthma in an unmonitored setting or in absence of resuscitative equipment. (4)
- Known or suspected gastrointestinal obstruction, including paralytic ileus. (4)
- Hypersensitivity to hydrocodone, homatropine, or any of the inactive ingredients in TUSSIGON. (4)
Warnings and Precautions
See Boxed WARNINGS
- Life-threatening respiratory depression in patients with chronic pulmonary disease or in elderly, cachectic, or debilitated patients: Monitor closely, particularly during initiation of therapy. (5.4)
- Activities requiring mental alertness: Avoid engaging in hazardous tasks requiring mental alertness such as driving or operating machinery. (5.6)
- Risks of use in patients with head injury, impaired consciousness, increased intracranial pressure, or brain tumors: Avoid use. May increase intracranial pressure and obscure the clinical course of head injuries. (5.10)
- Seizures in patients with seizure disorders: Monitor during therapy. (5.11)
- Severe hypotension: Monitor during initiation of therapy. Avoid use in patients with circulatory shock. (5.12)
- Adrenal insufficiency: If diagnosed, treat with physiologic replacement of corticosteroids, and wean patient off of the opioid. (5.14)
Adverse Reactions/Side Effects
Common adverse reactions include: Sedation (somnolence, mental clouding, lethargy), impaired mental and physical performance, lightheadedness, dizziness, headache, dry mouth, nausea, vomiting, and constipation. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Pfizer, Inc. at 1-800-438-1985 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Serotonergic Drugs: Concomitant use may result in serotonin syndrome. Discontinue if serotonin syndrome is suspected. (7.5)
- Monoamine Oxidase Inhibitors (MAOIs): Can potentiate the effects of hydrocodone. Avoid concomitant use in patients receiving MAOIs or within 14 days of stopping an MAOI. (7.6)
- Muscle Relaxants: Avoid concomitant use. (7.7)
- Diuretics: Hydrocodone may reduce the efficacy of diuretics. Monitor for reduced effect. (7.8)
- Anticholinergic drugs: Concurrent use may cause paralytic ileus. (5.9, 7.9)
Use In Specific Populations
- Pregnancy: Avoid use in pregnant women. May cause fetal harm. (8.1)
- Lactation: Breast-feeding not recommended. (8.2)
- Renal Impairment: Use with caution in patients with severe renal impairment. (8.6)
- Hepatic Impairment: Use with caution in patients with severe hepatic impairment. (8.7)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 6/2018
Full Prescribing Information
WARNING: ADDICTION, ABUSE, AND MISUSE; LIFE-THREATENING RESPIRATORY DEPRESSION; ACCIDENTAL INGESTION; MEDICATION ERRORS; CYTOCHROME P450 3A4 INTERACTION; CONCOMITANT USE WITH BENZODIAZEPINES OR OTHER CNS DEPRESSANTS; INTERACTION WITH ALCOHOL; NEONATAL OPIOID WITHDRAWAL SYNDROME
1. Indications and Usage for Tussigon
TUSSIGON is indicated for the symptomatic relief of cough in patients 18 years of age and older.
2. Tussigon Dosage and Administration
2.1 Important Dosage and Administration Instructions
Administer TUSSIGON by the oral route only.
Advise patients not to increase the dose or dosing frequency of TUSSIGON because serious adverse events such as respiratory depression may occur with overdosage [see Warnings and Precautions (5.2), Overdosage (10)]. The dosage of TUSSIGON should not be increased if cough fails to respond; an unresponsive cough should be reevaluated for possible underlying pathology [see Dosage and Administration (2.3), Warnings and Precautions (5.4)].
2.2 Recommended Dosage
Adults 18 years of age and older: One (1) tablet every 4 to 6 hours as needed; not to exceed six (6) tablets in 24 hours.
2.3 Monitoring, Maintenance, and Discontinuation of Therapy
Prescribe TUSSIGON for the shortest duration that is consistent with individual patient treatment goals [see Warnings and Precautions (5.1)].
Monitor patients closely for respiratory depression, especially within the first 24–72 hours of initiating therapy [see Warnings and Precautions (5.2)].
Reevaluate patients with unresponsive cough in 5 days or sooner for possible underlying pathology, such as foreign body or lower respiratory tract disease [see Warnings and Precautions (5.4)]. If a patient requires a refill, reevaluate the cause of the cough and assess the need for continued treatment with TUSSIGON, the relative incidence of adverse reactions, and the development of addiction, abuse, or misuse [see Warnings and Precautions (5.1)].
Do not abruptly discontinue TUSSIGON in a physically-dependent patient [see Drug Abuse and Dependence (9.3)]. When a patient who has been taking TUSSIGON regularly and may be physically dependent no longer requires therapy with TUSSIGON, taper the dose gradually, by 25% to 50% every 2 to 4 days, while monitoring carefully for signs and symptoms of withdrawal. If the patient develops these signs or symptoms, raise the dose to the previous level and taper more slowly, either by increasing the interval between decreases, decreasing the amount of change in dose, or both.
3. Dosage Forms and Strengths
Tablet: Each tablet contains hydrocodone bitartrate 5 mg and homatropine methylbromide 1.5 mg [see Description (11)].
4. Contraindications
TUSSIGON is contraindicated for:
- All children younger than 6 years of age [see Warnings and Precautions (5.2, 5.3), Use in Specific Populations (8.4)].
TUSSIGON is also contraindicated in patients with:
- Significant respiratory depression [see Warnings and Precautions (5.2)].
- Acute or severe bronchial asthma in an unmonitored setting or in the absence of resuscitative equipment [see Warnings and Precautions (5.4)].
- Known or suspected gastrointestinal obstruction, including paralytic ileus [see Warnings and Precautions (5.9)].
- Hypersensitivity to hydrocodone, homatropine, or any of the inactive ingredients in TUSSIGON [see Adverse Reactions (6)].
5. Warnings and Precautions
5.1 Addiction, Abuse, and Misuse
TUSSIGON contains hydrocodone, a Schedule II controlled substance. As an opioid, TUSSIGON exposes users to the risks of addiction, abuse, and misuse [see Drug Abuse and Dependence (9)], which can lead to overdose and death [see Overdosage (10)]. Reserve TUSSIGON for use in adult patients for whom the benefits of cough suppression are expected to outweigh the risks, and in whom an adequate assessment of the etiology of the cough has been made. Assess each patient's risk prior to prescribing TUSSIGON, prescribe TUSSIGON for the shortest duration that is consistent with individual patient treatment goals, monitor all patients regularly for the development of addiction or abuse, and refill only after reevaluation of the need for continued treatment.
Although the risk of addiction in any individual is unknown, it can occur in patients appropriately prescribed TUSSIGON. Addiction can occur at recommended dosages and if the drug is misused or abused. Risks are increased in patients with a personal or family history of substance abuse (including drug or alcohol abuse or addiction) or mental illness (e.g., major depression).
Opioids are sought by drug abusers and people with addiction disorders and are subject to criminal diversion. Consider these risks when prescribing or dispensing TUSSIGON. Strategies to reduce these risks include prescribing the drug in the smallest appropriate quantity and advising the patient on the proper disposal of unused drug [see Patient Counseling Information (17)]. Contact local state professional licensing board or state controlled substances authority for information on how to prevent and detect abuse or diversion of this product.
5.2 Life-Threatening Respiratory Depression
Serious, life-threatening, or fatal respiratory depression has been reported with the use of opioids, including hydrocodone, one of the active ingredients in TUSSIGON. Hydrocodone produces dose-related respiratory depression by directly acting on the brain stem respiratory center that controls respiratory rhythm and may produce irregular and periodic breathing. Respiratory depression, if not immediately recognized and treated, may lead to respiratory arrest and death. Management of respiratory depression includes discontinuation of TUSSIGON, close observation, supportive measures, and use of opioid antagonists (e.g. naloxone), depending on the patient's clinical status [see Overdosage (10)]. Carbon dioxide (CO2) retention from opioid-induced respiratory depression can exacerbate the sedating effects of opioids.
While serious, life-threatening, or fatal respiratory depression can occur at any time during the use of TUSSIGON, the risk is greatest during the initiation of therapy, when TUSSIGON is used concomitantly with other drugs that may cause respiratory depression [see Warnings and Precautions (5.8)], in patients with chronic pulmonary disease or decreased respiratory reserve, and in patients with altered pharmacokinetics or altered clearance (e.g. elderly, cachectic, or debilitated patients) [see Warnings and Precautions (5.4)].
To reduce the risk of respiratory depression, proper dosing of TUSSIGON is essential [see Dosage and Administration (2.1), Warnings and Precautions (5.5)]. Monitor patients closely, especially within the first 24–72 hours of initiating therapy or when used in patients at higher risk.
Overdose of hydrocodone in adults has been associated with fatal respiratory depression, and the use of hydrocodone in children younger than 6 years of age has been associated with fatal respiratory depression when used as recommended. Accidental ingestion of even one dose of TUSSIGON, especially by children, can result in respiratory depression and death.
5.3 Risks with Use in Pediatric Populations
Children are particularly sensitive to the respiratory depressant effects of hydrocodone [see Warnings and Precautions (5.2)]. Because of the risk of life-threatening respiratory depression and death, TUSSIGON is contraindicated in children less than 6 years of age [see Contraindications (4)].
Use of TUSSIGON in children also exposes them to the risks of addiction, abuse, and misuse [see Drug Abuse and Dependence (9)], which can lead to overdose and death [see Warnings and Precautions (5.1), Overdosage (10)]. Because the benefits of symptomatic treatment of cough associated with allergies or the common cold do not outweigh the risks of use of hydrocodone in pediatric patients, TUSSIGON is not indicated for use in patients younger than 18 years of age [see Indications (1), Use in Specific Populations (8.4)].
5.5 Risk of Accidental Overdose and Death due to Medication Errors
Dosing errors can result in accidental overdose and death. To reduce the risk of overdose and respiratory depression, ensure that the dose of TUSSIGON is communicated clearly and dispensed accurately [see Dosage and Administration (2.1)].
5.6 Activities Requiring Mental Alertness: Risks of Driving and Operating Machinery
Hydrocodone, one of the active ingredients in TUSSIGON, may produce marked drowsiness and impair the mental and/or physical abilities required for the performance of potentially hazardous tasks such as driving a car or operating machinery. Advise patients to avoid engaging in hazardous tasks requiring mental alertness and motor coordination after ingestion of TUSSIGON. Avoid concurrent use of TUSSIGON with alcohol or other central nervous system depressants because additional impairment of central nervous system performance may occur [see Warnings and Precautions (5.8)].
5.7 Risks from Concomitant Use or Discontinuation of Cytochrome P450 3A4 Inhibitors and Inducers
Concomitant use of TUSSIGON with a CYP3A4 inhibitor, such as macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g., ketoconazole), and protease inhibitors (e.g., ritonavir), may increase plasma concentrations of hydrocodone and prolong opioid adverse reactions, which may cause potentially fatal respiratory depression [see Warnings and Precautions (5.2)], particularly when an inhibitor is added after a stable dose of TUSSIGON is achieved. Similarly, discontinuation of a CYP3A4 inducer, such as rifampin, carbamazepine, and phenytoin, in TUSSIGON-treated patients may increase hydrocodone plasma concentrations and prolong opioid adverse reactions.
Concomitant use of TUSSIGON with CYP3A4 inducers or discontinuation of a CYP3A4 inhibitor could decrease hydrocodone plasma concentrations, decrease opioid efficacy or, possibly, lead to a withdrawal syndrome in a patient who had developed physical dependence to hydrocodone.
Avoid the use of TUSSIGON in patients who are taking a CYP3A4 inhibitor or inducer. If concomitant use of TUSSIGON with a CYP3A4 inhibitor or inducer is necessary, monitor patients for signs and symptoms that may reflect opioid toxicity and opioid withdrawal [see Drug Interactions (7.2, 7.3)].
5.8 Risks from Concomitant Use with Benzodiazepines or other CNS Depressants
Concomitant use of opioids, including TUSSIGON, with benzodiazepines, or other CNS depressants, including alcohol, may result in profound sedation, respiratory depression, coma, and death. Because of these risks, avoid use of opioid cough medications in patients taking benzodiazepines, other CNS depressants, or alcohol [see Drug Interactions (7.1, 7.4)].
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioids alone. Because of similar pharmacologic properties, it is reasonable to expect similar risk with concomitant use of opioid cough medications and benzodiazepines, other CNS depressants, or alcohol.
Advise both patients and caregivers about the risks of respiratory depression and sedation if TUSSIGON is used with benzodiazepines, alcohol, or other CNS depressants [see Patient Counseling Information (17)].
Patients must not consume alcoholic beverages, or prescription or non-prescription products containing alcohol, while on TUSSIGON therapy. The co-ingestion of alcohol with TUSSIGON may result in increased plasma levels and a potentially fatal overdose of hydrocodone [see Drug Interactions (7.1)].
5.9 Risks of Use in Patients with Gastrointestinal Conditions
TUSSIGON is contraindicated in patients with known or suspected gastrointestinal obstruction, including paralytic ileus [see Contraindications (4)]. The use of hydrocodone in TUSSIGON may obscure the diagnosis or clinical course of patients with acute abdominal conditions.
The concurrent use of anticholinergics with TUSSIGON may produce paralytic ileus [see Drug Interactions (7.9)].
The hydrocodone in TUSSIGON may result in constipation or obstructive bowel disease, especially in patients with underlying intestinal motility disorders. Use with caution in patients with underlying intestinal motility disorders.
The hydrocodone in TUSSIGON may cause spasm of the sphincter of Oddi, resulting in an increase in biliary tract pressure. Opioids may cause increases in serum amylase [see Warnings and Precautions (5.15)]. Monitor patients with biliary tract disease, including acute pancreatitis for worsening symptoms.
5.10 Risks of Use in Patients with Head Injury, Impaired Consciousness, Increased Intracranial Pressure, or Brain Tumors
Avoid the use of TUSSIGON in patients with head injury, intracranial lesions, or a pre-existing increase in intracranial pressure. In patients who may be susceptible to the intracranial effects of CO2 retention (e.g., those with evidence of increased intracranial pressure or brain tumors), TUSSIGON may reduce respiratory drive, and the resultant CO2 retention can further increase intracranial pressure. Furthermore, opioids produce adverse reactions that may obscure the clinical course of patients with head injuries.
5.11 Increased Risk of Seizures in Patients with Seizure Disorders
The hydrocodone in TUSSIGON may increase the frequency of seizures in patients with seizure disorders, and may increase the risk of seizures occurring in other clinical settings associated with seizures. Monitor patients with a history of seizure disorders for worsened seizure control during TUSSIGON therapy.
5.12 Severe Hypotension
TUSSIGON may cause severe hypotension including orthostatic hypotension and syncope in ambulatory patients. There is increased risk in patients whose ability to maintain blood pressure has already been compromised by a reduced blood volume or concurrent administration of certain CNS depressant drugs (e.g., phenothiazines or general anesthetics) [see Drug Interactions (7.4)]. Monitor these patients for signs of hypotension after initiating TUSSIGON.
In patients with circulatory shock, TUSSIGON may cause vasodilation that can further reduce cardiac output and blood pressure. Avoid the use of TUSSIGON in patients with circulatory shock.
5.13 Neonatal Opioid Withdrawal Syndrome
TUSSIGON is not recommended for use in pregnant women. Prolonged use of TUSSIGON during pregnancy can result in withdrawal in the neonate. Neonatal opioid withdrawal syndrome, unlike opioid withdrawal syndrome in adults, may be life-threatening if not recognized and treated, and requires management according to protocols developed by neonatology experts. Observe newborns for signs of neonatal opioid withdrawal syndrome and manage accordingly. Advise pregnant women using opioids for a prolonged period of the risk of neonatal opioid withdrawal syndrome and ensure that appropriate treatment will be available [see Use in Specific Populations (8.1), Patient Counseling Information (17)].
5.14 Adrenal Insufficiency
Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use. Presentation of adrenal insufficiency may include non-specific symptoms and signs including nausea, vomiting, anorexia, fatigue, weakness, dizziness, and low blood pressure. If adrenal insufficiency is suspected, confirm the diagnosis with diagnostic testing as soon as possible. If adrenal insufficiency is diagnosed, treat with physiologic replacement doses of corticosteroids. Wean the patient off of the opioid to allow adrenal function to recover and continue corticosteroid treatment until adrenal function recovers. Other opioids may be tried as some cases reported use of a different opioid without recurrence of adrenal insufficiency. The information available does not identify any particular opioids as being more likely to be associated with adrenal insufficiency.
6. Adverse Reactions/Side Effects
The following serious adverse reactions are described, or described in greater detail, in other sections:
- Addiction, abuse, and misuse [see Warnings and Precautions (5.1), Drug Abuse and Dependence (9.3)]
- Life-threatening respiratory depression [see Warnings and Precautions (5.2, 5.3, 5.4, 5.8), Overdosage (10)]
- Accidental overdose and death due to medication errors [see Warnings and Precautions (5.5)]
- Decreased mental alertness with impaired mental and/or physical abilities [see Warnings and Precautions (5.6)]
- Interactions with benzodiazepines and other CNS depressants [see Warnings and Precautions (5.8), Drug Interactions (7.1, 7.4)]
- Paralytic ileus, gastrointestinal adverse reactions [see Warnings and Precautions (5.9)]
- Increased intracranial pressure [see Warnings and Precautions (5.10)]
- Obscured clinical course in patients with head injuries [see Warnings and Precautions (5.10)]
- Seizures [see Warnings and Precautions (5.11)]
- Severe hypotension [see Warnings and Precautions (5.12)]
- Neonatal Opioid Withdrawal Syndrome [see Warnings and Precautions (5.13)]
- Adrenal insufficiency [see Warnings and Precautions (5.14)]
The following adverse reactions have been identified during clinical studies, in the literature, or during post-approval use of hydrocodone and/or homatropine. Because these reactions may be reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The most common adverse reactions to TUSSIGON include: Sedation (somnolence, mental clouding, lethargy), impaired mental and physical performance, lightheadedness, dizziness, headache, dry mouth, nausea, vomiting, and constipation.
Other reactions include:
Anaphylaxis: Anaphylaxis has been reported with hydrocodone, one of the ingredients in TUSSIGON.
Body as a whole: Coma, death, fatigue, falling injuries, lethargy.
Cardiovascular: Peripheral edema, increased blood pressure, decreased blood pressure, tachycardia, chest pain, palpitation, syncope, orthostatic hypotension, prolonged QT interval, hot flush.
Central Nervous System: Facial dyskinesia, insomnia, migraine, increased intracranial pressure, seizure, tremor.
Dermatologic: Flushing, hyperhidrosis, pruritus, rash.
Endocrine/Metabolic: Cases of serotonin syndrome, a potentially life-threatening condition, have been reported during concomitant use of opioids with serotonergic drugs. Cases of adrenal insufficiency have been reported with opioid use, more often following greater than one month of use. Cases of androgen deficiency have occurred with chronic use of opioids.
Gastrointestinal: Abdominal pain, bowel obstruction, decreased appetite, diarrhea, difficulty swallowing, dry mouth, GERD, indigestion, pancreatitis, paralytic ileus, biliary tract spasm (spasm of the sphincter of Oddi).
Genitourinary: Urinary tract infection, ureteral spasm, spasm of vesicle sphincters, urinary retention.
Laboratory: Increases in serum amylase.
Musculoskeletal: Arthralgia, backache, muscle spasm.
Ophthalmic: Miosis (constricted pupils), visual disturbances.
Psychiatric: Agitation, anxiety, confusion, fear, dysphoria, depression.
Reproductive: Hypogonadism, infertility.
Respiratory: Bronchitis, cough, dyspnea, nasal congestion, nasopharyngitis, respiratory depression, sinusitis, upper respiratory tract infection.
Other: Drug abuse, drug dependence, opioid withdrawal syndrome.
7. Drug Interactions
No specific drug interaction studies have been conducted with TUSSIGON.
7.1 Alcohol
Concomitant use of alcohol with TUSSIGON can result in an increase of hydrocodone plasma levels and potentially fatal overdose of hydrocodone. Instruct patients not to consume alcoholic beverages or use prescription or nonprescription products containing alcohol while on TUSSIGON therapy [see Warnings and Precautions (5.8), Clinical Pharmacology (12.3)].
7.2 Inhibitors of CYP3A4 and CYP2D6
The concomitant use of TUSSIGON and CYP3A4 inhibitors, such as macrolide antibiotics (e.g., erythromycin), azole-antifungal agents (e.g. ketoconazole), or protease inhibitors (e.g., ritonavir), can increase the plasma concentration of hydrocodone, resulting in increased or prolonged opioid effects. These effects could be more pronounced with concomitant use of TUSSIGON and CYP2D6 and CYP3A4 inhibitors, particularly when an inhibitor is added after a stable dose of TUSSIGON is achieved [see Warnings and Precautions (5.7)]. After stopping a CYP3A4 inhibitor, as the effects of the inhibitor decline, the hydrocodone plasma concentration will decrease [see Clinical Pharmacology (12.3)], resulting in decreased opioid efficacy or a withdrawal syndrome in patients who had developed physical dependence to hydrocodone.
Avoid the use of TUSSIGON while taking a CYP3A4 or CYP2D6 inhibitor. If concomitant use is necessary, monitor patients for respiratory depression and sedation at frequent intervals.
7.3 CYP3A4 Inducers
The concomitant use of TUSSIGON and CYP3A4 inducers such as rifampin, carbamazepine, or phenytoin, can decrease the plasma concentration of hydrocodone [see Clinical Pharmacology (12.3)], resulting in decreased efficacy or onset of a withdrawal syndrome in patients who have developed physical dependence to hydrocodone [see Warnings and Precautions (5.7)]. After stopping a CYP3A4 inducer, as the effects of the inducer decline, the hydrocodone plasma concentration will increase [see Clinical Pharmacology (12.3)], which could increase or prolong both the therapeutic effects and adverse reactions, and may cause serious respiratory depression.
Avoid the use of TUSSIGON in patients who are taking CYP3A4 inducers. If concomitant use of a CYP3A4 inducer is necessary, follow the patient for reduced efficacy.
7.4 Benzodiazepines and Other CNS Depressants
Due to additive pharmacologic effect, the concomitant use of benzodiazepines or other CNS depressants, including alcohol, other sedatives/hypnotics, anxiolytics, tranquilizers, muscle relaxants, general anesthetics, antipsychotics, and other opioids, can increase the risk of hypotension, respiratory depression, profound sedation, coma, and death. Avoid the use of TUSSIGON in patients who are taking benzodiazepines or other CNS depressants [see Warnings and Precautions (5.8)], and instruct patients to avoid consumption of alcohol while on TUSSIGON [see Drug Interactions (7.1), Patient Counseling Information (17)].
7.5 Serotonergic Drugs
The concomitant use of opioids with other drugs that affect the serotonergic neurotransmitter system has resulted in serotonin syndrome. If concomitant use is warranted, carefully observe the patient, particularly during treatment initiation. Discontinue TUSSIGON if serotonin syndrome is suspected.
7.6 Monoamine Oxidase Inhibitors (MAOIs)
Avoid the use of TUSSIGON in patients who are taking monoamine oxidase inhibitors (MAOIs) or have taken MAOIs within 14 days. The use of MAOIs or tricyclic antidepressants with hydrocodone, one of the active ingredients in TUSSIGON, may increase the effect of either the antidepressant or hydrocodone. MAOI interactions with opioids may manifest as serotonin syndrome or opioid toxicity (e.g., respiratory depression, coma).
7.7 Muscle Relaxants
Hydrocodone may enhance the neuromuscular blocking action of skeletal muscle relaxants and produce an increased degree of respiratory depression. Avoid the use of TUSSIGON in patients taking muscle relaxants. If concomitant use is necessary, monitor patients for signs of respiratory depression that may be greater than otherwise expected.
7.8 Diuretics
Opioids can reduce the efficacy of diuretics by inducing the release of antidiuretic hormone. Monitor patients for signs of diminished diuresis and/or effects on blood pressure and increase the dosage of the diuretic as needed.
7.9 Anticholinergic Drugs
The concomitant use of anticholinergic drugs with TUSSIGON may increase risk of urinary retention and/or severe constipation, which may lead to paralytic ileus [see Warnings and Precautions (5.9)]. Monitor patients for signs of urinary retention or reduced gastric motility when TUSSIGON is used concomitantly with anticholinergic drugs.
8. Use In Specific Populations
8.1 Pregnancy
8.2 Lactation
8.4 Pediatric Use
TUSSIGON is not indicated for use in patients younger than 18 years of age because the benefits of symptomatic treatment of cough associated with allergies or the common cold do not outweigh the risks for use of hydrocodone in these patients [see Indications (1), Warnings and Precautions (5.3)].
Life-threatening respiratory depression and death have occurred in children who received hydrocodone [see Warnings and Precautions (5.2)]. Because of the risk of life-threatening respiratory depression and death, TUSSIGON is contraindicated in children less than 6 years of age [see Contraindications (4)].
8.5 Geriatric Use
Clinical studies have not been conducted with TUSSIGON in geriatric populations.
Use caution when considering the use of TUSSIGON in patients 65 years of age or older. Elderly patients may have increased sensitivity to hydrocodone; greater frequency of decreased hepatic, renal, or cardiac function; or concomitant disease or other drug therapy [see Warnings and Precautions (5.4)].
Respiratory depression is the chief risk for elderly patients treated with opioids, including TUSSIGON. Respiratory depression has occurred after large initial doses of opioids were administered to patients who were not opioid-tolerant or when opioids were co-administered with other agents that depress respiration [see Warnings and Precautions (5.4, 5.8)].
Hydrocodone is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, monitor these patients closely for respiratory depression, sedation, and hypotension.
8.6 Renal Impairment
The pharmacokinetics of TUSSIGON has not been characterized in patients with renal impairment. Patients with renal impairment may have higher plasma concentrations than those with normal function [see Clinical Pharmacology (12.3)]. TUSSIGON should be used with caution in patients with severe impairment of renal function, and patients should be monitored closely for respiratory depression, sedation, and hypotension.
8.7 Hepatic Impairment
The pharmacokinetics of TUSSIGON has not been characterized in patients with hepatic impairment. Patients with severe hepatic impairment may have higher plasma concentrations than those with normal hepatic function [see Clinical Pharmacology (12.3)]. Therefore, TUSSIGON should be used with caution in patients with severe impairment of hepatic function, and patients should be monitored closely for respiratory depression, sedation, and hypotension.
9. Drug Abuse and Dependence
9.3 Dependence
Psychological dependence, physical dependence, and tolerance may develop upon repeated administration of opioids; therefore, TUSSIGON should be prescribed and administered for the shortest duration that is consistent with individual patient treatment goals and patients should be reevaluated prior to refills [see Dosage and Administration (2.3), Warnings and Precautions (5.1)].
Physical dependence, the condition in which continued administration of the drug is required to prevent the appearance of a withdrawal syndrome, assumes clinically significant proportions only after several weeks of continued oral opioid use, although some mild degree of physical dependence may develop after a few days of opioid therapy.
If TUSSIGON is abruptly discontinued in a physically-dependent patient, a withdrawal syndrome may occur. Withdrawal also may be precipitated through the administration of drugs with opioid antagonist activity (e.g., naloxone, nalmefene), mixed agonist/antagonist analgesics (e.g., pentazocine, butorphanol, nalbuphine), or partial agonists (e.g., buprenorphine). Some or all of the following can characterize this syndrome: restlessness, lacrimation, rhinorrhea, yawning, perspiration, chills, myalgia, and mydriasis. Other signs and symptoms also may develop, including irritability, anxiety, backache, joint pain, weakness, abdominal cramps, insomnia, nausea, anorexia, vomiting, diarrhea, or increased blood pressure, respiratory rate, or heart rate.
Infants born to mothers physically dependent on opioids will also be physically dependent and may exhibit respiratory difficulties and withdrawal signs [see Use in Specific Populations (8.1)].
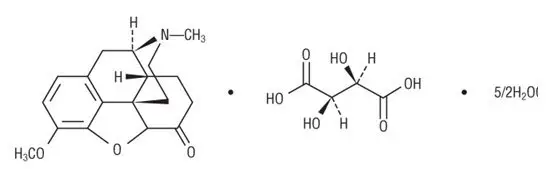
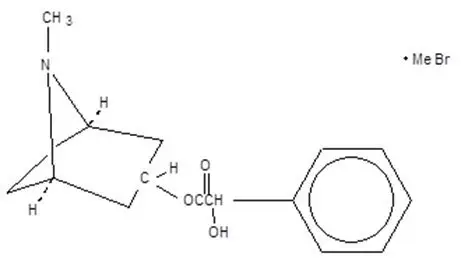
11. Tussigon Description
TUSSIGON tablets contain hydrocodone an opioid agonist, and homatropine, a muscarinic antagonist.
Each tablet of TUSSIGON contains 5 mg of hydrocodone bitartrate, USP and 1.5 mg of homatropine methylbromide, USP for oral administration.
TUSSIGON also contains the following inactive ingredients: Colloidal Silicon Dioxide NF, FD & C Blue No. 1 Aluminum Lake, Lactose Monohydrate NF, Microcrystalline Cellulose NF, Pregelatinized Starch NF, Stearic Acid NF, Talc USP.
12. Tussigon - Clinical Pharmacology
13. Nonclinical Toxicology
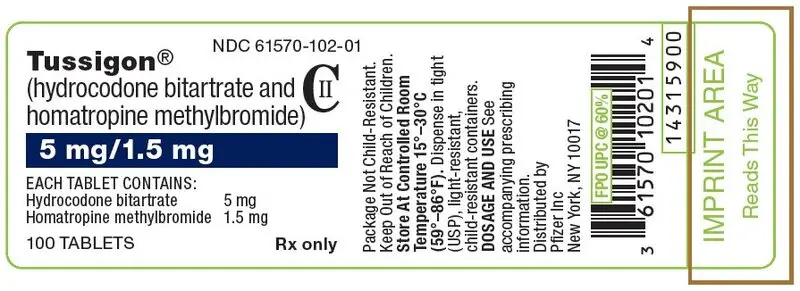
16. How is Tussigon supplied
TUSSIGON is supplied in the following strength and package configuration:
| Package Configuration | Tablet Strength (mg) | NDC | Tablet Description |
|---|---|---|---|
| Bottles of 100 | hydrocodone bitartrate (5 mg) and homatropine methylbromide (1.5 mg) | 61570-102-01 | blue, scored tablet |
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
| MEDICATION GUIDE TUSSIGON (tuh-se-gone) (hydrocodone bitartrate and homatropine methylbromide) tablets, C-II |
||
|---|---|---|
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised: June 2018 | |
| What is the most important information I should know about TUSSIGON tablets? TUSSIGON is not for children under 18 years of age. TUSSIGON can cause serious side effects, including:
|
||
|
|
|
|
||
What are TUSSIGON tablets?
|
||
| Who should not take TUSSIGON tablets? TUSSIGON is not for children under 18 years of age. See "What is the most important information I should know about TUSSIGON?" Do not take TUSSIGON if you:
|
||
| Before you take TUSSIGON tablets, tell your healthcare provider about all of your medical conditions, including if you: | ||
|
|
|
Taking TUSSIGON with certain other medicines can cause side effects or affect how well TUSSIGON or the other medicines work. Do not start or stop taking other medicines without talking to your healthcare provider. Especially tell your healthcare provider if you:
|
||
How should I take TUSSIGON tablets?
|
||
What should I avoid while taking TUSSIGON tablets?
|
||
| What are the possible side effects of TUSSIGON tablets? TUSSIGON can cause serious side effects, including:
|
||
|
|
|
| The most common side effects of TUSSIGON include: | ||
|
|
|
Other side effects include:
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||
How should I store TUSSIGON tablets?
|
||
| How should I dispose of TUSSIGON tablets?
Follow your state or local guidelines on how to safely throw away TUSSIGON. |
||
| General information about the safe and effective use of TUSSIGON tablets.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use TUSSIGON for a condition for which it was not prescribed. Do not give TUSSIGON to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about TUSSIGON that is written for health professionals. |
||
| What are the ingredients in TUSSIGON tablets? Active ingredients: hydrocodone bitartrate and homatropine methylbromide. Inactive ingredients: Colloidal Silicon Dioxide NF, FD & C Blue No. 1 Aluminum Lake, Lactose Monohydrate NF, Microcrystalline Cellulose NF, Pregelatinized Starch NF, Stearic Acid NF, Talc USP. |
||
| This product's label may have been updated. For current full prescribing information, please visit www.pfizer.com.
LAB-0834-4.0 |
||
| TUSSIGON
hydrocodone bitartrate and homatropine methylbromide tablet |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Labeler - Pfizer Laboratories Div Pfizer Inc (134489525) |