Drug Class: Urinary antispasmodics
Precautions
Drug Interactions:
Although the exact mechanism of this drug interaction is unknown, methylene blue inhibits the action of monoamine oxidase A— an enzyme responsible for breaking down serotonin in the brain. It is believed that when methylene blue is given to patients taking serotonergic psychiatric medications, high levels of serotonin can build up in the brain, causing toxicity. This is referred to as Serotonin Syndrome. Signs and symptoms of Serotonin Syndrome include mental changes (confusion, hyperactivity, memory problems), muscle twitching, excessive sweating, shivering or shaking, diarrhea, trouble with coordination, and/or fever.
Additional Information for Healthcare Professionals:
Methylene blue can interact with serotonergic psychiatric medications and cause serious CNS toxicity.
In emergency situations requiring life-threatening or urgent treatment with methylene blue (as described above), the availability of alternative interventions should be considered and the benefit of methylene blue treatment should be weighed against the risk of serotonin toxicity. If methylene blue must be administered to a patient receiving a serotonergic drug, the serotonergic drug must be immediately stopped, and the patient should be closely monitored for emergent symptoms of CNS toxicity for two weeks (five weeks if fluoxetine [Prozac] was taken), or until 24 hours after the last dose of methylene blue, whichever comes first.
In non-emergency situations when non-urgent treatment with methylene blue is contemplated and planned, the serotonergic psychiatric medication should be stopped to allow its activity in the brain to dissipate. Most serotonergic psychiatric drugs should be stopped at least 2 weeks in advance of methylene blue treatment. Fluoxetine (Prozac), which has a longer half-life compared to similar drugs, should be stopped at least 5 weeks in advance.
Treatment with the serotonergic psychiatric medication may be resumed 24 hours after the last dose of methylene blue.
Serotonergic psychiatric medications should not be started in a patient receiving methylene blue. Wait until 24 hours after the last dose of methylene blue before starting the antidepressant.
Educate your patients to recognize the symptoms of serotonin toxicity or CNS toxicity and advise them to contact a healthcare professional immediately if they experience any symptoms while taking serotonergic psychiatric medications or methylene blue.
As a result of hyoscyamine's effects on gastrointestinal motility and gastric emptying, absorption of other oral medications may be decreased during concurrent use with this combination medication.
Urinary alkalizers and thiazide diuretics:
May cause the urine to become alkaline reducing the effectiveness of methenamine by inhibiting its conversion to formaldehyde.
Antimuscarinics:
Concurrent use may intensify antimuscarinic effects of hyoscyamine because of secondary antimuscarinic activities of these medications.
Antacids/antidiarrheals:
Concurrent use may reduce absorption of hyoscyamine resulting in decreased therapeutic effectiveness. Concurrent use with antacids may cause urine to become alkaline reducing the effectiveness of methenamine by inhibiting its conversion to formaldehyde. Doses of these medications should be spaced 1 hour apart from doses of hyoscyamine.
Antimyasthenics:
Concurrent use with hyoscyamine may further reduce intestinal motility, therefore, caution is recommended.
Ketoconazole and hyoscyamine may cause increased gastrointestinal pH. Concurrent administration with hyoscyamine may result in marked reduction in the absorption of ketoconazole. Patients should be advised to take this combination at least 2 hours after ketoconazole.
Monoamine oxidase (MAO) inhibitors:
Concurrent use with hyoscyamine may intensify antimuscarinic side effects.
Opioid (narcotic) analgesics may result in increased risk of severe constipation.
Sulfonamides:
These drugs may precipitate with formaldehyde in the urine increasing the danger of crystalluria.
Patients should be advised that the urine and/or stools may become blue to blue-green as a result of the excretion of methylene blue.
Pregnancy/Reproduction (FDA Pregnancy Category C):
Hyoscyamine and methenamine cross the placenta. Studies have not been done in either animals or humans. It is not known whether URAMIT MB™ can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity.
URAMIT MB™ should be given to a pregnant woman only if clearly needed.
Nursing mothers:
Methenamine and traces of hyoscyamine are excreted in breast milk. Caution should be exercised when URAMIT MB™ is administered to a nursing mother.
Prolonged use:
There have been no studies to establish the safety of prolonged use in humans. No known long-term animal studies have been performed to evaluate carcinogenic potential.
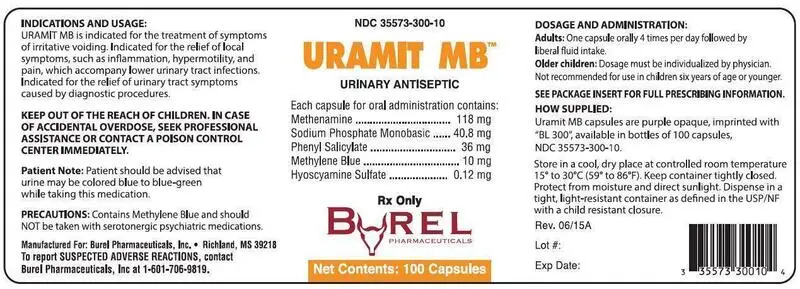
| URAMIT MB
methenamine, sodium phosphate, monobasic, monohydrate, phenyl salicylate, methylene blue, and hyoscyamine sulfate capsule |
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
|
|||||||||||||||||||||
| Labeler - Burel Pharmaceuticals, Inc (002152814) |