Drug Detail:Valtoco (Diazepam nasal [ dye-az-e-pam ])
Drug Class: Benzodiazepine anticonvulsants
Highlights of Prescribing Information
VALTOCO® (diazepam nasal spray), CIV
Initial U.S. Approval: 1963
WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS; ABUSE, MISUSE, AND ADDICTION; and DEPENDENCE AND WITHDRAWAL REACTIONS
See full prescribing information for complete boxed warning
- Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. (5.1, 7.1)
- The use of benzodiazepines, including VALTOCO, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose or death. Before prescribing VALTOCO and throughout treatment, assess each patient's risk for abuse, misuse, and addiction. (5.2)
- Although VALTOCO is indicated only for intermittent use (1, 2), if used more frequently than recommended, abrupt discontinuation or rapid dosage reduction of VALTOCO may precipitate acute withdrawal reactions, which can be life-threatening. For patients using VALTOCO more frequently than recommended, to reduce the risk of withdrawal reactions, use a gradual taper to discontinue VALTOCO. (5.3)
Recent Major Changes
| Warnings and Precautions (5.7) | 1/2023 |
Indications and Usage for Valtoco
VALTOCO is a benzodiazepine indicated for the acute treatment of intermittent, stereotypic episodes of frequent seizure activity (i.e., seizure clusters, acute repetitive seizures) that are distinct from a patient's usual seizure pattern in patients with epilepsy 6 years of age and older. (1)
Valtoco Dosage and Administration
Administer VALTOCO by the nasal route only. (2.3)
Dosage is dependent on the patient's age and weight. (2.2)
Initial Dose: VALTOCO 5 mg and 10 mg doses are administered as a single spray intranasally into one nostril. Administration of 15 mg and 20 mg doses requires two nasal spray devices, one spray into each nostril. (2.2)
Second Dose: A second dose, when required, may be administered at least 4 hours after the initial dose. If administered, use a new blister pack. (2.2)
Maximum Dosage and Treatment Frequency: Do not use more than 2 doses to treat a single episode. It is recommended that VALTOCO be used to treat no more than one episode every five days and no more than five episodes per month. (2.2)
Dosage Forms and Strengths
Nasal spray: 5 mg, 7.5 mg, or 10 mg of diazepam in 0.1 mL. (3)
Contraindications
- Hypersensitivity to diazepam. (4)
- Acute narrow-angle glaucoma. (4)
Warnings and Precautions
- CNS Depression: May cause an increased CNS-depressant effect when used with alcohol or other CNS depressants. (5.4)
- Suicidal Behavior and Ideation: Antiepileptic drugs increase the risk of suicidal ideation and behavior. (5.5)
- Glaucoma: VALTOCO can increase intraocular pressure in patients with glaucoma. VALTOCO may be used in patients with open-angle glaucoma only if they are receiving appropriate therapy. (4, 5.6)
- Neonatal Sedation and Withdrawal Syndrome: VALTOCO use during pregnancy can result in neonatal sedation and/or neonatal withdrawal. (5.7, 8.1)
Adverse Reactions/Side Effects
The most common adverse reactions (at least 4%) were somnolence, headache, and nasal discomfort. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Neurelis, Inc. at 1-866-696-3873 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- CYP2C19 and CYP3A4 Inhibitors: Adverse reactions with VALTOCO may be increased. (7.3)
- Inducers of CYP2C19 and CYP3A4 Inducers: Exposure of diazepam after VALTOCO administration may be decreased. (7.3)
Use In Specific Populations
- Pregnancy: Based on animal data, may cause fetal harm. (8.1)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 8/2023
Full Prescribing Information
WARNING: RISKS FROM CONCOMITANT USE WITH OPIOIDS; ABUSE, MISUSE, AND ADDICTION; and DEPENDENCE AND WITHDRAWAL REACTIONS
- Concomitant use of benzodiazepines and opioids may result in profound sedation, respiratory depression, coma, and death. Reserve concomitant prescribing of these drugs for patients for whom alternative treatment options are inadequate. Limit dosages and durations to the minimum required. Follow patients for signs and symptoms of respiratory depression and sedation [see Warnings and Precautions (5.1) and Drug Interactions (7.1)].
- The use of benzodiazepines, including VALTOCO, exposes users to risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes. Before prescribing VALTOCO and throughout treatment, assess each patient's risk for abuse, misuse, and addiction [see Warnings and Precautions (5.2)].
- The continued use of benzodiazepines may lead to clinically significant physical dependence. The risks of dependence and withdrawal increase with longer treatment duration and higher daily dose. Although VALTOCO is indicated only for intermittent use [see Indications and Usage (1) and Dosage and Administration (2)], if used more frequently than recommended, abrupt discontinuation or rapid dosage reduction of VALTOCO may precipitate acute withdrawal reactions, which can be life-threatening. For patients using VALTOCO more frequently than recommended, to reduce the risk of withdrawal reactions, use a gradual taper to discontinue VALTOCO [see Warnings and Precautions (5.3)].
1. Indications and Usage for Valtoco
VALTOCO® is indicated for the acute treatment of intermittent, stereotypic episodes of frequent seizure activity (i.e., seizure clusters, acute repetitive seizures) that are distinct from a patient's usual seizure pattern in patients with epilepsy 6 years of age and older.
2. Valtoco Dosage and Administration
2.1 Instructions Prior to Dosing
Prior to treatment, healthcare professionals should instruct the individual administering VALTOCO on how to identify seizure clusters and use the product appropriately [see Dosage and Administration (2.3) and Patient Counseling Information (17)].
2.2 Dosing Information
The recommended dose of VALTOCO nasal spray is 0.2 mg/kg or 0.3 mg/kg, depending on the patient's age and weight. See Table 1 for specific recommendations.
The following table provides the acceptable weight ranges for each dose and age category, such that patients will receive between 90% and 180% of the calculated recommended dose.
| Dose Based on Age and Weight | Administration | |||
|---|---|---|---|---|
| 6 to 11 Years of Age (0.3 mg/kg) | 12 Years of Age and Older (0.2 mg/kg) | Dose (mg) | Number of Nasal Spray Devices | Number of Sprays |
| Weight (kg) | Weight (kg) | |||
| 10 to 18 | 14 to 27 | 5 | One 5 mg device | One spray in one nostril |
| 19 to 37 | 28 to 50 | 10 | One 10 mg device | One spray in one nostril |
| 38 to 55 | 51 to 75 | 15 | Two 7.5 mg devices | One spray in each nostril |
| 56 to 74 | 76 and up | 20 | Two 10 mg devices | One spray in each nostril |
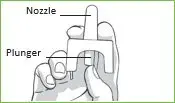
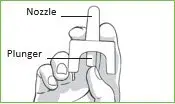
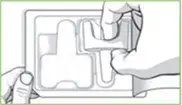
2.3 Important Administration Instructions
VALTOCO is for intranasal use only.
No device assembly is required. VALTOCO is a ready-to-use nasal spray device. VALTOCO nasal spray delivers its entire contents upon activation. Do not prime or attempt to use for more than one administration per device.
Patients and caregivers should be counseled to read carefully the "Instructions for Use" for complete directions on how to properly administer VALTOCO.
3. Dosage Forms and Strengths
VALTOCO is available in 5 mg, 7.5 mg, and 10 mg strengths. Each VALTOCO nasal spray device contains 0.1 mL solution.
4. Contraindications
VALTOCO nasal spray is contraindicated in patients with:
- Known hypersensitivity to diazepam
- Acute narrow angle glaucoma [see Warnings and Precautions (5.6)]
5. Warnings and Precautions
5.1 Risk of Concomitant Use with Opioids
Concomitant use of benzodiazepines, including VALTOCO, and opioids may result in profound sedation, respiratory depression, coma, and death [see Drug Interactions (7.1)]. Because of these risks, reserve concomitant prescribing of benzodiazepines and opioids for patients for whom alternative treatment options are inadequate.
Observational studies have demonstrated that concomitant use of opioid analgesics and benzodiazepines increases the risk of drug-related mortality compared to use of opioids alone. If a decision is made to prescribe VALTOCO concomitantly with opioids, prescribe the lowest effective dosages and minimum durations of concomitant use, and follow patients closely for signs and symptoms of respiratory depression and sedation. Advise both patients and caregivers about the risks of respiratory depression and sedation when VALTOCO is used with opioids.
5.2 Abuse, Misuse, and Addiction
The use of benzodiazepines, including VALTOCO, exposes users to the risks of abuse, misuse, and addiction, which can lead to overdose or death. Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the maximum recommended dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death [see Drug Abuse and Dependence (9.2)].
Before prescribing VALTOCO and throughout treatment, assess each patient's risk for abuse, misuse, and addiction. Use of VALTOCO, particularly in patients at elevated risk, necessitates counseling about the risks and proper use of VALTOCO along with monitoring for signs and symptoms of abuse, misuse, and addiction. Do not exceed the recommended dosing frequency; avoid or minimize concomitant use of CNS depressants and other substances associated with abuse, misuse, and addiction (e.g., opioid analgesics, stimulants); and advise patients on the proper disposal of unused drug. If a substance use disorder is suspected, evaluate the patient and institute (or refer them for) early treatment, as appropriate.
5.3 Dependence and Withdrawal Reactions After Use of VALTOCO More Frequently Than Recommended
For patients using VALTOCO more frequently than recommended, to reduce the risk of withdrawal reactions, use a gradual taper to discontinue VALTOCO (a patient-specific plan should be used to taper the dose).
Patients at an increased risk of withdrawal adverse reactions after benzodiazepine discontinuation or rapid dosage reduction include those who take higher dosages, and those who have had longer durations of use.
5.4 CNS Depression
Benzodiazepines, including VALTOCO, may produce CNS depression. Caution patients against engaging in hazardous activities requiring mental alertness (e.g., operating machinery, driving a motor vehicle, or riding a bicycle) until the effects of the drug, such as drowsiness, have subsided, and as their medical condition permits. Although VALTOCO is indicated for use solely on an intermittent basis, the potential for synergistic CNS-depressant effects when used simultaneously with alcohol or other CNS depressants must be considered by the prescriber and appropriate recommendations made to the patient and/or caregiver.
5.5 Suicidal Behavior and Ideation
Antiepileptic drugs (AEDs), including VALTOCO, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed. The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5-100 years) in the clinical trials analyzed. Table 2 shows absolute and relative risk by indication for all evaluated AEDs.
| Indication | Placebo Patients with Events/1000 Patients | Drug Patients with Events per 1000 Patients | Relative Risk: Incidence of Drug Events in Drug Patients /Incidence in Placebo Patients | Risk Difference: Additional Drug Patients with Events per 1000 Patients |
|---|---|---|---|---|
| Epilepsy | 1.0 | 3.4 | 3.5 | 2.4 |
| Psychiatric | 5.7 | 8.5 | 1.5 | 2.9 |
| Other | 1.0 | 1.8 | 1.9 | 0.9 |
| Total | 2.4 | 4.3 | 1.8 | 1.9 |
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing VALTOCO or any other AED must balance the risk of suicidal thoughts or behaviors with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
5.6 Glaucoma
Benzodiazepines, including VALTOCO, can increase intraocular pressure in patients with glaucoma. VALTOCO may be used in patients with open-angle glaucoma only if they are receiving appropriate therapy. VALTOCO is contraindicated in patients with narrow-angle glaucoma.
5.7 Neonatal Sedation and Withdrawal Syndrome
Use of VALTOCO late in pregnancy can result in sedation (respiratory depression, lethargy, hypotonia) and/or withdrawal symptoms (hyperreflexia, irritability, restlessness, tremors, inconsolable crying, and feeding difficulties) in the neonate [see Use in Specific Populations (8.1)]. Monitor neonates exposed to VALTOCO during pregnancy or labor for signs of sedation and monitor neonates exposed to VALTOCO during pregnancy for signs of withdrawal; manage these neonates accordingly.
5.8 Risk of Serious Adverse Reactions in Infants due to Benzyl Alcohol Preservative
VALTOCO is not approved for use in neonates or infants. Serious and fatal adverse reactions including "gasping syndrome" can occur in neonates and low birth weight infants treated with benzyl alcohol-preserved drugs, including VALTOCO. The "gasping syndrome" is characterized by central nervous system depression, metabolic acidosis, and gasping respirations. The minimum amount of benzyl alcohol at which serious adverse reactions may occur is not known (VALTOCO contains 10.5 mg of benzyl alcohol per 0.1 mL) [see Use in Specific Populations (8.4)].
6. Adverse Reactions/Side Effects
The following serious adverse reactions are discussed elsewhere in the labeling:
- Risk of Concomitant Use with Opioids [see Warnings and Precautions (5.1)]
- Abuse, Misuse, and Addiction [see Warnings and Precautions (5.2)]
- Dependence and Withdrawal Reactions After Use of VALTOCO More Frequently Than Recommended [see Warnings and Precautions (5.3)]
- CNS depression [see Warnings and Precautions (5.4)]
- Suicidal Behavior and Ideation [see Warnings and Precautions (5.5)]
- Glaucoma [see Warnings and Precautions (5.6)]
- Neonatal Sedation and Withdrawal Syndrome [see Warnings and Precautions (5.7)]
- Risk of Serious Adverse Reactions in Infants due to Benzyl Alcohol Preservative [see Warnings and Precautions (5.8)].
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to the rates in the clinical studies of another drug and may not reflect the rates observed in practice. The safety of VALTOCO is supported by clinical trials using diazepam rectal gel, as well as open-label, repeat-dose studies of VALTOCO in healthy subjects and epilepsy patients.
Diazepam Rectal Gel
In studies previously conducted with diazepam rectal gel, adverse event data were collected from double-blind, placebo-controlled studies and open-label studies. The majority of adverse events were mild to moderate in severity and transient in nature.
Two patients who received diazepam rectal gel died seven to 15 weeks following treatment; neither of these deaths was deemed related to diazepam rectal gel.
The most frequent adverse reactions (at least 4%) in the two double-blind, placebo-controlled studies were somnolence, headache, and diarrhea. Adverse events were usually mild or moderate in intensity.
Approximately 1.4% of the 573 patients who received diazepam rectal gel in clinical trials of epilepsy discontinued treatment because of an adverse event. The adverse reaction most frequently associated with discontinuation (occurring in three patients) was somnolence. Other adverse reactions most commonly associated with discontinuation and occurring in two patients were hypoventilation and rash. Adverse reactions associated with discontinuation occurring in one patient were asthenia, hyperkinesia, incoordination, vasodilatation, and urticaria.
In the two double-blind, placebo-controlled, parallel-group studies [see Clinical Studies (14)], the proportion of patients who discontinued treatment because of adverse events was 2% for the group treated with diazepam rectal gel, versus 2% for the placebo group. In the diazepam rectal gel group, one patient discontinued because of rash and one patient discontinued because of lethargy.
| Adverse Reaction | Diazepam Rectal Gel N=101 % | Placebo N=104 % |
|---|---|---|
| Somnolence | 23 | 8 |
| Headache | 5 | 4 |
| Diarrhea | 4 | <1 |
| Ataxia | 3 | <1 |
| Dizziness | 3 | 2 |
| Euphoria | 3 | 0 |
| Incoordination | 3 | 0 |
| Rash | 3 | 0 |
| Asthma | 2 | 0 |
| Vasodilation | 2 | 0 |
7. Drug Interactions
7.1 Effect of Concomitant Use of Benzodiazepines and Opioids
The concomitant use of benzodiazepines and opioids increases the risk of respiratory depression because of actions at different receptor sites in the CNS that control respiration. Benzodiazepines interact at GABA-A sites, and opioids interact primarily at mu receptors. When benzodiazepines and opioids are combined, the potential for benzodiazepines to significantly worsen opioid-related respiratory depression exists [see Warnings and Precautions (5.1)]. Limit dosage and duration of concomitant use of benzodiazepines and opioids, and follow patients closely for respiratory depression and sedation.
7.2 CNS Depressants and Alcohol
Coadministration of other CNS depressants (e.g., valproate) or consumption of alcohol may potentiate the CNS-depressant effects of diazepam [see Warnings and Precautions (5.4)].
7.3 Effect of Other Drugs on VALTOCO Metabolism
Potential interactions may occur when diazepam is given concurrently with agents that affect CYP2C19 and CYP3A4 activity.
7.4 Effect of VALTOCO on the Metabolism of Other Drugs
Diazepam is a substrate for CYP2C19 and CYP3A4; therefore, it is possible that VALTOCO may interfere with the metabolism of drugs which are substrates for CYP2C19 (e.g., omeprazole, propranolol, and imipramine) and CYP3A4 (e.g., cyclosporine, paclitaxel, theophylline, and warfarin) leading to a potential drug-drug interaction.
8. Use In Specific Populations
8.1 Pregnancy
Data
Human Data
Published data from observational studies on the use of benzodiazepines during pregnancy do not report a clear association with benzodiazepines and major birth defects.
Although early studies reported an increased risk of congenital malformations with diazepam and chlordiazepoxide, there was no consistent pattern noted. In addition, the majority of more recent case-control and cohort studies of benzodiazepine use during pregnancy, which were adjusted for confounding exposures to alcohol, tobacco, and other medications, have not confirmed these findings.
Animal Data
Diazepam has been shown to produce increased incidences of fetal malformations in mice and hamsters when given orally at single doses of 100 mg/kg or greater (approximately 13 times the maximum recommended human dose [MRHD = 0.6mg/kg/day] or greater on a mg/m2 basis). Cleft palate and exencephaly are the most common and consistently reported malformations produced in these species by administration of high, maternally-toxic doses of diazepam during organogenesis.
In published animal studies, administration of benzodiazepines or other drugs that enhance GABAergic inhibition to neonatal rats has been reported to result in widespread apoptotic neurodegeneration in the developing brain at plasma concentrations relevant for seizure control in humans. The window of vulnerability to these changes in rats (postnatal days 0-14) includes a period of brain development that takes place during the third trimester of pregnancy in humans.
8.4 Pediatric Use
Safety and effectiveness of VALTOCO have been established in pediatric patients 6 years to 16 years of age. Use of VALTOCO in this age group is supported by evidence from adequate and well-controlled studies of diazepam rectal gel in adult and pediatric patients, adult bioavailability studies comparing VALTOCO with diazepam rectal gel, patient pharmacokinetic data, and an open-label safety study of VALTOCO including patients 6 years to 16 years of age [see Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14)].
Safety and effectiveness of VALTOCO in pediatric patients below the age of 6 have not been established.
VALTOCO is not approved for use in neonates or infants.
- Prolonged CNS depression has been observed in neonates treated with diazepam.
- Serious adverse reactions including fatal reactions and the "gasping syndrome" occurred in premature neonates and low-birth-weight infants in the neonatal intensive care unit who received drugs containing benzyl alcohol as a preservative. In these cases, benzyl alcohol dosages of 99 to 234 mg/kg/day produced high levels of benzyl alcohol and its metabolites in the blood and urine (blood levels of benzyl alcohol were 0.61 to 1.378 mmol/L). Additional adverse reactions included gradual neurological deterioration, seizures, intracranial hemorrhage, hematologic abnormalities, skin breakdown, hepatic and renal failure, hypotension, bradycardia, and cardiovascular collapse. Preterm, low-birth-weight infants may be more likely to develop these reactions because they may be less able to metabolize benzyl alcohol. The minimum amount of benzyl alcohol at which serious adverse reactions may occur is not known (VALTOCO contains 10.5 mg of benzyl alcohol per 0.1 mL) [see Warnings and Precautions (5.8)].
8.5 Geriatric Use
Clinical studies of VALTOCO did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects.
Therefore, in elderly patients, VALTOCO should be used with caution because of an increase in half-life with a corresponding decrease in the clearance of free diazepam [see Clinical Pharmacology (12.3)]. It is also recommended that the dosage be decreased to reduce the likelihood of ataxia or oversedation.
9. Drug Abuse and Dependence
9.2 Abuse
VALTOCO is a benzodiazepine and a CNS depressant with a potential for abuse and addiction. Abuse is the intentional, non-therapeutic use of a drug, even once, for its desirable psychological or physiological effects. Misuse is the intentional use, for therapeutic purposes, of a drug by an individual in a way other than prescribed by a health care provider or for whom it was not prescribed. Drug addiction is a cluster of behavioral, cognitive, and physiological phenomena that may include a strong desire to take the drug, difficulties in controlling drug use (e.g., continuing drug use despite harmful consequences, giving a higher priority to drug use than other activities and obligations), and possible tolerance or physical dependence. Even taking benzodiazepines as prescribed may put patients at risk for abuse and misuse of their medication. Abuse and misuse of benzodiazepines may lead to addiction.
Abuse and misuse of benzodiazepines often (but not always) involve the use of doses greater than the maximum recommended dosage and commonly involve concomitant use of other medications, alcohol, and/or illicit substances, which is associated with an increased frequency of serious adverse outcomes, including respiratory depression, overdose, or death. Benzodiazepines are often sought by individuals who abuse drugs and other substances, and by individuals with addictive disorders [see Warnings and Precautions (5.2)].
The following adverse reactions have occurred with benzodiazepine abuse and/or misuse: abdominal pain, amnesia, anorexia, anxiety, aggression, ataxia, blurred vision, confusion, depression, disinhibition, disorientation, dizziness, euphoria, impaired concentration and memory, indigestion, irritability, muscle pain, slurred speech, tremors, and vertigo.
The following severe adverse reactions have occurred with benzodiazepine abuse and/or misuse: delirium, paranoia, suicidal ideation and behavior, seizures, coma, breathing difficulty, and death. Death is more often associated with polysubstance use (especially benzodiazepines with other CNS depressants such as opioids and alcohol).
In the clinical studies with VALTOCO at recommended doses, abuse-related adverse events included euphoria, somnolence, sedation, anterograde amnesia, depression, anxiety, hallucinations, and restlessness.
9.3 Dependence
10. Overdosage
Overdosage of benzodiazepines is characterized by central nervous system depression ranging from drowsiness to coma. In mild to moderate cases, symptoms can include drowsiness, confusion, dysarthria, lethargy, hypnotic state, diminished reflexes, ataxia, and hypotonia. Rarely, paradoxical or disinhibitory reactions (including agitation, irritability, impulsivity, violent behavior, confusion, restlessness, excitement, and talkativeness) may occur. In severe overdosage cases, patients may develop respiratory depression and coma. Overdosage of benzodiazepines in combination with other CNS depressants (including alcohol and opioids) may be fatal [see Warnings and Precautions (5.2)]. Markedly abnormal (lowered or elevated) blood pressure, heart rate, or respiratory rate raise the concern that additional drugs and/or alcohol are involved in the overdosage.
In managing benzodiazepine overdosage, employ general supportive measures, including intravenous fluids and airway maintenance. Flumazenil, a specific benzodiazepine receptor antagonist indicated for the complete or partial reversal of the sedative effects of benzodiazepines in the management of benzodiazepine overdosage, can lead to withdrawal and adverse reactions, including seizures, particularly in the context of mixed overdosage with drugs that increase seizure risk (e.g., tricyclic and tetracyclic antidepressants) and in patients with long-term benzodiazepine use and physical dependency. The risk of withdrawal seizures with flumazenil use may be increased in patients with epilepsy. Flumazenil is contraindicated in patients who have received a benzodiazepine for control of a potentially life-threatening condition (e.g., status epilepticus). If the decision is made to use flumazenil, it should be used as an adjunct to, not as a substitute for, supportive management of benzodiazepine overdosage. See the flumazenil injection Prescribing Information.
Consider contacting the Poison Help line (1-800-222-1222) or a medical toxicologist for additional overdosage management recommendations.
11. Valtoco Description
Diazepam, the active ingredient of VALTOCO nasal spray, is a benzodiazepine anticonvulsant with the chemical name 7-chloro-1,3-dihydro-1-methyl-5-phenyl-2H-1,4-benzodiazepin-2-one. The structural formula is as follows:
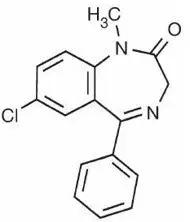
The inactive ingredients in VALTOCO nasal spray include benzyl alcohol (10.5 mg per 0.1 mL), dehydrated alcohol, n-dodecyl beta-D-maltoside, and vitamin E. VALTOCO nasal spray is a clear pale amber liquid.
12. Valtoco - Clinical Pharmacology
12.1 Mechanism of Action
The exact mechanism of action for diazepam is not fully understood, but it is thought to involve potentiation of GABAergic neurotransmission resulting from binding at the benzodiazepine site of the GABAA receptor.
12.2 Pharmacodynamics
The effects of diazepam on the CNS are dependent on the dose administered, the route of administration, and the presence or absence of other medications.
14. Clinical Studies
The efficacy of VALTOCO is based on the relative bioavailability of VALTOCO nasal spray compared to diazepam rectal gel in healthy adults [see Clinical Pharmacology (12.3)].
The effectiveness of diazepam rectal gel has been established in two adequate and well-controlled clinical studies in children and adults exhibiting seizure patterns.
A randomized, double-blind study compared sequential doses of diazepam rectal gel and placebo in 91 patients (47 children, 44 adults) exhibiting the appropriate seizure profile. The first dose was given at the onset of an identified episode. Children were dosed again four hours after the first dose and were observed for a total of 12 hours. Adults were dosed at four and 12 hours after the first dose and were observed for a total of 24 hours. Primary outcomes for this study were seizure frequency during the period of observation and a global assessment that took into account the severity and nature of the seizures as well as their frequency.
The median seizure frequency for the diazepam rectal gel treated group was zero seizures per hour, compared to a median seizure frequency of 0.3 seizures per hour for the placebo group, a difference that was statistically significant (p < 0.0001). All three categories of the global assessment (seizure frequency, seizure severity, and "overall") were also found to be statistically significant in favor of diazepam rectal gel (p < 0.0001). The following histogram displays the results for the "overall" category of the global assessment.
Figure 1: Caregiver Overall Global Assessment of the Efficacy of Diazepam Rectal Gel
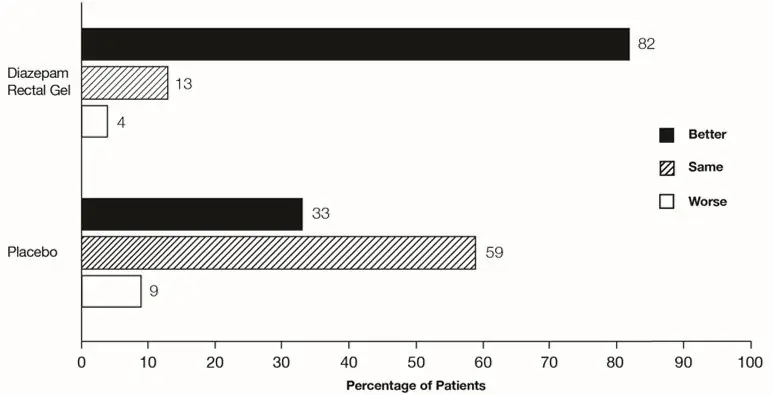
Patients treated with diazepam rectal gel experienced prolonged time-to-next-seizure compared to placebo (p = 0.0002) as shown in the following graph.
Figure 2: Kaplan-Meier Survival Analysis of Time-to-Next-Seizure - First Study
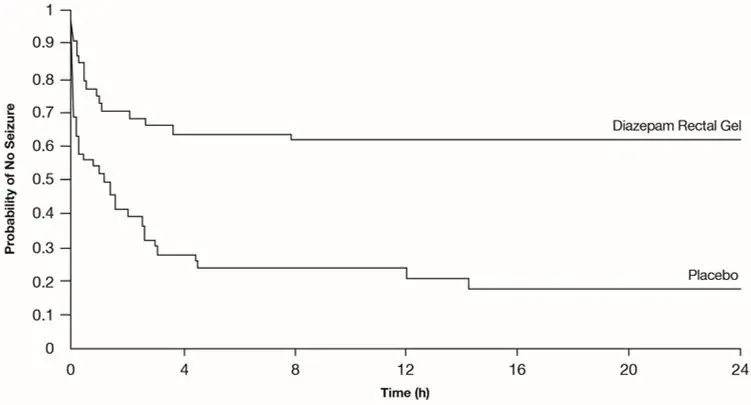
In addition, 62% of patients treated with diazepam rectal gel were seizure-free during the observation period compared to 20% of placebo patients.
Analysis of response by gender and age revealed no substantial differences between treatment in either of these subgroups. Analysis of response by race was considered unreliable, due to the small percentage of non-Caucasians.
A second double-blind study compared single doses of diazepam rectal gel and placebo in 114 patients (53 children, 61 adults). The dose was given at the onset of the identified episode and patients were observed for a total of 12 hours. The primary outcome in this study was seizure frequency. The median seizure frequency for the diazepam rectal gel-treated group was zero seizures per 12 hours, compared to a median seizure frequency of 2.0 seizures per 12 hours for the placebo group, a difference that was statistically significant (p < 0.03). Patients treated with diazepam rectal gel experienced prolonged time-to-next-seizure compared to placebo (p = 0.0072) as shown in Figure 3.
Figure 3: Kaplan-Meier Survival Analysis of Time-to-Next-Seizure - Second Study
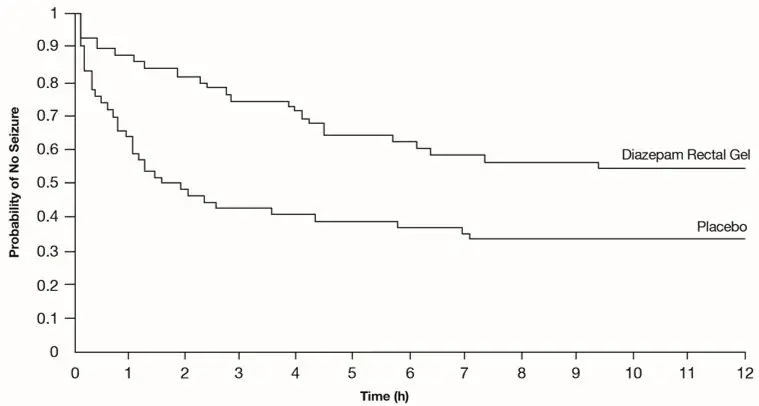
In addition, 55% of patients treated with diazepam rectal gel were seizure-free during the observation period compared to 34% of patients receiving placebo. Overall, caregivers judged diazepam rectal gel to be more effective than placebo (p = 0.018), based on a 10 centimeter visual analog scale. In addition, investigators also evaluated the effectiveness of diazepam rectal gel and judged diazepam rectal gel to be more effective than placebo (p < 0.001).
An analysis of response by gender revealed a statistically significant difference between treatments in females but not in males in this study, and the difference between the 2 genders in response to the treatments reached borderline statistical significance. Analysis of response by race was considered unreliable, due to the small percentage of non-Caucasians.
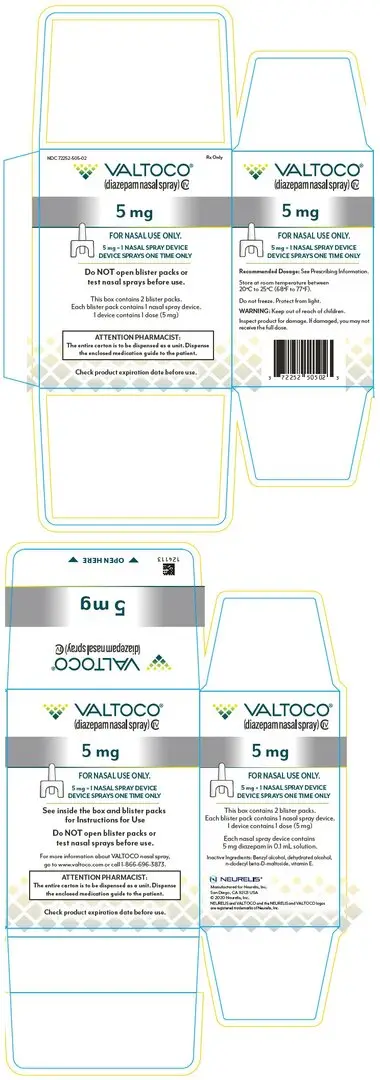
16. How is Valtoco supplied
16.1 How Supplied
VALTOCO is available in 5 mg, 7.5 mg, and 10 mg strengths. VALTOCO is supplied and packaged in doses of 5 mg, 10 mg, 15 mg, or 20 mg (see Table 4).
| Description | Contents | NDC |
|---|---|---|
| 5 mg carton | 2 individual blister packs, each containing one 5 mg nasal spray device | 72252-505-02 |
| 10 mg carton | 2 individual blister packs, each containing one 10 mg nasal spray device | 72252-510-02 |
| 15 mg carton | 2 individual blister packs, each containing two 7.5 mg nasal spray devices | 72252-515-04 |
| 20 mg carton | 2 individual blister packs, each containing two 10 mg nasal spray devices | 72252-520-04 |
16.2 Storage and Handling
Do not open individual blister packs or test nasal spray devices before use.
Each single-dose nasal spray device sprays one (1) time and cannot be re-used.
Do not use if the nasal spray unit appears damaged.
Store VALTOCO at 20°C to 25°C (68°F to 77°F); excursions permitted from 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature]. Do not freeze. Protect from light.
17. Patient Counseling Information
Advise the patient and/or caregiver to read the FDA-approved patient labeling (Medication Guide and Instructions for Use).
| MEDICATION GUIDE VALTOCO® (val-toe-koe) (diazepam nasal spray), CIV |
||||
|---|---|---|---|---|
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised: 01/2023 | |||
|
What is the most important information I should know about VALTOCO? |
||||
|
||||
|
||||
|
||||
|
||||
|
||||
|
|
|||
|
||||
| What is VALTOCO? | ||||
|
||||
|
||||
| Before using VALTOCO, tell your healthcare provider about all of your medical conditions, including if you: | ||||
|
||||
| Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Using VALTOCO with certain other medicines can cause side effects or affect how well VALTOCO or the other medicines work. Do not start or stop other medicines without talking to your healthcare provider. | ||||
| How should I use VALTOCO? | ||||
|
||||
| What should I do after I give VALTOCO? | ||||
|
||||
| If needed, a second dose may be given at least 4 hours after the first dose, using a new pack of VALTOCO. Do not give more than 2 doses of VALTOCO to treat a seizure cluster. A second dose should not be given if there is concern about the person's breathing, they need help with their breathing, or have extreme drowsiness. |
||||
| Do not use VALTOCO for more than 1 seizure cluster episode every 5 days. Do not use VALTOCO for more than 5 seizure cluster episodes in 1 month. | ||||
| What should I avoid while using VALTOCO?
See "What is the most important information I should know about VALTOCO?" What are the possible side effects of VALTOCO? VALTOCO may cause serious side effects, including: |
||||
|
||||
| The most common side effects of VALTOCO include: | ||||
|
|
|
||
| These are not all of the possible side effects of VALTOCO. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||||
| How should I store VALTOCO? | ||||
|
||||
| General information about the safe and effective use of VALTOCO. | ||||
| Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use VALTOCO for a condition for which it was not prescribed. Do not give VALTOCO to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about VALTOCO that is written for health professionals. | ||||
| What are the ingredients in VALTOCO? | ||||
| Active ingredient: diazepam | ||||
| Inactive ingredients: benzyl alcohol, dehydrated alcohol, n-dodecyl beta-D-maltoside, and vitamin E. | ||||
| Distributed by Neurelis, Inc., San Diego, CA 92121 USA. NEURELIS and VALTOCO and the NEURELIS and VALTOCO logos are registered trademarks of Neurelis, Inc. For more information, go to www.valtoco.com or call 1-866-696-3873. |
||||
| VALTOCO
diazepam spray |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| VALTOCO
diazepam spray |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| VALTOCO
diazepam spray |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| VALTOCO
diazepam spray |
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
|
|||||||||||||||||||||||||
| Labeler - Neurelis, Inc (080524527) |