Drug Detail:Videx ec (Didanosine [ dye-dan-oh-seen ])
Drug Class: Nucleoside reverse transcriptase inhibitors (NRTIs)
Highlights of Prescribing Information
Enteric-Coated Beadlets
Initial U.S. Approval: 1991
WARNING: PANCREATITIS, LACTIC ACIDOSIS andHEPATOMEGALY with STEATOSIS
See full prescribing information for complete boxed warning.
- Fatal and nonfatal pancreatitis. VIDEX EC should be suspended in patients with suspected pancreatitis and discontinued in patients with confirmed pancreatitis. (5.1)
- Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases. Suspend treatment if clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity occur. Fatal lactic acidosis has been reported in pregnant individuals who received the combination of didanosine and stavudine. (5.2) Coadministration of VIDEX EC with stavudine is contraindicated. (4)
Indications and Usage for Videx EC
VIDEX EC (didanosine, USP) is a nucleoside reverse transcriptase inhibitor for use in combination with other antiretroviral agents for the treatment of human immunodeficiency virus (HIV)-1 infection. (1)
Videx EC Dosage and Administration
- •
- Adult patients: Administered on an empty stomach. Dosing is based on body weight. (2.1)
- •
- Pediatric patients: Ages 6 to 18 years, can safely swallow capsules and body weight at least 20 kg. Administered on an empty stomach, dosing is based on body weight. (2.1)
|
Body Weight |
Dose |
|
20 kg to less than 25 kg |
200 mg once daily |
|
25 kg to less than 60 kg |
250 mg once daily |
|
at least 60 kg |
400 mg once daily |
- •
- Renal impairment: Dose reduction is recommended. (2.2)
- •
- Coadministration with tenofovir: Dose reduction is recommended. Patients should be monitored closely for didanosine-associated adverse reactions. (2.3, 7.1)
Dosage Forms and Strengths
Capsules: 125 mg, 200 mg, 250 mg, 400 mg (3)
Contraindications
Coadministration with stavudine, allopurinol or ribavirin is contraindicated. (4)
Warnings and Precautions
- Pancreatitis: Suspension or discontinuation of didanosine may be necessary. (5.1) Coadministration of VIDEX EC with stavudine is contraindicated. (4)
- Lactic acidosis and severe hepatomegaly with steatosis: Suspend didanosine in patients who develop clinical symptoms or signs with or without laboratory findings. (5.2)
- Hepatic toxicity: Interruption or discontinuation of didanosine must be considered upon worsening of liver disease. (5.3) Coadministration of VIDEX EC with stavudine is contraindicated. (4)
- Non-cirrhotic portal hypertension: Discontinue didanosine in patients with evidence of non-cirrhotic portal hypertension. (5.4)
- Patients may develop peripheral neuropathy (5.5), retinal changes and optic neuritis (5.6), immune reconstitution syndrome (5.7), and lipoatrophy (5.8).
Adverse Reactions/Side Effects
- •
- In adults, the most common adverse reactions (greater than 10%, all grades) are diarrhea, peripheral neurologic symptoms/neuropathy, nausea, headache, rash, and vomiting. (6.1)
- •
- Adverse reactions in pediatric patients were consistent with those in adults. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Bristol-Myers Squibb at 1-800-721-5072 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
Coadministration of VIDEX EC can alter the concentration of other drugs and other drugs may alter the concentration of didanosine. The potential drug-drug interactions must be considered prior to and during therapy. (4, 7, 12.3)
Use In Specific Populations
- Pregnancy: Fatal lactic acidosis has been reported in pregnant individuals who received both didanosine and stavudine with other agents. Coadministration of VIDEX EC with stavudine is contraindicated. (4, 5.2, 8.1)
- Lactation: Breastfeeding is not recommended due to the potential for HIV-1 transmission. (8.2)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 12/2020
Full Prescribing Information
WARNING: PANCREATITIS, LACTIC ACIDOSIS and HEPATOMEGALY with STEATOSIS
Fatal and nonfatal pancreatitis has occurred during therapy with didanosine used alone or in combination regimens in both treatment-naive and treatment-experienced patients, regardless of degree of immunosuppression. VIDEX EC should be suspended in patients with suspected pancreatitis and discontinued in patients with confirmed pancreatitis [see Warnings and Precautions (5.1)].
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination, including didanosine and other antiretrovirals. Fatal lactic acidosis has been reported in pregnant individuals who received the combination of didanosine and stavudine with other antiretroviral agents. Coadministration of VIDEX EC and stavudine is contraindicated because of increased risk of serious and/or life-threatening events [see Contraindications (4) and Warnings and Precautions (5.2)]. Suspend treatment if clinical or laboratory findings suggestive of lactic acidosis or pronounced hepatotoxicity occurs.
1. Indications and Usage for Videx EC
VIDEX® EC (didanosine, USP), also known as ddI, in combination with other antiretroviral agents is indicated for the treatment of human immunodeficiency virus (HIV)-1 infection [see Clinical Studies (14)].
2. Videx EC Dosage and Administration
VIDEX EC should be administered on an empty stomach. VIDEX EC Delayed-Release Capsules should be swallowed intact.
2.1 Recommended Dosage (Adult and Pediatric Patients)
The recommended total daily dose is based on body weight and is administered as one capsule given on a once-daily schedule as outlined in Table 1.
The recommended total daily dose to be administered once daily to pediatric patients weighing at least 20 kg who can swallow capsules is based on body weight (kg), consistent with the recommended adult dosing guidelines (see Table 1). Please consult the complete prescribing information for VIDEX (didanosine) Pediatric Powder for Oral Solution for dosage and administration of didanosine to pediatric patients weighing less than 20 kg or who can not swallow capsules.
|
Body Weight |
Dose |
|
20 kg to less than 25 kg |
200 mg once daily |
|
25 kg to less than 60 kg |
250 mg once daily |
|
at least 60 kg |
400 mg once daily |
2.2 Renal Impairment
Dosing recommendations for VIDEX EC and VIDEX Pediatric Powder for Oral Solution are different for patients with renal impairment. Please consult the complete prescribing information on administration of VIDEX (didanosine) Pediatric Powder for Oral Solution to patients with renal impairment.
Adult Patients
In adult patients with impaired renal function, the dose of VIDEX EC should be adjusted to compensate for the slower rate of elimination. The recommended doses and dosing intervals of VIDEX EC in adult patients with renal insufficiency are presented in Table 2.
| Creatinine Clearance
(mL/min) | Dosage (mg) | |
|---|---|---|
| at least 60 kg | less than 60 kg | |
| a Based on studies using a buffered formulation of didanosine. b Not suitable for use in patients less than 60 kg with CLcr less than 10 mL/min. An alternate formulation of didanosine should be used. |
||
|
at least 60 |
400 once daily |
250 once daily |
|
30-59 |
200 once daily |
125 once daily |
|
10-29 |
125 once daily |
125 once daily |
|
less than 10 |
125 once daily |
b |
Pediatric Patients
Urinary excretion is also a major route of elimination of didanosine in pediatric patients, therefore the clearance of didanosine may be altered in pediatric patients with renal impairment. Although there are insufficient data to recommend a specific dose adjustment of VIDEX EC in this patient population, a reduction in the dose should be considered (see Table 2).
Patients Requiring Continuous Ambulatory Peritoneal Dialysis (CAPD) or Hemodialysis
For patients requiring CAPD or hemodialysis, follow dosing recommendations for patients with creatinine clearance of less than 10 mL/min, shown in Table 2. It is not necessary to administer a supplemental dose of didanosine following hemodialysis.
2.3 Dose Adjustment
Concomitant Therapy with Tenofovir Disoproxil Fumarate
In patients who are also taking tenofovir disoproxil fumarate, a dose reduction of VIDEX EC to 250 mg (adults weighing at least 60 kg with creatinine clearance of at least 60 mL/min) or 200 mg (adults weighing less than 60 kg with creatinine clearance of at least 60 mL/min) once daily taken together with tenofovir disoproxil fumarate and a light meal (400 kilocalories or less, 20% fat or less) or in the fasted state is recommended. The appropriate dose of VIDEX EC coadministered with tenofovir disoproxil fumarate in patients with creatinine clearance of less than 60 mL/min has not been established [see Drug Interactions (7) and Clinical Pharmacology (12.3)].
3. Dosage Forms and Strengths
VIDEX EC (didanosine, USP) Delayed-Release Capsules are white, opaque capsules as described below:
- •
- 125 mg capsule imprinted with “BMS 125 mg 6671” in Tan
- •
- 200 mg capsule imprinted with “BMS 200 mg 6672” in Green
- •
- 250 mg capsule imprinted with “BMS 250 mg 6673” in Blue
- •
- 400 mg capsule imprinted with “BMS 400 mg 6674” in Red
4. Contraindications
VIDEX EC is contraindicated when coadministered with the following medications:
- Stavudine- potential for serious and/or life-threatening events, notably pancreatitis, lactic acidosis, hepatotoxicity, and peripheral neuropathy [see Warnings and Precautions (5.1, 5.2, 5.3, 5.5)].
- Allopurinol- systemic exposures of didanosine are increased, which may increase didanosine-associated toxicity [see Clinical Pharmacology (12.3)].
- Ribavirin- exposures of the active metabolite of didanosine (dideoxyadenosine 5′-triphosphate) are increased. Fatal hepatic failure, as well as peripheral neuropathy, pancreatitis, and symptomatic hyperlactatemia/lactic acidosis have been reported in patients receiving both didanosine and ribavirin.
5. Warnings and Precautions
5.1 Pancreatitis
Fatal and nonfatal pancreatitis has occurred during therapy with didanosine used alone or in combination regimens in both treatment-naive and treatment-experienced patients, regardless of degree of immunosuppression. VIDEX EC should be suspended in patients with signs or symptoms of pancreatitis and discontinued in patients with confirmed pancreatitis. Patients treated with VIDEX EC in combination with stavudine may be at increased risk for pancreatitis; the coadministration of VIDEX EC and stavudine is contraindicated [see Contraindications (4)].
When treatment with life-sustaining drugs known to cause pancreatic toxicity is required, suspension of VIDEX EC (didanosine) therapy is recommended. In patients with risk factors for pancreatitis, VIDEX EC should be used with extreme caution and only if clearly indicated. Patients with advanced HIV-1 infection, especially the elderly, are at increased risk of pancreatitis and should be followed closely. Patients with renal impairment may be at greater risk for pancreatitis if treated without dose adjustment. The frequency of pancreatitis is dose related. [see Adverse Reactions (6)].
5.2 Lactic Acidosis/Severe Hepatomegaly with Steatosis
Lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination, including didanosine and other antiretrovirals. A majority of these cases have been in women. Obesity and prolonged nucleoside exposure may be risk factors. Fatal lactic acidosis has been reported in pregnant individuals who received the combination of didanosine and stavudine with other antiretroviral agents. Coadministration of VIDEX EC and stavudine is contraindicated [see Contraindications (4) and Use in Specific Populations (8.1)]. Particular caution should be exercised when administering VIDEX EC to any patient with known risk factors for liver disease; however, cases have also been reported in patients with no known risk factors. Treatment with VIDEX EC should be suspended in any patient who develops clinical signs or symptoms with or without laboratory findings consistent with symptomatic hyperlactatemia, lactic acidosis, or pronounced hepatotoxicity (which may include hepatomegaly and steatosis even in the absence of marked transaminase elevations).
5.3 Hepatic Toxicity
The safety and efficacy of VIDEX EC have not been established in HIV-infected patients with significant underlying liver disease. During combination antiretroviral therapy, patients with preexisting liver dysfunction, including chronic active hepatitis, have an increased frequency of liver function abnormalities, including severe and potentially fatal hepatic adverse events, and should be monitored according to standard practice. If there is evidence of worsening liver disease in such patients, interruption or discontinuation of treatment must be considered.
Hepatotoxicity and hepatic failure resulting in death were reported during postmarketing surveillance in HIV-infected patients treated with hydroxyurea and other antiretroviral agents. Fatal hepatic events were reported most often in patients treated with the combination of hydroxyurea, didanosine, and stavudine. Coadministration of VIDEX EC and stavudine is contraindicated; the combination of VIDEX EC and hydroxyurea should be avoided. [see Contraindications (4) and Drug Interactions (7.2)].
5.4 Non-cirrhotic Portal Hypertension
Postmarketing cases of non-cirrhotic portal hypertension have been reported, including cases leading to liver transplantation or death. Cases of didanosine-associated non-cirrhotic portal hypertension were confirmed by liver biopsy in patients with no evidence of viral hepatitis. Onset of signs and symptoms ranged from months to years after start of didanosine therapy. Common presenting features included elevated liver enzymes, esophageal varices, hematemesis, ascites, and splenomegaly.
Patients receiving VIDEX EC should be monitored for early signs of portal hypertension (e.g., thrombocytopenia and splenomegaly) during routine medical visits. Appropriate laboratory testing including liver enzymes, serum bilirubin, albumin, complete blood count, and international normalized ratio (INR) and ultrasonography should be considered. VIDEX EC should be discontinued in patients with evidence of non-cirrhotic portal hypertension.
5.5 Peripheral Neuropathy
Peripheral neuropathy, manifested by numbness, tingling, or pain in the hands or feet, has been reported in patients receiving didanosine therapy. Peripheral neuropathy has occurred more frequently in patients with advanced HIV disease, in patients with a history of neuropathy, or in patients being treated with neurotoxic drug therapy. Discontinuation of VIDEX EC should be considered in patients who develop peripheral neuropathy [see Contraindications (4), Adverse Reactions (6), and Drug Interactions (7.2)].
5.6 Retinal Changes and Optic Neuritis
Retinal changes and optic neuritis have been reported in patients taking didanosine. Periodic retinal examinations should be considered for patients receiving VIDEX EC [see Adverse Reactions (6)].
5.7 Immune Reconstitution Syndrome
Immune reconstitution syndrome has been reported in patients treated with combination antiretroviral therapy, including VIDEX EC. During the initial phase of combination antiretroviral treatment, patients whose immune system responds may develop an inflammatory response to indolent or residual opportunistic infections (such as Mycobacterium avium infection, cytomegalovirus, Pneumocystis jiroveci pneumonia [PCP], or tuberculosis), which may necessitate further evaluation and treatment.
Autoimmune disorders (such as Graves’ disease, polymyositis, and Guillain-Barré syndrome) have also been reported to occur in the setting of immune reconstitution; however, the time to onset is more variable, and can occur many months after initiation of treatment.
5.8 Lipoatrophy
Treatment with VIDEX EC has been associated with loss of subcutaneous fat, which is most evident in the face, limbs, and buttocks. The incidence and severity of lipoatrophy are related to cumulative exposure, and is often not reversible when VIDEX EC treatment is stopped. Patients receiving VIDEX EC should be frequently examined and questioned for signs of lipoatrophy, and if feasible, therapy should be switched to an alternative regimen if there is suspicion of lipoatrophy.
6. Adverse Reactions/Side Effects
The following adverse reactions are discussed in greater detail in other sections:
- Pancreatitis [see Warnings and Precautions (5.1)]
- Lactic acidosis/severe hepatomegaly with steatosis [see Warnings and Precautions (5.2)]
- Hepatic toxicity [see Warnings and Precautions (5.3)]
- Non-cirrhotic portal hypertension [see Warnings and Precautions (5.4)]
- Peripheral neuropathy [see Warnings and Precautions (5.5)]
- Retinal changes and optic neuritis [see Warnings and Precautions (5.6)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Clinical Trials Experience in Adult Subjects
Study AI454-152 was a 48-week, randomized, open-label study comparing VIDEX EC (400 mg once daily) plus stavudine (40 mg twice daily) plus nelfinavir (750 mg three times daily) to zidovudine (300 mg) plus lamivudine (150 mg) combination tablets twice daily plus nelfinavir (750 mg three times daily) in 511 treatment-naive patients. Selected clinical adverse reactions that occurred in combination with other antiretroviral agents are provided in Table 3.
| Adverse Reactions | Percent of Patientsb,c | |
|---|---|---|
| VIDEX EC + stavudine
+ nelfinavir n=258 | zidovudine/lamivudined
+ nelfinavir n=253 |
|
| a Median duration of treatment was 62 weeks in the VIDEX EC + stavudine + nelfinavir group and 61 weeks in the zidovudine/lamivudine + nelfinavir group. b Percentages based on treated patients. c The incidences reported included all severity grades and all reactions regardless of causality. d Zidovudine/lamivudine combination tablet. * This event was not observed in this study arm. |
||
|
Diarrhea |
57 |
58 |
|
Peripheral Neurologic Symptoms/Neuropathy |
25 |
11 |
|
Nausea |
24 |
36 |
|
Headache |
22 |
17 |
|
Rash |
14 |
12 |
|
Vomiting |
14 |
19 |
|
Pancreatitis (see below) |
less than 1 |
* |
In clinical trials using a buffered formulation of didanosine, pancreatitis resulting in death was observed in one patient who received didanosine plus stavudine plus nelfinavir, one patient who received didanosine plus stavudine plus indinavir, and 2 of 68 patients who received didanosine plus stavudine plus indinavir plus hydroxyurea. In an early access program, pancreatitis resulting in death was observed in one patient who received VIDEX EC plus stavudine plus hydroxyurea plus ritonavir plus indinavir plus efavirenz [see Warnings and Precautions (5)].
The frequency of pancreatitis is dose related. In phase 3 studies with buffered formulations of didanosine, incidence ranged from 1% to 10% with doses higher than are currently recommended and 1% to 7% with recommended dose.
Selected laboratory abnormalities that occurred in a study of VIDEX EC in combination with other antiretroviral agents are shown in Table 4.
| Percent of Patientsb | |||||||
|---|---|---|---|---|---|---|---|
| VIDEX EC + stavudine
+ nelfinavir n=258 | zidovudine/lamivudinec
+ nelfinavir n=253 |
||||||
| Parameter | Grades 3-4d | All Grades | Grades 3-4d | All Grades | |||
| a Median duration of treatment was 62 weeks in the VIDEX EC + stavudine + nelfinavir group and 61 weeks in the zidovudine/lamivudine + nelfinavir group. b Percentages based on treated patients. c Zidovudine/lamivudine combination tablet. d Greater than 5 × ULN for SGOT and SGPT, at least 2.1 × ULN for lipase, and at least 2.6 × ULN for bilirubin (ULN = upper limit of normal). |
|||||||
|
SGOT (AST) |
5 |
46 |
5 |
19 |
|||
|
SGPT (ALT) |
6 |
44 |
5 |
22 |
|||
|
Lipase |
5 |
23 |
2 |
13 |
|||
|
Bilirubin |
less than 1 |
9 |
less than 1 |
3 |
|||
Clinical Trials Experience in Pediatric Patients
In clinical trials, 743 pediatric patients between 2 weeks and 18 years of age have been treated with didanosine. Adverse reactions and laboratory abnormalities reported to occur in these patients were generally consistent with the safety profile of didanosine in adults.
In pediatric phase 1 studies, pancreatitis occurred in 2 of 60 (3%) patients treated at entry doses below 300 mg/m2/day and in 5 of 38 (13%) patients treated at higher doses. In study ACTG 152, pancreatitis occurred in none of the 281 pediatric patients who received didanosine 120 mg/m2 every 12 hours and in less than 1% of the 274 pediatric patients who received didanosine 90 mg/m2 every 12 hours in combination with zidovudine [see Clinical Studies (14)].
Retinal changes and optic neuritis have been reported in pediatric patients.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of didanosine. Because they are reported voluntarily from a population of unknown size, estimates of frequency cannot be made. These reactions have been chosen for inclusion due to their seriousness, frequency of reporting, causal connection to VIDEX EC, or a combination of these factors.
Blood and Lymphatic System Disorders - anemia, leukopenia, and thrombocytopenia.
Body as a Whole - abdominal pain, alopecia, anaphylactoid reaction, asthenia, chills/fever, pain.
Digestive Disorders - anorexia, dyspepsia, and flatulence.
Exocrine Gland Disorders - pancreatitis (including fatal cases) [see Warnings and Precautions (5.1)], sialoadenitis, parotid gland enlargement, dry mouth, and dry eyes.
Hepatobiliary Disorders - symptomatic hyperlactatemia/lactic acidosis and hepatic steatosis [see Warnings and Precautions (5.2)]; non-cirrhotic portal hypertension [see Warnings and Precautions (5.4)]; hepatitis and liver failure.
Metabolic Disorders - diabetes mellitus, elevated serum alkaline phosphatase level, elevated serum amylase level, elevated serum gamma-glutamyltransferase level, elevated serum uric acid level, hypoglycemia, and hyperglycemia.
Musculoskeletal Disorders - myalgia (with or without increases in creatine kinase), rhabdomyolysis including acute renal failure and hemodialysis, arthralgia, and myopathy.
Ophthalmologic Disorders - retinal depigmentation and optic neuritis [see Warnings and Precautions (5.6)].
7. Drug Interactions
7.1 Established Drug Interactions
Clinical recommendations based on the results of drug interaction studies are listed in Table 5. Pharmacokinetic results of drug interaction studies are shown in Tables 9-12 [see Contraindications (4), Clinical Pharmacology (12.3)].
| Drug | Effect | Clinical Comment |
|---|---|---|
| ↑ Indicates increase. ↓ Indicates decrease. a Coadministration of didanosine with food decreases didanosine concentrations. Thus, although not studied, it is possible that coadministration with heavier meals could reduce didanosine concentrations further. |
||
|
ganciclovir |
↑ didanosine concentration |
If there is no suitable alternative to ganciclovir, then use in combination with VIDEX EC with caution. Monitor for didanosine-associated toxicity. |
|
methadone |
↓ didanosine concentration |
If coadministration of methadone and didanosine is necessary, the recommended formulation of didanosine is VIDEX EC. Patients should be closely monitored for adequate clinical response when VIDEX EC is coadministered with methadone, including monitoring for changes in HIV RNA viral load. Do not coadminister methadone with VIDEX pediatric powder due to significant decreases in didanosine concentrations. |
|
nelfinavir |
No interaction 1 hour after didanosine |
Administer nelfinavir 1 hour after VIDEX EC. |
|
tenofovir disoproxil fumarate |
↑ didanosine concentration |
A dose reduction of VIDEX EC to the following dosage once daily taken together with tenofovir disoproxil fumarate and a light meal (400 kilocalories or less and 20% fat or less) or in the fasted state is recommended.a
Patients should be monitored for didanosine-associated toxicities and clinical response. |
Exposure to didanosine is increased when coadministered with tenofovir disoproxil fumarate [Table 5 and see Clinical Pharmacokinetics (12.3, Tables 9 and 10)]. Increased exposure may cause or worsen didanosine-related clinical toxicities, including pancreatitis, symptomatic hyperlactatemia/lactic acidosis, and peripheral neuropathy. Coadministration of tenofovir disoproxil fumarate with VIDEX EC should be undertaken with caution, and patients should be monitored closely for didanosine-related toxicities and clinical response. VIDEX EC should be suspended if signs or symptoms of pancreatitis, symptomatic hyperlactatemia, or lactic acidosis develop [see Dosage and Administration (2.3), Warnings and Precautions (5)]. Suppression of CD4 cell counts has been observed in patients receiving tenofovir disoproxil fumarate with didanosine at a dose of 400 mg daily.
7.2 Predicted Drug Interactions
Predicted drug interactions with VIDEX EC are listed in Table 6.
| Drug or Drug Class | Effect | Clinical Comment |
|---|---|---|
| ↑ Indicates increase. a Only if other drugs are not available and if clearly indicated. If treatment with life-sustaining drugs that cause pancreatic toxicity is required, suspension of VIDEX EC is recommended [see Warnings and Precautions (5.1)]. b [see Warnings and Precautions (5.6)]. |
||
|
Drugs that may cause pancreatic toxicity |
↑ risk of pancreatitis |
Use only with extreme caution.a |
|
Neurotoxic drugs |
↑ risk of neuropathy |
Use with caution.b |
|
Hydroxyurea |
↑ risk of pancreatitis, |
Use should be avoided. |
8. Use In Specific Populations
8.1 Pregnancy
Pregnancy Exposure Registry
There is a pregnancy exposure registry that monitors pregnancy outcomes in individuals exposed to VIDEX EC during pregnancy. Healthcare providers are encouraged to register patients by calling the Antiretroviral Pregnancy Registry (APR) at 1-800-258-4263.
Risk Summary
Fatal lactic acidosis has been reported in pregnant individuals who received the combination of didanosine and stavudine with other antiretroviral agents. It is unclear if pregnancy augments the risk of lactic acidosis/hepatic steatosis syndrome reported in nonpregnant individuals receiving nucleoside analogues [see Warnings and Precautions (5.2)]. Coadministration of VIDEX EC and stavudine is contraindicated [see Contraindications (4)].
Based on APR reports, congenital malformations were reported when administered during pregnancy. The prevalence of birth defects was 4.7% in the first trimester compared with 2.7% in the U.S. reference population of the Metropolitan Atlanta Congenital Defects Program (MACDP) and 4.2% in the Texas Birth Defects Registry (TBDR) (see Data). No pattern of defects was identified by the APR. Based on these findings, the clinical relevance is uncertain.
The rate of miscarriage is not reported in the APR. In the U.S. general population, the estimated background risks of miscarriage in clinically recognized pregnancies is 15 to 20%, respectively.
In animal reproduction studies, no evidence of adverse developmental outcomes was observed with didanosine at systemic exposures (AUC) up to 12 (rats) and 14 (rabbits) times the exposure in humans at the recommended daily human dose of VIDEX EC (see Data).
Clinical Considerations
Maternal Adverse Reactions
Cases of lactic acidosis syndrome, sometimes fatal, have occurred in pregnant individuals using VIDEX EC in combination with stavudine. VIDEX EC is associated with an increased risk of lactic acidosis syndrome/hepatic steatosis syndrome [see Warnings and Precautions (5.2)]
Data
Human Data
Based on prospective reports to the APR of exposure to didanosine-containing regimens during pregnancy (including 427 exposed in the first trimester and 462 exposed in the second/third trimester), the prevalence of birth defects in live births was 4.7% (95% CI: 2.9% to 7.1%) with first trimester exposure to didanosine-containing regimens and 4.3% (95% CI: 2.7% to 6.6%) with the second/third trimester exposure to didanosine-containing regimens compared with the background birth defect rate of 2.7% in the U.S. reference population of the MACDP and 4.2% in the TBDR.
Prospective reports from the APR of overall major birth defects in pregnancies exposed to VIDEX EC is compared with a U.S.
background major birth defect rate. Methodological limitations of the APR include the use of MACDP and TBDR as the external comparator groups. Limitations of using external comparators include differences in methodology and populations, as well as confounding due to the underlying disease.
Animal Data
Didanosine was administered orally at up to 1000 mg per kg daily to pregnant rats and at up to 600 mg per kg daily to pregnant rabbits on gestation Days 7 to 17 and 6 to 18, respectively, and also to rats 14 days before mating through weaning. No adverse effects on embryo-fetal development (rats and rabbits) were observed up to the highest dose tested. During organogenesis, systemic exposures (AUC) to didanosine were up to 12 (rats) and 14.2 (rabbits) times the estimated human exposure at the recommended daily human dose. Didanosine and/or its metabolites are transferred to the fetus through the placenta. In the rat pre/postnatal development study, didanosine administered to pregnant rats reduced food intake and body weight gains in pups at a maternally toxic exposure (approximately 12 times the exposure at the recommended human dose).
8.2 Lactation
Risk Summary
The Centers for Disease Control and Prevention recommend that HIV-1-infected mothers in the United States not breastfeed their infants to avoid risking postnatal transmission of HIV-1 infection. It is not known whether didanosine is present in human breast milk, affects human milk production, or has effects on the breastfed infant. When administered to lactating rats, didanosine was present in milk (see Data).
Because of the potential for (1) HIV-1 transmission (in HIV-negative infants), (2) developing viral resistance (in HIV-positive infants) and (3) adverse reactions in breastfed infants similar to those seen in adults, instruct mothers not to breastfeed if they are receiving VIDEX EC.
Data
Didanosine and its metabolites were excreted into the milk of lactating rats following a single oral dose of 50 mg per kg on lactation Day 14, with milk concentrations 5 times that of maternal plasma concentrations at 8 and 24 hours post-dose.
8.4 Pediatric Use
Use of didanosine in pediatric patients from 2 weeks of age through adolescence is supported by evidence from adequate and well-controlled studies of didanosine in adult and pediatric patients [see Dosage and Administration (2), Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14)]. Additional pharmacokinetic studies in pediatric patients support use of VIDEX EC in pediatric patients who weigh at least 20 kg.
8.5 Geriatric Use
In an Expanded Access Program using a buffered formulation of didanosine for the treatment of advanced HIV infection, patients aged 65 years and older had a higher frequency of pancreatitis (10%) than younger patients (5%) [see Warnings and Precautions (5.1)]. Clinical studies of didanosine, including those for VIDEX EC, did not include sufficient numbers of subjects aged 65 years and over to determine whether they respond differently than younger subjects. Didanosine is known to be substantially excreted by the kidney, and the risk of toxic reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection. In addition, renal function should be monitored and dosage adjustments should be made accordingly [see Dosage and Administration (2.2)].
8.6 Renal Impairment
Patients with renal impairment (creatinine clearance of less than 60 mL/min) may be at greater risk of toxicity from didanosine due to decreased drug clearance [see Clinical Pharmacology (12.3)]. A dose reduction is recommended for these patients [see Dosage and Administration (2)].
10. Overdosage
There is no known antidote for didanosine overdosage. In phase 1 studies, in which buffered formulations of didanosine were initially administered at doses ten times the currently recommended dose, toxicities included: pancreatitis, peripheral neuropathy, diarrhea, hyperuricemia, and hepatic dysfunction. Didanosine is not dialyzable by peritoneal dialysis, although there is some clearance by hemodialysis [see Clinical Pharmacology (12.3)].
11. Videx EC Description
VIDEX® EC is the brand name for an enteric-coated formulation of didanosine, USP, a synthetic purine nucleoside analogue active against HIV-1. VIDEX EC Delayed-Release Capsules, containing enteric-coated beadlets, are available for oral administration in strengths of 125, 200, 250, and 400 mg of didanosine. The inactive ingredients in the beadlets include carboxymethylcellulose sodium 12, diethyl phthalate, methacrylic acid copolymer, sodium hydroxide, sodium starch glycolate, and talc. The capsule shells contain gelatin and titanium dioxide. The capsules are imprinted with edible inks.
Didanosine is also available in a powder formulation. Please consult the prescribing information for VIDEX (didanosine) Pediatric Powder for Oral Solution for additional information.
The chemical name for didanosine is 2′,3′-dideoxyinosine. The structural formula is:
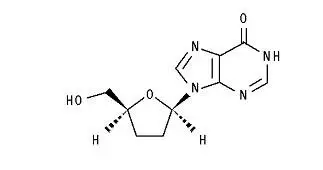
Didanosine is a white crystalline powder with the molecular formula C10H12N4O3 and a molecular weight of 236.2. The aqueous solubility of didanosine at 25° C and pH of approximately 6 is 27.3 mg/mL. Didanosine is unstable in acidic solutions. For example, at pH less than 3 and 37° C, 10% of didanosine decomposes to hypoxanthine in less than 2 minutes. In VIDEX EC, an enteric coating is used to protect didanosine from degradation by stomach acid.
12. Videx EC - Clinical Pharmacology
12.3 Pharmacokinetics
The pharmacokinetic parameters of didanosine in HIV-infected adult and pediatric patients are summarized in Table 7, by weight ranges that correspond to recommended doses (Table 1). Didanosine is rapidly absorbed, with peak plasma concentrations generally observed from 0.25 to 1.50 hours following oral dosing with a buffered formulation. Increases in plasma didanosine concentrations were dose proportional over the range of 50 to 400 mg. In adults, the mean (± standard deviation) oral bioavailability following single oral dosing with a buffered formulation is 42 (±12)%. After oral administration, the urinary recovery of didanosine is approximately 18 (±8)% of the dose. The CSF-plasma ratio following IV administration is 21 (±0.03)%. Steady-state pharmacokinetic parameters did not differ significantly from values obtained after a single dose. Binding of didanosine to plasma proteins in vitro was low (less than 5%). Based on data from in vitro and animal studies, it is presumed that the metabolism of didanosine in man occurs by the same pathways responsible for the elimination of endogenous purines.
| a The pharmacokinetic parameters (mean ± standard deviation) of didanosine were determined by a population pharmacokinetic model based on combined clinical studies. | ||||
|
Parametera |
Pediatrics |
Adults |
||
|
20 kg to less than 25 kg |
25 kg to less than 60 kg |
At least 60 kg |
At least 60 kg |
|
|
Apparent clearance (L/h) |
89.5 ± 21.6 |
116.2 ± 38.6 |
196.0 ± 55.8 |
174.5 ± 69.7 |
|
Apparent volume of distribution (L) |
98.1 ± 30.2 |
154.7 ± 55.0 |
363 ± 137.7 |
308.3 ± 164.3 |
|
Elimination half-life (h) |
0.75 ± 0.13 |
0.92 ± 0.09 |
1.26 ± 0.19 |
1.19 ± 0.21 |
|
Steady-state AUC (mg•h/L) |
2.38 ± 0.66 |
2.36 ± 0.70 |
2.25 ± 0.89 |
2.65 ± 1.07 |
Comparison of Didanosine Formulations
In VIDEX EC, the active ingredient, didanosine, is protected against degradation by stomach acid by the use of an enteric coating on the beadlets in the capsule. The enteric coating dissolves when the beadlets empty into the small intestine, the site of drug absorption. With buffered formulations of didanosine, administration with antacid provides protection from degradation by stomach acid.
In healthy volunteers, as well as subjects infected with HIV-1, the AUC is equivalent for didanosine administered as the VIDEX EC formulation relative to a buffered tablet formulation. The peak plasma concentration (Cmax) of didanosine, administered as VIDEX EC, is reduced approximately 40% relative to didanosine buffered tablets. The time to the peak concentration (Tmax) increases from approximately 0.67 hours for didanosine buffered tablets to 2.0 hours for VIDEX EC.
Effect of Food
In the presence of food, the Cmax and AUC for VIDEX EC were reduced by approximately 46% and 19%, respectively, compared to the fasting state [see Dosage and Administration (2)]. VIDEX EC should be taken on an empty stomach.
Special Populations
Renal Insufficiency: Data from two studies using a buffered formulation of didanosine indicated that the apparent oral clearance of didanosine decreased and the terminal elimination half-life increased as creatinine clearance decreased (see Table 8). Following oral administration, didanosine was not detectable in peritoneal dialysate fluid (n=6); recovery in hemodialysate (n=5) ranged from 0.6% to 7.4% of the dose over a 3-4 hour dialysis period. The absolute bioavailability of didanosine was not affected in patients requiring dialysis. [See Dosage and Administration (2.2)].
| Parameter | Creatinine Clearance (mL/min) | Dialysis Patients
n=11 |
|||
|---|---|---|---|---|---|
| at least 90
n=12 | 60-90
n=6 | 30-59
n=6 | 10-29
n=3 |
||
| ND = not determined due to anuria. CLcr = creatinine clearance. CL/F = apparent oral clearance. CLR = renal clearance. |
|||||
|
CLcr (mL/min) |
112 ± 22 |
68 ± 8 |
46 ± 8 |
13 ± 5 |
ND |
|
CL/F (mL/min) |
2164 ± 638 |
1566 ± 833 |
1023 ± 378 |
628 ± 104 |
543 ± 174 |
|
CLR (mL/min) |
458 ± 164 |
247 ± 153 |
100 ± 44 |
20 ± 8 |
less than 10 |
|
T½ (h) |
1.42 ± 0.33 |
1.59 ± 0.13 |
1.75 ± 0.43 |
2.0 ± 0.3 |
4.1 ± 1.2 |
Hepatic Impairment: The pharmacokinetics of didanosine have been studied in 12 non-HIV-infected subjects with moderate (n=8) to severe (n=4) hepatic impairment (Child-Pugh Class B or C). Mean AUC and Cmax values following a single 400 mg dose of didanosine were approximately 13% and 19% higher, respectively, in patients with hepatic impairment compared to matched healthy subjects. No dose adjustment is needed, because a similar range and distribution of AUC and Cmax values was observed for subjects with hepatic impairment and matched healthy controls. [see Dosage and Administration (2.3)].
Pediatric Patients: The pharmacokinetics of didanosine have been evaluated in HIV-exposed and HIV-infected pediatric patients from birth to adulthood.
A population pharmacokinetic analysis was conducted on pooled didanosine plasma concentration data from 9 clinical trials in 106 pediatric (neonate to 18 years of age) and 45 adult patients (greater than 18 years of age). Results showed that body weight is the primary factor associated with oral clearance. Based on the data analyzed, dosing schedule (once versus twice daily) and formulation (powder for oral solution, tablet, and delayed-release capsule) did not have an effect on oral clearance. Didanosine exposure similar to that at recommended adult doses can be achieved in pediatric patients with a weight-based dosing scheme [see Dosage and Administration (2)].
Geriatric Patients: Didanosine pharmacokinetics have not been studied in patients over 65 years of age [see Use in Specific Populations (8.5)].
Gender: The effects of gender on didanosine pharmacokinetics have not been studied.
Drug Interactions
Tables 9 and 10 summarize the effects on AUC and Cmax, with a 90% confidence interval (CI) when available, following coadministration of VIDEX EC with a variety of drugs. For clinical recommendations based on drug interaction studies for drugs in bold font [see Dosage and Administration (2.3) and Drug Interactions (7.1)].
| % Change of Didanosine
Pharmacokinetic Parametersa |
||||
|---|---|---|---|---|
| Drug | Didanosine Dosage | n | AUC of
Didanosine (90% CI) | Cmax of
Didanosine (90% CI) |
| ↑ Indicates increase. ↓ Indicates decrease. ↔ Indicates no change, or mean increase or decrease of less than 10%. a The 90% confidence intervals for the percent change in the pharmacokinetic parameter are displayed. b All studies conducted in healthy volunteers at least 60 kg with creatinine clearance of at least 60 mL/min. c Tenofovir disoproxil fumarate. d 373 kilocalories, 8.2 grams fat. e Compared with VIDEX EC 250 mg administered alone under fasting conditions. f Compared with VIDEX EC 400 mg administered alone under fasting conditions. g Comparisons are made to historical controls (n=148, pooled from 5 studies) conducted in healthy subjects. The number of subjects evaluated for AUC and Cmax is 15 and 16, respectively. |
||||
|
tenofovir,b,c 300 mg |
400 mg single dose fasting |
26 |
↑ 48% |
↑ 48% |
|
tenofovir,b,c 300 mg |
400 mg single dose |
25 |
↑ 60% |
↑ 64% |
|
tenofovir,b,c 300 mg |
200 mg single dose |
33 |
↑ 16% |
↓ 12% |
|
250 mg single dose |
33 |
↔ |
↓ 20% |
|
|
325 mg single dose |
33 |
↑ 13% |
↓ 11% |
|
|
methadone, chronic maintenance dose |
400 mg single dose |
15, 16g |
↓ 17% |
↓ 16% |
| % Change of Coadministered Drug
Pharmacokinetic Parametersa,b |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Drug | Didanosine Dosage | n | AUC of Coadministered Drug
(90% CI) | Cmax of Coadministered Drug
(90% CI) |
|||||
| ↔ Indicates no change, or mean increase or decrease of less than 10%. a The 90% confidence intervals for the percent change in the pharmacokinetic parameter are displayed. b All studies conducted in healthy volunteers at least 60 kg with creatinine clearance of at least 60 mL/min. c Tenofovir disoproxil fumarate. d 373 kilocalories, 8.2 grams fat. |
|||||||||
|
ciprofloxacin, 750 mg |
400 mg single dose |
16 |
↔ |
↔ |
|||||
|
indinavir, 800 mg |
400 mg single dose |
23 |
↔ |
↔ |
|||||
|
ketoconazole, 200 mg |
400 mg single dose |
21 |
↔ |
↔ |
|||||
|
tenofovir,c 300 mg |
400 mg single dose |
25 |
↔ |
↔ |
|||||
|
tenofovir,c 300 mg |
400 mg single dose |
25 |
↔ |
↔ |
|||||
Didanosine Buffered Formulations: Tables 11 and 12 summarize the effects on AUC and Cmax, with a 90% or 95% CI when available, following coadministration of buffered formulations of didanosine with a variety of drugs. The results of these studies may be expected to apply to VIDEX EC. For most of the listed drugs, no clinically significant pharmacokinetic interactions were noted. For clinical recommendations based on drug interaction studies for drugs in bold font, [see Dosage and Administration (2.3) for Concomitant Therapy with Tenofovir Disoproxil Fumarate), Contraindications (4), and Drug Interactions (7.1)].
| % Change of Didanosine
Pharmacokinetic Parametersa |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Drug | Didanosine Dosage | n | AUC of Didanosine
(95% CI) | Cmax of Didanosine
(95% CI) |
||||||||||
| ↑ Indicates increase. ↓ Indicates decrease. ↔ Indicates no change, or mean increase or decrease of less than 10%. a The 95% confidence intervals for the percent change in the pharmacokinetic parameter are displayed. b 90% CI. c HIV-infected patients. NA = Not available. |
||||||||||||||
|
allopurinol, |
200 mg single dose |
2 |
↑ 312% |
↑ 232% |
||||||||||
|
healthy volunteer, 300 mg/day |
400 mg single dose |
14 |
↑ 113% |
↑ 69% |
||||||||||
|
ganciclovir, 1000 mg every 8 hours, |
200 mg every 12 hours |
12 |
↑ 111% |
NA |
||||||||||
|
ciprofloxacin, 750 mg every 12 hours for 3 days, 2 hours before didanosine |
200 mg every 12 hours |
8c |
↓ 16% |
↓ 28% |
||||||||||
|
indinavir, 800 mg single dose | ||||||||||||||
|
simultaneous |
200 mg single dose |
16 |
↔ |
↔ |
||||||||||
|
1 hour before didanosine |
200 mg single dose |
16 |
↓ 17% |
↓ 13% |
||||||||||
|
ketoconazole, 200 mg/day for 4 days, |
375 mg every 12 hours |
12c |
↔ |
↓ 12% |
||||||||||
|
loperamide, 4 mg every 6 hours for 1 day |
300 mg single dose |
12c |
↔ |
↓ 23% |
||||||||||
|
metoclopramide, 10 mg single dose |
300 mg single dose |
12c |
↔ |
↑ 13% |
||||||||||
|
ranitidine, 150 mg single dose, |
375 mg single dose |
12c |
↑ 14% |
↑ 13% |
||||||||||
|
rifabutin, 300 mg or 600 mg/day for 12 days |
167 mg or 250 mg every 12 hours |
11 |
↑ 13% |
↑ 17% |
||||||||||
|
ritonavir, 600 mg every 12 hours for 4 days |
200 mg every 12 hours |
12 |
↓ 13% |
↓ 16% |
||||||||||
|
stavudine, 40 mg every 12 hours for 4 days |
100 mg every 12 hours |
10 |
↔ |
↔ |
||||||||||
|
sulfamethoxazole, 1000 mg single dose |
200 mg single dose |
8c |
↔ |
↔ |
||||||||||
|
trimethoprim, 200 mg single dose |
200 mg single dose |
8c |
↔ |
↑ 17% |
||||||||||
|
zidovudine, 200 mg every 8 hours for 3 days |
200 mg every 12 hours |
6c |
↔ |
↔ |
||||||||||
| % Change of Coadministered Drug
Pharmacokinetic Parametersa |
|||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Drug | Didanosine Dosage | n | AUC of Coadministered Drug
(95% CI) | Cmax of Coadministered Drug
(95% CI) |
|||||||||||||||
| ↑ Indicates increase. ↓ Indicates decrease. ↔ Indicates no change, or mean increase or decrease of less than 10%. a The 95% confidence intervals for the percent change in the pharmacokinetic parameter are displayed. b HIV-infected patients. NA = Not available. |
|||||||||||||||||||
|
dapsone, 100 mg single dose |
200 mg every 12 hours for 14 days |
6b |
↔ |
↔ |
|||||||||||||||
|
ganciclovir, 1000 mg every 8 hours, |
200 mg every 12 hours |
12b |
↓ 21% |
NA |
|||||||||||||||
|
nelfinavir, 750 mg single dose, |
200 mg single dose |
10b |
↑ 12% |
↔ |
|||||||||||||||
|
ranitidine, 150 mg single dose, |
375 mg single dose |
12b |
↓ 16% |
↔ |
|||||||||||||||
|
ritonavir, 600 mg every 12 hours for 4 days |
200 mg every 12 hours |
12 |
↔ |
↔ |
|||||||||||||||
|
stavudine, 40 mg every 12 hours for 4 days |
100 mg every 12 hours |
10b |
↔ |
↑ 17% |
|||||||||||||||
|
sulfamethoxazole, 1000 mg single dose |
200 mg single dose |
8b |
↓ 11% |
↓ 12% |
|||||||||||||||
|
trimethoprim, 200 mg single dose |
200 mg single dose |
8b |
↑ 10% |
↓ 22% |
|||||||||||||||
|
zidovudine, 200 mg every 8 hours for 3 days |
200 mg every 12 hours |
6b |
↓ 10% |
↓ 16.5% |
|||||||||||||||
12.4 Microbiology
Mechanism of Action
Didanosine is a synthetic nucleoside analogue of the naturally occurring nucleoside deoxyadenosine in which the 3′-hydroxyl group is replaced by hydrogen. Intracellularly, didanosine is converted by cellular enzymes to the active metabolite, dideoxyadenosine 5′-triphosphate. Dideoxyadenosine 5′-triphosphate inhibits the activity of HIV-1 reverse transcriptase both by competing with the natural substrate, deoxyadenosine 5′-triphosphate, and by its incorporation into viral DNA causing termination of viral DNA chain elongation.
Antiviral Activity in Cell Culture
The anti-HIV-1 activity of didanosine was evaluated in a variety of HIV-1 infected lymphoblastic cell lines and monocyte/macrophage cell cultures. The concentration of drug necessary to inhibit viral replication by 50% (EC50) ranged from 2.5 to 10 μM (1 μM = 0.24 μg/mL) in lymphoblastic cell lines and 0.01 to 0.1 μM in monocyte/macrophage cell cultures.
Resistance
HIV-1 isolates with reduced sensitivity to didanosine have been selected in cell culture and were also obtained from patients treated with didanosine. Genetic analysis of isolates from didanosine-treated patients showed amino acid substitutions K65R, L74V, and M184V in reverse transcriptase. The L74V substitution was most frequently observed in clinical isolates. Phenotypic analysis of HIV-1 isolates from 60 patients (some with prior zidovudine treatment) receiving 6 to 24 months of didanosine monotherapy showed that isolates from 10 of 60 patients exhibited an average of a 10-fold decrease in susceptibility to didanosine in cell culture compared to baseline isolates. Clinical isolates that exhibited a decrease in didanosine susceptibility harbored one or more didanosine resistance-associated substitutions.
Cross-resistance
HIV-1 isolates from 2 of 39 patients receiving combination therapy for up to 2 years with didanosine and zidovudine exhibited decreased susceptibility to didanosine, lamivudine, stavudine, and zidovudine in cell culture. These isolates harbored five substitutions (A62V, V75I, F77L, F116Y, and Q151M) in reverse transcriptase. In data from clinical studies, the presence of thymidine analogue mutation substitutions (M41L, D67N, L210W, T215Y, K219Q) has been shown to decrease the response to didanosine.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Lifetime carcinogenicity studies were conducted in mice and rats for 22 and 24 months, respectively. In the mouse study, initial doses of 120, 800, and 1200 mg/kg/day for each sex were lowered after 8 months to 120, 210, and 210 mg/kg/day for females and 120, 300, and 600 mg/kg/day for males. The two higher doses exceeded the maximally tolerated dose in females and the high dose exceeded the maximally tolerated dose in males. The low dose in females represented 0.68-fold maximum human exposure and the intermediate dose in males represented 1.7-fold maximum human exposure based on relative AUC comparisons. In the rat study, initial doses were 100, 250, and 1000 mg/kg/day, and the high dose was lowered to 500 mg/kg/day after 18 months. The upper dose in male and female rats represented 3-fold maximum human exposure.
Didanosine induced no significant increase in neoplastic lesions in mice or rats at maximally tolerated doses.
Didanosine was positive in the following genetic toxicology assays: 1) the Escherichia coli tester strain WP2 uvrA bacterial mutagenicity assay; 2) the L5178Y/TK+/- mouse lymphoma mammalian cell gene mutation assay; 3) the in vitro chromosomal aberrations assay in cultured human peripheral lymphocytes; 4) the in vitro chromosomal aberrations assay in Chinese Hamster Lung cells; and 5) the BALB/c 3T3 in vitro transformation assay. No evidence of mutagenicity was observed in an Ames Salmonella bacterial mutagenicity assay or in rat and mouse in vivo micronucleus assays.
Reproduction studies have been performed in rats and rabbits at doses up to 12 and 14 times the estimated human exposure at the recommended daily human dose of VIDEX EC, respectively, and have revealed no evidence of impaired fertility or harm to the fetus due to didanosine.
13.2 Animal Toxicology and/or Pharmacology
Evidence of a dose-limiting skeletal muscle toxicity has been observed in mice and rats (but not in dogs) following long-term (greater than 90 days) dosing with didanosine at doses that were approximately 1.2 to 12 times the estimated human exposure. The relationship of this finding to the potential of didanosine to cause myopathy in humans is unclear. However, human myopathy has been associated with administration of didanosine and other nucleoside analogues.
14. Clinical Studies
14.1 Adult Patients
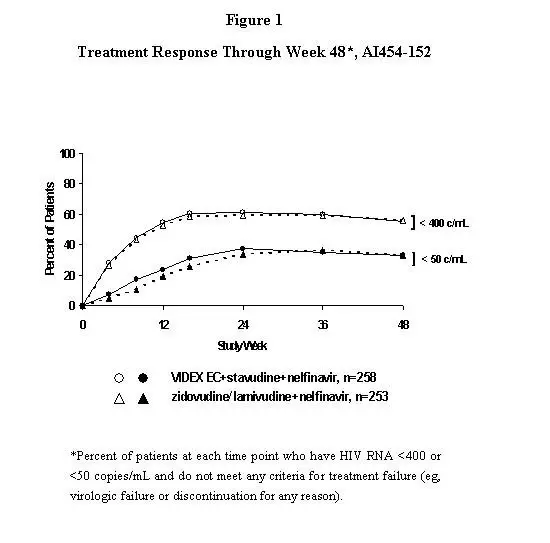
Study AI454-152 was a 48-week, randomized, open-label study comparing VIDEX EC (400 mg once daily) plus stavudine (40 mg twice daily) plus nelfinavir (750 mg three times daily) to zidovudine (300 mg) plus lamivudine (150 mg) combination tablets twice daily plus nelfinavir (750 mg three times daily) in 511 treatment-naive patients, with a mean CD4 cell count of 411 cells/mm3 (range 39 to 1105 cells/mm3) and a mean plasma HIV-1 RNA of 4.71 log10 copies/mL (range 2.8 to 5.9 log10 copies/mL) at baseline. Patients were primarily males (72%) and Caucasian (53%) with a mean age of 35 years (range 18 to 73 years). The percentages of patients with HIV-1 RNA less than 400 and less than 50 copies/mL and outcomes of patients through 48 weeks are summarized in Figure 1 and Table 13, respectively.
| Outcome | Percent of Patients with HIV-1 RNA less than 400 copies/mL
(less than 50 copies/mL) |
|
|---|---|---|
| VIDEX EC + stavudine
+ nelfinavir n=258 | zidovudine/lamivudinea
+ nelfinavir n=253 |
|
| a Zidovudine/lamivudine combination tablet. b Corresponds to rates at Week 48 in Figure 1. c Subjects achieved and maintained confirmed HIV-1 RNA less than 400 copies/mL (less than 50 copies/mL) through Week 48. d Includes viral rebound at or before Week 48 and failure to achieve confirmed HIV-1 RNA less than 400 copies/mL (less than 50 copies/mL) through Week 48. e Includes lost to follow-up, subject’s withdrawal, discontinuation due to physician’s decision, never treated, and other reasons. |
||
|
Responderb,c |
55% (33%) |
56% (33%) |
|
Virologic failured |
22% (45%) |
21% (43%) |
|
Death or discontinued due to disease progression |
1% (1%) |
2% (2%) |
|
Discontinued due to adverse event |
6% (6%) |
7% (7%) |
|
Discontinued due to other reasonse |
16% (16%) |
15% (16%) |
14.2 Pediatric Patients
Efficacy in pediatric patients was demonstrated in a randomized, double-blind, controlled study (ACTG 152, conducted 1991-1995) involving 831 patients 3 months to 18 years of age treated for more than 1.5 years with zidovudine (180 mg/m2 every 6 hours), didanosine (120 mg/m2 every 12 hours), or zidovudine (120 mg/m2 every 6 hours) plus didanosine (90 mg/m2 every 12 hours). Patients treated with didanosine or didanosine plus zidovudine had lower rates of HIV-1 disease progression or death compared with those treated with zidovudine alone.
16. How is Videx EC supplied
VIDEX EC (didanosine, USP) Delayed-Release Capsules are white, opaque capsules that are packaged in bottles with child-resistant closures as described in Table 14.
|
125 mg capsule imprinted with “BMS 125 mg 6671” in Tan |
|
|
NDC No. 0087-6671-17 |
30 capsules/bottle |
|
200 mg capsule imprinted with “BMS 200 mg 6672” in Green |
|
|
NDC No. 0087-6672-17 |
30 capsules/bottle |
|
250 mg capsule imprinted with “BMS 250 mg 6673” in Blue |
|
|
NDC No. 0087-6673-17 |
30 capsules/bottle |
|
400 mg capsule imprinted with “BMS 400 mg 6674” in Red |
|
|
NDC No. 0087-6674-17 |
30 capsules/bottle |
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Pancreatitis
Inform patients that a serious toxicity of VIDEX EC, used alone and in combination regimens, is pancreatitis, which may be fatal [see Warnings and Precautions (5.1)].
Lactic Acidosis and Severe Hepatomegaly with Steatosis
Inform patients that lactic acidosis and severe hepatomegaly with steatosis, including fatal cases, have been reported with the use of nucleoside analogues alone or in combination, including didanosine and other antiretrovirals. Advise pregnant individuals of the potential risks of lactic acidosis syndrome/hepatic steatosis syndrome [see Contraindications (4), Warnings and Precautions (5.2) and Use in Specific Populations (8.1)].
Hepatic Toxicity
Inform patients that hepatotoxicity, including fatal hepatic adverse events, has been reported in patients with preexisting liver dysfunction. The safety and efficacy of VIDEX EC have not been established in HIV-infected patients with significant underlying liver disease. [see Warnings and Precautions (5.3)].
Non-cirrhotic Portal Hypertension
Inform patients that non-cirrhotic portal hypertension has been reported in patients taking VIDEX EC, including cases leading to liver transplantation or death. [see Warnings and Precautions (5.4)].
Peripheral Neuropathy
Inform patients that peripheral neuropathy, manifested by numbness, tingling, or pain in hands or feet, may develop during therapy with VIDEX EC (didanosine). Instruct patients that peripheral neuropathy occurs with greatest frequency in patients with advanced HIV-1 disease or a history of peripheral neuropathy, and that discontinuation of VIDEX EC may be required if toxicity develops [see Warnings and Precautions (5.5)].
Retinal Changes and Optic Neuritis
Inform patients that retinal changes and optic neuritis, which may result in blurred vision, have been reported in adult and pediatric patients. Advise patients to have regular eye exams while taking VIDEX EC [see Warnings and Precautions (5.6)].
Immune Reconstitution Syndrome
Advise patients to inform their healthcare provider immediately of any symptoms of infection, as in some patients with advanced HIV infection (AIDS), signs and symptoms of inflammation from previous infections may occur soon after anti-HIV treatment is started [see Warnings and Precautions (5.7)].
Lipoatrophy
Inform patient that loss of body fat (e.g., from arms, legs, or face) may occur in individuals receiving antiretroviral therapy including VIDEX EC. Monitor patients receiving VIDEX EC to monitor for clinical signs and symptoms of lipoatrophy. Patients should be routinely questioned about body changes related to lipoatrophy [see Warnings and Precautions (5.8)].
Drug Interactions
VIDEX EC may interact with many drugs; therefore, advise patients to report to their healthcare provider the use of any other prescription of non-prescription medication or herbal products, including alcohol, which may exacerbate VIDEX EC toxicities. Patients should avoid alcohol with VIDEX EC [see Contraindications (4), Drug Interactions (7)].
Pregnancy Registry
Inform patients that there is an antiretroviral pregnancy registry to monitor fetal outcomes of pregnant individuals exposed to VIDEX EC [see Use in Specific Populations (8.1)].
Lactation
Advise mothers with HIV-1 not to breastfeed because HIV-1 can be passed to the baby in breast milk. [see Use in Specific Populations (8.2)].
Dosing Information
Instruct patients to swallow the capsule whole on an empty stomach and to not open the capsule.
Instruct patients not to miss a dose but if they do, patients should take VIDEX EC as soon as possible. Inform patients that it is important to take VIDEX EC on a regular dosing schedule and to avoid missing doses as it can result in development of resistance.
Revised: December 2019
Medication Guide
VIDEX EC (VY-dex Ee-see)
(didanosine, USP)
Delayed-Release Capsules
Enteric-Coated Beadlets
What is the most important information I should know about VIDEX EC?
VIDEX EC can cause serious side effects, including:
- Inflammation of your pancreas (pancreatitis) can happen in people who take VIDEX EC and can lead to death. People who take VIDEX EC in combination with the medicine stavudine may be at an increased risk for pancreatitis. Do not take VIDEX EC with stavudine.
Call your healthcare provider right away if you have any of the following symptoms of pancreatitis:
|
|
|
|
- Build-up of an acid in your blood (lactic acidosis). Lactic acidosis can happen in some people who take VIDEX EC or similar medicines (nucleoside analogues). Lactic acidosis is a serious medical emergency that can lead to death. There have been deaths reported in pregnant women who get lactic acidosis after taking VIDEX EC and stavudine. Do not take VIDEX EC with stavudine.
Call your healthcare provider right away if you have any of the following symptoms which could be signs of lactic acidosis:
|
|
|
|
|
|
|
|
- Severe liver problems, including liver failure, can happen in people who take VIDEX EC. Your liver may become large (hepatomegaly), you may develop fat in the liver (steatosis), or you may have high blood pressure in the large vein of the liver (portal hypertension). Severe liver problems can lead to liver transplantation or death in some people taking VIDEX EC. Taking VIDEX EC with medicines that contain hydroxyurea or stavudine may increase your risk for liver problems.
You may be more likely to get lactic acidosis or severe liver problems if you are a female, are very overweight (obese), or have been taking nucleoside analogue medicines for a long time.
Call your healthcare provider right away if you have any of the following symptoms of severe liver problems:
|
|
For more information about side effects, see "What are the possible side effects of VIDEX EC?".
What is VIDEX EC?
VIDEX EC is a prescription medicine that is used with other antiretroviral medicines to treat Human Immunodeficiency Virus (HIV)-1 infection.
HIV-1 is the virus that causes Acquired Immune Deficiency Syndrome (AIDS).
Do not take VIDEX EC if you take:
|
|
|
Before you take VIDEX EC, tell your healthcare provider about all of your medical conditions, including if you:
- have or had problems with your pancreas
- have or had kidney problems
- have or had liver problems, including hepatitis
- have or had numbness, tingling, or pain in the hands or feet (peripheral neuropathy)
- are receiving dialysis
- drink alcoholic beverages
- are pregnant or plan to become pregnant. It is not known if VIDEX EC will harm your unborn baby. Pregnancy Registry: There is a pregnancy registry for women who take antiretroviral medicines, including VIDEX EC during pregnancy. The purpose of the registry is to collect information about the health of you and your baby. Talk to your healthcare provider about how you can take part in this registry.
- are breastfeeding or plan to breastfeed. Do not breastfeed if you take VIDEX EC.
- You should not breastfeed if you have HIV-1 because of the risk of passing HIV-1 to your baby.
- It is not known if VIDEX EC can pass into your breast milk and if it could harm your baby.
Talk with your healthcare provider about the best way to feed your baby.
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins and herbal supplements.
Some medicines interact with VIDEX EC. Keep a list of your medicines and show it to your healthcare provider and pharmacist when you get a new medicine.
- You can ask your healthcare provider or pharmacist for a list of medicines that interact with VIDEX EC.
- Do not start taking a new medicine without telling your healthcare provider. Your healthcare provider can tell you if it is safe to take VIDEX EC with other medicines.
How should I take VIDEX EC?
- Take VIDEX EC exactly as your healthcare provider tells you to take it.
- Your healthcare provider will tell you how much VIDEX EC to take and when to take it.
- Take VIDEX EC on an empty stomach.
- Take VIDEX EC capsules whole. If you cannot swallow VIDEX EC capsules whole, tell your healthcare provider. You may need a different medicine.
- Your healthcare provider may change your dose. Do not change your dose of VIDEX EC without talking to your healthcare provider.
- Do not miss a dose of VIDEX EC. If you miss a dose of VIDEX EC, take it as soon as possible.
- It is important to take VIDEX EC on a regular schedule. The virus in your blood may increase and the virus may become harder to treat if you miss doses.
- Your healthcare provider may lower your dosage of VIDEX EC if your kidneys are not working well.
- If you take too much VIDEX EC, go to the nearest emergency room right away.
What are the possible side effects of VIDEX EC?
VIDEX EC can cause serious side effects, including:
- See "What is the most important information I should know about VIDEX EC?"
- Numbness, tingling, or pain in your hands or feet (peripheral neuropathy). Peripheral neuropathy is common during treatment with VIDEX EC and can be severe. Peripheral neuropathy happens more often in people who have advanced HIV-1 disease, have a history of peripheral neuropathy, or in people who are being treated with medicines that can cause neurologic problems. Tell your healthcare provider if you get numbness, tingling, or pain in your hands or feet during treatment with VIDEX EC.
- Vision changes. Call your healthcare provider if you have changes in vision, such as blurred vision. You should have regular eye exams while taking VIDEX EC.
- Changes in your immune system (immune reconstitution syndrome). Your immune system may get stronger and begin to fight infections that have been hidden in your body for a long time. Tell your healthcare provider if you start having new or worse symptoms of infection after you start taking HIV medicine.
- Loss of body fat (lipoatrophy) can happen with VIDEX use. These changes may include less fat in your legs, arms, face, and buttocks.
The most common side effects of VIDEX EC include:
|
|
|
|
|
These are not all the possible side effects of VIDEX EC.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store VIDEX EC?
- Store VIDEX EC capsules in a tightly closed container between 59 °F to 86 °F (15 °C to 30 °C)
Keep VIDEX EC and all medicines out of the reach of children.
General information about the safe and effective use of VIDEX EC.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use VIDEX EC for a condition for which it was not prescribed. Do not give VIDEX EC to other people, even if they have the same symptoms that you have. It may harm them.
You can ask your pharmacist or healthcare provider for information about VIDEX EC that is written for health professionals.
What are the ingredients in VIDEX EC?
Active Ingredients: didanosine, USP
Inactive Ingredients: carboxymethylcellulose sodium 12, diethyl phthalate, methacrylic acid copolymer, sodium hydroxide, sodium starch glycolate, and talc
Capsule shell: gelatin, and titanium dioxide.
VIDEX® EC is a registered trademark of Bristol-Myers Squibb Company. Distributed by: Bristol-Myers Squibb Company Princeton, NJ 08543 USA
For more information, go to www.bms.com/products/Pages/prescribing.aspx or call 1-800-321-1335.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Revised December 2018
VIDEX EC 125 mg Representative Packaging
See HOW SUPPLIED section for a complete list of available packages of VIDEX EC.
30 Capsules NDC 0087-6671-17
125 mg
VIDEX®EC
(didanosine, USP)
delayed-release capsules
enteric-coated beadlets
Detach and dispense
the accompanying
Medication Guide
to the patient.
Rx only
VIDEX EC 200 mg Representative Packaging
30 Capsules NDC 0087-6672-17
200 mg
VIDEX®EC
(didanosine, USP)
delayed-release capsules
enteric-coated beadlets
Detach and dispense
the accompanying
Medication Guide
to the patient.
Rx only
| VIDEX EC
didanosine capsule, delayed release |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| VIDEX EC
didanosine capsule, delayed release |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| VIDEX EC
didanosine capsule, delayed release |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| VIDEX EC
didanosine capsule, delayed release |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Bristol-Myers Squibb Company (102826703) |