Drug Detail:Vytorin (Ezetimibe and simvastatin [ ez-et-i-mibe-and-sim-va-stat-in ])
Drug Class: Antihyperlipidemic combinations
Highlights of Prescribing Information
VYTORIN® (ezetimibe and simvastatin) tablets, for oral use
Initial U.S. Approval: 2004
Recent Major Changes
| Warnings and Precautions | |
| Immune-Mediated Necrotizing Myopathy (5.2) | 9/2020 |
Indications and Usage for Vytorin
VYTORIN, which contains a cholesterol absorption inhibitor and an HMG-CoA reductase inhibitor (statin), is indicated as adjunctive therapy to diet to:
- reduce elevated total-C, LDL-C, Apo B, TG, and non-HDL-C, and to increase HDL-C in patients with primary (heterozygous familial and non-familial) hyperlipidemia or mixed hyperlipidemia. (1.1)
- reduce elevated total-C and LDL-C in patients with homozygous familial hypercholesterolemia (HoFH), as an adjunct to other lipid-lowering treatments. (1.2)
Limitations of Use (1.3)
- No incremental benefit of VYTORIN on cardiovascular morbidity and mortality over and above that demonstrated for simvastatin has been established.
- VYTORIN has not been studied in Fredrickson Type I, III, IV, and V dyslipidemias.
Vytorin Dosage and Administration
- Dose range is 10/10 mg/day to 10/40 mg/day. (2.1)
- Recommended usual starting dose is 10/10 or 10/20 mg/day. (2.1)
- Due to the increased risk of myopathy, including rhabdomyolysis, use of the 10/80-mg dose of VYTORIN should be restricted to patients who have been taking VYTORIN 10/80 mg chronically (e.g., for 12 months or more) without evidence of muscle toxicity. (2.2)
- Patients who are currently tolerating the 10/80-mg dose of VYTORIN who need to be initiated on an interacting drug that is contraindicated or is associated with a dose cap for simvastatin should be switched to an alternative statin or statin-based regimen with less potential for the drug-drug interaction. (2.2)
- Due to the increased risk of myopathy, including rhabdomyolysis, associated with the 10/80-mg dose of VYTORIN, patients unable to achieve their LDL-C goal utilizing the 10/40-mg dose of VYTORIN should not be titrated to the 10/80-mg dose, but should be placed on alternative LDL-C-lowering treatment(s) that provides greater LDL-C lowering. (2.2)
- Dosing of VYTORIN should occur either ≥2 hours before or ≥4 hours after administration of a bile acid sequestrant. (2.3, 7.5)
Dosage Forms and Strengths
- Tablets (ezetimibe mg/simvastatin mg): 10/10, 10/20, 10/40, 10/80 (3)
Contraindications
- Concomitant administration of strong CYP3A4 inhibitors. (4, 5.1)
- Concomitant administration of gemfibrozil, cyclosporine, or danazol. (4, 5.1)
- Hypersensitivity to any component of this medication (4, 6.2)
- Active liver disease or unexplained persistent elevations of hepatic transaminase levels (4, 5.3)
- Women who are pregnant or may become pregnant (4, 8.1)
- Nursing mothers (4, 8.3)
Warnings and Precautions
- Patients should be advised of the increased risk of myopathy, including rhabdomyolysis, with the 10/80-mg dose. (5.1)
- Patients should be advised to report promptly any unexplained and/or persistent muscle pain, tenderness, or weakness. VYTORIN should be discontinued immediately if myopathy is diagnosed or suspected. (5.1)
- Skeletal muscle effects (e.g., myopathy and rhabdomyolysis): Risks increase with higher doses and concomitant use of certain medicines. Predisposing factors include advanced age (≥65), female gender, uncontrolled hypothyroidism, and renal impairment. Rare cases of rhabdomyolysis with acute renal failure secondary to myoglobinuria have been reported. (4, 5.1, 8.5, 8.6)
- Immune-Mediated Necrotizing Myopathy (IMNM): There have been rare reports of IMNM, an autoimmune myopathy, associated with statin use. IMNM is characterized by: proximal muscle weakness and elevated serum creatine kinase, which persist despite discontinuation of statin treatment; positive anti-HMG CoA reductase antibody; muscle biopsy showing necrotizing myopathy; and improvement with immunosuppressive agents. (5.2)
- Liver enzyme abnormalities: Persistent elevations in hepatic transaminases can occur. Check liver enzyme tests before initiating therapy and as clinically indicated thereafter. (5.3)
Adverse Reactions/Side Effects
- Common (incidence ≥2% and greater than placebo) adverse reactions in clinical trials: headache, increased ALT, myalgia, upper respiratory tract infection, and diarrhea. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., at 1-877-888-4231 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
| Interacting Agents | Prescribing Recommendations |
|---|---|
|
|
| Strong CYP3A4 Inhibitors, (e.g., itraconazole, ketoconazole, posaconazole, voriconazole, erythromycin, clarithromycin, telithromycin, HIV protease inhibitors, boceprevir, telaprevir, nefazodone, cobicistat-containing products), gemfibrozil, cyclosporine, danazol | Contraindicated with VYTORIN |
| Niacin (≥1 g/day) | For Chinese patients, not recommended with VYTORIN |
| Verapamil, diltiazem, dronedarone | Do not exceed 10/10 mg VYTORIN daily |
| Amiodarone, amlodipine, ranolazine | Do not exceed 10/20 mg VYTORIN daily |
| Lomitapide | For patients with HoFH, do not exceed 10/20 mg VYTORIN daily* |
| Daptomycin | Temporarily suspend VYTORIN |
| Grapefruit juice | Avoid grapefruit juice |
- Coumarin anticoagulants: simvastatin prolongs INR. Achieve stable INR prior to starting VYTORIN. Monitor INR frequently until stable upon initiation or alteration of VYTORIN therapy. (7.8)
- Cholestyramine: Combination decreases exposure of ezetimibe. (2.3, 7.5)
- Other Lipid-lowering Medications: Use with fenofibrates increases the risk of adverse skeletal muscle effects. Caution should be used when prescribing with VYTORIN. (5.1, 7.2)
- Fenofibrates: Combination increases exposure of ezetimibe. If cholelithiasis is suspected in a patient receiving ezetimibe and a fenofibrate, gallbladder studies are indicated and alternative lipid-lowering therapy should be considered. (7.2, 7.7, 12.3)
Use In Specific Populations
- Moderate to severe renal impairment: Doses exceeding 10/20 mg/day should be used with caution and close monitoring (2.5, 8.6).
- Chinese patients: May be at higher risk of myopathy; monitor appropriately (5.1, 8.8).
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 12/2020
Full Prescribing Information
1. Indications and Usage for Vytorin
Therapy with lipid-altering agents should be only one component of multiple risk factor intervention in individuals at significantly increased risk for atherosclerotic vascular disease due to hypercholesterolemia. Drug therapy is indicated as an adjunct to diet when the response to a diet restricted in saturated fat and cholesterol and other nonpharmacologic measures alone has been inadequate.
1.1 Primary Hyperlipidemia
VYTORIN® is indicated for the reduction of elevated total cholesterol (total-C), low-density lipoprotein cholesterol (LDL-C), apolipoprotein B (Apo B), triglycerides (TG), and non-high-density lipoprotein cholesterol (non-HDL-C), and to increase high-density lipoprotein cholesterol (HDL-C) in patients with primary (heterozygous familial and non-familial) hyperlipidemia or mixed hyperlipidemia.
2. Vytorin Dosage and Administration
2.1 Recommended Dosing
The usual dosage range is 10/10 mg/day to 10/40 mg/day. The recommended usual starting dose is 10/10 mg/day or 10/20 mg/day. VYTORIN should be taken as a single daily dose in the evening, with or without food. Patients who require a larger reduction in LDL-C (greater than 55%) may be started at 10/40 mg/day in the absence of moderate to severe renal impairment (estimated glomerular filtration rate less than 60 mL/min/1.73 m2). After initiation or titration of VYTORIN, lipid levels may be analyzed after 2 or more weeks and dosage adjusted, if needed.
2.2 Restricted Dosing for 10/80 mg
Due to the increased risk of myopathy, including rhabdomyolysis, particularly during the first year of treatment, use of the 10/80-mg dose of VYTORIN should be restricted to patients who have been taking VYTORIN 10/80 mg chronically (e.g., for 12 months or more) without evidence of muscle toxicity [see Warnings and Precautions (5.1)].
Patients who are currently tolerating the 10/80-mg dose of VYTORIN who need to be initiated on an interacting drug that is contraindicated or is associated with a dose cap for simvastatin should be switched to an alternative statin or statin-based regimen with less potential for the drug-drug interaction.
Due to the increased risk of myopathy, including rhabdomyolysis, associated with the 10/80-mg dose of VYTORIN, patients unable to achieve their LDL-C goal utilizing the 10/40-mg dose of VYTORIN should not be titrated to the 10/80-mg dose, but should be placed on alternative LDL-C-lowering treatment(s) that provides greater LDL-C lowering.
2.4 Patients with Homozygous Familial Hypercholesterolemia
The recommended dosage for patients with homozygous familial hypercholesterolemia is VYTORIN 10/40 mg/day in the evening [see Dosage and Administration, Restricted Dosing for 10/80 mg (2.2)]. VYTORIN should be used as an adjunct to other lipid-lowering treatments (e.g., LDL apheresis) in these patients or if such treatments are unavailable.
Simvastatin exposure is approximately doubled with concomitant use of lomitapide; therefore, the dose of VYTORIN should be reduced by 50% if initiating lomitapide. VYTORIN dosage should not exceed 10/20 mg/day (or 10/40 mg/day for patients who have previously taken simvastatin 80 mg/day chronically, e.g., for 12 months or more, without evidence of muscle toxicity) while taking lomitapide.
2.5 Patients with Renal Impairment/Chronic Kidney Disease
In patients with mild renal impairment (estimated GFR greater than or equal to 60 mL/min/1.73 m2), no dosage adjustment is necessary. In patients with chronic kidney disease and estimated glomerular filtration rate less than 60 mL/min/1.73 m2, the dose of VYTORIN is 10/20 mg/day in the evening. In such patients, higher doses should be used with caution and close monitoring [see Warnings and Precautions (5.1); Clinical Pharmacology (12.3)].
3. Dosage Forms and Strengths
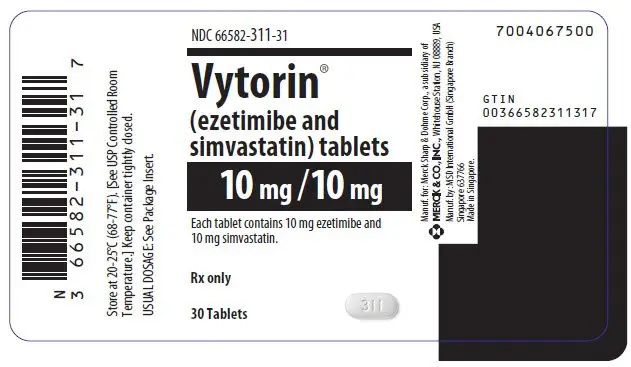
- VYTORIN® 10/10, (ezetimibe 10 mg and simvastatin 10 mg tablets) are white to off-white capsule-shaped tablets with code "311" on one side.
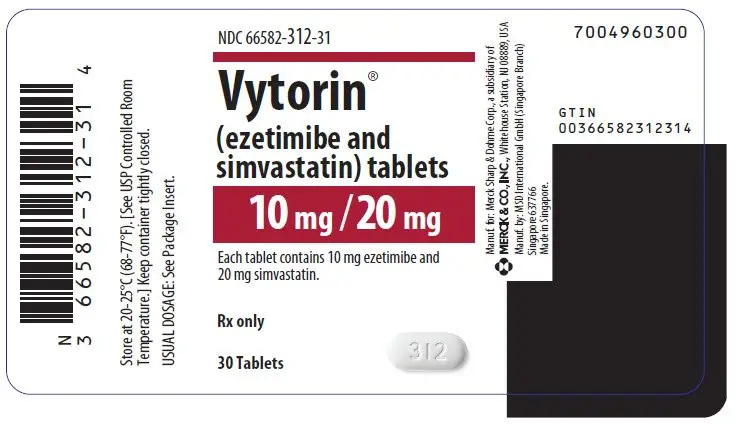
- VYTORIN® 10/20, (ezetimibe 10 mg and simvastatin 20 mg tablets) are white to off-white capsule-shaped tablets with code "312" on one side.
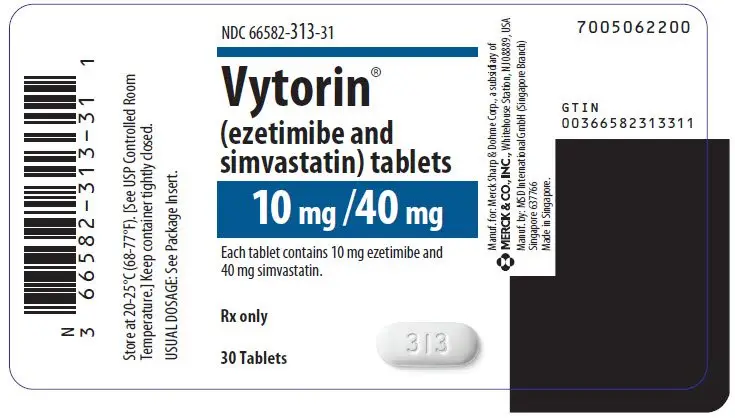
- VYTORIN® 10/40, (ezetimibe 10 mg and simvastatin 40 mg tablets) are white to off-white capsule-shaped tablets with code "313" on one side.
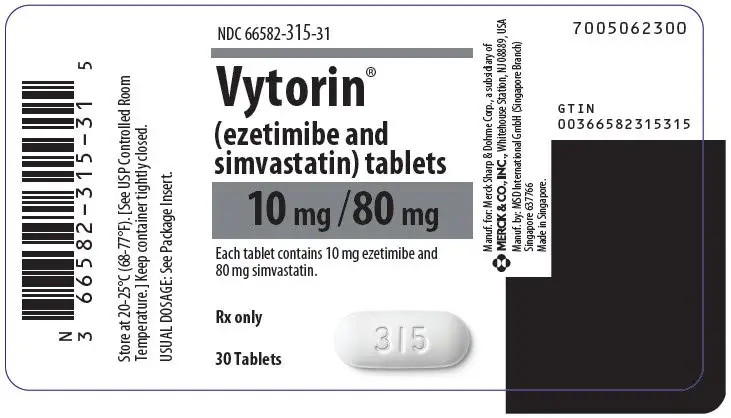
- VYTORIN® 10/80, (ezetimibe 10 mg and simvastatin 80 mg tablets) are white to off-white capsule-shaped tablets with code "315" on one side.
4. Contraindications
VYTORIN is contraindicated in the following conditions:
- Concomitant administration of strong CYP3A4 inhibitors (e.g., itraconazole, ketoconazole, posaconazole, voriconazole, HIV protease inhibitors, boceprevir, telaprevir, erythromycin, clarithromycin, telithromycin, nefazodone, and cobicistat-containing products) [see Warnings and Precautions (5.1)].
- Concomitant administration of gemfibrozil, cyclosporine, or danazol [see Warnings and Precautions (5.1)].
- Hypersensitivity to any component of this medication [see Adverse Reactions (6.2)].
- Active liver disease or unexplained persistent elevations in hepatic transaminase levels [see Warnings and Precautions (5.3)].
- Women who are pregnant or may become pregnant. Serum cholesterol and triglycerides increase during normal pregnancy, and cholesterol or cholesterol derivatives are essential for fetal development. Because HMG-CoA reductase inhibitors (statins), such as simvastatin, decrease cholesterol synthesis and possibly the synthesis of other biologically active substances derived from cholesterol, VYTORIN may cause fetal harm when administered to a pregnant woman. Atherosclerosis is a chronic process and the discontinuation of lipid-lowering drugs during pregnancy should have little impact on the outcome of long-term therapy of primary hypercholesterolemia. There are no adequate and well-controlled studies of VYTORIN use during pregnancy; however, in rare reports congenital anomalies were observed following intrauterine exposure to statins. In rat and rabbit animal reproduction studies, simvastatin revealed no evidence of teratogenicity. VYTORIN should be administered to women of childbearing age only when such patients are highly unlikely to conceive. If the patient becomes pregnant while taking this drug, VYTORIN should be discontinued immediately and the patient should be apprised of the potential hazard to the fetus [see Use in Specific Populations (8.1)].
- Nursing mothers. It is not known whether simvastatin is excreted into human milk; however, a small amount of another drug in this class does pass into breast milk. Because statins have the potential for serious adverse reactions in nursing infants, women who require VYTORIN treatment should not breastfeed their infants [see Use in Specific Populations (8.3)].
5. Warnings and Precautions
5.1 Myopathy/Rhabdomyolysis
Simvastatin occasionally causes myopathy manifested as muscle pain, tenderness or weakness with creatine kinase above ten times the upper limit of normal (ULN). Myopathy sometimes takes the form of rhabdomyolysis with or without acute renal failure secondary to myoglobinuria, and rare fatalities have occurred. The risk of myopathy is increased by elevated plasma levels of simvastatin and simvastatin acid. Predisposing factors for myopathy include advanced age (≥65 years), female gender, uncontrolled hypothyroidism, and renal impairment. Chinese patients may be at increased risk for myopathy [see Use in Specific Populations (8.8)].
The risk of myopathy, including rhabdomyolysis, is dose related. In a clinical trial database in which 41,413 patients were treated with simvastatin, 24,747 (approximately 60%) of whom were enrolled in studies with a median follow-up of at least 4 years, the incidence of myopathy was approximately 0.03% and 0.08% at 20 and 40 mg/day, respectively. The incidence of myopathy with 80 mg (0.61%) was disproportionately higher than that observed at the lower doses. In these trials, patients were carefully monitored and some interacting medicinal products were excluded.
In a clinical trial in which 12,064 patients with a history of myocardial infarction were treated with simvastatin (mean follow-up 6.7 years), the incidence of myopathy (defined as unexplained muscle weakness or pain with a serum creatine kinase [CK] >10 times upper limit of normal [ULN]) in patients on 80 mg/day was approximately 0.9% compared with 0.02% for patients on 20 mg/day. The incidence of rhabdomyolysis (defined as myopathy with a CK >40 times ULN) in patients on 80 mg/day was approximately 0.4% compared with 0% for patients on 20 mg/day. The incidence of myopathy, including rhabdomyolysis, was highest during the first year and then notably decreased during the subsequent years of treatment. In this trial, patients were carefully monitored and some interacting medicinal products were excluded.
The risk of myopathy, including rhabdomyolysis, is greater in patients on simvastatin 80 mg compared with other statin therapies with similar or greater LDL-C-lowering efficacy and compared with lower doses of simvastatin. Therefore, the 10/80-mg dose of VYTORIN should be used only in patients who have been taking VYTORIN 10/80 mg chronically (e.g., for 12 months or more) without evidence of muscle toxicity [see Dosage and Administration, Restricted Dosing for 10/80 mg (2.2)]. If, however, a patient who is currently tolerating the 10/80-mg dose of VYTORIN needs to be initiated on an interacting drug that is contraindicated or is associated with a dose cap for simvastatin, that patient should be switched to an alternative statin or statin-based regimen with less potential for the drug-drug interaction. Patients should be advised of the increased risk of myopathy, including rhabdomyolysis, and to report promptly any unexplained muscle pain, tenderness or weakness. If symptoms occur, treatment should be discontinued immediately [see Warnings and Precautions (5.2)].
In the Study of Heart and Renal Protection (SHARP), 9270 patients with chronic kidney disease were allocated to receive VYTORIN 10/20 mg daily (n=4650) or placebo (n=4620). During a median follow-up period of 4.9 years, the incidence of myopathy (defined as unexplained muscle weakness or pain with a serum creatine kinase [CK] >10 times upper limit of normal [ULN]) was 0.2% for VYTORIN and 0.1% for placebo: the incidence of rhabdomyolysis (defined as myopathy with a CK > 40 times ULN) was 0.09% for VYTORIN and 0.02% for placebo.
In postmarketing experience with ezetimibe, cases of myopathy and rhabdomyolysis have been reported. Most patients who developed rhabdomyolysis were taking a statin prior to initiating ezetimibe. However, rhabdomyolysis has been reported with ezetimibe monotherapy and with the addition of ezetimibe to agents known to be associated with increased risk of rhabdomyolysis, such as fibric acid derivatives. VYTORIN and a fenofibrate, if taking concomitantly, should both be immediately discontinued if myopathy is diagnosed or suspected.
All patients starting therapy with VYTORIN or whose dose of VYTORIN is being increased should be advised of the risk of myopathy, including rhabdomyolysis, and told to report promptly any unexplained muscle pain, tenderness or weakness particularly if accompanied by malaise or fever or if muscle signs and symptoms persist after discontinuing VYTORIN. VYTORIN therapy should be discontinued immediately if myopathy is diagnosed or suspected. In most cases, muscle symptoms and CK increases resolved when simvastatin treatment was promptly discontinued. Periodic CK determinations may be considered in patients starting therapy with VYTORIN or whose dose is being increased, but there is no assurance that such monitoring will prevent myopathy.
Many of the patients who have developed rhabdomyolysis on therapy with simvastatin have had complicated medical histories, including renal insufficiency usually as a consequence of long-standing diabetes mellitus. Such patients taking VYTORIN merit closer monitoring.
VYTORIN therapy should be discontinued if markedly elevated CPK levels occur or myopathy is diagnosed or suspected. VYTORIN therapy should also be temporarily withheld in any patient experiencing an acute or serious condition predisposing to the development of renal failure secondary to rhabdomyolysis, e.g., sepsis; hypotension; major surgery; trauma; severe metabolic, endocrine, or electrolyte disorders; or uncontrolled epilepsy.
5.2 Immune-Mediated Necrotizing Myopathy
There have been rare reports of immune-mediated necrotizing myopathy (IMNM), an autoimmune myopathy, associated with statin use. IMNM is characterized by: proximal muscle weakness and elevated serum creatine kinase, which persist despite discontinuation of statin treatment; positive anti-HMG CoA reductase antibody; muscle biopsy showing necrotizing myopathy; and improvement with immunosuppressive agents. Additional neuromuscular and serologic testing may be necessary. Treatment with immunosuppressive agents may be required. Consider risk of IMNM carefully prior to initiation of a different statin. If therapy is initiated with a different statin, monitor for signs and symptoms of IMNM.
5.3 Liver Enzymes
In three placebo-controlled, 12-week trials, the incidence of consecutive elevations (≥3 × ULN) in serum transaminases was 1.7% overall for patients treated with VYTORIN and appeared to be dose-related with an incidence of 2.6% for patients treated with VYTORIN 10/80. In controlled long-term (48-week) extensions, which included both newly-treated and previously-treated patients, the incidence of consecutive elevations (≥3 × ULN) in serum transaminases was 1.8% overall and 3.6% for patients treated with VYTORIN 10/80. These elevations in transaminases were generally asymptomatic, not associated with cholestasis, and returned to baseline after discontinuation of therapy or with continued treatment.
In SHARP, 9270 patients with chronic kidney disease were allocated to receive VYTORIN 10/20 mg daily (n=4650), or placebo (n=4620). During a median follow-up period of 4.9 years, the incidence of consecutive elevations of transaminases (>3 × ULN) was 0.7% for VYTORIN and 0.6% for placebo.
It is recommended that liver function tests be performed before the initiation of treatment with VYTORIN, and thereafter when clinically indicated. There have been rare postmarketing reports of fatal and non-fatal hepatic failure in patients taking statins, including simvastatin. If serious liver injury with clinical symptoms and/or hyperbilirubinemia or jaundice occurs during treatment with VYTORIN, promptly interrupt therapy. If an alternate etiology is not found do not restart VYTORIN. Note that ALT may emanate from muscle, therefore ALT rising with CK may indicate myopathy [see Warnings and Precautions (5.1)].
VYTORIN should be used with caution in patients who consume substantial quantities of alcohol and/or have a past history of liver disease. Active liver diseases or unexplained persistent transaminase elevations are contraindications to the use of VYTORIN.
6. Adverse Reactions/Side Effects
The following serious adverse reactions are discussed in greater detail in other sections of the label:
- Rhabdomyolysis and myopathy [see Warnings and Precautions (5.1)]
- Liver enzyme abnormalities [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
Because the below reactions are reported voluntarily from a population of uncertain size, it is generally not possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following adverse reactions have been reported in postmarketing experience for VYTORIN or ezetimibe or simvastatin: pruritus; alopecia; erythema multiforme; a variety of skin changes (e.g., nodules, discoloration, dryness of skin/mucous membranes, changes to hair/nails); dizziness; muscle cramps; myalgia; arthralgia; pancreatitis; paresthesia; peripheral neuropathy; vomiting; nausea; anemia; erectile dysfunction; interstitial lung disease; myopathy/rhabdomyolysis [see Warnings and Precautions (5.1)]; hepatitis/jaundice; fatal and non-fatal hepatic failure; depression; cholelithiasis; cholecystitis; thrombocytopenia; elevations in liver transaminases; elevated creatine phosphokinase.
There have been rare reports of immune-mediated necrotizing myopathy associated with statin use [see Warnings and Precautions (5.1)].
Hypersensitivity reactions, including anaphylaxis, angioedema, rash, and urticaria have been reported.
In addition, an apparent hypersensitivity syndrome has been reported rarely that has included one or more of the following features: anaphylaxis, angioedema, lupus erythematous-like syndrome, polymyalgia rheumatica, dermatomyositis, vasculitis, purpura, thrombocytopenia, leukopenia, hemolytic anemia, positive ANA, ESR increase, eosinophilia, arthritis, arthralgia, urticaria, asthenia, photosensitivity, fever, chills, flushing, malaise, dyspnea, toxic epidermal necrolysis, erythema multiforme, including Stevens-Johnson syndrome.
There have been rare postmarketing reports of cognitive impairment (e.g., memory loss, forgetfulness, amnesia, memory impairment, confusion) associated with statin use. These cognitive issues have been reported for all statins. The reports are generally nonserious, and reversible upon statin discontinuation, with variable times to symptom onset (1 day to years) and symptom resolution (median of 3 weeks).
7. Drug Interactions
[See Clinical Pharmacology (12.3).]
VYTORIN
7.1 Strong CYP3A4 Inhibitors, Cyclosporine, or Danazol
Strong CYP3A4 inhibitors: The risk of myopathy is increased by reducing the elimination of the simvastatin component of VYTORIN. Hence when VYTORIN is used with an inhibitor of CYP3A4 (e.g., as listed below), elevated plasma levels of HMG-CoA reductase inhibitory activity increases the risk of myopathy and rhabdomyolysis, particularly with higher doses of VYTORIN. [See Warnings and Precautions (5.1) and Clinical Pharmacology (12.3).] Concomitant use of drugs labeled as having a strong inhibitory effect on CYP3A4 is contraindicated [see Contraindications (4)]. If treatment with itraconazole, ketoconazole, posaconazole, voriconazole, erythromycin, clarithromycin or telithromycin is unavoidable, therapy with VYTORIN must be suspended during the course of treatment.
Cyclosporine or Danazol: The risk of myopathy, including rhabdomyolysis is increased by concomitant administration of cyclosporine or danazol. Therefore, concomitant use of these drugs is contraindicated [see Contraindications (4), Warnings and Precautions (5.1) and Clinical Pharmacology (12.3)].
7.2 Lipid-Lowering Drugs That Can Cause Myopathy When Given Alone
Gemfibrozil: Contraindicated with VYTORIN [see Contraindications (4) and Warnings and Precautions (5.1)].
Fenofibrates (e.g., fenofibrate and fenofibric acid): Caution should be used when prescribing with VYTORIN [see Warnings and Precautions (5.1) and Drug Interactions (7.7)].
7.3 Amiodarone, Dronedarone, Ranolazine, or Calcium Channel Blockers
The risk of myopathy, including rhabdomyolysis, is increased by concomitant administration of amiodarone, dronedarone, ranolazine, or calcium channel blockers such as verapamil, diltiazem or amlodipine [see Dosage and Administration (2.3) and Warnings and Precautions (5.1) and Table 6 in Clinical Pharmacology (12.3)].
7.4 Niacin
Cases of myopathy/rhabdomyolysis have been observed with simvastatin coadministered with lipid-modifying doses (≥1 g/day niacin) of niacin-containing products. The risk of myopathy is greater in Chinese patients. In a clinical trial (median follow-up 3.9 years) involving patients at high risk of cardiovascular disease and with well-controlled LDL-C levels on simvastatin 40 mg/day with or without ezetimibe 10 mg/day, there was no incremental benefit on cardiovascular outcomes with the addition of lipid-modifying doses (≥1 g/day) of niacin. Coadministration of VYTORIN with lipid-modifying doses (≥1 g/day) of niacin is not recommended in Chinese patients. It is unknown if this risk applies to other Asian patients [see Warnings and Precautions (5.1) and Use in Specific Populations (8.8)].
7.5 Cholestyramine
Concomitant cholestyramine administration decreased the mean AUC of total ezetimibe approximately 55%. The incremental LDL-C reduction due to adding VYTORIN to cholestyramine may be reduced by this interaction.
7.6 Digoxin
In one study, concomitant administration of digoxin with simvastatin resulted in a slight elevation in plasma digoxin concentrations. Patients taking digoxin should be monitored appropriately when VYTORIN is initiated.
7.7 Fenofibrates (e.g., fenofibrate and fenofibric acid)
The safety and effectiveness of VYTORIN administered with fibrates have not been established. Because it is known that the risk of myopathy during treatment with HMG-CoA reductase inhibitors is increased with concurrent administration of fenofibrates, VYTORIN should be administered with caution when used concomitantly with a fenofibrate [see Warnings and Precautions (5.1)].
Fenofibrates may increase cholesterol excretion into the bile, leading to cholelithiasis. In a preclinical study in dogs, ezetimibe increased cholesterol in the gallbladder bile [see Animal Toxicology and/or Pharmacology (13.2)]. If cholelithiasis is suspected in a patient receiving VYTORIN and a fenofibrate, gallbladder studies are indicated and alternative lipid-lowering therapy should be considered [see the product labeling for fenofibrate and fenofibric acid].
7.8 Coumarin Anticoagulants
Simvastatin 20-40 mg/day modestly potentiated the effect of coumarin anticoagulants: the prothrombin time, reported as International Normalized Ratio (INR), increased from a baseline of 1.7 to 1.8 and from 2.6 to 3.4 in a normal volunteer study and in a hypercholesterolemic patient study, respectively. With other statins, clinically evident bleeding and/or increased prothrombin time has been reported in a few patients taking coumarin anticoagulants concomitantly. In such patients, prothrombin time should be determined before starting VYTORIN and frequently enough during early therapy to ensure that no significant alteration of prothrombin time occurs. Once a stable prothrombin time has been documented, prothrombin times can be monitored at the intervals usually recommended for patients on coumarin anticoagulants. If the dose of VYTORIN is changed or discontinued, the same procedure should be repeated. Simvastatin therapy has not been associated with bleeding or with changes in prothrombin time in patients not taking anticoagulants.
Concomitant administration of ezetimibe (10 mg once daily) had no significant effect on bioavailability of warfarin and prothrombin time in a study of twelve healthy adult males. There have been postmarketing reports of increased INR in patients who had ezetimibe added to warfarin. Most of these patients were also on other medications.
The effect of VYTORIN on the prothrombin time has not been studied.
7.9 Colchicine
Cases of myopathy, including rhabdomyolysis, have been reported with simvastatin coadministered with colchicine, and caution should be exercised when prescribing VYTORIN with colchicine.
7.10 Daptomycin
Cases of rhabdomyolysis have been reported with VYTORIN administered with daptomycin. Both VYTORIN and daptomycin can cause myopathy and rhabdomyolysis when given alone and the risk of myopathy and rhabdomyolysis may be increased by coadministration. Temporarily suspend VYTORIN in patients taking daptomycin [see Warnings and Precautions (5.1)].
8. Use In Specific Populations
8.3 Nursing Mothers
It is not known whether simvastatin is excreted in human milk. Because a small amount of another drug in this class is excreted in human milk and because of the potential for serious adverse reactions in nursing infants, women taking simvastatin should not nurse their infants. A decision should be made whether to discontinue nursing or discontinue drug, taking into account the importance of the drug to the mother [see Contraindications (4)].
In rat studies, exposure to ezetimibe in nursing pups was up to half of that observed in maternal plasma. It is not known whether ezetimibe or simvastatin are excreted into human breast milk. Because a small amount of another drug in the same class as simvastatin is excreted in human milk and because of the potential for serious adverse reactions in nursing infants, women who are nursing should not take VYTORIN [see Contraindications (4)].
8.4 Pediatric Use
The effects of ezetimibe coadministered with simvastatin (n=126) compared to simvastatin monotherapy (n=122) have been evaluated in adolescent boys and girls with heterozygous familial hypercholesterolemia (HeFH). In a multicenter, double-blind, controlled study followed by an open-label phase, 142 boys and 106 postmenarchal girls, 10 to 17 years of age (mean age 14.2 years, 43% females, 82% Caucasians, 4% Asian, 2% Blacks, 13% multiracial) with HeFH were randomized to receive either ezetimibe coadministered with simvastatin or simvastatin monotherapy. Inclusion in the study required 1) a baseline LDL-C level between 160 and 400 mg/dL and 2) a medical history and clinical presentation consistent with HeFH. The mean baseline LDL-C value was 225 mg/dL (range: 161-351 mg/dL) in the ezetimibe coadministered with simvastatin group compared to 219 mg/dL (range: 149-336 mg/dL) in the simvastatin monotherapy group. The patients received coadministered ezetimibe and simvastatin (10 mg, 20 mg, or 40 mg) or simvastatin monotherapy (10 mg, 20 mg, or 40 mg) for 6 weeks, coadministered ezetimibe and 40 mg simvastatin or 40 mg simvastatin monotherapy for the next 27 weeks, and open-label coadministered ezetimibe and simvastatin (10 mg, 20 mg, or 40 mg) for 20 weeks thereafter.
The results of the study at Week 6 are summarized in Table 3. Results at Week 33 were consistent with those at Week 6.
| Total-C | LDL-C | Apo B | Non-HDL-C | TG* | HDL-C | |
|---|---|---|---|---|---|---|
|
||||||
| Mean percent difference between treatment groups | -12% | -15% | -12% | -14% | -2% | +0.1% |
| 95% Confidence Interval | (-15%, -9%) | (-18%, -12%) | (-15%, -9%) | (-17%, -11%) | (-9, +4) | (-3, +3) |
From the start of the trial to the end of Week 33, discontinuations due to an adverse reaction occurred in 7 (6%) patients in the ezetimibe coadministered with simvastatin group and in 2 (2%) patients in the simvastatin monotherapy group.
During the trial, hepatic transaminase elevations (two consecutive measurements for ALT and/or AST ≥3 × ULN) occurred in four (3%) individuals in the ezetimibe coadministered with simvastatin group and in two (2%) individuals in the simvastatin monotherapy group. Elevations of CPK (≥10 × ULN) occurred in two (2%) individuals in the ezetimibe coadministered with simvastatin group and in zero individuals in the simvastatin monotherapy group.
In this limited controlled study, there was no significant effect on growth or sexual maturation in the adolescent boys or girls, or on menstrual cycle length in girls.
Coadministration of ezetimibe with simvastatin at doses greater than 40 mg/day has not been studied in adolescents. Also, VYTORIN has not been studied in patients younger than 10 years of age or in pre-menarchal girls.
8.5 Geriatric Use
Of the 10,189 patients who received VYTORIN in clinical studies, 3242 (32%) were 65 and older (this included 844 (8%) who were 75 and older). No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients but greater sensitivity of some older individuals cannot be ruled out. Since advanced age (≥65 years) is a predisposing factor for myopathy, VYTORIN should be prescribed with caution in the elderly. [See Clinical Pharmacology (12.3).]
Because advanced age (≥65 years) is a predisposing factor for myopathy, including rhabdomyolysis, VYTORIN should be prescribed with caution in the elderly. In a clinical trial of patients treated with simvastatin 80 mg/day, patients ≥65 years of age had an increased risk of myopathy, including rhabdomyolysis, compared to patients <65 years of age. [See Warnings and Precautions (5.1) and Clinical Pharmacology (12.3).]
8.6 Renal Impairment
In the SHARP trial of 9270 patients with moderate to severe renal impairment (6247 non-dialysis patients with median serum creatinine 2.5 mg/dL and median estimated glomerular filtration rate 25.6 mL/min/1.73 m2, and 3023 dialysis patients), the incidence of serious adverse events, adverse events leading to discontinuation of study treatment, or adverse events of special interest (musculoskeletal adverse events, liver enzyme abnormalities, incident cancer) was similar between patients ever assigned to VYTORIN 10/20 mg (n=4650) or placebo (n=4620) during a median follow-up of 4.9 years. However, because renal impairment is a risk factor for statin-associated myopathy, doses of VYTORIN exceeding 10/20 mg should be used with caution and close monitoring in patients with moderate to severe renal impairment. [See Dosage and Administration (2.5), Adverse Reactions (6.1), and Clinical Studies (14.3).]
8.7 Hepatic Impairment
VYTORIN is contraindicated in patients with active liver disease or unexplained persistent elevations in hepatic transaminases. [See Contraindications (4) and Warnings and Precautions (5.3).]
8.8 Chinese Patients
In a clinical trial in which patients at high risk of cardiovascular disease were treated with simvastatin 40 mg/day (median follow-up 3.9 years), the incidence of myopathy was approximately 0.05% for non-Chinese patients (n=7367) compared with 0.24% for Chinese patients (n=5468). The incidence of myopathy for Chinese patients on simvastatin 40 mg/day or ezetimibe and simvastatin 10/40 mg/day coadministered with extended-release niacin 2 g/day was 1.24%.
Chinese patients may be at higher risk for myopathy, monitor patients appropriately. Coadministration of VYTORIN with lipid-modifying doses (≥1 g/day niacin) of niacin-containing products is not recommended in Chinese patients [see Warnings and Precautions (5.1), Drug Interactions (7.4)].
11. Vytorin Description
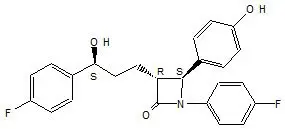
VYTORIN contains ezetimibe, a selective inhibitor of intestinal cholesterol and related phytosterol absorption, and simvastatin, an HMG-CoA reductase inhibitor.
The chemical name of ezetimibe is 1-(4-fluorophenyl)-3(R)-[3-(4-fluorophenyl)-3(S)-hydroxypropyl]-4(S)-(4-hydroxyphenyl)-2-azetidinone. The empirical formula is C24H21F2NO3 and its molecular weight is 409.4.
Ezetimibe is a white, crystalline powder that is freely to very soluble in ethanol, methanol, and acetone and practically insoluble in water. Its structural formula is:
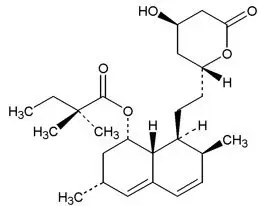
Simvastatin, an inactive lactone, is hydrolyzed to the corresponding β-hydroxyacid form, which is an inhibitor of HMG-CoA reductase. Simvastatin is butanoic acid, 2,2-dimethyl-,1,2,3,7,8,8a-hexahydro-3,7-dimethyl-8-[2-(tetrahydro-4-hydroxy-6-oxo-2H-pyran-2-yl)-ethyl]-1-naphthalenyl ester, [1S-[1α,3α,7β,8β(2S*,4S*),-8aβ]]. The empirical formula of simvastatin is C25H38O5 and its molecular weight is 418.57.
Simvastatin is a white to off-white, nonhygroscopic, crystalline powder that is practically insoluble in water and freely soluble in chloroform, methanol and ethanol. Its structural formula is:
VYTORIN is available for oral use as tablets containing 10 mg of ezetimibe, and 10 mg of simvastatin (VYTORIN 10/10), 20 mg of simvastatin (VYTORIN 10/20), 40 mg of simvastatin (VYTORIN 10/40), or 80 mg of simvastatin (VYTORIN 10/80). Each tablet contains the following inactive ingredients: butylated hydroxyanisole NF, citric acid monohydrate USP, croscarmellose sodium NF, hypromellose USP, lactose monohydrate NF, magnesium stearate NF, microcrystalline cellulose NF, and propyl gallate NF.
12. Vytorin - Clinical Pharmacology
12.2 Pharmacodynamics
Clinical studies have demonstrated that elevated levels of total-C, LDL-C and Apo B, the major protein constituent of LDL, promote human atherosclerosis. In addition, decreased levels of HDL-C are associated with the development of atherosclerosis. Epidemiologic studies have established that cardiovascular morbidity and mortality vary directly with the level of total-C and LDL-C and inversely with the level of HDL-C. Like LDL, cholesterol-enriched triglyceride-rich lipoproteins, including VLDL, intermediate-density lipoproteins (IDL), and remnants, can also promote atherosclerosis. The independent effect of raising HDL-C or lowering TG on the risk of coronary and cardiovascular morbidity and mortality has not been determined.
12.3 Pharmacokinetics
The results of a bioequivalence study in healthy subjects demonstrated that the VYTORIN (ezetimibe and simvastatin) 10 mg/10 mg to 10 mg/80 mg combination tablets are bioequivalent to coadministration of corresponding doses of ezetimibe (ZETIA®) and simvastatin (ZOCOR®) as individual tablets.
Drug Interactions [See also Drug Interactions (7).]
No clinically significant pharmacokinetic interaction was seen when ezetimibe was coadministered with simvastatin. No specific pharmacokinetic drug interaction studies with VYTORIN have been conducted other than the following study with NIASPAN (Niacin extended-release tablets).
Cytochrome P450: Ezetimibe had no significant effect on a series of probe drugs (caffeine, dextromethorphan, tolbutamide, and IV midazolam) known to be metabolized by cytochrome P450 (1A2, 2D6, 2C8/9 and 3A4) in a "cocktail" study of twelve healthy adult males. This indicates that ezetimibe is neither an inhibitor nor an inducer of these cytochrome P450 isozymes, and it is unlikely that ezetimibe will affect the metabolism of drugs that are metabolized by these enzymes.
In a study of 12 healthy volunteers, simvastatin at the 80-mg dose had no effect on the metabolism of the probe cytochrome P450 isoform 3A4 (CYP3A4) substrates midazolam and erythromycin. This indicates that simvastatin is not an inhibitor of CYP3A4 and, therefore, is not expected to affect the plasma levels of other drugs metabolized by CYP3A4.
Simvastatin acid is a substrate of the transport protein OATP1B1. Concomitant administration of medicinal products that are inhibitors of the transport protein OATP1B1 may lead to increased plasma concentrations of simvastatin acid and an increased risk of myopathy. For example, cyclosporine has been shown to increase the AUC of statins; although the mechanism is not fully understood, the increase in AUC for simvastatin acid is presumably due, in part, to inhibition of CYP3A4 and/or OATP1B1.
Simvastatin is a substrate for CYP3A4. Inhibitors of CYP3A4 can raise the plasma levels of HMG-CoA reductase inhibitory activity and increase the risk of myopathy. [See Warnings and Precautions (5.1); Drug Interactions (7.1).]
Simvastatin
| Coadministered Drug or Grapefruit Juice | Dosing of Coadministered Drug or Grapefruit Juice | Dosing of Simvastatin | Geometric Mean Ratio (Ratio* with / without coadministered drug) No Effect = 1.00 |
||
|---|---|---|---|---|---|
| AUC | Cmax | ||||
|
|||||
| Contraindicated with VYTORIN [see Contraindications (4) and Warnings and Precautions (5.1)] | |||||
| Telithromycin† | 200 mg QD for 4 days | 80 mg | simvastatin acid‡ | 12 | 15 |
| simvastatin | 8.9 | 5.3 | |||
| Nelfinavir† | 1250 mg BID for 14 days | 20 mg QD for 28 days | simvastatin acid‡ | ||
| simvastatin | 6 | 6.2 | |||
| Itraconazole† | 200 mg QD for 4 days | 80 mg | simvastatin acid‡ | 13.1 | |
| simvastatin | 13.1 | ||||
| Posaconazole | 100 mg (oral suspension) QD for 13 days | 40 mg | simvastatin acid‡ | 7.3 | 9.2 |
| simvastatin | 10.3 | 9.4 | |||
| 200 mg (oral suspension) QD for 13 days | 40 mg | simvastatin acid‡ | 8.5 | 9.5 | |
| simvastatin | 10.6 | 11.4 | |||
| Gemfibrozil | 600 mg BID for 3 days | 40 mg | simvastatin acid‡ | 2.85 | 2.18 |
| simvastatin | 1.35 | 0.91 | |||
| Avoid grapefruit juice with VYTORIN [see Warnings and Precautions (5.1)] | |||||
| Grapefruit Juice§
(high dose) | 200 mL of double-strength TID¶ | 60 mg single dose | simvastatin acid | 7 | |
| simvastatin | 16 | ||||
| Grapefruit Juice§
(low dose) | 8 oz (about 237 mL) of single-strength# | 20 mg single dose | simvastatin acid | 1.3 | |
| simvastatin | 1.9 | ||||
| Avoid taking with >10/10 mg VYTORIN, based on clinical and/or postmarketing simvastatin experience [see Warnings and Precautions (5.1)] | |||||
| Verapamil SR | 240 mg QD Days 1-7 then 240 mg BID on Days 8-10 | 80 mg on Day 10 | simvastatin acid | 2.3 | 2.4 |
| simvastatin | 2.5 | 2.1 | |||
| Diltiazem | 120 mg BID for 10 days | 80 mg on Day 10 | simvastatin acid | 2.69 | 2.69 |
| simvastatin | 3.10 | 2.88 | |||
| Diltiazem | 120 mg BID for 14 days | 20 mg on Day 14 | simvastatin | 4.6 | 3.6 |
| Dronedarone | 400 mg BID for 14 days | 40 mg QD for 14 days | simvastatin acid | 1.96 | 2.14 |
| simvastatin | 3.90 | 3.75 | |||
| Avoid taking with >10/20 mg VYTORIN, based on clinical and/or postmarketing simvastatin experience [see Warnings and Precautions (5.1)] | |||||
| Amiodarone | 400 mg QD for 3 days | 40 mg on Day 3 | simvastatin acid | 1.75 | 1.72 |
| simvastatin | 1.76 | 1.79 | |||
| Amlodipine | 10 mg QD for 10 days | 80 mg on Day 10 | simvastatin acid | 1.58 | 1.56 |
| simvastatin | 1.77 | 1.47 | |||
| Ranolazine SR | 1000 mg BID for 7 days | 80 mg on Day 1 and Days 6-9 | simvastatin acid | 2.26 | 2.28 |
| simvastatin | 1.86 | 1.75 | |||
| Avoid taking with >10/20 mg VYTORIN (or 10/40 mg for patients who have previously taken 80 mg simvastatin chronically, e.g., for 12 months or more, without evidence of muscle toxicity), based on clinical experience | |||||
| Lomitapide | 60 mg QD for 7 days | 40 mg single dose | simvastatin acid | 1.7 | 1.6 |
| simvastatin | 2 | 2 | |||
| Lomitapide | 10 mg QD for 7 days | 20 mg single dose | simvastatin acid | 1.4 | 1.4 |
| simvastatin | 1.6 | 1.7 | |||
| No dosing adjustments required for the following: | |||||
| Fenofibrate | 160 mg QD for 14 days | 80 mg QD on Days 8-14 | simvastatin acid | 0.64 | 0.89 |
| simvastatin | 0.89 | 0.83 | |||
| Propranolol | 80 mg single dose | 80 mg single dose | total inhibitor | 0.79 | ↓ from 33.6 to 21.1 ng∙eq/mL |
| active inhibitor | 0.79 | ↓ from 7.0 to 4.7 ng∙eq/mL | |||
13. Nonclinical Toxicology
14. Clinical Studies
14.1 Primary Hyperlipidemia
VYTORIN
VYTORIN reduces total-C, LDL-C, Apo B, TG, and non-HDL-C, and increases HDL-C in patients with hyperlipidemia. Maximal to near maximal response is generally achieved within 2 weeks and maintained during chronic therapy.
VYTORIN is effective in men and women with hyperlipidemia. Experience in non-Caucasians is limited and does not permit a precise estimate of the magnitude of the effects of VYTORIN.
Five multicenter, double-blind studies conducted with either VYTORIN or coadministered ezetimibe and simvastatin equivalent to VYTORIN in patients with primary hyperlipidemia are reported: two were comparisons with simvastatin, two were comparisons with atorvastatin, and one was a comparison with rosuvastatin.
In a multicenter, double-blind, placebo-controlled, 12-week trial, 1528 hyperlipidemic patients were randomized to one of ten treatment groups: placebo, ezetimibe (10 mg), simvastatin (10 mg, 20 mg, 40 mg, or 80 mg), or VYTORIN (10/10, 10/20, 10/40, or 10/80).
When patients receiving VYTORIN were compared to those receiving all doses of simvastatin, VYTORIN significantly lowered total-C, LDL-C, Apo B, TG, and non-HDL-C. The effects of VYTORIN on HDL-C were similar to the effects seen with simvastatin. Further analysis showed VYTORIN significantly increased HDL-C compared with placebo. (See Table 7.) The lipid response to VYTORIN was similar in patients with TG levels greater than or less than 200 mg/dL.
| Treatment | |||||||
|---|---|---|---|---|---|---|---|
| (Daily Dose) | N | Total-C | LDL-C | Apo B | HDL-C | TG* | Non-HDL-C |
|
|||||||
| Pooled data (All VYTORIN doses)‡ | 609 | -38 | -53 | -42 | +7 | -24 | -49 |
| Pooled data (All simvastatin doses)‡ | 622 | -28 | -39 | -32 | +7 | -21 | -36 |
| Ezetimibe 10 mg | 149 | -13 | -19 | -15 | +5 | -11 | -18 |
| Placebo | 148 | -1 | -2 | 0 | 0 | -2 | -2 |
| VYTORIN by dose | |||||||
| 10/10 | 152 | -31 | -45 | -35 | +8 | -23 | -41 |
| 10/20 | 156 | -36 | -52 | -41 | +10 | -24 | -47 |
| 10/40 | 147 | -39 | -55 | -44 | +6 | -23 | -51 |
| 10/80 | 154 | -43 | -60 | -49 | +6 | -31 | -56 |
| Simvastatin by dose | |||||||
| 10 mg | 158 | -23 | -33 | -26 | +5 | -17 | -30 |
| 20 mg | 150 | -24 | -34 | -28 | +7 | -18 | -32 |
| 40 mg | 156 | -29 | -41 | -33 | +8 | -21 | -38 |
| 80 mg | 158 | -35 | -49 | -39 | +7 | -27 | -45 |
In a multicenter, double-blind, controlled, 23-week study, 710 patients with known CHD or CHD risk equivalents, as defined by the NCEP ATP III guidelines, and an LDL-C ≥130 mg/dL were randomized to one of four treatment groups: coadministered ezetimibe and simvastatin equivalent to VYTORIN (10/10, 10/20, and 10/40) or simvastatin 20 mg. Patients not reaching an LDL-C <100 mg/dL had their simvastatin dose titrated at 6-week intervals to a maximal dose of 80 mg.
At Week 5, the LDL-C reductions with VYTORIN 10/10, 10/20, or 10/40 were significantly larger than with simvastatin 20 mg (see Table 8).
| Simvastatin 20 mg | VYTORIN 10/10 | VYTORIN 10/20 | VYTORIN 10/40 |
|
|---|---|---|---|---|
| N | 253 | 251 | 109 | 97 |
| Mean baseline LDL-C | 174 | 165 | 167 | 171 |
| Percent change LDL-C | -38 | -47 | -53 | -59 |
In a multicenter, double-blind, 6-week study, 1902 patients with primary hyperlipidemia, who had not met their NCEP ATP III target LDL-C goal, were randomized to one of eight treatment groups: VYTORIN (10/10, 10/20, 10/40, or 10/80) or atorvastatin (10 mg, 20 mg, 40 mg, or 80 mg).
Across the dosage range, when patients receiving VYTORIN were compared to those receiving milligram-equivalent statin doses of atorvastatin, VYTORIN lowered total-C, LDL-C, Apo B, and non-HDL-C significantly more than atorvastatin. Only the 10/40 mg and 10/80 mg VYTORIN doses increased HDL-C significantly more than the corresponding milligram-equivalent statin dose of atorvastatin. The effects of VYTORIN on TG were similar to the effects seen with atorvastatin. (See Table 9.)
| Treatment | |||||||
|---|---|---|---|---|---|---|---|
| (Daily Dose) | N | Total-C‡ | LDL-C‡ | Apo B‡ | HDL-C | TG* | Non-HDL-C‡ |
|
|||||||
| VYTORIN by dose | |||||||
| 10/10 | 230 | -34§ | -47§ | -37§ | +8 | -26 | -43§ |
| 10/20 | 233 | -37§ | -51§ | -40§ | +7 | -25 | -46§ |
| 10/40 | 236 | -41§ | -57§ | -46§ | +9§ | -27 | -52§ |
| 10/80 | 224 | -43§ | -59§ | -48§ | +8§ | -31 | -54§ |
| Atorvastatin by dose | |||||||
| 10 mg | 235 | -27 | -36 | -31 | +7 | -21 | -34 |
| 20 mg | 230 | -32 | -44 | -37 | +5 | -25 | -41 |
| 40 mg | 232 | -36 | -48 | -40 | +4 | -24 | -45 |
| 80 mg | 230 | -40 | -53 | -44 | +1 | -32 | -50 |
In a multicenter, double-blind, 24-week, forced-titration study, 788 patients with primary hyperlipidemia, who had not met their NCEP ATP III target LDL-C goal, were randomized to receive coadministered ezetimibe and simvastatin equivalent to VYTORIN (10/10 and 10/20) or atorvastatin 10 mg. For all three treatment groups, the dose of the statin was titrated at 6-week intervals to 80 mg. At each pre-specified dose comparison, VYTORIN lowered LDL-C to a greater degree than atorvastatin (see Table 10).
| Treatment | N | Total-C | LDL-C | Apo B | HDL-C | TG* | Non-HDL-C |
|---|---|---|---|---|---|---|---|
|
|||||||
| Week 6 | |||||||
| Atorvastatin 10 mg‡ | 262 | -28 | -37 | -32 | +5 | -23 | -35 |
| VYTORIN 10/10§ | 263 | -34¶ | -46¶ | -38¶ | +8¶ | -26 | -43¶ |
| VYTORIN 10/20# | 263 | -36¶ | -50¶ | -41¶ | +10¶ | -25 | -46¶ |
| Week 12 | |||||||
| Atorvastatin 20 mg | 246 | -33 | -44 | -38 | +7 | -28 | -42 |
| VYTORIN 10/20 | 250 | -37¶ | -50¶ | -41¶ | +9 | -28 | -46¶ |
| VYTORIN 10/40 | 252 | -39¶ | -54¶ | -45¶ | +12¶ | -31 | -50¶ |
| Week 18 | |||||||
| Atorvastatin 40 mg | 237 | -37 | -49 | -42 | +8 | -31 | -47 |
| VYTORIN 10/40Þ | 482 | -40¶ | -56¶ | -45¶ | +11¶ | -32 | -52¶ |
| Week 24 | |||||||
| Atorvastatin 80 mg | 228 | -40 | -53 | -45 | +6 | -35 | -50 |
| VYTORIN 10/80Þ | 459 | -43¶ | -59¶ | -49¶ | +12¶ | -35 | -55¶ |
In a multicenter, double-blind, 6-week study, 2959 patients with primary hyperlipidemia, who had not met their NCEP ATP III target LDL-C goal, were randomized to one of six treatment groups: VYTORIN (10/20, 10/40, or 10/80) or rosuvastatin (10 mg, 20 mg, or 40 mg).
The effects of VYTORIN and rosuvastatin on total-C, LDL-C, Apo B, TG, non-HDL-C and HDL-C are shown in Table 11.
| Treatment (Daily Dose) | N | Total-C‡ | LDL-C‡ | Apo B‡ | HDL-C | TG* | Non-HDL-C‡ |
|---|---|---|---|---|---|---|---|
|
|||||||
| VYTORIN by dose | |||||||
| 10/20 | 476 | -37§ | -52§ | -42§ | +7 | -23§ | -47§ |
| 10/40 | 477 | -39¶ | -55¶ | -44¶ | +8 | -27 | -50¶ |
| 10/80 | 474 | -44# | -61# | -50# | +8 | -30# | -56# |
| Rosuvastatin by dose | |||||||
| 10 mg | 475 | -32 | -46 | -37 | +7 | -20 | -42 |
| 20 mg | 478 | -37 | -52 | -43 | +8 | -26 | -48 |
| 40 mg | 475 | -41 | -57 | -47 | +8 | -28 | -52 |
In a multicenter, double-blind, 24-week trial, 214 patients with type 2 diabetes mellitus treated with thiazolidinediones (rosiglitazone or pioglitazone) for a minimum of 3 months and simvastatin 20 mg for a minimum of 6 weeks were randomized to receive either simvastatin 40 mg or the coadministered active ingredients equivalent to VYTORIN 10/20. The median LDL-C and HbA1c levels at baseline were 89 mg/dL and 7.1%, respectively.
VYTORIN 10/20 was significantly more effective than doubling the dose of simvastatin to 40 mg. The median percent changes from baseline for VYTORIN vs. simvastatin were: LDL-C -25% and -5%; total-C -16% and -5%; Apo B -19% and -5%; and non-HDL-C -23% and -5%. Results for HDL-C and TG between the two treatment groups were not significantly different.
14.2 Homozygous Familial Hypercholesterolemia (HoFH)
A double-blind, randomized, 12-week study was performed in patients with a clinical and/or genotypic diagnosis of HoFH. Data were analyzed from a subgroup of patients (n=14) receiving simvastatin 40 mg at baseline. Increasing the dose of simvastatin from 40 to 80 mg (n=5) produced a reduction of LDL-C of 13% from baseline on simvastatin 40 mg. Coadministered ezetimibe and simvastatin equivalent to VYTORIN (10/40 and 10/80 pooled, n=9), produced a reduction of LDL-C of 23% from baseline on simvastatin 40 mg. In those patients coadministered ezetimibe and simvastatin equivalent to VYTORIN (10/80, n=5), a reduction of LDL-C of 29% from baseline on simvastatin 40 mg was produced.
14.3 Chronic Kidney Disease (CKD)
The Study of Heart and Renal Protection (SHARP) was a multinational, randomized, placebo-controlled, double-blind trial that investigated the effect of VYTORIN on the time to a first major vascular event (MVE) among 9438 patients with moderate to severe chronic kidney disease (approximately one-third on dialysis at baseline) who did not have a history of myocardial infarction or coronary revascularization. An MVE was defined as nonfatal MI, cardiac death, stroke, or any revascularization procedure. Patients were allocated to treatment using a method that took into account the distribution of 8 important baseline characteristics of patients already enrolled and minimized the imbalance of those characteristics across the groups.
For the first year, 9438 patients were allocated 4:4:1, to VYTORIN 10/20, placebo, or simvastatin 20 mg daily, respectively. The 1-year simvastatin arm enabled the comparison of VYTORIN to simvastatin with regard to safety and effect on lipid levels. At 1 year the simvastatin-only arm was re-allocated 1:1 to VYTORIN 10/20 or placebo. A total of 9270 patients were ever allocated to VYTORIN 10/20 (n=4650) or placebo (n=4620) during the trial. The median follow-up duration was 4.9 years. Patients had a mean age of 61 years; 63% were male, 72% were Caucasian, and 23% were diabetic; and, for those not on dialysis at baseline, the median serum creatinine was 2.5 mg/dL and the median estimated glomerular filtration rate (eGFR) was 25.6 mL/min/1.73 m2, with 94% of patients having an eGFR < 45 mL/min/1.73m2. Eligibility did not depend on lipid levels. Mean LDL-C at baseline was 108 mg/dL. At 1 year, the mean LDL-C was 26% lower in the simvastatin arm and 38% lower in the VYTORIN arm relative to placebo. At the midpoint of the study (2.5 years), the mean LDL-C was 32% lower for VYTORIN relative to placebo. Patients no longer taking study medication were included in all lipid measurements.
In the primary intent-to-treat analysis, 639 (15.2%) of 4193 patients initially allocated to VYTORIN and 749 (17.9%) of 4191 patients initially allocated to placebo experienced an MVE. This corresponded to a relative risk reduction of 16% (p=0.001) (see Figure 1). Similarly, 526 (11.3%) of 4650 patients ever allocated to VYTORIN and 619 (13.4%) of 4620 patients ever allocated to placebo experienced a major atherosclerotic event (MAE; a subset of the MVE composite that excluded non-coronary cardiac deaths and hemorrhagic stroke), corresponding to a relative risk reduction of 17% (p=0.002). The trial demonstrated that treatment with VYTORIN 10/20 mg versus placebo reduced the risk for MVE and MAE in this CKD population. The study design precluded drawing conclusions regarding the independent contribution of either ezetimibe or simvastatin to the observed effect.
The treatment effect of VYTORIN on MVE was attenuated among patients on dialysis at baseline compared with those not on dialysis at baseline. Among 3023 patients on dialysis at baseline, VYTORIN reduced the risk of MVE by 6% (RR 0.94: 95% CI 0.80-1.09) compared with 22% (RR 0.78: 95% CI 0.69-0.89) among 6247 patients not on dialysis at baseline (interaction P=0.08).
| Figure 1: Effect of VYTORIN on the Primary Endpoint of Risk of Major Vascular Events |
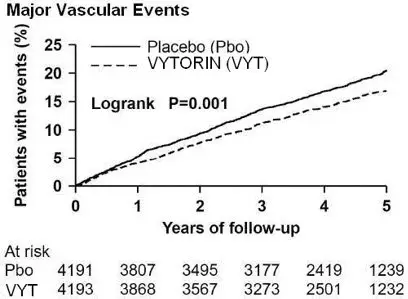 |
The individual components of MVE in all patients ever allocated to VYTORIN or placebo are presented in Table 12.
| Outcome | VYTORIN 10/20 (N=4650) | Placebo (N=4620) | Risk Ratio (95% CI) | P-value |
|---|---|---|---|---|
|
||||
| Major Vascular Events | 701 (15.1%) | 814 (17.6%) | 0.85 (0.77-0.94) | 0.001 |
| Nonfatal MI | 134 (2.9%) | 159 (3.4%) | 0.84 (0.66-1.05) | 0.12 |
| Cardiac Death | 253 (5.4%) | 272 (5.9%) | 0.93 (0.78-1.10) | 0.38 |
| Any Stroke | 171 (3.7%) | 210 (4.5%) | 0.81 (0.66-0.99) | 0.038 |
| Non-hemorrhagic Stroke | 131 (2.8%) | 174 (3.8%) | 0.75 (0.60-0.94) | 0.011 |
| Hemorrhagic Stroke | 45 (1.0%) | 37 (0.8%) | 1.21 (0.78-1.86) | 0.40 |
| Any Revascularization | 284 (6.1%) | 352 (7.6%) | 0.79 (0.68-0.93) | 0.004 |
Among patients not on dialysis at baseline, VYTORIN did not reduce the risk of progressing to end-stage renal disease compared with placebo (RR 0.97: 95% CI 0.89-1.05).
16. How is Vytorin supplied
No. 3873 — Tablets VYTORIN 10/10 are white to off-white capsule-shaped tablets with code "311" on one side.
They are supplied as follows:
NDC 66582-311-31 bottles of 30
NDC 66582-311-54 bottles of 90
NDC 66582-311-87 bottles of 10,000 (If repackaged in blisters, then opaque or light-resistant blisters should be used.)
No. 3874 — Tablets VYTORIN 10/20 are white to off-white capsule-shaped tablets with code "312" on one side.
They are supplied as follows:
NDC 66582-312-31 bottles of 30
NDC 66582-312-54 bottles of 90
No. 3875 — Tablets VYTORIN 10/40 are white to off-white capsule-shaped tablets with code "313" on one side.
They are supplied as follows:
NDC 66582-313-31 bottles of 30
NDC 66582-313-54 bottles of 90
No. 3876 — Tablets VYTORIN 10/80 are white to off-white capsule-shaped tablets with code "315" on one side.
They are supplied as follows:
NDC 66582-315-31 bottles of 30
NDC 66582-315-54 bottles of 90
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Patients should be advised to adhere to their National Cholesterol Education Program (NCEP)-recommended diet, a regular exercise program, and periodic testing of a fasting lipid panel.
Patients should be advised about substances they should not take concomitantly with VYTORIN [see Contraindications (4) and Warnings and Precautions (5.1)]. Patients should also be advised to inform other healthcare professionals prescribing a new medication or increasing the dose of an existing medication that they are taking VYTORIN.
17.1 Muscle Pain
All patients starting therapy with VYTORIN should be advised of the risk of myopathy, including rhabdomyolysis, and told to report promptly any unexplained muscle pain, tenderness or weakness particularly if accompanied by malaise or fever or if these muscle signs or symptoms persist after discontinuing VYTORIN. Patients using the 10/80-mg dose should be informed that the risk of myopathy, including rhabdomyolysis, is increased with the use of the 10/80-mg dose. The risk of myopathy, including rhabdomyolysis, occurring with use of VYTORIN is increased when taking certain types of medication or consuming grapefruit juice. Patients should discuss all medication, both prescription and over the counter, with their healthcare professional.
17.2 Liver Enzymes
It is recommended that liver function tests be performed before the initiation of VYTORIN, and thereafter when clinically indicated. All patients treated with VYTORIN should be advised to report promptly any symptoms that may indicate liver injury, including fatigue, anorexia, right upper abdominal discomfort, dark urine or jaundice.
17.3 Pregnancy
Women of childbearing age should be advised to use an effective method of birth control to prevent pregnancy while using VYTORIN. Discuss future pregnancy plans with your patients, and discuss when to stop taking VYTORIN if they are trying to conceive. Patients should be advised that if they become pregnant they should stop taking VYTORIN and call their healthcare professional.
Patient Information
VYTORIN® (VI-tor-in)
(ezetimibe and simvastatin)
Tablets
Read this Patient Information carefully before you start taking VYTORIN® and each time you get a refill. There may be new information. This information does not take the place of talking with your doctor about your medical condition or your treatment. If you have any questions about VYTORIN, ask your doctor. Only your doctor can determine if VYTORIN is right for you.
What is VYTORIN?
VYTORIN is a prescription medicine that contains 2 cholesterol lowering medicines, ezetimibe and simvastatin. VYTORIN is used along with diet to:
- lower the level of your "bad" cholesterol (LDL)
- increase the level of your "good" cholesterol (HDL)
- lower the level of fat in your blood (triglycerides)
VYTORIN is for patients who cannot control their cholesterol levels by diet and exercise alone.
VYTORIN has not been shown to reduce heart attacks or strokes more than simvastatin alone.
It is not known if VYTORIN is safe and effective in children under 10 years of age or in girls who have not started their period (menses).
The usual dose of VYTORIN is 10/10 mg to 10/40 mg 1 time each day.
VYTORIN 10/80 mg increases your chance of developing muscle damage. The 10/80 mg dose should only be used by people who:
- have been taking VYTORIN 10/80 mg chronically (such as 12 months or more) without having muscle damage
- do not need to take certain other medicines with VYTORIN that would increase your chance of getting muscle damage.
If you are unable to reach your LDL-cholesterol goal using VYTORIN 10/40 mg, your doctor should switch you to another cholesterol-lowering medicine.
Who should not take VYTORIN?
Do not take VYTORIN if you take:
- Certain anti-fungal medicines including:
- itraconazole
- ketoconazole
- posaconazole
- voriconazole
- HIV protease inhibitors (indinavir, nelfinavir, ritonavir, saquinavir, tipranavir, or atazanavir)
- Certain hepatitis C virus protease inhibitors (such as boceprevir or telaprevir)
- Certain antibiotics, including:
- erythromycin
- clarithromycin
- telithromycin
- nefazodone
- medicines containing cobicistat
- A fibric acid medicine for lowering cholesterol called gemfibrozil
- cyclosporine
- danazol
Ask your doctor or pharmacist for a list of these medicines if you are not sure.
Also do not take VYTORIN if you:
- are allergic to ezetimibe or simvastatin or any of the ingredients in VYTORIN. See the end of this leaflet for a complete list of ingredients in VYTORIN.
- have liver problems.
- are pregnant or plan to become pregnant. VYTORIN may harm your unborn baby. If you are a woman of childbearing age, you should use an effective method of birth control to prevent pregnancy while using VYTORIN. If you become pregnant while taking VYTORIN, stop taking VYTORIN and call your doctor.
- are breastfeeding or plan to breastfeed. It is not known if VYTORIN passes into your breast milk. You and your doctor should decide the best way to feed your baby if you take VYTORIN.
What should I tell my doctor before and while taking VYTORIN?
Tell your doctor if you:
- have unexplained muscle aches or weakness
- have kidney problems
- have or have had liver problems or drink more than 2 glasses of alcohol daily
- have thyroid problems
- are 65 years of age or older
- are Chinese
Also see "What are the possible side effects of VYTORIN?"
Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements.
Tell your doctor who prescribes VYTORIN if another doctor increases the dose of another medicine you are taking.
Talk to your doctor before you start taking any new medicines.
Taking VYTORIN with certain other medicines may affect each other causing side effects. VYTORIN may affect the way other medicines work, and other medicines may affect how VYTORIN works.
Taking VYTORIN with certain substances can increase the risk of muscle problems. It is especially important to tell your doctor if you take:
- fibric acid derivatives (such as fenofibrate)
- amiodarone or dronedarone (drugs used to treat an irregular heartbeat)
- verapamil, diltiazem, amlodipine, or ranolazine (drugs used to treat high blood pressure, chest pain associated with heart disease, or other heart conditions)
- grapefruit juice (which should be avoided while taking VYTORIN)
- colchicine (a medicine used to treat gout)
- lomitapide (a medicine used to treat a serious and rare genetic cholesterol condition)
- daptomycin (a drug used to treat complicated skin and bloodstream infections)
- large doses of niacin or nicotinic acid
Tell your doctor if you are taking niacin or a niacin-containing product, as this may increase your risk of muscle problems, especially if you are Chinese.
It is also important to tell your doctor if you are taking coumarin anticoagulants (drugs that prevent blood clots, such as warfarin).
Tell your doctor about all the medicines you take, including any prescription and nonprescription medicines, vitamins, and herbal supplements.
How should I take VYTORIN?
- Take VYTORIN exactly as your doctor tells you to take it.
- Do not change your dose or stop taking VYTORIN without talking to your doctor.
- Take VYTORIN 1 time each day in the evening.
- Take VYTORIN with or without food.
- While taking VYTORIN, continue to follow your cholesterol-lowering diet and to exercise as your doctor told you to.
- If you miss a dose, do not take an extra dose. Just resume your usual schedule.
- Your doctor should do fasting blood tests to check your cholesterol while you take VYTORIN. Your doctor may change your dose of VYTORIN if needed.
- If you take too much VYTORIN, call your doctor or Poison Control Center at 1-800-222-1222 or go to the nearest hospital emergency room right away.
What are the possible side effects of VYTORIN?
VYTORIN may cause serious side effects, including:
-
Muscle pain, tenderness and weakness (myopathy). Muscle problems, including muscle breakdown, can be serious in some people and rarely cause kidney damage that can lead to death.
Tell your doctor right away if:- you have unexplained muscle pain, tenderness, or weakness, especially if you have a fever or feel more tired than usual, while you take VYTORIN.
- you have muscle problems that do not go away even after your doctor has advised you to stop taking VYTORIN. Your doctor may do further tests to diagnose the cause of your muscle problems.
- are taking certain other medicines while you take VYTORIN
- are 65 years of age or older
- are female
- have thyroid problems (hypothyroidism) that are not controlled
- have kidney problems
- are taking higher doses of VYTORIN, particularly the 10/80 mg dose
- are Chinese
-
Liver problems. Your doctor should do blood tests to check your liver before you start taking VYTORIN and if you have any symptoms of liver problems while you take VYTORIN. Call your doctor right away if you have the following symptoms of liver problems:
- loss of appetite
- upper belly pain
- dark urine
- yellowing of your skin or the whites of your eyes
- feel tired or weak
The most common side effects of VYTORIN include:
- headache
- increased liver enzyme levels
- muscle pain
- upper respiratory infection
- diarrhea
Additional side effects that have been reported in general use with VYTORIN or with ezetimibe or simvastatin tablets (tablets that contain the active ingredients of VYTORIN) include:
- allergic reactions including swelling of the face, lips, tongue, and/or throat that may cause difficulty in breathing or swallowing (which may require treatment right away), rash, hives; joint pain; inflammation of the pancreas; nausea; dizziness; tingling sensation; depression; gallstones; trouble sleeping; poor memory; memory loss; confusion; erectile dysfunction; breathing problems including persistent cough and/or shortness of breath or fever.
Tell your doctor if you have any side effect that bothers you or does not go away.
These are not all the possible side effects of VYTORIN. For more information, ask your doctor or pharmacist.
Call your doctor about medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store VYTORIN?
- Store VYTORIN at room temperature between 68°F to 77°F (20°C to 25°C).
- Keep VYTORIN in its original container until you use it.
- Keep VYTORIN in a tightly closed container, and keep VYTORIN out of light.
Keep VYTORIN and all medicines out of the reach of children.
General Information about the safe and effective use of VYTORIN.
VYTORIN works to reduce your cholesterol in two ways. It reduces the cholesterol absorbed in your digestive tract, as well as the cholesterol your body makes by itself. VYTORIN does not help you lose weight.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use VYTORIN for a condition for which it was not prescribed. Do not give VYTORIN to other people, even if they have the same condition that you have. It may harm them.
This Patient Information summarizes the most important information about VYTORIN. If you would like more information, talk with your doctor. You can ask your pharmacist or doctor for information about VYTORIN that is written for health professionals.
For more information, go to www.VYTORIN.com, or call 1-800-672-6372.
What are the ingredients in VYTORIN?
Active Ingredients: ezetimibe and simvastatin
Inactive Ingredients: butylated hydroxyanisole NF, citric acid monohydrate USP, croscarmellose sodium NF, hypromellose USP, lactose monohydrate NF, magnesium stearate NF, microcrystalline cellulose NF, and propyl gallate NF.
This Patient Information has been approved by the U.S. Food and Drug Administration.
| VYTORIN
ezetimibe and simvastatin tablet |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| VYTORIN
ezetimibe and simvastatin tablet |
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
| VYTORIN
ezetimibe and simvastatin tablet |
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
| VYTORIN
ezetimibe and simvastatin tablet |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| Labeler - Merck Sharp & Dohme Corp. (001317601) |