Drug Detail:Xembify (subcutaneous) (Immune globulin (subcutaneous) [ im-myoon-glob-yoo-lin ])
Drug Class: Immune globulins
Highlights of Prescribing Information
XEMBIFY (immune globulin subcutaneous, human – klhw)
20% solution
Initial U.S. Approval: 2019
WARNING: THROMBOSIS
See full prescribing information for complete boxed warning.
- Thrombosis may occur with immune globulin products, including XEMBIFY. Risk factors may include: advanced age, prolonged immobilization, hypercoagulable conditions, history of venous or arterial thrombosis, use of estrogens, indwelling vascular catheters, hyperviscosity, and cardiovascular risk factors. Thrombosis may occur in the absence of known risk factors.
- For patients at risk of thrombosis, administer XEMBIFY at the minimum dose and infusion rate practicable. Ensure adequate hydration in patients before administration. Monitor for signs and symptoms of thrombosis and assess blood viscosity in patients at risk for hyperviscosity.
Indications and Usage for Xembify
XEMBIFY® (immune globulin subcutaneous, human- klhw) is a 20% immune globulin solution for subcutaneous injection indicated for treatment of Primary Humoral Immunodeficiency (PI) in patients 2 years of age and older. (1)
Xembify Dosage and Administration
For subcutaneous infusion only.
Before switching to XEMBIFY, obtain the patient’s serum IgG trough level to guide subsequent dose adjustments.
Dose (2.1)
-
Switching from immune globulin intravenous (human), 10% (IVIG) to XEMBIFY: calculate the dose by using a dose adjustment factor (1.37)
- Weekly: Begin XEMBIFY one week after last IVIG infusion.
- Establish initial weekly dose by converting the monthly (or every 3 weeks) IVIG dose into an equivalent weekly dose and increasing it using a dose adjustment factor (1.37).
Initial weekly = Prior IVIG dose (in grams) × 1.37
dose (grams) Number of weeks between IVIG doses
- Frequent dosing (2-7 times per week): Divide the calculated weekly dose by the desired number of times per week.
- Switching from immune globulin subcutaneous (human) treatment (IGSC): Weekly dose (grams) should be the same as the weekly dose of prior IGSC treatment (grams).
Administration (2.3)
Infusion sites: up to 6 infusion sites simultaneously, with at least 2 inches (5 cm) between sites avoiding bony prominences. Rotate sites for each administration
Dosage Forms and Strengths
XEMBIFY is a solution containing 0.2 g/mL (200 mg/mL; 20%) protein solution for subcutaneous infusion. (3)
Contraindications
- Anaphylactic or severe systemic reactions to human immunoglobulin or inactive ingredients of XEMBIFY such as polysorbate 80. (4)
- IgA deficient patients with antibodies against IgA and a history of hypersensitivity (4)
Warnings and Precautions
- Hypersensitivity and anaphylactic reactions may occur. IgA deficient patients with antibodies against IgA are at greater risk of developing severe hypersensitivity or anaphylactic reactions. (5.1)
- Aseptic Meningitis Syndrome (AMS) may occur within two days of treatment. (5.3)
- Monitor for renal function in patients at risk for renal failure. (5.4)
- Hemolysis can develop. Risk factors include high doses and non-O blood group. Closely monitor for hemolysis and hemolytic anemia. (5.5)
- Monitor patients for pulmonary adverse reactions (transfusion-related acute lung injury [TRALI]). (5.6)
- XEMBIFY is made from human plasma and may carry a risk of transmitting infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent. (5.7)
- Passive transfer of antibodies may confound serologic testing. (5.8)
Adverse Reactions/Side Effects
The most common adverse reactions in ≥ 5% of subjects in the clinical trial were local adverse reactions including infusion site erythema (redness), infusion site pain, infusion site swelling (puffiness), infusion site bruising, infusion site nodule, infusion site pruritus (itching), infusion site induration (firmness), infusion site scab, infusion site edema, and systemic reactions including cough and diarrhea. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Grifols Therapeutics LLC at 1-800-520-2807 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
(6)
Drug Interactions
The passive transfer of antibodies may transiently interfere with the response to live virus vaccines, such as measles, mumps, rubella, and varicella. (7.2)
Use In Specific Populations
Geriatric: In patients over 65 years, do not exceed the recommended dose and infuse XEMBIFY at the minimum rate practicable. (8.5)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 8/2020
Full Prescribing Information
WARNING: THROMBOSIS
- Thrombosis may occur with immune globulin products, including XEMBIFY. Risk factors may include: advanced age, prolonged immobilization, hypercoagulable conditions, history of venous or arterial thrombosis, use of estrogens, indwelling central vascular catheters, hyperviscosity, and cardiovascular risk factors. Thrombosis may occur in the absence of known risk factors. [see Warnings and Precautions (5.2), Patient Counseling Information (17)]
- For patients at risk of thrombosis, administer XEMBIFY at the minimum dose and infusion rate practicable. Ensure adequate hydration in patients before administration. Monitor for signs and symptoms of thrombosis and assess blood viscosity in patients at risk for hyperviscosity. [see Warnings and Precautions (5.2)]
1. Indications and Usage for Xembify
XEMBIFY® (immune globulin subcutaneous, human – klhw) is a 20% immune globulin solution for subcutaneous injection indicated for treatment of primary humoral immunodeficiency (PI) in patients 2 years of age and older. This includes, but is not limited to, congenital agammaglobulinemia, common variable immunodeficiency, X-linked agammaglobulinemia, Wiskott-Aldrich syndrome, and severe combined immunodeficiencies.[1-4]
2. Xembify Dosage and Administration
For subcutaneous infusion only.
Before switching to XEMBIFY, obtain the patient’s serum IgG trough level to guide subsequent dose adjustments.
2.1 Dose
Individualize the dose based on the patient’s pharmacokinetic and clinical response.
Measure the patient’s serum IgG trough level as early as 5 weeks after initiating XEMBIFY treatment to determine if a dose adjustment is needed.
Monitor the patient’s IgG trough level every 2 to 3 months to determine subsequent dose adjustments and dosing intervals as needed (Table 1).
Doses divided over the course of a week or once weekly achieve similar exposure when administered regularly at steady-state.
For frequent dosing (2-7 times per week), divide the calculated weekly dose by the desired number of times per week.
For dose adjustments, calculate the difference (in mg/dL) of the patient’s serum IgG trough level from the target IgG trough level, then find this difference in Table 1 (below). Locate the corresponding amount (in mL) by which to increase or decrease the weekly dose based on the patient’s body weight. For example, if a patient with a body weight of 70 kg has an actual IgG trough level of 900 mg/dL and the target level is 1,000 mg/dL, this results in a difference of 100 mg/dL. Therefore, increase the weekly dose of subcutaneous dose by 5 mL.
The patient’s clinical response should be the primary consideration in dose adjustment. If a patient on XEMBIFY does not maintain an adequate clinical response or a serum IgG trough level equivalent to that of a previous treatment, adjust the dose accordingly.
|
|||||||||||||
| Difference From Target IgG Trough Level (mg/dL) | Body Weight (kg) | ||||||||||||
| 10 | 15 | 20 | 30 | 40 | 50 | 60 | 70 | 80 | 90 | 100 | 110 | 120 | |
| Dose Adjustment (mL per Week)* | |||||||||||||
| 50 | 0 | 1 | 1 | 1 | 2 | 2 | 2 | 3 | 3 | 3 | 4 | 4 | 5 |
| 100 | 1 | 1 | 2 | 2 | 3 | 4 | 5 | 5 | 6 | 7 | 8 | 8 | 9 |
| 150 | 1 | 2 | 2 | 3 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 13 | 14 |
| 200 | 2 | 2 | 3 | 5 | 6 | 8 | 9 | 11 | 12 | 14 | 15 | 17 | 18 |
| 250 | 2 | 3 | 4 | 6 | 8 | 9 | 11 | 13 | 15 | 17 | 19 | 21 | 23 |
| 300 | 2 | 3 | 5 | 7 | 9 | 11 | 14 | 16 | 18 | 20 | 23 | 25 | 27 |
| 350 | 3 | 4 | 5 | 8 | 11 | 13 | 16 | 19 | 21 | 24 | 27 | 29 | 32 |
| 400 | 3 | 5 | 6 | 9 | 12 | 15 | 18 | 21 | 24 | 27 | 30 | 33 | 36 |
| 450 | 3 | 5 | 7 | 10 | 14 | 17 | 20 | 24 | 27 | 31 | 34 | 38 | 41 |
| 500 | 4 | 6 | 8 | 11 | 15 | 19 | 23 | 27 | 30 | 34 | 38 | 42 | 45 |
Switching to XEMBIFY from IVIG
Begin treatment with XEMBIFY one week after the patient’s last IVIG infusion. Calculate the initial weekly dose of XEMBIFY. Divide the previous monthly (or every 3 weeks) IVIG dose in grams by the number of weeks between IVIG infusions, then multiply this dose by the dose adjustment factor of 1.37.
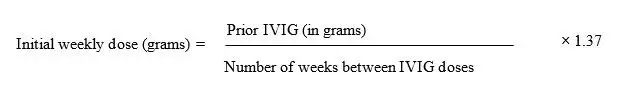
To convert the XEMBIFY dose (in grams) to milliliters (mL), multiply the calculated Initial SC dose (in grams) by 5.
Provided the total weekly dose is maintained, any dosing interval from daily up to weekly will achieve similar systemic IgG exposure when administered regularly at steady-state.
Switching to XEMBIFY from subcutaneous immune globulin (IGSC)
Administer the same weekly dose of XEMBIFY (in grams) as the weekly dose of prior IGSC treatment (in grams).
2.2 Preparation and Handling
XEMBIFY is a clear to slightly opalescent, and colorless or pale yellow solution.
Visually inspect XEMBIFY for particulate matter and discoloration prior to administration, whenever solution and container permit.
Do not use if the solution is cloudy or turbid.
Do not shake.
Do not dilute.
The XEMBIFY vial is for single use only.
Do not store any vial that has been entered by a needle during preparation for infusion, punctured, partially used, or opened.
Administer within 8 hours after beginning infusion preparation (i.e., once XEMBIFY is transferred from the vial into a syringe).
Administer XEMBIFY separately from other drugs or medications that the patient may be receiving.
Do not mix XEMBIFY with other medications including immune globulins from other manufacturers.
Do not use after expiration date.
Discard unused portion.
2.3 Administration
For subcutaneous infusion only.
Prior to use, allow the solution to reach ambient room temperature.
Do not shake.
Follow the steps below and use aseptic technique to administer XEMBIFY.
1. Inspect the vials: inspect for clarity, color, and expiration date (s).
2. Prepare for infusion:
Gather supplies: XEMBIFY vial(s), ancillary supplies, sharps container, patient’s
treatment diary/logbook, and the infusion pump.
Prepare a clean work area.
Wash hands.
3. Remove the protective cap from the vial to expose the central portion of the stopper.
If the packaging shows any sign of tampering, do not use the product and notify
Grifols Therapeutics LLC immediately [1-800-520-2807].
4. Wipe the stopper with alcohol and allow to dry.
|  |
|  |
|
|
|  |
|  |
|  |
12. Repeat priming and needle insertion steps using a new needle, administration tubing
and a new infusion site. Secure the needle in place by applying sterile gauze or
transparent dressing over the site.
13. Infuse XEMBIFY at a maximum rate of 25 mL per hour per infusion site using up to
6 infusion sites (most patients used 4 infusion sites). Ensure that the infusion sites are
at least 2 inches (5 cm) apart for patients of all ages. The number of infusion sites is
at healthcare provider discretion. Children will require less total volume for a specific
XEMBIFY dose (mg/kg body weight) than adults. The healthcare provider may
choose a smaller volume/site for children and/or fewer infusion sites to achieve the
target total dose, depending on the needs of the child. The total dose volume of
XEMBIFY is divided by the desired volume (mL/site) to obtain number of infusion
sites to be used.
| Volume to Be Infused SC | Rate | Number of Sites (most frequent is 4) | Site Distance Apart |
| 25 mL per site | ≤ 25 mL/hr/infusion site | ≤ 6 | ≥ 2 inches (5 cm) |
Record information about the infusion (e.g., lot number, expiration date, dose, date,
time, infusion site location(s), side effects) in a patient treatment record or infusion
log.
14. Discard the needle(s) and infusion line(s) in an appropriate container. Follow the
manufacturer’s instructions for storage of the infusion pump.
15. Discard partially used vial(s).
3. Dosage Forms and Strengths
XEMBIFY is a protein solution containing 20% IgG (200 mg/mL; 0.2 g/mL) for subcutaneous infusion.
4. Contraindications
XEMBIFY is contraindicated in:
Patients who have had an anaphylactic or severe systemic reaction to the administration of human immune globulin.
IgA deficient patients with antibodies against IgA and history of hypersensitivity to human immune globulin treatment.
5. Warnings and Precautions
5.1 Hypersensitivity
Severe hypersensitivity reactions may occur with human immune globulin products, including XEMBIFY. If a hypersensitivity reaction occurs, discontinue the XEMBIFY infusion immediately and institute appropriate treatment.
XEMBIFY contains IgA. Patients with known anti-IgA antibodies have a greater risk of developing potentially severe hypersensitivity and/or anaphylactic reactions. XEMBIFY is contraindicated in IgA deficient patients with antibodies against IgA and history of hypersensitivity to human immune globulin treatment. [see Contraindications (4)]
5.2 Thrombosis
Thrombosis may occur following treatment with immune globulin products, including XEMBIFY.[5-7] Risk factors may include: advanced age, prolonged immobilization, hypercoagulable conditions, history of venous or arterial thrombosis, use of estrogens, indwelling central vascular catheters, hyperviscosity, and cardiovascular risk factors. Thrombosis may occur in the absence of known risk factors.
Consider baseline assessment of blood viscosity in patients at risk for hyperviscosity, including those with cryoglobulins, fasting chylomicronemia/markedly high triacylglycerols (triglycerides), or monoclonal gammopathies. For patients at risk of thrombosis, administer XEMBIFY at the minimum dose and infusion rate practicable. Ensure adequate hydration in patients before administration. Monitor for signs and symptoms of thrombosis and assess blood viscosity in patients at risk for hyperviscosity. [see Boxed Warning, Dosage and Administration (2.3), Patient Counseling Information (17)]
5.3 Aseptic Meningitis Syndrome (AMS)
AMS has been reported with the use of human immune globulin administered intravenously and subcutaneously. It usually begins within several hours to 2 days following immune globulin treatment. AMS may occur more frequently in females than in males.
AMS is characterized by the following signs and symptoms: severe headache, nuchal rigidity, drowsiness, fever, photophobia, painful eye movements, nausea and vomiting. Cerebrospinal fluid (CSF) studies frequently show pleocytosis up to several thousand cells per cubic millimeter, predominantly from the granulocytic series, and elevated protein levels up to several hundred mg/dL, but negative culture results. To rule out other causes of meningitis, conduct a thorough neurological examination on patients exhibiting such symptoms and signs, including CSF studies. AMS may occur more frequently in association with high doses (>2 g/kg) and/or rapid infusion of immune globulin products. Discontinuation of immune globulin treatment has resulted in remission of AMS within several days without sequelae.
5.4 Renal Dysfunction/Failure
Acute renal dysfunction/failure, acute tubular necrosis, proximal tubular nephropathy, osmotic nephrosis and death may occur upon use of human immune globulin products, especially those containing sucrose.[8,9] XEMBIFY does not contain sucrose. Ensure that patients are not volume depleted prior to administration of XEMBIFY.
In patients at risk of developing renal dysfunction, including patients with any degree of preexisting renal insufficiency or predisposition to acute renal failure (such as diabetes mellitus, age greater than 65 years, volume depletion, sepsis, paraproteinemia, or patients receiving known nephrotoxic drugs), monitor renal function and consider lower, more frequent dosing. [see Dosage and Administration (2.3)]
Periodic monitoring of renal function and urine output is particularly important in patients judged to have a potential increased risk for developing acute renal failure. Assess renal function, including measurement of blood urea nitrogen (BUN)/serum creatinine, prior to the initial infusion of XEMBIFY and again at appropriate intervals thereafter. If renal function deteriorates, consider discontinuation of XEMBIFY. [see Patient Counseling Information (17)]
5.5 Hemolysis
IgG products, including XEMBIFY can contain blood group antibodies that may act as hemolysins and induce in vivo coating of red blood cells (RBCs) with immunoglobulin, causing a positive direct antiglobulin (Coombs’) test result and hemolysis.[10-13] Delayed hemolytic anemia can develop subsequent to human immune globulin therapy due to enhanced RBC sequestration, and acute hemolysis consistent with intravascular hemolysis has been reported. [see Adverse Reactions (6)]
Monitor XEMBIFY recipients for clinical signs and symptoms of hemolysis, particularly patients with risk factors such as non-O blood group, or patients receiving high IgG doses (≥ 2 grams/kg).[14] Underlying inflammatory state in an individual patient may increase the risk of hemolysis, but its role is uncertain.[15]
If signs and/or symptoms of hemolysis are present after XEMBIFY infusion, perform appropriate confirmatory laboratory testing.
5.6 Transfusion-related Acute Lung Injury (TRALI)
Noncardiogenic pulmonary edema may occur in patients following treatment with human immune globulin products.[16] TRALI is characterized by severe respiratory distress, pulmonary edema, hypoxemia, normal left ventricular function, and fever. Symptoms typically occur within 1 to 6 hours after treatment.
Monitor patients for pulmonary adverse reactions. If TRALI is suspected, perform appropriate tests for the presence of anti-neutrophil and anti-HLA antibodies in both the product and patient serum. TRALI may be managed using oxygen therapy with adequate ventilatory support.
5.7 Transmissible Infectious Agents
Because XEMBIFY is made from human blood, it may carry a risk of transmitting infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent. This also applies to unknown or emerging viruses and other pathogens. No cases of transmission of viral diseases or CJD have been associated with the use of XEMBIFY. ALL infections suspected by a physician to have possibly been transmitted by XEMBIFY should be reported by the physician or other healthcare provider to Grifols Therapeutics LLC [1-800-520-2807].
5.8 Interference with Laboratory Tests
After infusion with XEMBIFY, the transitory rise of various passively transferred antibodies in the patient’s blood may yield false-positive serological testing results, with the potential for misleading interpretation. Passive transmission of antibodies to erythrocyte antigens (e.g., A, B, and D) may cause a positive direct or indirect antiglobulin (Coombs’) test.
6. Adverse Reactions/Side Effects
The most common adverse reactions in ≥ 5% of subjects in the clinical trial were local adverse reactions including infusion site erythema (redness), infusion site pain, infusion site swelling (puffiness), infusion site bruising, infusion site nodule, infusion site pruritus (itching), infusion site induration (firmness), infusion site scab, infusion site edema, and systemic reactions including cough and diarrhea.
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of one drug cannot be directly compared to rates in other clinical trials of another drug and may not reflect the rates observed in clinical practice.
Clinical safety data are based on an open-label, single-arm prospective multi-center study of 49 subjects with primary immunodeficiency (PI) who received subcutaneous XEMBIFY for at least 6 months.
A total of 49 subjects received 1053 XEMBIFY infusions, including 14 subjects between 2 to 16 years of age during the clinical trial. The average number of infusions per subject was 21.5 infusions, median 24 infusions (range 1-26 infusions). There were a total of 390 local infusion site reactions which occurred at a rate per infusion of 0.370 (about 1 in 2.7 infusions). Of these, the most common was infusion site erythema which had a median duration of 24.9 hours. Infusion site swelling, and infusion site pain had median durations of 24.5 and 22.8 hours, respectively. Local infusion site reactions of all kinds by site of infusion (where site of infusion was recorded) occurred in 50.0% and 52.6% of patients during infusions in the abdomen versus thigh, respectively, and across 773 abdominal infusions and 279 thigh infusions rates were 0.184 and 0.735 per infusion, respectively; this corresponds to 1 in 5.4 infusions (for abdomen) and 1 in 1.4 infusions (for thigh). No local infusion site reactions were severe or serious.
The adverse reactions occurring in ≥ 5% of subjects on XEMBIFY in the clinical trial for the duration of the subcutaneous (SC) phase are depicted in the table below which includes all treatment-emergent adverse reactions except infections.
|
||
| Adverse Reaction* | By Subject n (%)† (N=49 subjects) | By Infusion n (rate)‡ (N=1053 infusions) |
| Infusion site erythema | 19 (39%) | 123 (0.117) |
| Infusion site pain | 9 (18%) | 32 (0.030) |
| Infusion site swelling | 8 (16%) | 124 (0.118) |
| Infusion site bruising | 8 (16%) | 26 (0.025) |
| Infusion site nodule | 8 (16%) | 13 (0.012) |
| Infusion site pruritus | 5 (10%) | 28 (0.027) |
| Infusion site induration | 4 (8%) | 6 (0.006) |
| Infusion site scab | 3 (6%) | 6 (0.006) |
| Infusion site edema | 3 (6%) | 5 (0.005) |
| Cough | 3 (6%) | 4 (0.004) |
| Diarrhea | 3 (6%) | 3 (0.003) |
Four subjects discontinued XEMBIFY due to adverse reactions which were infusion site nodules, infusion site discomfort, skin papules/plaques, and arthralgia/myalgia.
6.2 Postmarketing Experience
Because postmarketing reporting of adverse reactions is voluntary and from a population of uncertain size, it is not always possible to reliably estimate the frequency of these reactions or establish a causal relationship to product exposure.
The following adverse reactions have been identified and reported during the postmarketing use of immune globulin products administered subcutaneously:
Cardiac disorders: Tachycardia
Nervous system disorders: Tremor and paresthesia
Respiratory, thoracic and mediastinal disorders: Dyspnea and laryngospasm
7. Drug Interactions
7.1 Serological Testing
Various passively transferred antibodies in immunoglobulin preparations, including XEMBIFY, can confound the results of serological testing.
7.2 Live Attenuated Virus Vaccines
Passive transfer of antibodies may transiently interfere with the immune response to live virus vaccines such as measles, mumps, rubella and varicella. Inform the immunizing healthcare provider of recent therapy with XEMBIFY so that appropriate measures may be taken.
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
No human data are available to indicate the presence or absence of drug associated risk. Animal reproduction studies have not been conducted with XEMBIFY. It is not known whether XEMBIFY can cause fetal harm when administered to a pregnant woman or can affect reproduction capacity. Immune globulins cross the placenta from maternal circulation increasingly after 30 weeks of gestation. In the U.S. general population, the estimated background risk of major birth defect and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
8.2 Lactation
Risk Summary
No human data are available to indicate the presence or absence of drug associated risk. The developmental and health benefits of breastfeeding should be considered along with the mother’s clinical need for XEMBIFY and any potential adverse effects on the breastfed infant from XEMBIFY or from the underlying maternal condition.
8.4 Pediatric Use
XEMBIFY was evaluated in 14 pediatric subjects with PI (2-16 years of age) in a multi-center clinical trial. The safety and efficacy profiles were similar to adult subjects. No pediatric-specific dose requirements were necessary to achieve the desired serum IgG levels.
8.5 Geriatric Use
Clinical studies of XEMBIFY did not include sufficient numbers of subjects over age 65 years to determine whether they respond differently from younger subjects. Three study subjects enrolled in the clinical trial were 65 years and older. In general, dose selection for an elderly patient should be cautious, usually starting at the low end of the dosing range, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
11. Xembify Description
XEMBIFY, immune globulin subcutaneous, human-klhw, is a 20% ready-to-use sterile, non-pyrogenic solution of human immune globulin protein for subcutaneous administration. The purity is ≥ 98% IgG with a sub-class distribution similar to that found in normal serum.
XEMBIFY consists of 18% to 22% protein in 0.16 M to 0.26 M glycine and 10 to 40 mcg/mL polysorbate 80 at a pH of 4.1 to 4.8. The solution is clear to slightly opalescent, and colorless or pale yellow. The osmolality range is 280 to 404 mOsmol/kg. XEMBIFY contains no preservative and is not made with natural rubber latex.
XEMBIFY is made from large pools of human plasma by a combination of cold ethanol fractionation, caprylate precipitation and filtration, and anion-exchange chromatography. Isotonicity is achieved by the addition of glycine. XEMBIFY is incubated in the final container (at the low pH of 4.1 to 4.8).
The capacity of the manufacturing process to remove and/or inactivate enveloped and non-enveloped viruses has been validated by laboratory spiking studies on a scaled down process model, using the following enveloped and non-enveloped viruses: human immunodeficiency virus, type I (HIV-1) as the relevant virus for HIV-1 and HIV-2; bovine viral diarrhea virus (BVDV) as a model for hepatitis C virus; pseudorabies virus (PRV) as a model for large enveloped DNA viruses (e.g. herpes viruses); West Nile Virus (WNV) as a relevant virus; Reovirus type 3 (Reo) as a model for non-enveloped viruses and for its resistance to physical and chemical inactivation; hepatitis A virus (HAV) as relevant non-enveloped virus, and porcine parvovirus (PPV) as a model for human parvovirus B19.
Overall virus clearance capacity was calculated only from steps that were mechanistically independent from each other and truly additive. In addition, each step was verified to provide robust virus reduction across the production range for key parameters.
| Process Step | Enveloped Virus | Non-Enveloped Virus | |||||
| HIV-1 | BVDV | PRV | WNV | Reo3 | HAV | PPV | |
|
|||||||
| Caprylate Precipitation/Depth Filtration | C/I*. | 2.7 | C/I* | C/I* | ≥3.5 | ≥3.6 | 4.0 |
| Caprylate Incubation† | ≥4.5 | ≥4.5 | ≥4.6 | ≥5.1 | NA‡ | NA‡ | NA‡ |
| Column Chromatography | ≥3.0 | 4.0 | ≥3.3 | ND§ | ≥4.0 | ≥1.4 | 4.2 |
| Nanofiltration | ≥3.7 | ≥4.1 | ND§ | ND§ | ≥1.8 | ND§ | 0.5 |
| Low pH Final Container Incubation | ≥5.3 | 4.9 | ≥5.1 | ≥5.3 | NA‡ | NA‡ | NA‡ |
| Overall Clearance Capacity | ≥16.5 | ≥20.2 | ≥13.0 | ≥10.4 | ≥9.3 | ≥5.0 | 8.2 |
Additionally, the manufacturing process was investigated for its capacity to decrease the infectivity of an experimental agent of transmissible spongiform encephalopathy (TSE), considered as a model for the variant Creutzfeldt-Jakob disease (vCJD), and Creutzfeldt-Jakob disease (CJD) agents.
Several of the individual production steps of the manufacturing process have been shown to decrease TSE infectivity of an experimental model agent. TSE reduction steps include depth filtrations (a total of ≥ 6.6 log10). These studies provide reasonable assurance that low levels of vCJD/CJD agent infectivity, if present in the starting material, would be removed.
12. Xembify - Clinical Pharmacology
12.1 Mechanism of Action
XEMBIFY supplies a broad spectrum of opsonizing and neutralizing immunoglobulin G (IgG) antibodies against bacterial, viral, parasitic, and mycoplasmal agents and their toxins. XEMBIFY also contains a spectrum of antibodies capable of interacting with and altering the activity of cells of the immune system. The role of these antibodies and the mechanism of action of XEMBIFY are not fully understood.
12.2 Pharmacodynamics
Human normal immunoglobulin contains mainly (IgG) with a broad spectrum of antibodies against infectious agents. Human normal immunoglobulin contains the IgG antibodies present in the normal population. XEMBIFY has a distribution of IgG subclasses closely proportional to that in native human plasma. Adequate doses of XEMBIFY may restore abnormally low IgG levels to the normal range.
12.3 Pharmacokinetics
Pharmacokinetic (PK) parameters of subcutaneously administered XEMBIFY were evaluated in subjects with primary immunodeficiency (PI) during a clinical trial. [see Clinical Studies (14)] Subjects were treated intravenously with a comparator product [GAMUNEX®-C, immune globulin injection (human), 10% caprylate/chromatography purified] during a 3-4 months run-in period prior to IV PK profiling in 50 subjects, and then 49 subjects switched to weekly subcutaneous infusions of XEMBIFY for 24 weeks at 137% of the intravenous dose with PK profiling at SC Week #13-14. A comparison of the area under the curve (AUC) for subcutaneous versus intravenous infusion was performed.
At this dose adjustment, the geometric least-squares means ratio of the AUC for subcutaneous XEMBIFY versus IV administration of GAMUNEX-C was 104% (90% CI: 100%-107%). The peak IgG level occurred at a mean of 76 hours after subcutaneous XEMBIFY administration. The average mean IgG trough level at steady state was higher with XEMBIFY (1245 mg/dL) compared with IV GAMUNEX-C (957 mg/dL) (average mean trough ratio SC/IV of 1.3). PK parameters of XEMBIFY are summarized in Table 4. PK parameters did not significantly differ between age groups (Table 5).
|
||||
| Phase | Statistics | AUC(0-7 days)
(h*mg/mL)* | Cmax (mg/mL) | tmax (hour) |
| IV | n | 49 | 49 | 49 |
| Mean±SD | 2122±418 | 22±4 | 5.814 | |
| CV% | 20 | 20 | ||
| SC | n | 39 | 41 | 41 |
| Mean±SD | 2183±481 | 14±3 | 76±36 | |
| CV% | 22 | 22 | 47 | |
| Min, Max | 1027, 3675 | 6, 23 | 0, 168† | |
| Age Group (years) Statistics | AUC(0-7 days)
(h*mg/mL) | Cmax (mg/mL) | Mean Trough (mg/mL) | tmax (hour) |
|
||||
| 2 -5 (n) | 1 | 1 | 1 | 1 |
| Mean±SD | 1839±NC* | 11±NC* | 11± NC* | 72±NC* |
| >5 -12 (n) | 5 | 5 | 6 | 5 |
| Mean±SD | 2156±276 | 14±2 | 12±2 | 71±26 |
| CV% | 13 | 13 | 15.3 | 37.16 |
| Min, Max | 1878, 2456 | 12, 16 | 10, 15 | 28.2, 100.8 |
| >12 -16 (n) | 4 | 5 | 5 | 5 |
| Mean±SD | 2400±406 | 15±3 | 14±2 | 73±50 |
| CV% | 17 | 18 | 15.2 | 68.44 |
| Min, Max | 2056, 2987 | 13, 20 | 11, 17 | 23.7, 143.1 |
| >16 (n) | 29 | 30 | 32 | 30 |
| Mean±SD | 2170±524 | 14±3 | 12±3 | 78±36 |
| CV% | 24 | 24 | 23.9 | 46.66 |
| Min, Max | 1027, 3675 | 6, 23 | 7, 20 | 0.00, 167.7 |
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No nonclinical studies were conducted to evaluate the carcinogenic or mutagenic effects of XEMBIFY or its effects on fertility.
13.2 Animal Toxicology and/or Pharmacology
Single and repeated dose toxicology studies were conducted in male New Zealand White rabbits. In a single-dose toxicity study, no adverse effects were observed with subcutaneous dose levels of 500, 1000 and 1500 mg/kg. In a repeated-dose toxicity study, the systemic safety and toxicity profiles of XEMBIFY and comparator GAMUNEX-C were similar following 5 consecutive daily subcutaneous doses at levels of 500, 1000 and 1500 mg/kg/day. Transient local injection site swelling was observed in XEMBIFY but not in the GAMUNEX-C groups.
In improper delivery route studies, XEMBIFY administered as a single intravenous, intra-arterial or perivascular dose of 100 mg/kg caused injection site irritation in New Zealand White rabbits. The findings were of higher incidence following perivascular administration of either XEMBIFY or GAMUNEX-C, and were within the norms of this route of administration in this species.
14. Clinical Studies
Study 1 was a prospective, open-label single-arm, multi-center clinical trial designed to evaluate pharmacokinetics and safety of XEMBIFY as compared to GAMUNEX-C. Efficacy was based on annualized serious bacterial infection (SBI) rate during the 6 months on XEMBIFY. The GAMUNEX-C run-in phase prior to XEMBIFY (subcutaneous phase) lasted 3 or 4 months to achieve steady state prior to pharmacokinetic profiling. The definition of SBI was either bacteremia/sepsis, bacterial meningitis, bacterial pneumonia, osteomyelitis/septic arthritis, or visceral abscess.
This clinical trial determined the safety and pharmacokinetics of XEMBIFY in 53 adult and pediatric subjects with PI (9.4% Hispanic or Latino; 90.6% White, 3.8% Black or African American, 5.7% American Indian or Alaskan Native). During the run-in and IV GAMUNEX-C phases 4 subjects discontinued (1 lost to follow-up, 2 withdrawal by subject, 1 adverse event). XEMBIFY was administered to a total of 49 subjects (14 children aged 2 to ≤ 16 years and 35 adults) with a mean ± SD dose of 179 ± 45 mg/kg/week for a median treatment duration of 24 weeks and mean ± SD of 21.6 ± 6.5 weeks. The median dose was 171 mg/kg/week and the range of doses was 71 mg/kg/week to 276 mg/kg/week. The total exposure of XEMBIFY was 20.28 subject-years and 1053 infusions.
Study 2 is an ongoing study in which XEMBIFY is being administered for 1 year and is being conducted in the European Union and Australia. A total of 61 subjects including 29 children were enrolled. The interim safety data in adult and pediatric study subjects appear consistent with the safety results of the clinical trial in Study 1.
The rate of serious bacterial infections (SBIs) which was an exploratory endpoint in Study 1, was 0.05 events per subject-year (1 event in 20 subject-years) (upper 99% confidence limit: 0.11) during XEMBIFY treatment. This annual rate was lower than 1.0 SBI/subject-year, the threshold specified as effective.
The summary of infections and associated events for subjects during subcutaneous treatment with XEMBIFY is summarized in Table 6.
|
|
| Parameters | Results |
| Number of Subjects (efficacy period) | 49 |
| Total number of subject days on treatment | 7,407 |
| Total number of subject-years on treatment | 20.28 |
| Infections
Annual rate of SBIs* (per subject-year) | 0.05 (95% CI: 0.02 - 0.10) |
| Annual rate of infections of any kind (per subject-year) | 2.4 (95% CI: 1.6 - 3.3) |
| Days on antibiotics (prophylactic) (rate per subject-year) | 27.7 (95% CI: 13.6 - 49.0) |
| Days on antibiotics (therapeutic) (rate per subject-year) | 28.9 (95% CI: 17.3 - 44.8) |
| Days missed work/school/unable to perform normal daily activities due to infections (rate per subject-year) | 2.3 (95% CI: 1.1 - 4.2) |
| Hospitalizations due to infections (rate per subject-year) | 0.05 (95% CI: 0.02 - 0.10) |
15. References
- Buckley RH, Schiff RI. The use of intravenous immune globulin in immunodeficiency diseases. N Engl J Med 1991;325(2):110-7.
- Cunningham-Rundles C, Bodian C. Common variable immunodeficiency: clinical and immunological features of 248 patients. Clin Immunol 1999;92(1):34-48.
- Pruzanski W, Sussman G, Dorian W, et al. Relationship of the dose of intravenous gammaglobulin to the prevention of infections in adults with common variable immunodeficiency. Inflammation 1996;20(4):353-9.
- Stephan JL, Vlekova V, Le Deist F, et al. Severe combined immunodeficiency: a retrospective single-center study of clinical presentation and outcome in 117 patients. J Pediatr 1993;123(4):564-72.
- Dalakas MC. High-dose intravenous immunoglobulin and serum viscosity: risk of precipitating thromboembolic events. Neurology 1994;44:223-6.
- Woodruff RK, Grigg AP, Firkin FC, et al. Fatal thrombotic events during treatment of autoimmune thrombocytopenia with intravenous immunoglobulin in elderly patients. Lancet 1986;2:217-8.
- Wolberg AS, Kon RH, Monroe DM, et al. Coagulation factor XI is a contaminant in intravenous immunoglobulin preparations. Am J Hematol 2000;65:30-4.
- Cayco AV, Perazella MA, Hayslett JP. Renal insufficiency after intravenous immune globulin therapy: a report of two cases and an analysis of the literature. J Am Soc Nephrol 1997;8(11):1788-94.
- Pierce LR, Jain N. Risks associated with the use of intravenous immunoglobulin. Trans Med Rev 2003;17:241-51.
- Copelan EA, Strohm PL, Kennedy MS, et al. Hemolysis following intravenous immune globulin therapy. Transfusion 1986;26:410-2.
- Thomas MJ, Misbah SA, Chapel HM, et al. Hemolysis after high-dose intravenous Ig. Blood 1993;15:3789.
- Wilson JR, Bhoopalam N, Fisher M. Hemolytic anemia associated with intravenous immunoglobulin. Muscle & Nerve 1997;20:1142-5.
- Kessary-Shoham H, Levy Y, Shoenfeld Y, et al. In vivo administration of intravenous immunoglobulin (IVIg) can lead to enhanced erythrocyte sequestration. J Autoimmun 1999;13:129-35.
- Kahwaji J, Barker E, Pepkowitz S, et al. Acute hemolysis after high-dose intravenous immunoglobulin therapy in highly HLA sensitized patients. Clin J Am Soc Nephrol 2009;4:1993-7.
- Daw Z, Padmore R, Neurath D, et al. Hemolytic transfusion reactions after administration of intravenous immune (gamma) globulin: A case series analysis. Transfusion 2008;48:1598-601.
- Rizk A, Gorson KC, Kenney L, et al. Transfusion-related acute lung injury after the infusion of IVIG. Transfusion 2001;41:264-8.
16. How is Xembify supplied
XEMBIFY is supplied in 1, 2, 4, and 10 gram single use vials.
| Package NDC Number | Container NDC Number | Size | Gram Protein |
| 13533-810-05 | 13533-810-06 | 5 ml | 1 |
| 13533-810-10 | 13533-810-11 | 10 ml | 2 |
| 13533-810-20 | 13533-810-21 | 20 ml | 4 |
| 13533-810-50 | 13533-810-51 | 50 ml | 10 |
Components used in the packaging are not made with natural rubber latex and contains no preservative.
Store XEMBIFY at 2–8°C (36–46°F).
Note: XEMBIFY may be stored at temperatures not to exceed 25°C (77°F) for up to 6
months any time prior to the expiration date. Following 25°C (77°F) storage, use the
product immediately or discard.
Do not freeze.
Do not use solutions that have been frozen.
Do not use after expiration date.
Discard unused portion.
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Information for Patients).
Ask about a history of IgA deficiency, and hypersensitivity reactions to immune globulin treatment. [see Warnings and Precautions (5.1)]
Inform patients to immediately report the following signs and symptoms to their healthcare provider: [see Boxed Warning and Warnings and Precautions]
Hypersensitivity reaction including hives, generalized urticaria, tightness of the chest,
wheezing, low blood pressure, and anaphylaxis [see Warnings and Precautions (5.1)]
Symptoms of thrombosis which may include: pain and/or swelling of an arm or leg with
warmth over the affected area, discoloration of an arm or leg, unexplained shortness of
breath, chest pain or discomfort that worsens on deep breathing, unexplained rapid pulse,
numbness or weakness on one side of the body [see Warnings and Precautions (5.2)]
Severe headache, neck stiffness, drowsiness, fever, sensitivity to light, painful eye
movements, nausea, and vomiting [see Warnings and Precautions (5.3)]
Decreased urine output, sudden weight gain, fluid retention/edema, and/or shortness of
breath [see Warnings and Precautions (5.4)]
Increased heart rate, fatigue, yellowing of the skin or eyes, and dark-colored urine [see
Warnings and Precautions (5.5)]
Trouble breathing, chest pain, blue lips or extremities, and fever [see
Warnings and Precautions (5.6)]
Inform patients/caregivers that because XEMBIFY is made from human blood, it may carry a risk of transmitting infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent. [see Warnings and Precautions (5.7)]
Inform patients that XEMBIFY can interfere with their immune response to live virus vaccines such as measles, mumps, rubella, and varicella. Inform patients to notify their healthcare provider of this potential interaction when they are receiving vaccinations. [see Drug Interactions (7.2)]
Self-administration
Advise the patient to read the FDA-approved patient labeling (Information for Patients).
If self-administration is deemed appropriate by the healthcare provider, provide clear instructions and training on subcutaneous infusion to the patient/caregiver, and document demonstration of their ability to independently administer subcutaneous infusions.
Ensure the patient/caregiver understands the importance of consistent subcutaneous infusions to maintain appropriate steady IgG levels.
Tell the patient/caregiver to start the infusion promptly after withdrawing XEMBIFY into the syringe. Ensure the patient/caregiver understands that administration should be completed within 2 hours to avoid the potential formation of particles caused by siliconized syringes.
Instruct patient to rotate infusion sites for subsequent infusions.
Instruct the patient/caregiver to keep a treatment diary/log book. This diary/log book should include information about each infusion such as, the time, date, dose, lot number(s), infusion sites, and any reactions.
Inform the patient that mild to moderate local infusion site reactions (e.g., pain, redness and itching) are a common side effect of subcutaneous treatment, but to contact their healthcare provider if a local reaction increases in severity or persists for more than a few days.
Instruct patient to return to the healthcare facility for evaluation at regular intervals so IgG levels can be checked in order to ensure IgG trough levels are adequate.
Manufactured by:
Grifols Therapeutics LLC
Research Triangle Park, NC 27709 USA
U.S. License No. 1871
3056462
INFORMATION FOR PATIENTS
XEMBIFY®
(immune globulin subcutaneous, human-klhw) 20% solution
The following summarizes important information about XEMBIFY (zem-ba-fi). Please read this information carefully before using this medicine. This patient information does not take the place of talking with your healthcare provider about your medical condition or your treatment, and it does not include all of the important information about XEMBIFY. If you have any questions after reading this, contact your healthcare provider.
What is XEMBIFY?
XEMBIFY is a ready-to-use, liquid medicine that contains immunoglobulin G (IgG) antibodies, which protect the body against infection. XEMBIFY is used to treat patients with primary immunodeficiency disease (PI).
There are many forms of PI. The most common types of PI result in an inability to make a very important type of protein called antibodies, which help the body fight off infections from bacteria or viruses. XEMBIFY is made from human plasma that is donated by healthy people. It contains antibodies collected from these healthy people that replace the missing antibodies in PI patients.
Who should NOT use XEMBIFY?
Do not use XEMBIFY if you have a known history of severe allergic reaction to immune globulin (human) or other blood products. If you have such a history, discuss this with your healthcare provider to determine if XEMBIFY is right for you.
Tell your healthcare provider if you have or ever had:
- a serious reaction to other medicines that contain immune globulin.
- an immunoglobulin A (IgA) deficiency.
- a history of heart or blood vessel disease.
- blood clots or “thick blood”.
- inability to move for some time.
How should I take XEMBIFY?
XEMBIFY is given under the skin (subcutaneously). Most of the time, infusions under the skin are given at home by self-infusion or by infusion with a caregiver’s help. Self-infusion is different from giving yourself a shot.
Instructions for taking XEMBIFY are at the end of this patient information. [see "Instructions for Use"] Only use XEMBIFY by yourself after you have been instructed by your healthcare provider.
What should I tell my healthcare provider before using XEMBIFY?
Tell your healthcare provider if you have had a serious reaction to other medicines that contain immune globulin. Also tell your healthcare provider if you have an immunoglobulin A (IgA) deficiency.
XEMBIFY can make certain types of vaccines (like measles/mumps/rubella or chickenpox) not work as well for you. Before you get a vaccine, tell the healthcare provider that you are taking XEMBIFY.
Tell your healthcare provider if you are pregnant or plan to become pregnant, or if you are nursing.
What are possible or reasonably likely side effects of XEMBIFY?
The most common side effects with XEMBIFY are:
Infusion site reactions, including but not limited to
infusion site erythema (redness)
infusion site pain
infusion site swelling (puffiness)
infusion site bruising
infusion site nodule
infusion site pruritus (itching)
infusion site induration (firmness)
infusion site scab
infusion site edema
Cough
Diarrhea
If any of the following problems occur after starting treatment with XEMBIFY, stop the infusion immediately and contact your healthcare provider or call emergency services. These could be signs of a serious problem.
Hives, swelling in the mouth or throat, itching, trouble breathing, wheezing, fainting or dizziness.
These could be signs of a serious allergic reaction.
Bad headache with nausea, vomiting, stiff neck, fever, and sensitivity to light.
These could be signs of irritation of the lining around your brain.
Reduced urination, sudden weight gain, or swelling in your legs. These could be signs of a kidney problem.
Pain, swelling, warmth, redness, or a lump in your legs or arms. These could be signs of a blood clot.
Brown or red urine, fast heart rate, yellow skin or eyes. These could be signs of a liver problem or a blood problem.
Chest pain or trouble breathing, or blue lips or extremities. These could be signs of a serious heart or lung problem.
Severe headache, stiff neck, fatigue, fever, sensitivity to light, painful eye movements, nausea and vomiting.
These could be signs of a type of brain inflammation called aseptic meningitis.
Fever over 100°F (37.8oC). This could be a sign of an infection.
Tell your healthcare provider about any side effects that concern you. You can ask your healthcare provider to give you the full prescribing information available to healthcare providers. You are encouraged to report side effects to Grifols Therapeutics LLC [1-800-520-2807].
How do I store XEMBIFY?
XEMBIFY comes in single use vials.
- Keep XEMBIFY refrigerated. Do not freeze.
- If needed, you can store XEMBIFY at room temperature for up to 6 months, but you must use it within that time or you must throw it away.
- Do not return XEMBIFY to the refrigerator if it was warmed to room temperature.
- Check the expiration date on the carton and vial label.
- Do not use XEMBIFY after the expiration date.
What else should I know about XEMBIFY?
Do not use XEMBIFY for a medical condition for which it was not prescribed. Do not share XEMBIFY with other people, even if they have the same diagnosis and symptoms that you have.
INSTRUCTIONS FOR USE
Infuse XEMBIFY only after you have been trained by your healthcare provider. Below are step-by-step instructions to help you remember how to use XEMBIFY. Ask your healthcare provider about any instructions you do not understand.
Before Using XEMBIFY
Prior to use, allow the solution to come to room temperature (68-77°F or 20-25°C). This can take 60 minutes or longer.
Do not apply heat or place in the microwave.
Step 1: Assemble supplies
Gather the XEMBIFY vial(s), ancillary supplies, sharps container, patient’s treatment diary/logbook, and the infusion pump.
Step 2: Clean surface
Set up your infusion area on a clean, flat, non-porous surface, such as a kitchen counter.
Avoid using porous surfaces such as wood. Clean the surface with an alcohol wipe using a circular motion from the center outward.
Step 3: Wash hands
Wash and dry your hands thoroughly before using XEMBIFY.
Your healthcare provider may recommend that you use antibacterial soap or that you wear gloves.

Step 4: Check vials
The liquid in the vial should be clear to slightly opalescent, and colorless or pale yellow.
Do not use the vial if:
- the solution is cloudy or discolored. The solution should be clear to slightly opalescent, and colorless or pale yellow.
- the protective cap is missing, or there is any evidence of tampering. Tell your healthcare provider immediately.
- the expiration date has passed.
Step 5: Remove the protective cap
Remove the protective cap from the vial to expose the middle of the stopper.
Wipe the stopper with alcohol and allow to dry.

Step 6: Transfer XEMBIFY from vial(s) to syringe
Do not allow your fingers or other objects to touch the inner stem of the plunger, the syringe tip, or other areas that can touch the XEMBIFY solution. Make sure needles are capped until used and that needles and syringes stay on the clean area created in Step 2. This is called “aseptic technique” to prevent germs from getting into the XEMBIFY.
Using aseptic technique, attach each needle to the syringe tip.

Step 7: Prepare the syringe and draw XEMBIFY solution into syringe
Remove cap from needle.
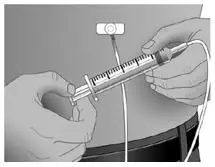
Pull the syringe plunger back to the level matching the amount of XEMBIFY to be withdrawn from the vial.
Place the XEMBIFY vial on a clean flat surface and insert the needle into the center of the vial stopper.
Inject air into the vial. The amount of air should match the amount of XEMBIFY to be withdrawn.
Turn the vial upside down and withdraw the correct amount of XEMBIFY. If multiple vials are required to get the correct dose, repeat Step 4.

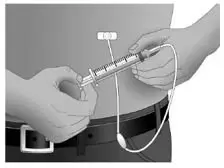
Step 8: Fill the pump reservoir and prepare the infusion pump
Follow the pump manufacturer’s instructions for filling the pump reservoir and preparing the infusion pump, administration tubing and Y-site connection tubing, if needed.
Prime the administration tubing with XEMBIFY to take out any air left in the tubing or needle. To prime, hold the syringe in one hand and the administration tubing’s capped needle in the other. Gently squeeze on the plunger until you see a drop of XEMBIFY come out of the needle.
Step 9: Select the number and location of infusion sites
Select one or more infusion sites as directed by your healthcare provider. The number and location of injection sites depends on the volume of the total dose.
Avoid: bony areas, visible blood vessels, scars, and any areas of inflammation (irritation) or infection.
Rotate sites between future infusions.
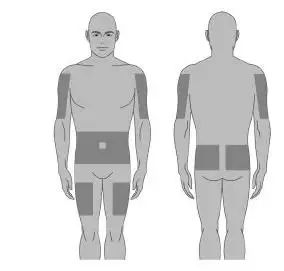
Step 10: Prepare the infusion site
Wipe the infusion site(s) with a sterile alcohol wipe beginning at the center of each infusion site and moving outward in circular motion. Allow the infusion site(s) to dry (at least 30 seconds).
Before infusion, sites should be clean, dry, and at least 2 inches (5cm) apart.
Step 11: Insert the needle
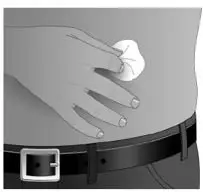
Grasp the skin between two fingers (pinch at least 1 inch (2.5 cm) of skin) and insert the needle at a 90-degree angle into the tissue underneath the skin or subcutaneous tissue.
Step 12: Make sure the needle is not in a blood vessel
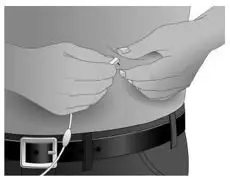
After inserting each needle into tissue (and before your infusion), make sure that a blood vessel has not been accidentally entered. To do this, attach a sterile syringe to the end of the primed administration tubing. Pull back on the syringe plunger and watch for any blood flowing back into administration tubing.
If you see any blood, remove and discard the needle and administration tubing.
Repeat priming and needle insertion steps using a new needle, administration tubing and a new infusion site.
Secure the needle in place by applying sterile gauze or transparent dressing over the site.
Step 13: Repeat for other sites, as needed
Step 14: Infuse XEMBIFY
Infuse XEMBIFY as soon as possible after it is prepared.
Follow the pump manufacturer’s instructions for filling the tubing and using the infusion pump.
Step 15: After infusion
Follow manufacturer’s instructions to turn off pump.
Undo and discard any dressing or tape.
Gently remove the inserted needle(s) or catheter(s).
Discard any unused solution in an appropriate waste container as instructed.
Discard any used administration equipment in an appropriate waste container.
Store your supplies in a safe place.
Follow manufacturer’s instructions to care for the infusion pump.
Step 16: Record each infusion
Remove the peel-off label with the product lot number from the XEMBIFY vial and use this to complete the patient record. Include information about each infusion such as: the time, date, dose, lot number(s), infusion sites, and any reactions.
Remember to bring your journal with you when you visit your healthcare provider. Your healthcare provider may ask to see your treatment diary/logbook.
Tell your healthcare provider about any problems you have during your infusions. Call your healthcare provider for medical advice about side effects. You can also report side effects to FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Manufactured by:
Grifols Therapeutics LLC
Research Triangle Park, NC 27709 USA
U.S. License No. 1871
3056462
Revised 8/2020
PACKAGE LABEL
NDC 13533-810-50
10 g / 50 mL
Immune Globulin
Subcutaneous,
Human - klhw, 20%
Xembify®
Solution for Subcutaneous Administration
Rx only
GRIFOLS
Contents:
One vial of Xembify®
No preservative
Sterile, Non-pyrogenic
Xembify® may be stored at 2–8°C (36–
46°F), AND product may be stored at
temperatures not to exceed 25°C (77°F)
for up to 6 months anytime prior to the
expiration date, after which the product
must be immediately used or discarded.
Do not freeze.
Date removed from refrigeration:
GRIFOLS
Refer to package insert for dosage
and administration.
Single Use Vial
Do not use if turbid.
Discard unused portion. Do not store
after entry into vial.
Each milliliter (mL) contains approxi-
mately 200 mg of protein, not less
than 98% of which is gamma
globulin, and approximately 15 mg
glycine and 25 mcg polysorbate 80.
Do not use the product if it shows
any signs of tampering and notify
Grifols Therapeutics LLC immediately.
Grifols Therapeutics LLC
Research Triangle Park,
NC 27709 USA
U.S. License No. 1871
GRIFOLS
GRIFOLS
GTIN (01)00313533810504
LOT XXXXXXXXXX
EXP DDMMMYYYY
SN XXXXXXXXXXXXXXXX
Immune Globulin
Subcutaneous,
Human – klhw, 20%
Xembify®
Carton: 3057222

NDC 13533-810-51
10 g / 50 mL
Immune Globulin
Subcutaneous,
Human - klhw, 20%
Xembify®
Solution for
subcutaneous administration
Rx Only
GRIFOLS
Refer to package insert for dosage and administration and compatibility
with other solutions.
Xembify® may be stored at 2–8°C (36–46°F), AND product may be stored at
temperatures not to exceed 25°C (77°F) for up to 6 months anytime prior to
the expiration date, after which the product must be immediately used or
discarded.
Single Use Vial, Discard unused portion
Do not use if turbid.
Grifols Therapeutics LLC
Research Triangle Park, NC 27709 USA
U.S. License No. 1871
Xembify® 10 g Protein in 50 mL PULL
Lot
3057120
Lot
Exp.

| XEMBIFY
immune globulin subcutaneous, human-klhw solution |
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||
| Labeler - GRIFOLS USA, LLC (048987452) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| GRIFOLS THERAPEUTICS LLC | 611019113 | manufacture(13533-810) | |




