Note: This document contains side effect information about onasemnogene abeparvovec. Some dosage forms listed on this page may not apply to the brand name Zolgensma.
Applies to onasemnogene abeparvovec: intravenous suspension.
Warning
Intravenous route (Suspension)
Serious Liver Injury and Acute Liver Failure: Cases of acute liver failure with fatal outcomes have been reported. Acute serious liver injury and elevated aminotransferases can also occur with onasemnogene abeparvovec-xioi.Patients with preexisting liver impairment may be at higher risk.Prior to infusion, assess liver function of all patients by clinical examination and laboratory testing (eg, hepatic aminotransferases [aspartate aminotransferase (AST) and alanine aminotransferase (ALT)], total bilirubin, and prothrombin time). Administer systemic corticosteroid to all patients before and after onasemnogene abeparvovec-xioi infusion. Continue to monitor liver function for at least 3 months after infusion, and at other times as clinically indicated.
Serious side effects of Zolgensma
Along with its needed effects, onasemnogene abeparvovec (the active ingredient contained in Zolgensma) may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor or nurse immediately if any of the following side effects occur while taking onasemnogene abeparvovec:
More common
- Clay-colored stools
- dark urine
- decreased appetite
- fever
- headache
- itching, skin rash
- light-colored stools
- loss of appetite
- nausea
- stomach pain or tenderness
- swelling of the feet or lower legs
- unusual tiredness or weakness
- vomiting
- yellow eyes or skin
Incidence not known
- Back pain
- black, tarry stools
- bleeding gums
- blood in the urine or stools
- blurred vision
- confusion
- decreased urine output
- dizziness
- dizziness, faintness, or lightheadedness when getting up suddenly from a lying or sitting position
- drowsiness
- pinpoint red spots on the skin
- seizures
- sudden weakness in the arms or legs
- sudden, severe chest pain
- sweating
- unusual bleeding or bruising
For Healthcare Professionals
Applies to onasemnogene abeparvovec: intravenous kit.
General
The most commonly reported adverse reactions have included elevated aminotransferases and vomiting.[Ref]
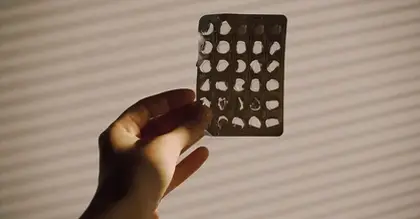
Hematologic
During clinical trials, transient decreases in platelet counts, some meeting the criteria for thrombocytopenia, have been reported.
Common (1% to 10%): Thrombocytopenia
Frequency not reported: Transient decreases in platelet count
Postmarketing reports: Thrombotic microangiopathy
Respiratory
Common (1% to 10%): Respiratory insufficiency[Ref]
One patient presented with respiratory insufficiency 12 days after receiving this drug. The patient was found to have respiratory syncytial virus (RSV) and parainfluenza in respiratory secretions; episodes of hypotension were followed by seizures. Approximately 30 days following the infusion, leukoencephalopathy was found and the patient died after withdrawal of life support, 52 days after this drug was infused.[Ref]
Cardiovascular
Common (1% to 10%): Elevated troponin-I levels[Ref]
Elevated cardiac troponin-I levels up to 0.176 mcg/L have been observed following infusion. The clinical importance of this finding is unknown; however, cardiac toxicity has been observed in animal studies.[Ref]
Gastrointestinal
Common (1% to 10%): Vomiting
Hepatic
Elevated aminotransferases (ALT and/or AST) to greater than the upper limit of normal (ULN) occurred in 12 of 44 patients in clinical trials. Two patients had AST and ALT elevations of up to 48 x ULN; these patients were otherwise asymptomatic with normal total bilirubin. Following corticosteroid management, these abnormalities resolved. One patient with preexisting transaminase elevations (who received this drug with the recommended corticosteroid regimen) became jaundiced about 7 weeks after the infusion. Laboratory testing showed an AST level approximately 80 x ULN and ALT level approximately 45 x ULN. Liver biopsy showed acute massive degeneration of hepatocytes, and massive mixed inflammatory infiltrate (primarily CD8-positive T-lymphocytes). Following treatment with corticosteroids, the patient recovered to baseline.[Ref]
Very common (10% or more): Elevated aminotransferases (27.3%)[Ref]
Other
Common (1% to 10%): Pyrexia