- Age-related macular degeneration (AMD) is a common eye condition in older adults that can affect central vision.
- Geographic atrophy is an advanced form of AMD that causes permanent vision changes.
- There is currently no cure for AMD or geographic atrophy.
- A new study shows how a wireless retinal implant may help restore central vision in people with geographic atrophy.
Researchers estimate that about
Of the people who have AMD, about 8 million globally have an advanced form of AMD called geographic atrophy. With geographic atrophy, the cells of the eye’s retina become damaged and begin to die, leading to irreversible vision loss.
While there are medications available to help slow down disease progression, there is currently no cure for AMD or geographic atrophy. People with geographic apathy learn to use and depend on low vision aids like magnifiers and special eyeglasses to help them read, identify faces, and complete everyday tasks.
Now, a new study recently published in the New England Journal of Medicine shows how a wireless retinal implant may help restore central vision in people with geographic atrophy.
For this study, researchers recruited 38 people with geographic atrophy to receive the new PRIMA implant, which had been developed by Daniel Palanker, PhD, a professor of ophthalmology at Stanford University.
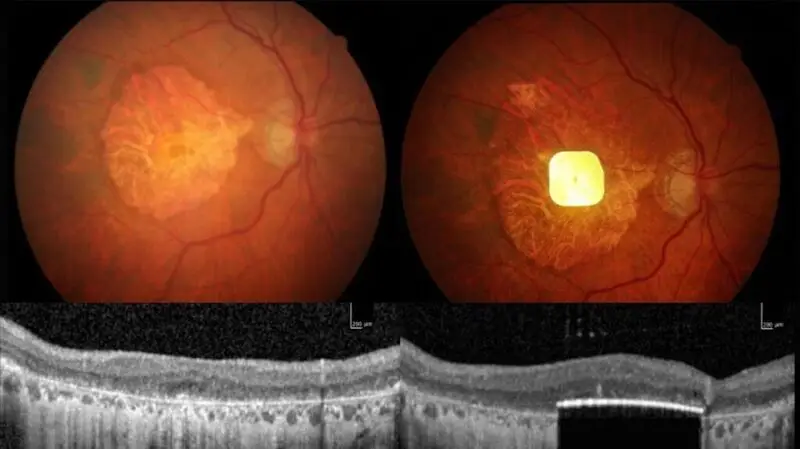
The PRIMA insert had been tested in a first-in-human trial, with its results published in August 2020, showing four of five people given the PRIMA insert showed a partial, but substantial return of their central vision in the eye given the implant.
The PRIMA system consists of a very small wireless chip that is implanted into the back of the eye, and a special pair of glasses. The chip transmits images to the glasses, allowing the person wearing them to see in real time.
The retinal implant is photovoltaic, which means it uses natural light to power itself.
For this study, researchers recruited 38 study participants over the age of 60 from 17 medical sites across five European countries, all who had geographic atrophy due to AMD, and vision worse than 20/320 in at least one of their eyes.
Study participants underwent a medical procedure to have the PRIMA implant placed in one eye. Within four to five weeks, they were given the special glasses to start using.
Scientists found that of the 32 participants who completed the trial, 26 experienced clinically meaningful improvements to their visual acuity after one year of using the PRIMA system. On average, participants regained the ability to see another five lines on the standard eye chart, with one improving by 12 lines.
Additionally, 27 study participants reportedly regained their ability to read, using the system to read letters and numbers at home.
“It’s the first time that any attempt at vision restoration has achieved such results in a large number of patients,” José-Alain Sahel, MD, Distinguished Professor and Chairman, Department of Ophthalmology in the School of Medicine at the University of Pittsburgh and Endowed Chair of The Eye and Ear Foundation and co-lead author of this study, said in a press release.
“More than 80% of the patients were able to read letters and words, and some of them are reading pages in a book. I don’t think we’ll ever be able to restore full 20/20 vision with the implant alone, but we are investigating tricks that could further improve people’s quality of life and take them above the threshold for legal blindness. One of the main requests we hear from patients is to be able to recognize faces and emotions again, and that’s something we’re working toward,” he said.
Medical News Today had the opportunity to speak with Benjamin Bert, MD, a board certified ophthalmologist at MemorialCare Orange Coast Medical Center in Fountain Valley, CA, about this study, who commented it is great to have new technologies being developed to help treat vision loss.
“This particular study expands the information about the PRIMA system, which is fascinating because it utilizes the remaining functional retinal anatomy while providing an artificial replacement for the damaged photoreceptor layer occurring in geographic atrophy caused by AMD,” Bert explained.
“As the population is aging and people are living longer, age-related conditions are increasing in prevalence. For that reason, it is important to continue to work on ways to help restore or at least partially restore vision for people suffering from age-related conditions like AMD. Any improvement in vision can help people remain independent as they age and help avoid trips and falls.”
— Benjamin Bert, MD
“In order to be comfortable in offering this to patients, it would be nice to know the longevity of the device, long-term support for the device, modifications to the surgical procedure to minimize complications, and the potential future prospects for upgrading the technology,” he added.
MNT also spoke with Jonathan Gloth, MD, a board certified ophthalmologist and fellowship trained vitreoretinal surgeon at Hackensack Meridian Jersey Shore University Medical Center and Ocean University Medical Center in New Jersey, who found this to be a promising study for patients with geographic atrophy.
“Though the initial sample size is small (38 patients) in the recently published article, 80% of patients achieved clinically significant visual improvement,” Gloth said. “This retinal implant is placed in a better location, the subretinal space, which affords these patients higher resolution and better visual acuity than previously studied prosthetic retinal implants.”
“It is imperative that we find ways to improve vision in patients with geographic atrophy as it affects over a million people in the United States and 8 million people worldwide. These patients suffer profound vision loss and lose the ability to read, drive, and recognize faces.”
— Jonathan Gloth, MD
“This study will have to be reproduced at a larger scale to further assess the safety of the device,” Gloth added. “81% of patients in this study suffered serious adverse effects. As retina specialists become more familiar with the surgical implantation technique, I expect this compaction rate to decline.”





