What do I need to know about colorectal cancer?
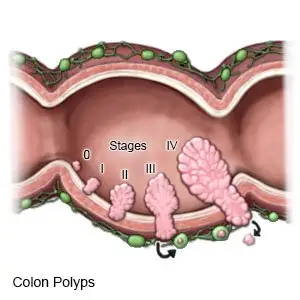
Colorectal cancer starts in the large intestine (colon) or rectum. The cancer may begin as a small polyp (lump of tissue) that grows inside your intestine.
 |
What increases my risk for colorectal cancer?
- Diseases of the colon, such as polyps or ulcerative colitis
- A family history of colon cancer
- Foods that are high in fat, or high amounts of red meat, such as beef
- Foods that are low in fiber, or not enough fruits and vegetables
- Lack of physical activity
- Cigarette smoking or heavy alcohol use
- Medical conditions such as diabetes or obesity
- Exposure to chemicals, such as asbestos
What are the signs and symptoms of colorectal cancer?
- Bloody or black bowel movements
- Abdominal pain or cramps, or a feeling of fullness
- Frequent fatigue or weakness
- Diarrhea or constipation
- Rectal pain
- Unexplained weight loss
How is colorectal cancer diagnosed?
Your healthcare provider will need to test polyps or tumors for cancer. Your provider will tell you which stage the cancer is in. Stages go from 0 to 4. Lower stages mean the cancer is only in the lining of the colon. Stage 4 is the highest and means the cancer has spread to other areas. Any of the following may be used to check for polyps or tumors:
- A digital rectal exam (DRE) means your healthcare provider inserts gloved fingers into your rectum. He or she may not be able to feel a tumor. The DRE is used with other tests to check for cancer.
- A bowel movement sample may be tested for blood.
- A biopsy is a procedure to take a sample of the tumor to be tested for cancer.
- An ultrasound or CT may show where the tumor is located, or if the cancer has spread. You may be given contrast liquid to help the tumor show up better. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid.
- A barium enema is an x-ray of the colon. A tube is put into your anus, and a liquid called barium is put through the tube. Barium is used so that healthcare providers can see your colon better on the x-ray.
- Genomic sequencing tests may show which cells are causing cancer. This can help your provider choose which medicine to give you.
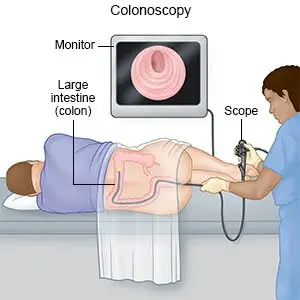
- A colonoscopy or sigmoidoscopy may be used to look at your colon. A tube with a light on the end will be put into your anus, and then moved forward into your colon. Your healthcare provider may take tissue samples to be tested for cancer.
How is colorectal cancer treated?
Your healthcare provider can help you understand which treatments may be best for you, based on the cancer stage. You may need 1 or more of the following:
- Chemotherapy (chemo) medicine is used to kill cancer cells. Chemo may be used to shrink the tumor or lymph nodes before surgery. Chemo may also be used after surgery to decrease the risk that cancer will come back. Chemo may be given with other treatment. Your provider can help you understand the benefits and risks, and if added chemo is right for you.
- Radiation therapy is used to kill cancer cells with x-rays or gamma rays. Radiation may be given either before or after surgery to kill cancer cells. It may be given alone or with chemo.
- Targeted therapy is medicine used to target specific cancer cells and kill them.
- Surgery may be used to remove the tumor. Surgery may be needed to remove part of your colon, rectum, or lymph nodes. This may help stop the cancer from spreading. Surgery may also be used to remove cancer cells that have spread to your liver or lung.
Treatment options
The following list of medications are in some way related to or used in the treatment of this condition.
- Xeloda
- Avastin
- Keytruda
- Opdivo
- Betaseron
View more treatment options
What can I do to manage or prevent colorectal cancer?
- Get screened as directed. Screening means you are checked for colorectal cancer, even if you do not have signs or symptoms. Screening is recommended starting at age 50 and continuing to age 75 if you are at average risk. Your healthcare provider may suggest screening starting at age 45. Screening may start before you are 45 or continue after you are 75 if your risk is high. Your provider will tell you how often to get screened. Timing depends on the type of screening and if polyps or other problems were found. Timing also depends on your age and if you are at increased risk for cancer. Screening may be recommended every 1, 2, 5, or 10 years.
- Do not smoke. Nicotine can damage blood vessels and make it hard to manage colorectal cancer. Smoking also increases your risk for new or returning cancer and delays healing after treatment. Do not use e-cigarettes or smokeless tobacco in place of cigarettes or to help you quit. They still contain nicotine. Ask your healthcare provider for information if you currently smoke and need help quitting.
- Limit or do not drink alcohol as directed. Men should limit alcohol to 2 drinks per day. Women should limit alcohol to 1 drink per day. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Drink liquids as directed. Ask how much liquid to drink each day and which liquids are best for you. If you have nausea or diarrhea from cancer treatment, extra liquids may help decrease your risk for dehydration.
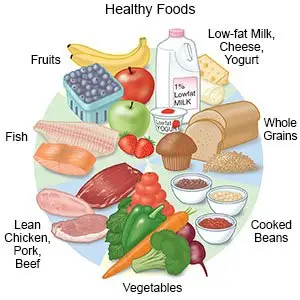
- Eat healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. You may need to change what you eat during treatment. Do not eat foods or drink liquids that cause gas, such as cabbage, beans, onions, or soda. A dietitian may help to plan the best meals and snacks for you.
- Be physically active as directed. Ask about the best exercise plan for you. Physical activity, such as exercise, may improve your energy levels and appetite.
Call your local emergency number (911 in the US) for any of the following:
- You suddenly feel lightheaded and short of breath.
- You have chest pain when you take a deep breath or cough.
- You cough up blood.
When should I seek immediate care?
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You vomit multiple times and cannot keep any food or liquids down.
- You see blood in your bowel movements.
When should I call my doctor or oncologist?
- You have a fever.
- You cannot control your diarrhea or constipation.
- Your pain is worse or does not go away after you take your pain medicine.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2023 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.




