Drug Detail:Probuphine implant (Buprenorphine (implant) [ bue-pre-nor-feen ])
Generic Name: buprenorphine hydrochloride 80mg
Drug Class:
Drug Addiction Treatment Act
Under the Drug Addiction Treatment Act (DATA) codified at 21 United States Code (U.S.C.) 823(g), use of this product in the treatment of opioid dependence is limited to Healthcare Providers who meet certain qualifying requirements, and who have notified the Secretary of Health and Human Services (HHS) of their intent to prescribe or dispense this product for the treatment of opioid dependence and have been assigned a unique identification number that must be included on every prescription.
Important Dosage and Administration Information
PROBUPHINE implants should be used only in patients who are opioid tolerant.
Each dose consists of four PROBUPHINE implants inserted subdermally in the inner side of the upper arm.
PROBUPHINE subdermal implants are intended to be in place for 6 months of treatment. Remove PROBUPHINE implants by the end of the sixth month.
New implants may be inserted subdermally in an area of the inner side of either upper arm that has not been previously used at the time of removal, if continued treatment is desired. If new implants are not inserted on the same day as the removal of implants, maintain patients on their previous dosage of transmucosal buprenorphine (i.e., the dose from which they were transferred to PROBUPHINE treatment) prior to additional PROBUPHINE treatment.
After one insertion in each arm, most patients should be transitioned back to a transmucosal buprenorphine-containing product for continued treatment. There is no experience with inserting additional implants into other sites in the arm to recommend an approach to a second insertion into a previously-used arm. Neither re-insertion into previously-used administration sites, nor into sites other than the upper arm, has been studied [see Dosage and Administration (2.4, 2.5, and 2.9), Warnings and Precautions (5.1)].
Patient Access to Naloxone for the Emergency Treatment of Opioid Overdose
Discuss the availability of naloxone for the emergency treatment of opioid overdose with the patient and caregiver. Because patients being treated for opioid use disorder have the potential for relapse, putting them at risk for opioid overdose, strongly consider prescribing naloxone for the emergency treatment of opioid overdose, both when initiating and renewing treatment with PROBUPHINE. Also consider prescribing naloxone if the patient has household members (including children) or other close contacts at risk for accidental ingestion or opioid overdose [see Warnings and Precautions (5.4)].
Advise patients and caregivers that naloxone may also be administered for a known or suspected overdose with buprenorphine, such as due to an accidental exposure of a household contact to a PROBUPHINE implant that has been expelled. Inform patients to call a Healthcare Provider immediately and follow protrusion or/and expulsion guidelines [see Patient Counseling Information (17)].
Higher than normal doses and repeated administration of naloxone may be necessary due to the long duration of action of PROBUPHINE and its affinity for the mu receptor.
Inform patients and caregivers of their options for obtaining naloxone as permitted by individual state naloxone dispensing and prescribing requirements or guidelines (e.g., by prescription, directly from a pharmacist, or as part of a community-based program) [see Patient Counseling Information (17)].
Healthcare Provider Training
All Healthcare Providers who intend to prescribe PROBUPHINE must successfully complete a live training program [see Warnings and Precautions (5.2)].
All Healthcare Providers performing insertions and/or removals of PROBUPHINE must successfully complete a live training program, and demonstrate procedural competency prior to inserting or removing the implants.
Information concerning the insertion and removal procedures can be obtained by calling 1-844-859-6341. The basis for successful use and subsequent removal of PROBUPHINE is a correct and carefully-performed subdermal insertion of the four implants in accordance with the instructions. As a prerequisite for participating in the live training program leading to certification, the Healthcare Provider must have performed at least one qualifying surgical procedure in the last 3 months. Qualifying procedures are those performed under local anesthesia using aseptic technique, and include, at a minimum, making skin incisions, or placing sutures [see Warnings and Precautions (5.2)].
Patient Selection
PROBUPHINE implants are only for use in patients who meet ALL of the following criteria:
- Achieved and sustained prolonged clinical stability on transmucosal buprenorphine
- Are currently on a maintenance dose of 8 mg per day or less of a Subutex or Suboxone sublingual tablet or its transmucosal buprenorphine product equivalent (the dose of transmucosal buprenorphine providing blood levels comparable or lower than the level provided by PROBUPHINE)
- Patients should not be tapered to a lower dose for the sole purpose of transitioning to PROBUPHINE.
- Stable transmucosal buprenorphine dose (of 8 mg per day or less of a sublingual Subutex tablet or Suboxone sublingual tablet or its transmucosal buprenorphine product equivalent) for three months or longer without any need for supplemental dosing or adjustments
Examples of acceptable doses of transmucosal buprenorphine include:
- Subutex (buprenorphine) sublingual tablet (generic equivalent) 8 mg or less
- Suboxone (buprenorphine and naloxone) sublingual tablet (generic equivalent) 8 mg/2 mg or less
- Bunavail (buprenorphine and naloxone) buccal film 4.2 mg/0.7 mg or less
- Zubsolv (buprenorphine and naloxone) sublingual tablets 5.7 mg/1.4 mg or less
Consider the following factors in determining clinical stability and suitability for PROBUPHINE treatment:
- period free from illicit opioid drug use
- stability of living environment
- participation in a structured activity/job
- consistency in participation in recommended behavioral therapy/peer support program
- consistency in compliance with clinic visit requirements
- minimal to no desire or need to use illicit opioids
- period without episodes of hospitalizations (addiction or mental health issues), emergency room visits, or crisis interventions
- social support system
Clinical Supervision
Examine the insertion site one week following insertion of PROBUPHINE for signs of infection or any problems with wound healing, including evidence of implant extrusion from the skin.
The recommended visit schedule for most patients is a frequency of no less than once-monthly for continued counseling and psychosocial support.
Although some patients may require occasional supplemental dosing with buprenorphine, patients should not be provided with prescriptions for transmucosal buprenorphine-containing products for as-needed use. Instead, patients who feel the need for supplemental dosing should be seen and evaluated promptly. Ongoing use of supplemental dosing with transmucosal buprenorphine indicates that the amount of buprenorphine delivered by PROBUPHINE is not adequate for stable maintenance. Consider use of alternate buprenorphine products for maintenance of treatment.
Insertion of PROBUPHINE
Preparation
Prior to inserting PROBUPHINE, carefully read the insertion instructions as well as the full prescribing information.
Before insertion of PROBUPHINE, confirm that:
- The patient does not have any contraindications for the use of PROBUPHINE [see Contraindications (4)].
- The patient has had a medical history and physical examination.
- The patient understands the benefits and risks of PROBUPHINE.
- The patient has received a copy of the Medication Guide included in the packaging.
- The patient does not have allergies to the antiseptic and anesthetic to be used during insertion.
Insert PROBUPHINE Under Aseptic Conditions.
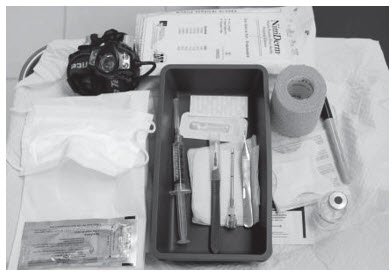
The Following Equipment is Needed for Implant Insertion:
- An examination table for the patient to lie on
- Instrument stand, sterile tray
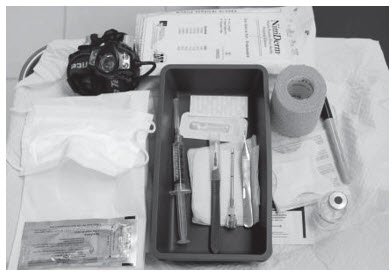
- Adequate lighting (e.g., headlamp)
- Sterile fenestrated drape
- Latex and talc-free sterile gloves
- EtOH prep
- Surgical marker
- Antiseptic solution (e.g., chlorhexidine)
- Local anesthetic (1% lidocaine with epinephrine 1:100,000)
- 5 mL syringe with 1.5 inch 25g needle
- Adson single tooth tissue forceps
- #15 blade scalpel
- ¼ inch thin adhesive strip (butterfly strip) (e.g., Steri-strip skin closures)
- 4×4 sterile gauze
- Adhesive bandages
- 3-inch pressure bandages
- Liquid adhesive (e.g., Mastisol)
- 4 PROBUPHINE implants
- 1 PROBUPHINE disposable applicator (Figure 1)
The applicator and its parts are shown in Figure 1.
Correctly performed subdermal insertion of the implants will facilitate their removal. Implants should be placed just under the skin to avoid the large blood vessels that lie in the subcutaneous deep tissue. If the implants are placed improperly, resulting in deep tissue placement, the implants will be more difficult to remove.
Figure 1

Insertion Procedure
Step 1. Have the patient lie on his/her back, with the intended arm flexed at the elbow and externally rotated, so that the hand is positioned next to the head (Figure 2).
Figure 2

Step 2. Identify the insertion site, which is at the inner side of the upper arm about 8-10 cm (3-4 inches) above the medial epicondyle of the humerus in the sulcus between the biceps and triceps muscle. Having the patient flex the biceps muscle may facilitate identification of the site (Figure 3).
Figure 3

Step 3. Clean insertion site with alcohol prep pad prior to marking the skin.
Step 4. Mark the insertion site with the surgical marker. The implants will be inserted through a small 2.5 mm-3mm subdermal incision.
Step 5. Using the surgical marker, mark the channel tracks where each implant will be inserted by drawing 4 lines with each line 4 cm in length. The implants will be positioned in a close fan-shaped distribution 4-6 mm apart with the fan opening towards the shoulder (Figure 4). The closer the implants lie to each other at time of insertion, the more easily they can be removed. There should be at least 5 mm between the incision and the implant when the implant is properly positioned.
Figure 4

Step 6. Put on sterile gloves.
Step 7. Using aseptic technique, place the sterile equipment, PROBUPHINE implants and the applicator on the sterile field of the instrument stand. One applicator is used to insert all four implants.
Step 8. Check applicator function by removing the obturator from the cannula and relocking it.
Step 9. Clean the insertion site with an antiseptic solution (e.g., chlorhexidine) using gentle repeated back-and-forth strokes for 30 seconds. When using triple swab stick applicators, use each swab stick sequentially within the 30 seconds. Allow the area to air dry for approximately 30 seconds and do not blot or wipe away.
Step 10. Apply the sterile drape to the arm of the patient.
Step 11. Anesthetize the insertion area at the incision site and just under the skin along the planned insertion channels using local anesthetic (for example, by injecting 5 mL lidocaine 1% with epinephrine 1:100,000).
Step 12. After determining that anesthesia is adequate and effective, make a shallow incision that is 2.5-3 mm in length.
Step 13. Lift the edge of the incision opening with a toothed forceps. While applying counter-traction to the skin, insert only the tip of the applicator at a slight angle (no greater than 20 degrees), into the subdermal space (depth of 3-4 mm below the skin), with the bevel-up stop marking on the cannula facing upwards and visible with the obturator locked fully into the cannula (Figure 5).
Figure 5

Figure 6

Figure 7

Step 14. Lower the applicator to a horizontal position, lift the skin up with the tip of the applicator but keep the cannula in the subdermal connective tissue (Figure 6). While tenting (lifting), gently advance the applicator subdermally along the channel marking on the skin until the proximal marking on the cannula just disappears into the incision (Figure 7).
Step 15. While holding the cannula in place, unlock the obturator and remove the obturator.
Step 16. Insert one implant into the cannula (Figure 8), re-insert the obturator, and gently push the obturator forward (mild resistance should be felt) until the obturator stop line is level with the bevel-up stop marking, which indicates the implant is positioned at the tip of the cannula (Figure 9). Do not force the implant beyond the end of the cannula with the obturator. There should be at least 5 mm between the incision and the implant when the implant is properly positioned.
| Figure 8 | Figure 9 |
|
|
|
Step 17. While holding the obturator fixed in place on the arm, retract the cannula along the obturator, leaving the implant in place (Figure 10). Note: do not push the obturator. By holding the obturator fixed in place on the arm and by retracting the cannula, the implant will be left in its correct subdermal position.
Figure 10

Step 18. Withdraw the cannula until the hub is flush with the obturator, and then twist the obturator clockwise to lock onto the cannula (Figure 11). Retract the applicator, bevel up, until the distal marking of the cannula is visualized at the incision opening (the sharp tip remaining in the subcutaneous space).
Figure 11

Step 19. Redirect the applicator to the next channel marking while stabilizing the previously inserted implant, with your index finger, away from the sharp tip (Figure 12). Follow steps 13 through 16 for the insertion of the three remaining implants through the same incision, placing implants in a close fan-shaped distribution 4-6 mm apart at the top of the implant. The applicator can now be removed.
Figure 12

Step 20. Always verify the presence of each implant by palpation of the patient's arm immediately after the insertion. By palpating both ends of the implant, you should be able to confirm the presence of the 26 mm implant (Figure 13). If you cannot feel each of the four implants, or are in doubt of their presence, use other methods to confirm the presence of the implant. Suitable methods to locate are: Ultrasound with a high frequency linear array transducer (10 MHz or greater) or Magnetic Resonance Imaging (MRI). Please note that the PROBUPHINE implants are not radiopaque and cannot be seen by X-ray or CT scan. If ultrasound and MRI fail, call 1-844-859-6341.
Figure 13

Step 21. Apply pressure to the incision site for approximately five minutes if necessary.
Step 22. Clean the incision site. Apply liquid adhesive to the skin margins and allow to dry before closing the incision with the ¼ inch thin adhesive strip (butterfly strip) (for example, Steri-strip skin closures).
Step 23. Place a small adhesive bandage over the insertion site.
Step 24. Apply a pressure bandage with sterile gauze to minimize bruising. The pressure bandage can be removed in 24 hours and the adhesive bandage can be removed in three to five days.
Step 25. Complete the PATIENT IDENTIFICATION CARD and give it to the patient to keep. Also, complete the PATIENT CHART STICKER and affix it to the patient medical record or scan or input into electronic medical record. Provide the patient with the Medication Guide and explain proper care of the insertion site.
Step 26. The applicator is for single use only. Dispose of the applicator in accordance with the Centers for Disease Control and Prevention guidelines for hazardous waste.
Step 27. Instruct the patient to apply an ice pack on his/her arm for 40 minutes every two hours for first 24 hours and as needed.
Step 28. Complete the PROBUPHINE REMS Insertion/Removal Log Form.
PROBUPHINE Removal Procedure
Before initiating the removal procedure, read the instructions for removal.
Identify the location of the implants by consulting the PATIENT IDENTIFICATION CARD and/or THE PATIENT CHART STICKER. The exact location of all implants in the arm (patients will have four implants) should be verified by palpation.
If all of the implants are not palpable, use other methods to confirm the presence of the implant(s). Non-palpable implants should always be located prior to attempted removal. Suitable methods to locate implants are: Ultrasound with a high frequency linear array transducer (10 MHz or greater) or Magnetic Resonance Imaging (MRI). Note that PROBUPHINE implants are not radiopaque and cannot be seen by X-ray or CT scan.
Report any event of failure to locate non-palpable implants using MRI or ultrasound, by calling 1-844-859-6341 for company surveillance purposes.
After localization of a non-palpable implant, removal should be performed under ultrasound guidance. Exploratory surgery without knowledge of the exact location of all implants is strongly discouraged.
There is a greater risk of injury to neural and vascular structures during removal of implants located deeper than the subdermal space. As the anatomical location of these structures must be taken into consideration during the removal of deeply inserted implants, the procedure should only be attempted by Healthcare Providers familiar with this anatomy. A surgical specialist consulted to assist with a difficult removal does not need to be certified in the REMS program.
Preparation
Before removal of PROBUPHINE, confirm that:
- The patient does not have allergies to the antiseptic or the anesthetic to be used. Implants should be removed under aseptic conditions.
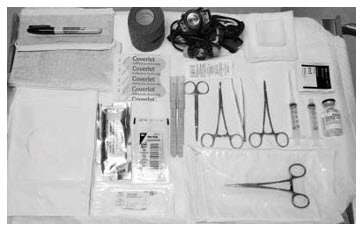
The Following Equipment is Needed for Implant Removal:
- An examination table for the patient to lie on
- Instrument stand
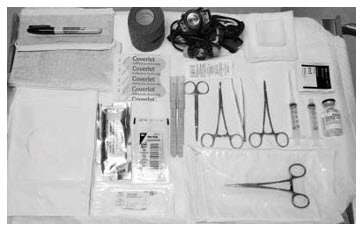
- Sterile tray
- Adequate lighting (e.g., headlamp)
- Sterile fenestrated drapes
- Latex and talc-free sterile gloves
- EtOH prep
- Antiseptic solution (e.g., chlorhexidine)
- Surgical marker
- Local anesthetic (e.g., 1% lidocaine with epinephrine 1:100,000)
- 5 mL syringe with 1.5 inch 25g needle
- Adson single tooth tissue forceps
- Mosquito forceps
- Two X-plant clamps (vasectomy fixation clamps with 2.5 mm ring diameter)
- Iris scissors
- Needle driver
- #15 blade scalpel
- Sterile ruler
- 4×4 sterile gauze
- Adhesive bandage
- 3-inch pressure bandage
- Sutures (e.g., 4-0 Prolene™ with an FS-2 cutting needle) (may be absorbable)
Removal Procedure
Step 1. Have the patient lie on his/her back, with the implant arm flexed at the elbow and externally rotated, so that the hand is positioned next to the head.
Step 2. Reconfirm the location of the implants by palpation.
Step 3. Clean removal site with alcohol prep pad prior to marking the skin.
Step 4. Mark the location of the implants with a surgical marker. In addition, mark the location of the incision, parallel to the axis of the arm, between the second and third implants (Figure 14).
Figure 14

Step 5. Put on sterile gloves.
Step 6. Using aseptic technique, place the sterile equipment on the sterile field of the instrument stand.
Step 7. Clean the removal site with an antiseptic solution (e.g., chlorhexidine) using gentle repeated back and forth strokes for 30 seconds. When using triple swab stick applicators, use each swab stick sequentially within the 30 seconds. Allow the area to air dry for approximately 30 seconds and do not blot or wipe away.
Step 8. Apply the sterile drape to the arm of the patient.
Step 9. Anesthetize the incision site and the subcutaneous space containing the implants (for example, by injecting 5-7 mL lidocaine 1% with epinephrine 1:100,000). Separate needles may be used for the incision site and the subcutaneous injections. NOTE: Be sure to inject the local anesthetic just beneath the implants; this will effectively lift the implants toward the skin, facilitating removal of the implants.
Step 10. After determining that anesthesia is adequate and effective, make a 7-10 mm incision with a scalpel, parallel to the axis of the arm, between the second and third implants.
Step 11. Pick up the skin edge with Adson single-toothed tissue forceps and separate the tissues above and below the first visualized implant using an iris scissors or a curved mosquito forceps (Figure 15). Grasp the center of the implant with the X-plant clamp and apply gentle traction. Use the technique of spreading and closing with either the iris scissors or mosquito forceps to separate the fibrous tissue (Figure 16). If the implant is encapsulated use the scalpel to shave the tissue sheath and carefully dissect the tissue around the implant. The implant can then be removed.
| Figure 15 | Figure 16 |
 |
 |
Step 12. Retract the next visible implant toward the incisional opening. You may see tenting of the skin at this point if the surrounding tissue is still adhering to the implant. Maintain gentle traction on the implant while you continue to dissect proximally and distally until the implant is free of all adhering tissue. At this point, you may require the use of your second X-plant clamp to remove the implant. If the implant is encapsulated use the scalpel to shave the tissue sheath and carefully dissect the tissue around the implant. The implant can then be removed.
Step 13. After removal of each implant confirm that the entire implant, which is 26 mm long, has been removed by measuring its length. If a partial implant (less than 26 mm) is removed, the remaining piece should be removed by following the same removal instructions. Follow steps 11 through 13 for the removal of the remaining implants through the same incision. Visual identification of whether an entire implant has been removed is unreliable. Therefore, it is important to measure the implant to ensure the entire implant has been removed.
Step 14. After removal of all four implants, clean the incision site.
Step 15. Close the incision with sutures.
Step 16. Place an adhesive bandage over the incision.
Step 17. Use the sterile gauze and apply gentle pressure for five minutes to the incision site to ensure hemostasis.
Step 18. Apply a pressure bandage with sterile gauze to minimize bruising. The pressure bandage can be removed in 24 hours and the adhesive bandage in three to five days.
Step 19. Counsel the patient on proper aseptic wound care. Instruct the patient to apply an ice pack to his/her arm for 40 minutes every two hours for first 24 hours and as needed.
Step 20. Schedule an appointment for the sutures to be removed.
Step 21. The removed implant contains a significant amount of residual buprenorphine. It must be handled with adequate security, accountability, and proper disposal, per facility procedure for a Schedule III drug product, and per applicable federal, state, and local regulations. Disposal of PROBUPHINE implants should also be in keeping with local, State and Federal regulations governing the disposal of pharmaceutical biohazardous waste.
Step 22. Complete the PROBUPHINE REMS Insertion/Removal Log Form.
If implant(s) or implant fragment(s) are not removed during a removal attempt, the patient should undergo imaging for localization as soon as is feasible. The subsequent removal attempt should be performed on the same day of localization. If localization and a second removal attempt are not performed on the same day as the initial removal attempt that necessitated imaging for localization, the wound should be closed with sutures in the interim.
Spontaneous Expulsion
If spontaneous expulsion of the implant occurs after insertion, the following steps should be taken:
- Schedule two appointments for the patient to return to the office of the inserting Healthcare Provider as soon as possible and to the office of the prescribing Healthcare Provider.
- Instruct the patient to place the implant in a plastic bag, store it safely out of reach of children, and to bring it to the Healthcare Provider office to determine whether the full implant has been expelled.
- If the patient returns the expelled implant, measure it to ensure that the entire implant was expelled (26 mm).
- Dispose of the removed implant in keeping with local, state, and federal regulations governing the disposal of pharmaceutical biohazardous waste, after measuring.
- Examine incision site for infection. If infected, treat appropriately and determine if remaining implants need to be removed.
- If the expelled implant is not intact, palpate the insertion location to identify the location of any remaining partial implant. Remove the remaining partial implant using the techniques described above.
- Call 1-844-859-6341 to obtain a new kit that will include four implants and return instructions for any unused implants.
- The prescribing Healthcare Provider must carefully monitor patient until the implant is replaced to evaluate for withdrawal or other clinical indicators that supplemental transmucosal buprenorphine may be needed.
- Schedule an appointment to insert replacement implant(s).
- Insert the replacement implant(s) in same arm either medially or laterally to in situ implants. Alternatively, replacement implant(s) may be inserted in the contralateral arm.
- Record the new serial number on the PROBUPHINE REMS Insertion/Removal Log Form.
Continuation of Therapy: Subsequent Insertion of PROBUPHINE in the Contralateral Arm
There is no clinical experience with insertion of PROBUPHINE beyond a single insertion in each arm. If continued treatment is desired at the end of the first six-month treatment cycle, PROBUPHINE implants may be replaced by new implants at the time of removal in the contralateral arm, following the insertion steps above to locate the appropriate insertion site.
If new implants are not inserted on the same day as the removal, patients should be maintained on their previous dose of transmucosal buprenorphine (i.e., the dose from which they were transferred to PROBUPHINE treatment) prior to additional PROBUPHINE treatment [see Dosage and Administration (2.6), Warnings and Precautions (5.1)].
There is no experience with inserting additional implants into other sites in the arm to recommend an approach to a second insertion into a previously-used arm. Neither re-insertion into previously used administration sites, nor into sites other than the upper arm, have been studied. It is important to avoid previously-implanted sites because the effect of scarring and fibrosis in previously-used insertion sites on either the effectiveness of PROBUPHINE or the safety of insertion have not been evaluated. After one insertion in each arm, additional cycles of treatment should only be considered if the potential benefits of continuing PROBUPHINE outweigh the potential risks of additional insertion and removal procedures, taking into account the experience of the Healthcare Provider with PROBUPHINE procedures and related procedures, and the clinical need of the patient for ongoing treatment with subdermal medication. In most cases, patients should be transitioned back to a transmucosal buprenorphine-containing product for continued treatment.