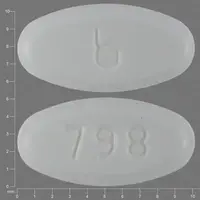
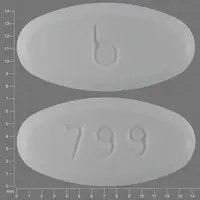
Generic name: buprenorphine
Drug class: Opioids (narcotic analgesics)
Availability: Prescription only
Pregnancy & Lactation: Risk data available
Brand names: Buprenex injection, Buprenorphine, Probuphine implant, Sublocade injection, Belbuca
What is Buprenorphine?
Buprenorphine is an opioid medication used to treat opioid use disorder (OUD), acute pain, and chronic pain.
Buprenorphine is used for opioid addiction to reduce cravings and withdrawal symptoms without causing euphoria or dangerous side effects and helps prevent relapse. It works by being a substitute for the drug being abused, so the patient has minimal discomfort, which allows the patient to focus on their recovery. Buprenorphine for OUD is used as part of a complete treatment program that also includes counseling and behavioral therapy.
For opioid use disorder, buprenorphine is available as long-acting injections (Sublocade, Brixadi) and sublingual tablets (Subutex discontinued, generics available).
Buprenorphine is used to treat acute pain that is severe enough to require an opioid analgesic and moderate to severe chronic pain that is not controlled by other medicines. For chronic around-the-clock pain, it is available as buprenorphine skin patches (Butrans) and buprenorphine buccal films (Belbuca), and for acute pain is available as an injection (Buprenex).
Buprenorphine-naloxone combinations are also available to be used for opioid addication and include sublingual film (Bunavail), sublingual film and sublingual tablets (Suboxone), and sublingual tablets (Zubsolv).
Buprenorphine's mechanism of action is that is a partial agonist at the mu-opioid receptor and an antagonist at the kappa-opioid receptor.
Is buprenorphine a controlled substance?
Yes, buprenorphine is a Schedule III controlled drug, which means it has a potential for abuse more than those in Schedules 4 and 5. If abused, it may lead to moderate or low physical dependence or high psychological dependence.
Related/similar drugs
aspirin, acetaminophen, tramadol, duloxetine, naproxen, oxycodone, TylenolWarnings
MISUSE OF OPIOID MEDICINE CAN CAUSE ADDICTION, OVERDOSE, OR DEATH. Keep buprenorphine in a place where others cannot get to it.
Patient Access to Naloxone for the Emergency Treatment of Opioid Overdose. Patients should have access to naloxone to treat opioid overdose based on the patient’s risk factors for overdose, such as currently using a CNS depressant, a history of an opioid use disorder, or previous opioid overdose. Having naloxone available is important if the patient has household members (including children) or other close contacts at risk for accidental exposure or overdose.
Taking this medicine during pregnancy may cause life-threatening withdrawal symptoms in the newborn.
Fatal side effects can occur if you use this medication with alcohol or with other drugs that cause drowsiness or slow your breathing.
How should I use Buprenorphine
Use buprenorphine exactly as it was prescribed for you. Follow the directions on your prescription label and read all medication guides. Your doctor may occasionally change your dose. Never use this medication in larger amounts, or for longer than prescribed.
Opioid Use Disorder
Buprenorphine Sublingual (for OUD)
Buprenorphine sublingual is usually taken only at the start of treatment for addiction (induction phase). Most people are later switched to long-acting buprenorphine (Sublocade injection or Brixadi injection) or another medicine that contains buprenorphine with naloxone (Bunavail, Suboxone, Zubsolv). You may receive your first doses of buprenorphine sublingual in a hospital or clinic setting until your condition improves. Use dry hands when handling the tablet. Place the tablet under your tongue and allow it to dissolve with your mouth closed. Do not chew the tablet or swallow it whole. If your doctor has prescribed more than 2 tablets per dose, place the correct number of tablets under your tongue at the same time and allow them to dissolve completely. Do not eat or drink anything until the tablet has completely dissolved in your mouth. Never crush or break a pill to inhale the powder or mix it into a liquid to inject the drug into your vein. Doing so could result in death.
Extended-release buprenorphine subcutaneous injection (for OUD)
Buprenorphine extended-release injection is given subcutaneously (just under the skin). Sublocade is given in the abdomen monthly, and Brixadi can be given in your buttock, thigh, upper arm, or stomach and can be given weekly or monthly.
Sublocade should only be used when patients have received treatment with an oral transmucosal (used under the tongue or inside the cheek) buprenorphine-containing medicine for 7 days and are taking a dose that controls withdrawal symptoms for at least seven days. Sublocade is injected as a liquid. After the injection, Sublocade changes to a solid form called a depot. The depot may be seen or felt as a small bump under your skin at the injection site on your abdomen for several weeks. The depot will get smaller over time. Do not try to remove the depot, and do not rub or massage the injection site. Sublocade is part of a complete treatment plan that should include counseling.
Brixadi should only be used if you are currently receiving buprenorphine treatment or if your healthcare provider has given you a test dose of buprenorphine first to see if you are able to tolerate it. If you are new to Brixadi treatment, the upper arm should only be used after 4 doses of Brixadi in your buttock, thigh, or stomach. Brixadi is injected as a liquid; after the injection, the liquid changes to a gel form called a depot. The depot is not always felt under the skin. Do not try to remove the depot. Brixadi is part of a complete treatment plan that should include counseling.
Pain
Buprenex (buprenorphine injection) is used for pain, it is given by deep intramuscular or slow (over at least 2 minutes) intravenous injection at up to 6-hour intervals, as needed.
Butrans skin patch is used for chronic around-the-clock pain. It is applied once a week and worn continuously for 1 week. Do not change your dose. Apply Butrans exactly as prescribed by your healthcare provider. Your doctor will prescribe you the lowest effective dose for the shortest time needed. Do not take hot baths or sunbathe, use hot tubs, saunas, heating pads, electric blankets, heated waterbeds, or tanning lamps as these can cause an overdose that can lead to death.
Belbuca buccal films are used for around-the-clock treatment of moderate to severe chronic pain. Using a finger, place the yellow side of the Belbuca buccal film against the inside of your moistened cheek. Press and hold the Belbuca buccal film in place for 5 seconds and then take your finger away. Once in place, the film will dissolve completely in about 30 minutes. Do not eat or drink anything until the Belbuca film has completely dissolved in your mouth. Rinse your mouth with water after the medicine dissolves. Wait one hour after the film dissolves to brush your teeth to prevent damage to the teeth and gums. Do not chew the Belbuca film or swallow it whole. You should receive regular dental checkups while using Belbuca.
General information about using this medicine.
Never share opioid medicine with another person, especially someone with a history of drug abuse or addiction. MISUSE CAN CAUSE ADDICTION, OVERDOSE, OR DEATH. Keep the medication in a place where others cannot get to it. Selling or giving away opioid medicine is against the law.
You may need frequent blood tests to check your liver function.
If you need surgery, tell the surgeon ahead of time that you are using this medicine.
Any medical care provider who treats you should know that you are being treated for opioid addiction and that you are on buprenorphine. Make sure your family members know how to provide this information in case they need to speak for you during an emergency.
Do not stop using this medication suddenly, or you could have unpleasant withdrawal symptoms. Ask your doctor how to safely stop using this medicine.
Store at room temperature away from moisture and heat. Keep track of your medicine. Buprenorphine is a drug of abuse, and you should be aware if anyone is using your medicine improperly or without a prescription.
Do not keep leftover opioid medication. Just one dose can cause death in someone using this medicine accidentally or improperly. Ask your pharmacist where to locate a drug take-back disposal program. If there is no take-back program, flush the unused medicine down the toilet.
For detailed dosing information click the link below.
Before Taking
You should not use this medicine if you are allergic to buprenorphine or:
- If you have used another narcotic drug within the past 4 hours.
To make sure this medication is safe for you, tell your doctor if you have ever had:
- methadone treatment;
- breathing problems, sleep apnea;
- abnormal curvature of the spine that affects breathing;
- liver disease (especially hepatitis B or C);
- kidney disease;
- enlarged prostate, urination problems;
- a head injury or brain tumor;
- alcoholism, hallucinations, mental illness; or
- problems with your stomach, gallbladder, adrenal gland, or thyroid.
Pregnancy
If you use buprenorphine while you are pregnant, your baby could become dependent on the drug. This can cause life-threatening withdrawal symptoms in the baby after it is born. Babies born dependent on habit-forming medicine may need medical treatment for several weeks.
Infertility
Chronic use of opioids may cause reduced fertility in females and males of reproductive potential. It is not known whether these effects on fertility are reversible
Breastfeeding
Buprenorphine can pass into breast milk and may cause drowsiness and breathing problems in a nursing baby. Ask your doctor about any risk to your baby.
What happens if I miss a dose?
Take the medicine as soon as you can, but skip the missed dose if it is almost time for your next dose. Do not take two doses at one time.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222. A buprenorphine overdose can be fatal, especially in a child or other person using the medicine without a prescription.
Overdose symptoms may include extreme drowsiness or weakness, cold or clammy skin, pinpoint pupils, slow heart rate, weak pulse, very slow breathing, or coma.
What should I avoid while using Buprenorphine?
Do not drink alcohol. Dangerous side effects or death could occur.
Avoid driving or operating machinery until you know how buprenorphine will affect you. Dizziness or drowsiness can cause falls, accidents, or severe injuries.
Buprenorphine side effects
Get emergency medical help if you have signs of an allergic reaction to buprenorphine: hives; difficult breathing; swelling of your face, lips, tongue, or throat.
Opioid medicine can slow or stop your breathing, and death may occur. A person caring for you should give naloxone and/or seek emergency medical attention if you have slow breathing with long pauses, blue colored lips, or if you are hard to wake up.
Call your doctor at once if you have:
- opioid withdrawal symptoms - shivering, goose bumps, increased sweating, feeling hot or cold, runny nose, watery eyes, diarrhea, muscle pain;
- noisy breathing, sighing, shallow breathing, breathing that stops during sleep;
- slow heartbeat or weak pulse;
- a light-headed feeling, like you might pass out;
- chest pain, trouble breathing;
- low cortisol levels - nausea, vomiting, loss of appetite, dizziness, worsening tiredness or weakness; or
- liver problems - nausea, upper stomach pain, itching, loss of appetite, dark urine, clay-colored stools, jaundice (yellowing of the skin or eyes).
Seek medical attention right away if you have symptoms of serotonin syndrome, such as: agitation, hallucinations, fever, sweating, shivering, fast heart rate, muscle stiffness, twitching, loss of coordination, nausea, vomiting, or diarrhea.
Common buprenorphine side effects may be more likely to occur, such as:
- constipation, nausea, vomiting;
- headache;
- increased sweating;
- sleep problems (insomnia); or
- pain anywhere in your body.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
See more: Buprenorphine Side EffectsWhat other drugs will affect Buprenorphine?
You may have breathing problems or withdrawal symptoms if you start or stop taking certain other medicines. Tell your doctor if you also use an antibiotic, antifungal medication, heart or blood pressure medication, seizure medication, or medicine to treat HIV or hepatitis C.
Buprenorphine can interact with many other drugs and cause dangerous side effects or death. Be sure your doctor knows if you also use:
- cold or allergy medicines, bronchodilator asthma/COPD medication, or a diuretic ("water pill");
- medicines for motion sickness, irritable bowel syndrome, or overactive bladder;
- other narcotic medications - opioid pain medicine or prescription cough medicine;
- a sedative like Valium - diazepam, alprazolam, lorazepam, Xanax, Klonopin, Versed, and others;
- drugs that make you sleepy or slow your breathing - a sleeping pill, muscle relaxer, medicine to treat mood disorders or mental illness; or
- drugs that affect serotonin levels in your body - a stimulant, or medicine for depression, Parkinson's disease, migraine headaches, serious infections, or nausea and vomiting.
This list is not complete. Other drugs may interact with buprenorphine, including prescription and over-the-counter medicines, vitamins, and herbal products. Not all possible interactions are listed here.