Generic name: naltrexone, naltrexone hydrochloride
Drug class: Antidotes, Drugs used in alcohol dependence
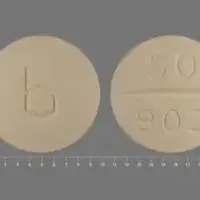
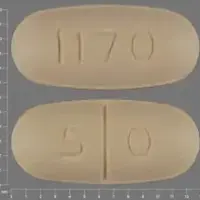
Dosage form: extended-release intramuscular injection (powder for suspension), oral tablet
Availability: Prescription only
Pregnancy & Lactation: Risk data available
Brand names: Vivitrol, Revia, Naltrexone (injection)
What is Naltrexone?
Naltrexone is a prescription medication used to treat alcohol use disorder and opioid use disorder. It helps you stop using these substances and remain off them.
Naltrexone belongs to a class of drugs known as opioid antagonists and works by blocking the mu opioid receptor. It blocks the effects of alcohol and opioid medications, preventing the intoxication these substances cause. Naltrexone also modifies how the hypothalamus, pituitary gland and adrenal gland (hypothalamic-pituitary-adrenal axis, HPA axis) interact to suppress the amount of alcohol consumed.
Naltrexone comes as an extended-release intramuscular injection (Vivitrol) and as oral tablets. The branded versions of naltrexone tablets (Revia, Depade) have been discontinued, but generic versions are available.
Naltrexone tablets were first approved by the US Food and Drug Administration (FDA) in 1984. In 2006, the FDA also approved Vivitrol, the extended-release intramuscular injection form of naltrexone.
What is naltrexone used for?
Naltrexone is a prescription medication that is used:
- to treat alcohol dependence
- for the blockade of the effects of exogenously administered opioids. To prevent relapse to opioid dependence, after opioid detoxification.
You should stop drinking alcohol or using opioids before starting naltrexone.
Naltrexone hydrochloride should not be used in children and adolescents under 18 years.
Warnings
Naltrexone can cause serious side effects, including:
1. Risk of opioid overdose.
You can accidentally overdose in two ways.
- Naltrexone blocks the effects of opioid drugs. Do not take large amounts of opioids, including opioid-containing medicines, such as heroin or prescription pain pills, to try to overcome the opioid-blocking effects of this medication. This can lead to serious injury, coma, or death.
- After you receive a dose of the extended-release injection form of this medication, its blocking effect slowly decreases and completely goes away over time. If you have used opioid street drugs or opioid-containing medicines in the past, using opioids in amounts that you used before treatment can lead to overdose and death. You may also be more sensitive to the effects of lower amounts of opioids:
- after you have gone through detoxification
- when your next naltrexone injection is due
- if you miss a dose of this medication
- after you stop naltrexone treatment
It is important that you tell your family and the people closest to you of this increased sensitivity to opioids and the risk of overdose.
You or someone close to you should call 911 or get emergency medical help right away if you:- have trouble breathing
- become very drowsy with slowed breathing
- have slow, shallow breathing (little chest movement with breathing)
- feel faint, very dizzy, confused, or have unusual symptoms
Talk to your healthcare provider about naloxone, a medicine that is available to patients for the emergency treatment of an opioid overdose.
Call 911 or get emergency medical help right away in all cases of known or suspected opioid overdose, even if naloxone is administered.
2. Severe reactions at the site of the naltrexone injection (injection site reactions).
Some people have had severe injection site reactions, including tissue death (necrosis), while receiving naltrexone injections. Some of these injection site reactions have required surgery. This medication must be injected by a healthcare provider. Call your healthcare provider right away if you notice any of the following at any of your injection sites:
- intense pain
- the area feels hard
- large area of swelling
- lumps
- blisters
- an open wound
- a dark scab
Tell your healthcare provider about any reaction at an injection site that concerns you, gets worse over time, or does not get better by two weeks after the injection.
3. Sudden opioid withdrawal.
Anyone who receives naltrexone must not use any type of opioid (must be opioid-free) including street drugs, prescription pain medicines, cough, cold, or diarrhea medicines that contain opioids, or opioid dependence treatments, buprenorphine or methadone, for at least 7 to 14 days before starting this medication. Using opioids in the 7 to 14 days before you start receiving treatment may cause you to suddenly have symptoms of opioid withdrawal when you receive treatment. Sudden opioid withdrawal can be severe, and you may need to go to the hospital.
You must be opioid-free before receiving naltrexone unless your healthcare provider decides that you don't need to go through detox first. Instead, your doctor may decide to give this medication in a medical facility that can treat you for sudden opioid withdrawal.
4. Liver damage or hepatitis. Naltrexone can cause liver damage or hepatitis.
Tell your healthcare provider if you have any of the following symptoms of liver problems during treatment with this medication:
- stomach area pain lasting more than a few days
- dark urine
- yellowing of the whites of your eyes
- tiredness
Your healthcare provider may need to stop treating you with this medication if you get signs or symptoms of a serious liver problem.
You must inform every doctor that treats you that you are taking Naltrexone. Non-opiate based anesthetics should be used if you require an anesthetic in an emergency situation. If you have to use opiate containing anesthetics, you may need higher doses than usual. You may also be more sensitive to the side-effects (breathing difficulties and circulatory problems).
How should I take Naltrexone
Using opioids in the 7 to 14 days before you start receiving naltrexone may cause you to suddenly have symptoms of opioid withdrawal. To avoid this you should not use opioids for a minimum of 7-10 days before starting treatment with naltrexone.
How to take naltrexone tablets
- Always take this medicine exactly as your doctor has told you. Check with your doctor or pharmacist if you are not sure.
- Take this medication once a day by mouth as your doctor tells you to.
- The amount of time you should take this medication for will be decided by your doctor. The usual length of treatment is three months. However, in certain cases, a longer period of treatment may be beneficial.
How you will receive a naltrexone injection
- Your injection will be given by a healthcare provider, about 1 time each month.
- Do not attempt to inject yourself with this medication. Serious reactions, some that may require hospitalization, might happen.
- Naltrexone is given as an injection into a muscle in your buttocks using a special needle that comes with it.
- After this medication is injected, it lasts for a month and it cannot be removed from the body.
Whenever you need medical treatment, be sure to tell the treating healthcare provider that you are receiving this medication and mention when you got your last dose. This is important because naltrexone can also block the effects of opioid-containing medicines that might be prescribed for you for pain, cough or colds, or diarrhea.
Carry written information with you at all times to alert healthcare providers that you are taking this medication so that they can treat you properly in an emergency. Ask your healthcare provider how you can get a wallet card to carry with you.
Dosing information
Tablets:
- Alcoholism: The recommended dose is 1 tablet (50 mg) once a day
- Opioid dependence: Start with half a tablet (25 mg) and if no withdrawal signs occur increase to the dose to 1 tablet (50 mg) a day from then on
Intramuscular injection:
- The recommended dose is naltrexone 380 mg delivered intramuscularly (IM) as a gluteal injection, every 4 weeks or once a month, alternating buttocks for each subsequent.
See the full prescribing information for further details about naltrexone dosing.
Before Taking
Do not use naltrexone if you:
- are using or have a physical dependence on/addiction to opioid-containing medicines or opioid street drugs.
To see whether you have a physical dependence on opioids, your healthcare provider may give you a small injection of a medicine called naloxone. This is called a naloxone challenge test. If you get symptoms of opioid withdrawal after the naloxone challenge test, do not start treatment with naltrexone at that time. Your healthcare provider may repeat the test after you have stopped using opioids to see whether it is safe to start this medication. - are having opioid withdrawal symptoms. Opioid withdrawal symptoms may happen when you have been taking opioids regularly and then stop.
Symptoms of opioid withdrawal may include:- anxiety
- sleeplessness
- yawning
- fever
- sweating
- teary eyes
- runny nose
- goose bumps
- shakiness
- hot or cold flushes
- muscle aches
- muscle twitches
- restlessness
- nausea and vomiting
- diarrhea
- stomach cramps
Tell your healthcare provider if you have any of these symptoms before taking this medication.
- are taking methadone
- have severe liver problems or acute hepatitis
- have severe kidney problems
- are allergic to naltrexone or any of the ingredients in the formulation of it you use or the liquid used to mix the injectable form (diluent). See below for a complete list of ingredients.
What should I tell my doctor before using naltrexone?
Before you receive naltrexone, tell your healthcare provider if you:
- have liver problems
- use or abuse street (illegal) drugs
- have hemophilia or other bleeding problems
- have kidney problems
- have any other medical conditions
- have alcohol dependence and use opioids
What happens if I miss a dose?
If you forget to take your naltrexone tablet, take it as soon as possible. However, if it is almost time for your next dose, skip the missed dose and go back to your regular dosing schedule. Do not take a double dose to make up for a forgotten dose.
If you miss your appointment for your naltrexone injection, schedule another appointment as soon as possible.
What happens if I overdose?
If you take more naltrexone tablets than you should, tell your Doctor or Pharmacist or contact your nearest hospital emergency department immediately.
What should I know about storage and disposal of this medication?
Keep this medication in the container it came in, tightly closed, and out of reach of children. Store it at room temperature and away from excess heat and moisture (not in the bathroom).
It is important to keep all medication out of sight and reach of children as many containers (such as weekly pill minders and those for eye drops, creams, patches, and inhalers) are not child-resistant and young children can open them easily. To protect young children from poisoning, always lock safety caps and immediately place the medication in a safe location – one that is up and away and out of their sight and reach. http://www.upandaway.org
Unneeded medications should be disposed of in special ways to ensure that pets, children, and other people cannot consume them. However, you should not flush this medication down the toilet. Instead, the best way to dispose of your medication is through a medicine take-back program. Talk to your pharmacist or contact your local garbage/recycling department to learn about take-back programs in your community. See the FDA's Safe Disposal of Medicines website (http://goo.gl/c4Rm4p) for more information if you do not have access to a take-back program.
What special dietary instructions should I follow?
Unless your doctor tells you otherwise, continue your normal diet.
What should I avoid while using Naltrexone?
Do not drive a car, operate machinery, or do other dangerous activities until you know how this medication affects you. Naltrexone may make you feel dizzy and sleepy.
Naltrexone side effects
Serious side effects of naltrexone include:
- See 'Important information' above
- Depressed mood. Sometimes this leads to suicide, or suicidal thoughts, and suicidal behavior. Tell your family members and people closest to you that you are taking this medication.
You, a family member, or the people closest to you should call your healthcare provider right away if you become depressed or have any of the following symptoms of depression, especially if they are new, worse, or worry you:- You feel sad or have crying spells.
- You are no longer interested in seeing your friends or doing things you used to enjoy.
- You are sleeping a lot more or a lot less than usual.
- You feel hopeless or helpless.
- You are more irritable, angry, or aggressive than usual.
- You are more or less hungry than usual or notice a big change in your body weight.
- You have trouble paying attention.
- You feel tired or sleepy all the time.
- You have thoughts about hurting yourself or ending your life.
- You have hallucinations.
- Pneumonia. Some people receiving this treatment have had a certain type of pneumonia that is caused by an allergic reaction. If this happens to you, you may need to be treated in the hospital. Tell your healthcare provider right away if you have any of these symptoms during treatment with naltrexone:
- shortness of breath or wheezing
- coughing that does not go away
- Serious allergic reactions. Serious allergic reactions can happen during or soon after an injection of naltrexone. Tell your healthcare provider or get medical help right away if you have any of these symptoms of a serious allergic reaction.
- skin rash
- swelling of your face, eyes, mouth, or tongue
- trouble breathing or wheezing
- chest pain
- feeling dizzy or faint
Common side effects of naltrexone include:
- nausea. Nausea may happen when you first start this medication, but it can improve overtime.
- vomiting
- sleepiness
- anxiety
- headache
- restlessness
- nervousness
- abdominal pain
- painful joints
- muscle pain and muscle cramps
- weakness
- decreased appetite
- heart palpitations
- increased heart rate
- ECG changes
- libido disorders
- thirst
- dizziness
- increase tear secretion
- chest pain
- diarrhea
- constipation
- rash
- delayed ejaculation and erectile dysfunction
- increased energy
- irritability
- increased sweating
- affective disorders
- cold symptoms
- trouble sleeping
- toothache
Tell your healthcare provider if you have any side effect that bothers you or that does not go away.
These are not all the side effects of this medication. For more information, ask your healthcare provider or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088.
See more: Naltrexone Side EffectsWhat other drugs will affect Naltrexone?
Tell your healthcare provider about all the medicines you take, including prescription and non-prescription medicines, vitamins, and herbal supplements.
Especially tell your healthcare provider if you take any opioid-containing medicines for pain, cough or colds, or diarrhea.
If you are being treated for alcohol dependence but also use or are addicted to opioid-containing medicines or opioid street drugs, it is important that you tell your healthcare provider before starting naltrexone to avoid having sudden opioid withdrawal symptoms when you start treatment.
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist when you get a new medicine.
What other information should I know?
Before having any laboratory tests, tell your doctor and the laboratory personnel that you are taking naltrexone.
Ask your doctor or pharmacist any questions you have about naltrexone.
It is important for you to keep a written list of all of the prescription and nonprescription (over-the-counter) medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.