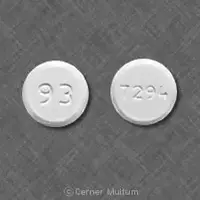
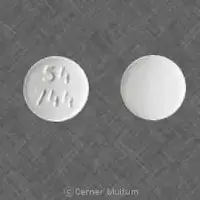
Generic name: lamisil
Availability: Prescription only
Pregnancy & Lactation: Risk data available
Brand names: Lamisil, Terbinafine
What is Terbinafine (systemic) (monograph)?
Introduction
Antifungal; synthetic allylamine structurally and pharmacologically related to naftifine.
Uses for Terbinafine (Systemic)
Onychomycosis
Treatment of dermatophyte infections of the toenail or fingernail (onychomycosis, tinea unguium) caused by susceptible fungi.
Has been effective in treatment of nail infections caused by most strains of Trichophyton rubrum and T. mentagrophytes. Although usually active in vitro against Epidermophyton floccosum, Candida albicans, and Scopulariopsis brevicaulis, efficacy in treatment of onychomycosis caused by these organisms has not been established in adequate and controlled studies.
Terbinafine may be particularly useful in patients who cannot tolerate azole antifungals (e.g., itraconazole) or when there are concerns regarding possible drug interactions between azoles and other drugs the patient is receiving. However, liver failure (sometimes leading to death or liver transplant) has occurred rarely in patients with or without preexisting liver disease who were receiving oral terbinafine for treatment of onychomycosis. (See Hepatotoxicity under Cautions.)
Tinea Capitis
Treatment of tinea capitis (scalp ringworm) caused by susceptible dermatophytes (e.g., Trichophyton, Microsporum).
Tinea capitis requires treatment with an oral antifungal. Topical therapies (e.g., shampoos containing selenium sulfide, povidone iodine, or ketoconazole; topical antifungals) sometimes used as adjuncts to an oral antifungal and may reduce fungal shedding and the risk of transmission or reinfection.
Oral griseofulvin is usual drug of choice; alternatives include oral fluconazole, itraconazole, or terbinafine.
Oral terbinafine appears to be as effective as oral griseofulvin for treatment of tinea capitis caused by Trichophyton, and requires a shorter duration of treatment which may increase compliance. However, there is some evidence that griseofulvin may be more effective than terbinafine when M. canis is the causative agent.
Tinea Corporis or Tinea Cruris
Treatment of tinea corporis† [off-label] (body ringworm) or tinea cruris† [off-label] (jock itch).
Topical antifungals usually are effective for treatment of uncomplicated tinea corporis. An oral antifungal (griseofulvin, fluconazole, itraconazole, terbinafine) may be necessary if tinea corporis is extensive, dermatophyte folliculitis is present, the infection does not respond to topical therapy, or the patient is immunocompromised because of coexisting disease or concomitant therapy.
Terbinafine (Systemic) Dosage and Administration
Administration
Oral Administration
Administer orally.
Take oral granules with food. Sprinkle contents of single-dose packet on a spoonful of pudding or other soft, non-acidic food (e.g., mashed potatoes); do not use applesauce or fruit-based food. Swallow entire spoonful (without chewing). If dosage requires 2 packets for each dose, sprinkle contents of both packets on a single spoonful of nonacidic food or sprinkle contents of the packets on 2 spoonfuls of nonacidic food.
Dosage
Available as terbinafine hydrochloride; dosage expressed in terms of terbinafine.
Pediatric Patients
Tinea Capitis
Oral
Granules in children ≥4 years of age: 125–250 mg once daily for 6 weeks. Use 125 mg once daily in those weighing <25 kg, 187.5 mg once daily in those weighing 25–35 kg, and 250 mg once daily in those weighing >35 kg.
Some evidence that a longer duration of treatment (e.g., 6–8 weeks) or higher dosage may be necessary when tinea capitis is caused by M. canis.
Adults
Onychomycosis
Fingernails
OralTablets: 250 mg daily given for 6 weeks. More prolonged treatment generally has not been more effective, although some patients may benefit from extended and/or repeated courses of terbinafine.
Fingernail infections usually are reevaluated ≥18 weeks after completion of treatment.
Toenails
OralTablets: 250 mg daily given for 12 weeks. Some patients who do not respond to the initial 12-week regimen may respond to a second course.
Toenail infections usually are reevaluated 6–9 months after completion of therapy.
Tinea Capitis
Oral
Granules: 125–250 mg once daily for 6 weeks. Use 187.5 mg once daily in those weighing 25–35 kg and 250 mg once daily in those weighing >35 kg.
Some evidence that a longer duration of treatment (e.g., 6–8 weeks) or higher dosage may be necessary when tinea capitis is caused by M. canis.
Tinea Corporis† [off-label] or Tinea Cruris† [off-label]
Oral
Tablets: 250 mg daily for 2–4 weeks has been used.
Special Populations
Hepatic Impairment
Not recommended in patients with preexisting liver disease (e.g., cirrhosis). (See Hepatic Impairment under Cautions.)
Renal Impairment
Not recommended in patients with renal impairment (i.e., Clcr ≤50 mL/minute) (See Renal Impairment under Cautions.)
Warnings
Contraindications
-
Hypersensitivity to terbinafine or any ingredient in the formulation.
Warnings/Precautions
Warnings
Hepatotoxicity
Hepatotoxicity, including abnormal liver function tests and severe cholestatic hepatitis, reported in some patients receiving oral terbinafine.
Liver failure, sometimes leading to death or liver transplant, occurred rarely in patients with or without preexisting liver disease receiving oral terbinafine for treatment of onychomycosis. Most patients had serious underlying systemic conditions; severity and outcome of hepatotoxicity may be worse in patients with active or chronic liver disease.
Not recommended in patients with chronic or active liver disease.
Assess hepatic function (serum AST and ALT) prior to initiation of oral terbinafine.
Discontinue terbinafine if there is biochemical or clinical evidence of liver injury, including increased ALT or AST concentrations, persistent nausea, anorexia, fatigue, vomiting, right upper abdominal pain or jaundice, dark urine, or pale stools.
Hematologic Effects
Transient decrease in absolute lymphocyte count (ALC) reported; clinical importance unknown. Severe neutropenia reported rarely; resolved with or without supportive therapy when terbinafine was discontinued.
Thrombocytopenia, agranulocytosis, pancytopenia, and anemia reported during postmarketing surveillance; causal relationship not established.
In patients with suspected immunodeficiency, consider monitoring CBCs if oral terbinafine is continued for >6 weeks.
If clinical signs and symptoms suggest secondary infection, perform CBC. If neutrophil count is ≤1000/mm3, discontinue terbinafine and initiate supportive therapy.
Dermatologic Effects
Serious skin reactions (e.g., Stevens-Johnson syndrome, toxic epidermal necrolysis) reported rarely.
Psoriasiform eruptions or exacerbation of psoriasis and acute, generalized exanthematous pustulosis reported.
If progressive rash occurs, discontinue terbinafine.
Lupus Erythematosus
Precipitation and exacerbation of cutaneous and systemic lupus erythematosus reported.
If patient develops clinical signs and symptoms suggestive of lupus erythematosus, discontinue terbinafine.
Sensitivity Reactions
Hypersensitivity Reactions
Angioedema and allergic reactions, including anaphylaxis, reported rarely.
General Precautions
Ocular Effects
Visual disturbances, including changes in ocular lens and retina, reported following use of oral terbinafine tablets for treatment of onychomycosis in adults; clinical importance unknown.
Although no ophthalmologic safety signal was identified in clinical trials using terbinafine oral granules, there were some reports of changes in visual acuity and some reports of color confusion in yellow-blue color vision assessments.
GI Effects
Taste disturbances (including taste loss) may occur. Usually resolves within several weeks after terbinafine is discontinued, but prolonged (>1 year) taste disturbance has been reported. May be severe enough to result in decreased food intake leading to substantial and unwanted weight loss.
Selection and Use of Antifungals for Onychomycosis
Prior to administration of oral terbinafine for treatment of onychomycosis, appropriate nail specimens for microbiologic studies (e.g., potassium hydroxide [KOH] preparation, fungal culture, or nail biopsy) should be obtained to confirm the diagnosis.
When selecting an antifungal for treatment of onychomycosis, consider reported adverse effects and risk of serious effects, need for prolonged therapy, cost, and risk of relapse.
Toenail infections generally require more prolonged antifungal therapy than fingernail infections.
The optimal clinical effect of terbinafine in treatment of onychomycosis is not seen until several months after mycologic cure and completion of treatment, and is related to the period required for outgrowth of healthy nail.
Possible Prescribing and Dispensing Errors
Ensure accuracy of prescription; similarity in spelling of lamotrigine (Lamictal) and terbinafine (Lamisil) may result in errors.
Specific Populations
Pregnancy
Category B.
Postpone use of oral terbinafine until after pregnancy is completed.
Lactation
Distributed into milk. Use not recommended.
Pediatric Use
Safety and efficacy of terbinafine tablets not established in children <18 years of age.
Safety and efficacy of terbinafine oral granules not established in children <4 years of age.
Geriatric Use
Terbinafine oral granules not studied in geriatric patients.
Hepatic Impairment
Clearance may be decreased substantially (about 50%) in adults with hepatic cirrhosis.
Not recommended in patients with chronic or active liver disease. (See Hepatotoxicity under Cautions.)
Renal Impairment
Clearance may be decreased substantially (about 50%) in adults with renal impairment (Clcr ≤50 mL/minute).
Not adequately studied in patients with Clcr ≤50 mL/minute; use in such patients not recommended.
Common Adverse Effects
GI effects (diarrhea, dyspepsia, nausea, vomiting, abdominal pain, taste disturbances), headache, fever, upper respiratory tract infection or symptoms (cough, nasopharyngitis, nasal congestion, pharyngolaryngeal pain, influenza), liver test abnormalities, dermatologic effects (rash, urticaria, pruritus).
How should I use Terbinafine (systemic) (monograph)
Administration
Oral Administration
Administer orally.
Take oral granules with food. Sprinkle contents of single-dose packet on a spoonful of pudding or other soft, non-acidic food (e.g., mashed potatoes); do not use applesauce or fruit-based food. Swallow entire spoonful (without chewing). If dosage requires 2 packets for each dose, sprinkle contents of both packets on a single spoonful of nonacidic food or sprinkle contents of the packets on 2 spoonfuls of nonacidic food.
Dosage
Available as terbinafine hydrochloride; dosage expressed in terms of terbinafine.
Pediatric Patients
Tinea Capitis
Oral
Granules in children ≥4 years of age: 125–250 mg once daily for 6 weeks. Use 125 mg once daily in those weighing <25 kg, 187.5 mg once daily in those weighing 25–35 kg, and 250 mg once daily in those weighing >35 kg.
Some evidence that a longer duration of treatment (e.g., 6–8 weeks) or higher dosage may be necessary when tinea capitis is caused by M. canis.
Adults
Onychomycosis
Fingernails
OralTablets: 250 mg daily given for 6 weeks. More prolonged treatment generally has not been more effective, although some patients may benefit from extended and/or repeated courses of terbinafine.
Fingernail infections usually are reevaluated ≥18 weeks after completion of treatment.
Toenails
OralTablets: 250 mg daily given for 12 weeks. Some patients who do not respond to the initial 12-week regimen may respond to a second course.
Toenail infections usually are reevaluated 6–9 months after completion of therapy.
Tinea Capitis
Oral
Granules: 125–250 mg once daily for 6 weeks. Use 187.5 mg once daily in those weighing 25–35 kg and 250 mg once daily in those weighing >35 kg.
Some evidence that a longer duration of treatment (e.g., 6–8 weeks) or higher dosage may be necessary when tinea capitis is caused by M. canis.
Tinea Corporis† [off-label] or Tinea Cruris† [off-label]
Oral
Tablets: 250 mg daily for 2–4 weeks has been used.
Special Populations
Hepatic Impairment
Not recommended in patients with preexisting liver disease (e.g., cirrhosis). (See Hepatic Impairment under Cautions.)
Renal Impairment
Not recommended in patients with renal impairment (i.e., Clcr ≤50 mL/minute) (See Renal Impairment under Cautions.)
What other drugs will affect Terbinafine (systemic) (monograph)?
Inhibits CYP2D6.
Drugs Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interactions possible with drugs that are substrates for CYP2D6 (e.g., tricyclic antidepressants, β-blockers, selective serotonin reuptake inhibitors [SSRIs], monoamine oxidase [MAO] inhibitors); may be clinically important if the drug has a narrow therapeutic window. Monitor carefully if terbinafine is used concomitantly with such drugs; dosage of the drug metabolized by CYP2D6 may need to be reduced.
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Antiarrhythmic agents (amiodarone, flecainide, propafenone) |
Potential increased antiarrhythmic concentrations Amiodarone: Possibility of substantially increased terbinafine concentrations and AUC |
Monitor carefully; reduced dosage of antiarrhythmic may be required |
|
Antidepressants |
Concomitant use of terbinafine and antidepressants metabolized by CYP2D6 (e.g., tricyclics, SSRIs, MAO inhibitors) may result in increased concentrations of the antidepressant Desipramine: Increased concentration and AUC of desipramine; effect may persist ≥4 weeks after discontinuance of terbinafine |
Monitor carefully; reduced dosage of tricyclic, SSRI, or MAO inhibitor antidepressant may be required |
|
Antifungals, azoles |
Fluconazole: Substantially increased terbinafine concentrations and AUC; effect on fluconazole pharmacokinetics not considered clinically important Ketoconazole: Possibility of substantially increased terbinafine concentrations and AUC |
|
|
Benzodiazepines |
Midazolam: Terbinafine does not affect midazolam pharmacokinetics Triazolam: Terbinafine does not have a clinically important effect on triazolam pharmacokinetics |
|
|
Caffeine |
Decreased clearance of caffeine |
|
|
Cimetidine |
Decreased clearance of terbinafine |
|
|
Cyclosporine |
Increased clearance of cyclosporine; no effect on terbinafine clearance |
|
|
Dextromethorphan |
Increased dextromethorphan/dextromethorphan metabolite ratio in urine |
|
|
Digoxin |
No effect on digoxin clearance |
|
|
Rifampin |
Substantially increased terbinafine clearance |
|
|
Sulfamethoxazole |
No clinically important effect on sulfamethoxazole pharmacokinetics |
|
|
Theophylline |
No clinically important effect on theophylline pharmacokinetics |
|
|
Trimethoprim |
No clinically important effect on trimethoprim pharmacokinetics |
|
|
Warfarin |
Increase or decrease in PT reported; causal relationship not established |
|
|
Zidovudine |
No clinically important effect on zidovudine pharmacokinetics |