- Attention deficit hyperactivity disorder (ADHD) is a developmental condition that may make it harder for people to stay focused and make impulsive behaviors more likely.
- Some people with ADHD may benefit from taking medications that help with such behaviors.
- However, research is ongoing about these medications’ potential risks and benefits.
- A recent study found that people taking ADHD medication long-term may be more at risk for cardiovascular disease.
ADHD is a neurodevelopmental disorder that can interfere with everyday life. People with ADHD may take certain medications to help with work and school performance and ultimately improve their quality of life.
A new
In their data collection from over 278,000 participants, the researchers found that individuals taking ADHD medication are at a higher risk for cardiovascular disease, particularly hypertension and arterial disease.
The study points to the critical need for physicians to carefully weigh the potential risks and benefits of people taking ADHD medications to help control specific symptoms.
The CDC estimates that
ADHD can involve several
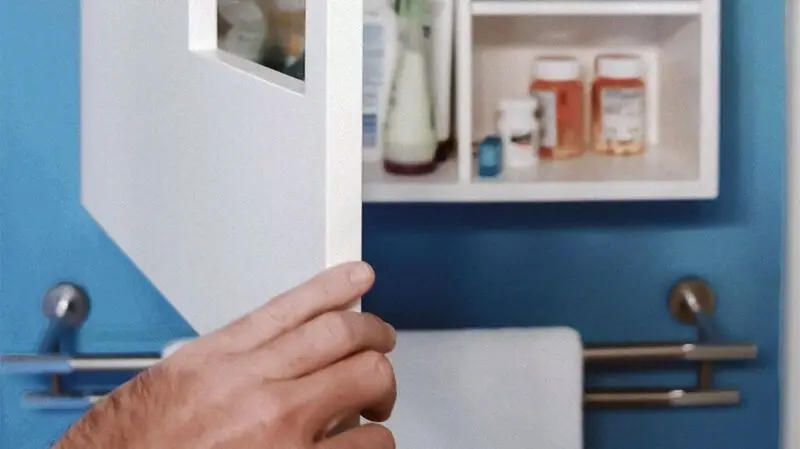
Treatment for ADHD can involve the use of certain medications that can help improve some behaviors and symptoms. Common medications include stimulants and non-stimulants. Sometimes, someone with ADHD may be on more than one medication to help with ADHD symptoms.
Researchers in the current study wrote that “[p]harmacological therapy, including both stimulants and nonstimulants, is recommended as the first-line treatment for ADHD in many countries. The use of ADHD medication has increased greatly in both children and adults during the past decades.”
Research is ongoing about the potential long-term effects of ADHD medication use. Gathering more data in this area can help doctors make informed decisions when prescribing ADHD medications.
This case-control study was conducted in Sweden. Researchers included 278,027 participants. Participants were ages 6–64 and had either received an ADHD diagnosis or were taking ADHD medication.
They looked at the timeframe of ADHD medication use, up to 14 years, and the incidence of several cardiovascular diseases, such as abnormal heart rhythms, heart failure, high blood pressure, and arterial disease. The researchers collected data via the National Inpatient Register, which records diagnoses, and the Swedish Prescribed Drug Register, which records data on dispensed medications.
In their analysis, they found that individuals taking ADHD medication were at a higher risk for cardiovascular disease, particularly within the first three cumulative years of taking ADHD medication.
After this, the associated risk remained more stable. Researchers found similar results among men and women and among children and adults.
Researchers further found that participants taking ADHD medication were particularly at risk for high blood pressure and arterial disease. However, the risk related to several other cardiovascular diseases was not statistically significant.
Dr. Keith C. Ferdinand, professor of medicine at the Tulane University School of Medicine, who was not involved in the study, noted to Medical News Today:
“This well-done, long term study did not did not observe any statistically significant increased risk for arrhythmias, heart failure, ischemic heart disease, thromboembolic disease, or cerebrovascular disease and should inform the public that these life threatening conditions were not clearly revealed as a driver of risks. Hence, it is reasonable to understand the real possibility of increased risk of hypertension and arterial disease, especially associated with stimulant medication use without suggesting that all ADHD medications, even used briefly, should always be avoided.”
Stimulant vs. non-stimulant medication for ADHD
The results also suggest that the risk for cardiovascular disease may be higher when taking stimulants rather than non-stimulants. The research points to the importance of weighing the risks and benefits of taking ADHD medication long-term.
Study authors Dr. Le Zhang and Dr. Zheng Chang explained to MNT:
“This longitudinal observational study found long-term exposure to ADHD medications was associated with an increased risk of CVDs [cardiovascular diseases], especially hypertension and arterial disease.”
“Clinicians should be vigilant in monitoring signs and symptoms of cardiovascular diseases, particularly among those receiving higher doses [of ADHD medications]. Treatment decisions, as always, should be based on careful[ly] weighing potential benefits and risks at individual patient level, rather than simple one-size-fits-all recommendations.”
— Study authors Dr. Le Zhang and Dr. Zheng Chang
This research does have certain limitations. First, it cannot prove that ADHD medication causes any cardiovascular disease problems.
It also only included individuals from one country, which could indicate the need for more diverse studies in the future. Future research can also have larger sample sizes.
Researchers note that there’s the possibility that there could have been some cases of cardiovascular disease that doctors had not diagnosed. They also note that there could have been exposure misclassification if participants did not take their medications the way medical professionals prescribed.
There is also the possibility of residual confounding, and results could have been affected by time-varying confounders. The research also did not look at the risk for cardiovascular disease among individuals who already had cardiovascular disease.
Study authors Dr. Le Zhang and Dr. Zheng Chang explained some components of future research to MNT:
“The current study did not examine the risk of CVD among individuals with pre-existing CVD. Further research needs to be done to examine the potential risks among individuals with pre-existing CVD. Individuals with pre-existing CVD represent a distinct clinical group that requires careful monitoring; thus, evaluating the risk among them necessitates a different study design that carefully considers the potential impact of prior knowledge and periodic monitoring.”





