Drug Detail:Boniva (Ibandronate (oral/injection) [ eye-ban-dro-nate ])
Drug Class: Bisphosphonates
Highlights of Prescribing Information
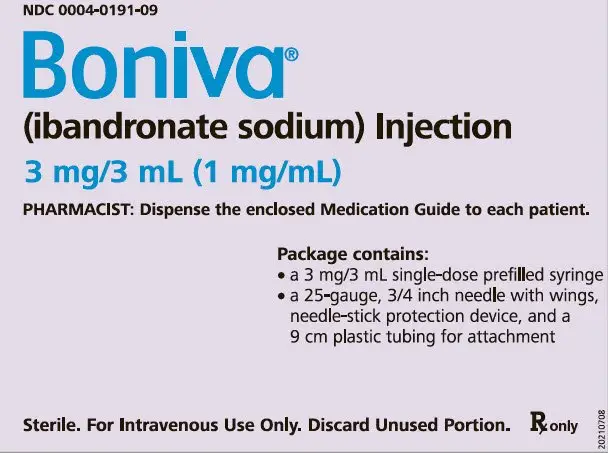
BONIVA ® (ibandronate sodium) Injection, for intravenous use
Initial U.S. Approval: 2003
Indications and Usage for Boniva
BONIVA Injection is a bisphosphonate indicated for the treatment of osteoporosis in postmenopausal women. (1.1)
Limitations of Use
Optimal duration of use has not been determined. For patients at low-risk for fracture, consider drug discontinuation after 3 to 5 years of use (1.2)
Boniva Dosage and Administration
- 3 mg every 3 months administered intravenously over a period of 15 to 30 seconds (2.2)
- Dosing Instructions:
- Only administer intravenously by a health care professional. (2.1)
- Do not mix with calcium-containing solutions or other intravenously administered drugs. (2.1)
- Do not administer more frequently than once every 3 months. (2.2)
- Instruct patients to take supplemental calcium and vitamin D if dietary intake is inadequate
Dosage Forms and Strengths
BONIVA Injection is supplied as a kit containing:
- a 3 mg/3 mL (1mg/mL) single-dose prefilled syringe
- a 25-gauge, 3/4 inch needle with wings, needle-stick protection device, and a 9 cm plastic tubing for attachment (3)
Contraindications
- Hypocalcemia (4)
- Hypersensitivity to BONIVA Injection (4)
Warnings and Precautions
-
Hypocalcemia can worsen. Correct hypocalcemia prior to use.
Adequately supplement patients with calcium and vitamin D (5.1) - Anaphylaxis, including fatal events, has been reported. (5.2)
- Renal Toxicity may be greater in patients with underlying renal impairment. Do not administer BONIVA injection to patients with severe renal impairment (creatinine clearance less than 30 mL/min). Monitor serum creatinine prior to each dose. (5.3)
- Tissue Damage with Inappropriate Drug Administration can occur. Do not administer BONIVA Injection intra-arterially or paravenously. (5.4)
- Osteonecrosis of the jaw (ONJ) has been reported. (5.5)
- Severe Bone, Joint, and/or Muscle Pain may occur, consider discontinuing use if symptoms occur. (5.6)
- Atypical Femur Fractures have been reported. Patients with new thigh or groin pain should be evaluated to rule out a femoral fracture. (5.7)
Adverse Reactions/Side Effects
The most frequently reported adverse reactions (>5%) are arthralgia, back pain, and abdominal pain. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Genentech at 1-888-835-2555 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 1/2022
Related/similar drugs
hydrochlorothiazide, alendronate, estradiol, Prolia, Fosamax, calcium carbonate, ReclastFull Prescribing Information
1. Indications and Usage for Boniva
1.1 Treatment of Postmenopausal Osteoporosis
BONIVA Injection is indicated for the treatment of osteoporosis in postmenopausal women. In postmenopausal women with osteoporosis, BONIVA increases bone mineral density (BMD) and reduces the incidence of vertebral fractures [see Clinical Studies (14)].
1.2 Important Limitations of Use
The safety and effectiveness of BONIVA for the treatment of osteoporosis are based on clinical data of one year duration. The optimal duration of use has not been determined. All patients on bisphosphonate therapy should have the need for continued therapy re-evaluated on a periodic basis. Patients at low-risk for fracture should be considered for drug discontinuation after 3 to 5 years of use. Patients who discontinue therapy should have their risk for fracture re-evaluated periodically.
2. Boniva Dosage and Administration
2.1 Important Administration Instructions
BONIVA Injection must be administered intravenously only by a health care professional. Care must be taken not to administer intra-arterially or paravenously as this could lead to tissue damage [see Warnings and Precautions (5.4)].
- Appropriate medical support and monitoring measures should be readily available when BONIVA Injection is administered. If anaphylactic or other severe hypersensitivity/allergic reactions occur, immediately discontinue the injection and initiate appropriate treatment [see Warnings and Precautions (5.2)].
- Visually inspect the liquid in the prefilled syringe for particulate matter and discoloration before administration. Do not use prefilled syringes with particulate matter or discoloration.
- Administer only with the enclosed needle.
- Discard any unused portion.
- Do not mix with calcium-containing solutions or other intravenously administered drugs.
- Prefilled syringes are single-dose only.
2.2 Dosage Information
The recommended dose of BONIVA Injection for the treatment of postmenopausal osteoporosis is 3 mg every 3 months administered intravenously over a period of 15 to 30 seconds. Do not administer more frequently than once every 3 months.
2.3 Laboratory Testing and Oral Examination Prior to Administration
Prior to administration of each dose obtain a serum creatinine [see Warnings and Precautions (5.3)]. Given that bisphosphonates have been associated with osteonecrosis of the jaw (ONJ), perform a routine oral examination prior to administration of BONIVA Injection.
2.4 Calcium and Vitamin D Supplementation
Instruct patients to take supplemental calcium and vitamin D if their dietary intake is inadequate [see Warnings and Precautions (5.1)].
2.5 Dosing After Missed Dose
If the dose is missed, administer as soon as it can be re-scheduled. Thereafter, BONIVA Injection should be scheduled every 3 months from the date of the last injection.
2.6 Dosage Modifications in Patients with Renal Impairment
Do not administer to patients with severe renal impairment (creatinine clearance less than 30 mL/minute) [see Warnings and Precautions (5.3) and Clinical Pharmacology (12.3)]. No dose adjustment is necessary for patients with mild or moderate renal impairment (creatinine clearance greater than or equal to 30 mL/min) [see Clinical Pharmacology (12.3)].
3. Dosage Forms and Strengths
BONIVA Injection is supplied as a kit containing:
- a 3 mg/3 mL (1 mg/mL) single-dose prefilled syringe
- a 25-gauge, 3/4 inch needle with wings, needle-stick protection device, and a 9 cm plastic tubing for attachment
4. Contraindications
Boniva is contraindicated in patients with the following conditions:
- Hypocalcemia [see Warnings and Precautions (5.1)]
- Known hypersensitivity to BONIVA Injection or to any of its excipients. Cases of anaphylaxis, including fatal events, have been reported. [see Warnings and Precautions (5.2), Adverse Reactions (6.2)]
5. Warnings and Precautions
5.1 Hypocalcemia and Mineral Metabolism
BONIVA Injection may cause a decrease in serum calcium values. Treat hypocalcemia, hypovitaminosis D, and other disturbances of bone and mineral metabolism before starting BONIVA Injection therapy.
Adequate intake of calcium and vitamin D is important in all patients. It is recommended that patients receive supplemental calcium and vitamin D if dietary intake is inadequate.
5.2 Anaphylactic Reaction
Cases of anaphylaxis, including fatal events, have been reported in patients treated with BONIVA Injection.
Appropriate medical support and monitoring measures should be readily available when BONIVA Injection is administered. If anaphylactic or other severe hypersensitivity/allergic reactions occur, immediately discontinue the injection and initiate appropriate treatment.
5.3 Renal Impairment
Treatment with intravenous bisphosphonates has been associated with renal toxicity manifested as deterioration in renal function and acute renal failure. Although no cases of acute renal failure were observed in controlled clinical trials in which intravenous BONIVA was administered as a 15- to 30-second bolus, acute renal failure has been reported postmarketing. Do not administer BONIVA Injection to patients with severe renal impairment (creatinine clearance less than 30 mL/min).
Obtain serum creatinine prior to each BONIVA Injection. After BONIVA Injection, assess renal function, as clinically appropriate, in patients with concomitant diseases or taking medications that have the potential for adverse effects on the kidney. BONIVA Injection should be withheld in patients with renal deterioration.
5.4 Tissue Damage Related to Inappropriate Drug Administration
BONIVA Injection must only be administered intravenously. Care must be taken not to administer BONIVA Injection intra-arterially or paravenously as this could lead to tissue damage.
Do not administer BONIVA Injection by any other route of administration. The safety and efficacy of BONIVA Injection following non-intravenous routes of administration have not been established.
5.5 Osteonecrosis of the Jaw
Osteonecrosis of the jaw (ONJ) has been reported in patients treated with bisphosphonates, including BONIVA Injection. Most cases have been in cancer patients treated with intravenous bisphosphonates undergoing dental procedures. Some cases have occurred in patients with postmenopausal osteoporosis treated with either oral or intravenous bisphosphonates. A routine oral examination should be performed by the prescriber prior to initiation of bisphosphonate treatment. Consider a dental examination with appropriate preventive dentistry prior to treatment with bisphosphonates in patients with a history of concomitant risk factors (e.g., cancer, chemotherapy, angiogenesis inhibitors, radiotherapy, corticosteroids, poor oral hygiene, pre-existing dental disease or infection, anemia, coagulopathy). Concomitant administration of drugs associated with ONJ may increase the risk of developing ONJ. The risk of ONJ may increase with duration of exposure to bisphosphonates.
While on treatment, patients with concomitant risk factors should avoid invasive dental procedures if possible. For patients who develop ONJ while on bisphosphonate therapy, dental surgery may exacerbate the condition. For patients requiring dental procedures, there are no data available to suggest whether discontinuation of bisphosphonate treatment reduces the risk of ONJ. The clinical judgment of the treating physician should guide the management plan of each patient based on individual benefit/risk assessment [see Adverse Reactions (6.1)].
5.6 Musculoskeletal Pain
Severe and occasionally incapacitating bone, joint, and/or muscle pain has been reported in patients taking BONIVA and other bisphosphonates [see Adverse Reactions (6.2)]. The time to onset of symptoms varied from one day to several months after starting the drug. Most patients had relief of symptoms after stopping the bisphosphonate. A subset of patients had recurrence of symptoms when rechallenged with the same drug or another bisphosphonate. Discontinue BONIVA if severe symptoms develop.
5.7 Atypical Subtrochanteric and Diaphyseal Femoral Fractures
Atypical, low-energy, or low-trauma fractures of the femoral shaft have been reported in bisphosphonate-treated patients. These fractures can occur anywhere in the femoral shaft from just below the lesser trochanter to above the supracondylar flare and are transverse or short oblique in orientation without evidence of comminution. Causality has not been established as these fractures also occur in osteoporotic patients who have not been treated with bisphosphonates.
Atypical femur fractures most commonly occur with minimal or no trauma to the affected area. They may be bilateral and many patients report prodromal pain in the affected area, usually presenting as dull, aching thigh pain, weeks to months before a complete fracture occurs. A number of reports note that patients were also receiving treatment with glucocorticoids (e.g., prednisone) at the time of fracture.
Any patient with a history of bisphosphonate exposure who presents with thigh or groin pain should be suspected of having an atypical fracture and should be evaluated to rule out an incomplete femur fracture. Patients presenting with an atypical fracture should also be assessed for symptoms and signs of fracture in the contralateral limb. Interruption of bisphosphonate therapy should be considered, pending a risk/benefit assessment, on an individual basis.
6. Adverse Reactions/Side Effects
Adverse reactions that appear in other sections of the labeling include:
- Hypocalcemia and Mineral Metabolism [see Warnings and Precautions (5.1)]
- Anaphylactic Reaction [see Warnings and Precautions (5.2)]
- Renal Impairment [see Warnings and Precautions (5.3)]
- Tissue Damage Related to Inappropriate Drug Administration [see Warnings and Precautions (5.4)]
- Osteonecrosis of the Jaw [see Warnings and Precautions (5.5)]
- Musculoskeletal Pain [see Warnings and Precautions (5.6)]
- Atypical Subtrochanteric and Diaphyseal Femoral Fractures [see Warnings and Precautions (5.7)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Quarterly Intravenous Injection –
In a 1-year, double-blind, multicenter study comparing BONIVA Injection administered intravenously as 3 mg every 3 months to BONIVA 2.5 mg daily oral tablet in women with postmenopausal osteoporosis, the overall safety and tolerability profiles of the two dosing regimens were similar. The incidence of serious adverse reactions was 8.0% in the BONIVA 2.5 mg daily group and 7.5% in the BONIVA Injection 3 mg once every 3 months group. The percentage of patients who withdrew from treatment due to adverse reactions was approximately 6.7% in the BONIVA 2.5 mg daily group and 8.5% in the BONIVA Injection 3 mg every 3 months group. Table 1 lists the adverse reactions reported in greater than 2% of patients.
| Body System/Adverse Reaction | BONIVA 2.5 mg Daily (Oral) % (n=465) | BONIVA 3 mg every 3 months (Intravenous) % (n=469) |
|---|---|---|
|
||
| Infections and Infestations | ||
| Influenza | 8 | 5 |
| Nasopharyngitis | 6 | 3 |
| Cystitis | 3 | 2 |
| Gastroenteritis | 3 | 2 |
| Urinary Tract Infection | 3 | 3 |
| Bronchitis | 3 | 2 |
| Upper Respiratory Tract Infection | 3 | 1 |
| Gastrointestinal Disorders | ||
| Abdominal Pain* | 6 | 5 |
| Dyspepsia | 4 | 4 |
| Nausea | 4 | 2 |
| Constipation | 4 | 3 |
| Diarrhea | 2 | 3 |
| Gastritis | 2 | 2 |
| Musculoskeletal and Connective Tissue Disorders | ||
| Arthralgia | 9 | 10 |
| Back Pain | 8 | 7 |
| Localized Osteoarthritis | 2 | 2 |
| Pain in Extremity | 2 | 3 |
| Myalgia | 1 | 3 |
| Nervous System Disorders | ||
| Dizziness | 3 | 2 |
| Headache | 3 | 4 |
| Psychiatric Disorders | ||
| Insomnia | 3 | 1 |
| Depression | 2 | 1 |
| General Disorders and Administration Site Conditions | ||
| Influenza-like Illness† | 1 | 5 |
| Fatigue | 1 | 3 |
| Skin and Subcutaneous Tissue Disorders | ||
| Rash‡ | 3 | 2 |
Daily Oral Tablet -
The safety of BONIVA 2.5 mg once daily in the treatment and prevention of postmenopausal osteoporosis was assessed in 3577 patients aged 41 – 82 years. The duration of the trials was 2 to 3 years, with 1134 patients exposed to placebo and 1140 exposed to BONIVA 2.5 mg. Patients with pre-existing gastrointestinal disease and concomitant use of non-steroidal anti-inflammatory drugs, proton pump inhibitors and H2 antagonists were included in these clinical trials. All patients received 500 mg calcium plus 400 international units vitamin D supplementation daily.
The incidence of all-cause mortality was 1% in the placebo group and 1.2% in the BONIVA 2.5 mg daily group. The incidence of serious adverse reactions was 20% in the placebo group and 23% in the BONIVA 2.5 mg daily oral tablet group. The percentage of patients who withdrew from treatment due to adverse reactions was approximately 17% in both the placebo group and the BONIVA 2.5 mg daily oral tablet group. Table 2 lists adverse reactions from the Treatment and Prevention Studies reported in greater than or equal to 2% of patients and in more patients treated with BONIVA 2.5 mg daily oral tablet than patients treated with placebo.
| Body System | Placebo % (n=1134) | BONIVA 2.5 mg daily % (n=1140) |
|---|---|---|
| Body as a Whole | ||
| Back Pain | 12 | 14 |
| Pain in Extremity | 6 | 8 |
| Asthenia | 2 | 4 |
| Allergic Reaction | 2 | 3 |
| Digestive System | ||
| Dyspepsia | 10 | 12 |
| Diarrhea | 5 | 7 |
| Tooth Disorder | 2 | 4 |
| Vomiting | 2 | 3 |
| Gastritis | 2 | 2 |
| Musculoskeletal System | ||
| Myalgia | 5 | 6 |
| Joint Disorder | 3 | 4 |
| Arthritis | 3 | 3 |
| Nervous System | ||
| Headache | 6 | 7 |
| Dizziness | 3 | 4 |
| Vertigo | 3 | 3 |
| Respiratory System | ||
| Upper Respiratory Infection | 33 | 34 |
| Bronchitis | 7 | 10 |
| Pneumonia | 4 | 6 |
| Pharyngitis | 2 | 3 |
| Urogenital System | ||
| Urinary Tract Infection | 4 | 6 |
6.2 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of BONIVA Injection. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Hypersensitivity: Allergic reactions including anaphylaxis with fatalities, angioedema, asthma exacerbation, bronchospasm, rash, Stevens-Johnson syndrome, erythema multiforme, and dermatitis bullous [see Contraindications (4), Warnings and Precautions (5.2)].
Hypocalcemia: Hypocalcemia [see Warnings and Precautions (5.1)].
Renal Toxicity: Acute renal failure [see Warnings and Precautions (5.3)].
Osteonecrosis of the Jaw: Osteonecrosis of the jaw and other oro-facial sites, including the external auditory canal [see Warnings and Precautions (5.5)].
Musculoskeletal Pain: Bone, joint, or muscle pain (musculoskeletal pain), described as severe or incapacitating [see Warnings and Precautions (5.6)].
Atypical Femoral Shaft Fracture: Atypical, low-energy, or low-trauma fractures of the femoral shaft [see Warnings and Precautions (5.7)].
Eye Inflammation: Iritis and uveitis. In some cases with other bisphosphonates, these events did not resolve until the bisphosphonate was discontinued.
7. Drug Interactions
7.1 Melphalan/Prednisolone
Intravenous ibandronate (6 mg) did not interact with intravenous melphalan (10 mg/m2) or oral prednisolone (60 mg/m2). [See Clinical Pharmacology (12.3)]
8. Use In Specific Populations
8.4 Pediatric Use
Safety and effectiveness of BONIVA in pediatric patients have not been established.
8.5 Geriatric Use
Of the patients receiving BONIVA Injection 3 mg every 3 months for 1 year, 51% were over 65 years of age. No overall differences in effectiveness or safety were observed between these patients and younger patients, but greater sensitivity in some older individuals cannot be ruled out.
10. Overdosage
No cases of overdose were reported in premarketing studies with BONIVA Injection. Overdosage with intravenous bisphosphonates may result in hypocalcemia, hypophosphatemia, and hypomagnesemia. Clinically relevant reductions in serum levels of calcium, phosphorus, and magnesium should be corrected by intravenous administration of calcium gluconate, potassium or sodium phosphate, and magnesium sulfate, respectively.
Dialysis would not be beneficial unless it is administered within 2 hours following the overdose.
11. Boniva Description
BONIVA (ibandronate sodium) is a nitrogen-containing bisphosphonate that inhibits osteoclast-mediated bone resorption. The chemical name for ibandronate sodium is 3-(N-methyl-N-pentyl)amino-1-hydroxypropane-1,1-diphosphonic acid, monosodium salt, monohydrate with the molecular formula C9H22NO7P2Na•H2O and a molecular weight of 359.24. Ibandronate sodium is a white- to off-white powder. It is freely soluble in water and practically insoluble in organic solvents. Ibandronate sodium has the following structural formula:
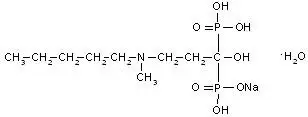
BONIVA Injection is intended for intravenous administration only. BONIVA Injection is available as a sterile, clear, colorless, ready-to-use solution in a prefilled syringe that delivers 3.375 mg of ibandronate monosodium salt monohydrate in 3 mL of solution, equivalent to a dose of 3 mg ibandronate free acid. Inactive ingredients include glacial acetic acid (1.53 mg), sodium acetate trihydrate (0.612 mg), sodium chloride (25.8 mg), and water (2980.683 mg). Glacial acetic acid and sodium acetate trihydrate are used to adjust pH.
12. Boniva - Clinical Pharmacology
12.1 Mechanism of Action
The action of ibandronate on bone is based on its affinity for hydroxyapatite, which is part of the mineral matrix of bone. Ibandronate inhibits osteoclast activity and reduces bone resorption and turnover. In postmenopausal women, it reduces the elevated rate of bone turnover, leading to, on average, a net gain in bone mass.
12.2 Pharmacodynamics
In studies of postmenopausal women, BONIVA Injection at doses of 0.5 mg to 3 mg produced biochemical changes indicative of inhibition of bone resorption, including decreases of biochemical markers of bone collagen degradation (cross-linked C-telopeptide of Type I collagen [CTX]). Changes in markers of bone formation (osteocalcin) were observed later than changes in resorption markers, as expected, due to the coupled nature of bone resorption and formation.
Year 1 results from an efficacy and safety study comparing BONIVA Injection 3 mg every 3 months and BONIVA 2.5 mg daily oral tablet demonstrated that both dosing regimens significantly suppressed serum CTX levels at Months 3, 6, and 12. The median pre-dose or trough serum CTX levels in the intent-to-treat population reached a nadir of 57% (BONIVA Injection) and 62% (BONIVA 2.5 mg tablets) below baseline values by Month 6, and remained stable at Month 12 of treatment.
13. Nonclinical Toxicology
13.2 Animal Pharmacology
Animal studies have shown that ibandronate is an inhibitor of osteoclast-mediated bone resorption. In the Schenk assay in growing rats, ibandronate inhibited bone resorption and increased bone volume, based on histologic examination of the tibial metaphyses. There was no evidence of impaired mineralization at the highest dose of 5 mg/kg/day (subcutaneously), which is 1000 times the lowest antiresorptive dose of 0.005 mg/kg/day in this model, and 5000 times the optimal antiresorptive dose of 0.001 mg/kg/day in the aged ovariectomized rat. This indicates that BONIVA Injection administered at a therapeutic dose is unlikely to induce osteomalacia.
Long-term daily or intermittent administration of ibandronate to ovariectomized rats or monkeys was associated with suppression of bone turnover and increases in bone mass. Vertebral BMD, trabecular density, and biomechanical strength were increased dose-dependently in rats and monkeys, at doses up to 8 to 4 times the human intravenous dose of 3 mg every 3 months, based on cumulative dose normalized for body surface area (mg/m2) and area under the curve (AUC) comparison, respectively. Ibandronate maintained the positive correlation between bone mass and strength at the ulna and femoral neck. New bone formed in the presence of ibandronate had normal histologic structure and did not show mineralization defects.
14. Clinical Studies
14.1 Treatment of Postmenopausal Osteoporosis
Quarterly Intravenous Injection
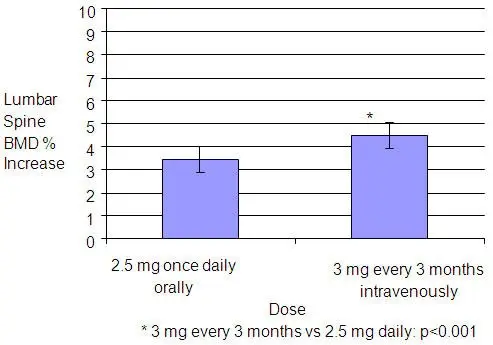
The effectiveness and safety of BONIVA Injection 3 mg once every 3 months were demonstrated in a randomized, double-blind, multinational, noninferiority study in 1358 women with postmenopausal osteoporosis (L2-L4 lumbar spine BMD, T-score below -2.5 SD at baseline). The control group received BONIVA 2.5 mg daily oral tablets. The primary efficacy parameter was the relative change from baseline to 1 year of treatment in lumbar spine BMD, which was compared between the intravenous injection and the daily oral treatment groups. All patients received 400 international units vitamin D and 500 mg calcium supplementation per day.
Daily Oral Tablets
The effectiveness and safety of BONIVA daily oral tablets were demonstrated in a randomized, double-blind, placebo-controlled, multinational study (Treatment Study) of 2946 women aged 55 to 80 years, who were on average 21 years postmenopause, who had a lumbar spine BMD 2 to 5 SD below the premenopausal mean (T-score) in at least one vertebra [L1-L4], and who had one to four prevalent vertebral fractures. BONIVA was evaluated at oral doses of 2.5 mg daily and 20 mg intermittently. The main outcome measure was the occurrence of new radiographically diagnosed, vertebral fractures after 3 years of treatment. The diagnosis of an incident vertebral fracture was based on both qualitative diagnosis by the radiologist and quantitative morphometric criterion. The morphometric criterion required the dual occurrence of two events: a relative height ratio or relative height reduction in a vertebral body of at least 20%, together with at least a 4 mm absolute decrease in height. All women received 400 international units vitamin D and 500 mg calcium supplementation per day.
Effect on Vertebral Fracture
BONIVA 2.5 mg daily oral tablet significantly reduced the incidence of new vertebral fractures compared to placebo. Over the course of the 3-year study, the risk for new vertebral fracture was 9.6% in the placebo-treated women and 4.7% in the women treated with BONIVA 2.5 mg daily oral tablet (p<0.001) (see Table 3).
| Proportion of Patients with Fracture (%) | ||||
|---|---|---|---|---|
| Placebo n=975 | BONIVA 2.5 mg Daily n=977 | Absolute Risk Reduction (%) 95% CI | Relative Risk Reduction (%) 95% CI |
|
|
||||
| New Vertebral Fracture | 9.6 | 4.7 | 4.9 | 52 † |
| 0-3 Year | (2.3, 7.4) | (29, 68) | ||
| New and Worsening Vertebral Fracture‡ | 10.4 | 5.1 | 5.3 | 52 |
| 0-3 Year | (2.6, 7.9) | (30, 67) | ||
| Clinical (Symptomatic) Vertebral Fracture | 5.3 | 2.8 | 2.5 | 49 |
| 0-3 Year | (0.6, 4.5) | (14, 69) | ||
Effect on BMD
BONIVA 2.5 mg daily oral tablet significantly increased BMD at the lumbar spine and hip relative to treatment with placebo. In the 3-year osteoporosis treatment study, BONIVA 2.5 mg daily oral tablet produced increases in lumbar spine BMD that were progressive over 3 years of treatment and were statistically significant relative to placebo at 6 months and at all later time points. Lumbar spine BMD increased by 6.4% after 3 years of treatment with BONIVA 2.5 mg daily oral tablet compared with 1.4% in the placebo group (p<0.0001). Table 4 displays the significant increases in BMD seen at the lumbar spine, total hip, femoral neck, and trochanter compared to placebo.
| Placebo | BONIVA 2.5 mg | |
|---|---|---|
|
||
| Lumbar Spine | 1.4 (n=693) | 6.4 (n=712) |
| Total Hip | -0.7 (n=638) | 3.1 (n=654) |
| Femoral Neck | -0.7 (n=683) | 2.6 (n=699) |
| Trochanter | 0.2 (n=683) | 5.3 (n=699) |
16. How is Boniva supplied
17. Patient Counseling Information
"See FDA-approved patient labeling (Medication Guide)"
Inform patients that BONIVA Injection must be administered intravenously by a health care professional.
Patients should be instructed to read the Medication Guide carefully before BONIVA is administered and to re-read it each time the prescription is renewed because it contains important information the patient should know about BONIVA.
Inform patients that BONIVA Injection is administered once every 3 months. If the dose is missed, the injection should be administered as soon as it can be rescheduled. Thereafter, injections should be scheduled every 3 months from the date of the last injection. Do not administer BONIVA Injection more frequently than once every 3 months.
Inform patients that they should take supplemental calcium and vitamin D if their dietary intake is inadequate [see Warnings and Precautions (5.1)].
Inform patients BONIVA injection should not be administered to patients with creatinine clearance less than 30 mL/min. A serum creatinine should be measured prior to each dose [see Warnings and Precautions (5.3)].
Inform patients that the most common side effects of BONIVA include arthralgia, back pain, hypertension, and abdominal pain. Flu-like symptoms (acute phase reaction) may occur within 3 days following infusion, and usually subside within 24-48 hours without specific therapy.
Inform patients that there have been reports of persistent pain and/or a non-healing sore of the mouth or jaw, primarily in patients treated with bisphosphonates for other illnesses. If they experience these symptoms, they should inform their physician or dentist.
Inform patients that severe bone, joint, and/or muscle pain have been reported in patients taking bisphosphonates, including BONIVA. Patients should report severe symptoms if they develop.
Inform patients that atypical femur fractures in patients on bisphosphonate therapy have been reported. Patients should report new thigh or groin pain and undergo evaluation to rule out a femoral fracture.
MEDICATION GUIDE
Boniva® (bon-EE-va)
(ibandronate sodium)
Injection for intravenous use
Read the Medication Guide that comes with BONIVA before you start taking it and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking with your doctor about your medical condition or treatment. Talk to your doctor if you have any questions about BONIVA.
What is the most important information I should know about BONIVA?
BONIVA Injection is given in your vein (intravenously) and only given by a healthcare provider. Do not give BONIVA Injection to yourself.
BONIVA may cause serious side effects including:
-
- Low calcium levels in your blood (hypocalcemia)
- Severe allergic reaction (anaphylactic reaction)
- Severe kidney problems
- Severe jaw bone problems (osteonecrosis)
- Bone, joint or muscle pain
- Unusual thigh bone fractures
- 1.
-
Low calcium levels in your blood (hypocalcemia).
BONIVA may lower the calcium levels in your blood. If you have low blood calcium before you start taking BONIVA, it may get worse during treatment. Your low blood calcium must be treated before you receive BONIVA. Most people with low blood calcium levels do not have symptoms, but some people may have symptoms. Call your doctor right away if you have symptoms of low blood calcium such as:- Spasms, twitches, or cramps in your muscles
- Numbness or tingling in your fingers, toes, or around your mouth
- 2.
-
Severe allergic reactions.
Some people who received BONIVA Injection had severe allergic reactions (anaphylactic reactions) that led to death. Get medical help right away if you have any of the symptoms of a serious allergic reaction such as:- Swelling of your face, lips, mouth or tongue
- Trouble breathing
- Wheezing
- Severe itching
- Skin rash, redness or swelling
- Dizziness or fainting
- Fast heartbeat or pounding in your chest
- Sweating
- 3.
-
Severe kidney problems.
Severe kidney problems, including kidney failure, may happen when you receive BONIVA. Your doctor should do blood tests to check your kidneys before you receive each dose of BONIVA. - 4.
-
Severe jaw bone problems (osteonecrosis).
Severe jaw bone problems may happen when you receive BONIVA. Your doctor may examine your mouth before you start BONIVA. Your doctor may tell you to see your dentist before you start BONIVA. It is important for you to practice good mouth care during treatment with BONIVA. - 5.
-
Bone, joint, or muscle pain.
Some people who receive BONIVA develop severe bone, joint, or muscle pain. - 6.
-
Unusual thigh bone fractures.
Some people have developed unusual fractures in their thigh bone. Symptoms of a fracture may include new or unusual pain in your hip, groin, or thigh.
Call your doctor right away if you have any of these side effects.
What is BONIVA?
BONIVA is a prescription medicine used to treat osteoporosis in women after menopause. BONIVA helps increase bone mass and helps reduce the chance of having a spinal fracture (break).
It is not known how long BONIVA works for the treatment of osteoporosis. You should see your doctor regularly to determine if BONIVA is still right for you.
It is not known if BONIVA is safe and effective in children.
Who should not receive BONIVA?
Do not receive BONIVA if you:
- Have low levels of calcium in your blood
- Are allergic to ibandronate sodium or any of the ingredients in BONIVA. See the end of this leaflet for a complete list of ingredients in BONIVA.
What should I tell my healthcare provider before receiving BONIVA?
Before you receive BONIVA, tell your doctor if you:
- Have low blood calcium
- Plan to have dental surgery or teeth removed
- Have kidney problems or other problems that may affect your kidneys
- Have been told you have trouble absorbing minerals in your stomach or intestines (malabsorption syndrome)
- Are pregnant or plan to become pregnant. It is not known if BONIVA can harm your unborn baby.
- Are breast-feeding or plan to breast-feed. It is not known if BONIVA passes into your milk and may harm your baby.
Tell your doctor and dentist about all the medicines you take, including prescription and non-prescription medicines, vitamins and herbal supplements.
Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist each time you get a new medicine.
How should I receive BONIVA?
- BONIVA Injection is given 1 time every 3 months by a healthcare provider.
- If you miss a dose of BONIVA, call your doctor or healthcare provider to schedule your next dose.
What are the possible side effects of BONIVA?
BONIVA may cause serious side effects.
- See "What is the most important information I should know about BONIVA?"
The most common side effects of BONIVA include:
- Pain in your bones, joints or muscles
- Back pain
- Abdominal pain
- Flu-like symptoms may happen within 3 days after you receive BONIVA. Symptoms include:
- fever
- chills
- bone, joint, or muscle pain
- fatigue
If you have flu-like symptoms, they should get better within 24 to 48 hours.
Some people have pain or a sore that will not heal in their mouth or jaw while they receive BONIVA. Tell your doctor or dentist if you have mouth or jaw problems.
Tell your doctor if you have any side effect that bothers you or that does not go away.
These are not all the possible side effects of BONIVA. For more information, ask your doctor or pharmacist.
Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. You may also report side effects to Genentech at 1-888-835-2555.
How should I store BONIVA if I need to pick it up from a pharmacy?
- Store BONIVA Injection at room temperature between 68°F and 77°F (20°C and 25°C).
Keep BONIVA Injection and all medicines out of the reach of children.
General information about the safe and effective use of BONIVA.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use BONIVA for a condition for which it was not prescribed. Do not give BONIVA to other people, even if they have the same symptoms you have. It may harm them.
This Medication Guide summarizes the most important information about BONIVA. If you would like more information, talk with your doctor. You can ask your doctor or pharmacist for information about BONIVA that is written for health professionals.
What are the ingredients in BONIVA?
Active ingredient: ibandronate sodium
Inactive ingredients: glacial acetic acid, sodium acetate trihydrate, sodium chloride, and water
This Medication Guide has been approved by the U.S. Food and Drug Administration.
| BONIVA
ibandronate sodium injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Genentech, Inc. (080129000) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Roche Diagnostics GmbH | 315028860 | ANALYSIS(0004-0191) , API MANUFACTURE(0004-0191) , PACK(0004-0191) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| F. Hoffmann-La Roche AG | 482242971 | ANALYSIS(0004-0191) , API MANUFACTURE(0004-0191) | |