Drug Detail:Dupixent (Dupilumab [ doo-pil-us-mab ])
Drug Class: Interleukin inhibitors
Highlights of Prescribing Information
DUPIXENT® (dupilumab) injection, for subcutaneous use
Initial U.S. Approval: 2017
Recent Major Changes
| Indications and Usage, Atopic Dermatitis (1.1) | 06/2022 |
| Indications and Usage, EoE (1.4) | 05/2022 |
| Indications and Usage, PN (1.5) | 09/2022 |
| Dosage and Administration, Atopic Dermatitis (2.1; 2.3) | 06/2022 |
| Dosage and Administration (2.1; 2.2; 2.4; 2.9) | 12/2021 |
| Dosage and Administration (2.1) | 10/2022 |
| Dosage and Administration, EoE (2.6; 2.8) | 05/2022 |
| Dosage and Administration, PN (2.7) | 09/2022 |
| Warnings and Precautions (5.1; 5.2; 5.7; 5.8; 5.9) | 12/2021 |
| Warnings and Precautions (5.2) | 05/2022 |
| Warnings and Precautions (5.2) | 09/2022 |
Indications and Usage for Dupixent
DUPIXENT is an interleukin-4 receptor alpha antagonist indicated:
Atopic Dermatitis
- for the treatment of adult and pediatric patients aged 6 months and older with moderate-to-severe AD whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. DUPIXENT can be used with or without topical corticosteroids. (1.1)
Asthma
- as an add-on maintenance treatment of adult and pediatric patients aged 6 years and older with moderate-to-severe asthma characterized by an eosinophilic phenotype or with oral corticosteroid dependent asthma. (1.2)
Limitations of Use: Not for the relief of acute bronchospasm or status asthmaticus. (1.2)
Chronic Rhinosinusitis with Nasal Polyposis
- as an add-on maintenance treatment in adult patients with inadequately controlled chronic rhinosinusitis with nasal polyposis (CRSwNP). (1.3)
Eosinophilic Esophagitis
- for the treatment of adult and pediatric patients aged 12 years and older, weighing at least 40 kg, with eosinophilic esophagitis (EoE). (1.4)
Prurigo Nodularis
- for the treatment of adult patients with prurigo nodularis (PN). (1.5)
Dupixent Dosage and Administration
Atopic Dermatitis
Dosage in Adults (2.3):
- Recommended dosage is an initial dose of 600 mg (two 300 mg injections), followed by 300 mg given every other week (Q2W).
Dosage in Pediatric Patients 6 Months to 5 Years of Age (2.3):
| Body Weight | Initial and Subsequent Dosage |
|---|---|
| 5 to less than 15 kg | 200 mg (one 200 mg injection) every 4 weeks (Q4W) |
| 15 to less than 30 kg | 300 mg (one 300 mg injection) every 4 weeks (Q4W) |
Dosage in Pediatric Patients 6 Years to 17 Years of Age (2.3):
| Body Weight | Initial Loading Dose | Subsequent Dosage* |
|---|---|---|
|
||
| 15 to less than 30 kg | 600 mg (two 300 mg injections) | 300 mg Q4W |
| 30 to less than 60 kg | 400 mg (two 200 mg injections) | 200 mg Q2W |
| 60 kg or more | 600 mg (two 300 mg injections) | 300 mg Q2W |
Asthma
Dosage in Adult and Pediatric Patients 12 Years and Older (2.4):
| Initial Loading Dose | Subsequent Dosage |
|---|---|
| 400 mg (two 200 mg injections) | 200 mg every 2 weeks (Q2W) |
| or | |
| 600 mg (two 300 mg injections) | 300 mg every 2 weeks (Q2W) |
| Dosage for patients with oral corticosteroid-dependent asthma or with co-morbid moderate-to-severe atopic dermatitis or adults with co-morbid chronic rhinosinusitis with nasal polyposis | |
| 600 mg (two 300 mg injections) | 300 mg every 2 weeks (Q2W) |
Dosage in Pediatric Patients 6 to 11 Years of Age (2.4):
| Body Weight | Initial Dose and Subsequent Dosage |
|---|---|
| 15 to less than 30 kg | 100 mg every other week (Q2W) or 300 mg every four weeks (Q4W) |
| ≥30 kg | 200 mg every other week (Q2W) |
For pediatric patients 6 to 11 years old with asthma and co-morbid moderate-to-severe atopic dermatitis, follow the recommended dosage as per Table 2 which includes an initial loading dose. (2.3)
Chronic Rhinosinusitis with Nasal Polyposis (2.5):
- Recommended dosage for adult patients is 300 mg given every other week (Q2W).
Eosinophilic Esophagitis (2.6):
- Recommended dosage for adult and pediatric patients 12 years of age and older, weighing at least 40 kg, is 300 mg given every week (QW).
Prurigo Nodularis (2.7):
- Recommended dosage for adult patients is an initial dose of 600 mg (two 300 mg injections), followed by 300 mg given every other week (Q2W).
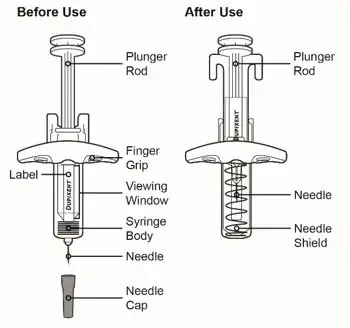
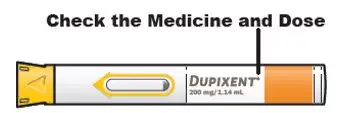
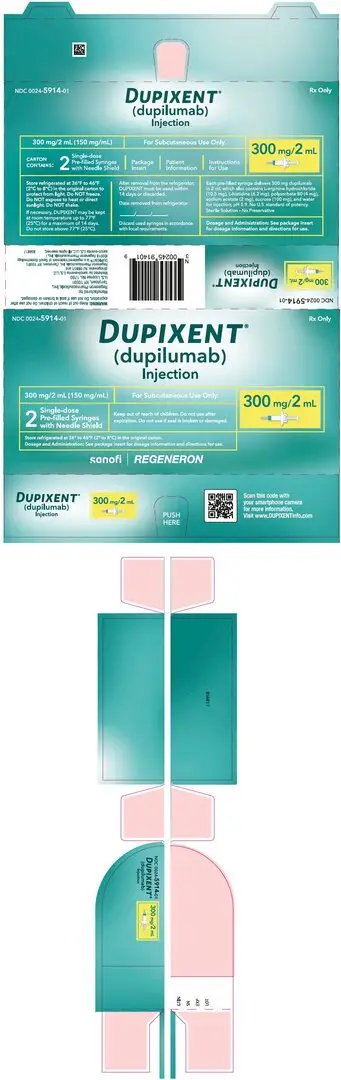
Dosage Forms and Strengths
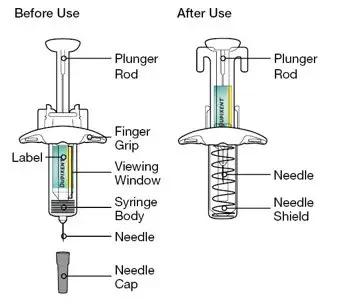
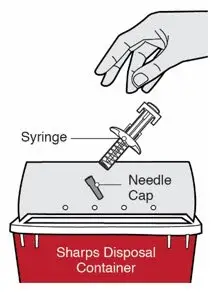
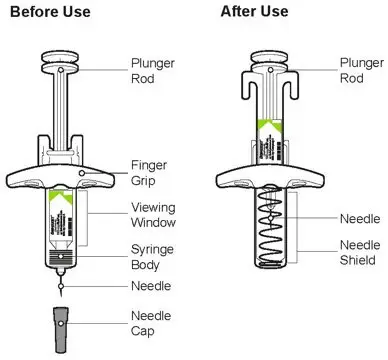
Single-Dose Pre-Filled Syringe with Needle Shield (3):
- Injection: 300 mg/2 mL
- Injection: 200 mg/1.14 mL
- Injection: 100 mg/0.67 mL
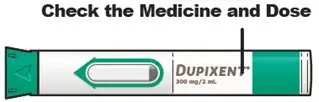
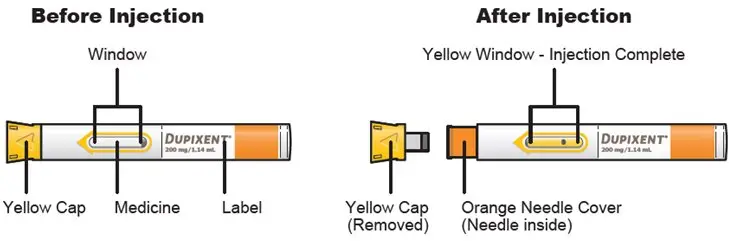
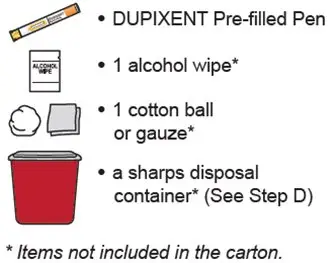
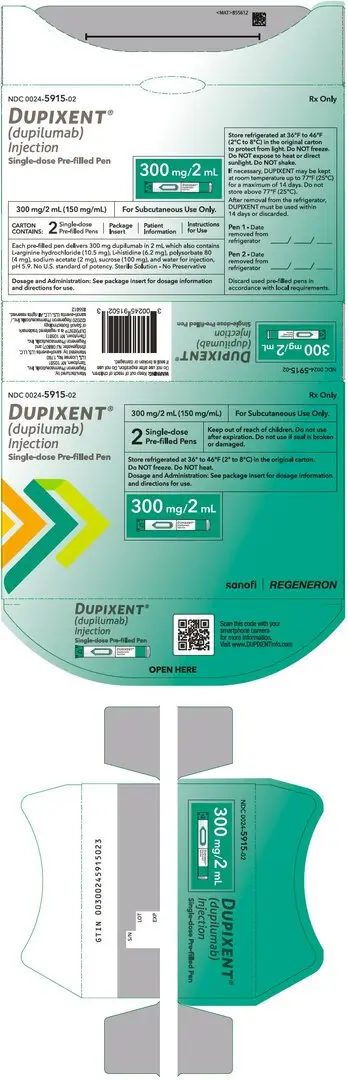
Single-Dose Pre-Filled Pen (3):
- Injection: 300 mg/2 mL
- Injection: 200 mg/1.14 mL
Contraindications
Known hypersensitivity to dupilumab or any excipients in DUPIXENT. (4)
Warnings and Precautions
- Hypersensitivity: Hypersensitivity reactions including anaphylaxis, serum sickness, angioedema, urticaria, rash, erythema nodosum, and erythema multiforme have occurred. Discontinue DUPIXENT in the event of a hypersensitivity reaction. (5.1)
- Conjunctivitis and Keratitis: Advise patients to report new onset or worsening eye symptoms to their healthcare provider. Consider ophthalmological examination, as appropriate. (5.2)
- Eosinophilic Conditions: Be alert to vasculitic rash, worsening pulmonary symptoms, and/or neuropathy, especially upon reduction of oral corticosteroids. (5.3)
- Reduction of Corticosteroid Dosage: Do not discontinue systemic, topical, or inhaled corticosteroids abruptly upon initiation of DUPIXENT. Decrease steroids gradually, if appropriate. (5.5)
- Arthralgia: Advise patients to report new onset or worsening joint symptoms to their healthcare provider. If symptoms persist or worsen, consider rheumatological evaluation and/or discontinuation of DUPIXENT. (5.7)
- Parasitic (Helminth) Infections: Treat pre-existing helminth infections before initiating DUPIXENT. If patients become infected while receiving DUPIXENT and do not respond to anti-helminth treatment, discontinue DUPIXENT until the infection resolves. (5.8)
- Vaccinations: Avoid use of live vaccines. (5.9)
Adverse Reactions/Side Effects
Most common adverse reactions are:
- Atopic Dermatitis (incidence ≥1%): injection site reactions, conjunctivitis, blepharitis, oral herpes, keratitis, eye pruritus, other herpes simplex virus infection, dry eye, and eosinophilia. (6.1)
- Asthma (incidence ≥1%): injection site reactions, oropharyngeal pain, and eosinophilia. (6.1)
- Chronic Rhinosinusitis with Nasal Polyposis (incidence ≥1%): injection site reactions, eosinophilia, insomnia, toothache, gastritis, arthralgia, and conjunctivitis. (6.1)
- Eosinophilic Esophagitis (incidence ≥2%): injection site reactions, upper respiratory tract infections, arthralgia, and herpes viral infections. (6.1)
- Prurigo Nodularis (incidence ≥2%): nasopharyngitis, conjunctivitis, herpes infection, dizziness, myalgia, and diarrhea. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Regeneron at 1-844-387-4936 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 10/2022
Full Prescribing Information
1. Indications and Usage for Dupixent
1.1 Atopic Dermatitis
DUPIXENT is indicated for the treatment of adult and pediatric patients aged 6 months and older with moderate-to-severe atopic dermatitis (AD) whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable. DUPIXENT can be used with or without topical corticosteroids.
1.2 Asthma
DUPIXENT is indicated as an add-on maintenance treatment of adult and pediatric patients aged 6 years and older with moderate-to-severe asthma characterized by an eosinophilic phenotype or with oral corticosteroid dependent asthma [see Clinical Studies (14)].
1.3 Chronic Rhinosinusitis with Nasal Polyposis
DUPIXENT is indicated as an add-on maintenance treatment in adult patients with inadequately controlled chronic rhinosinusitis with nasal polyposis (CRSwNP).
2. Dupixent Dosage and Administration
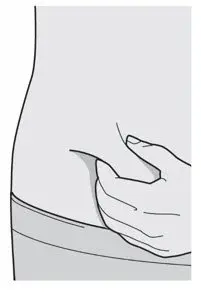
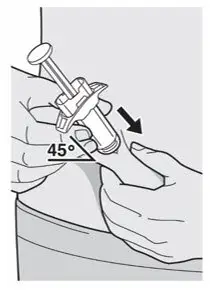
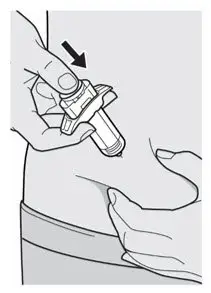
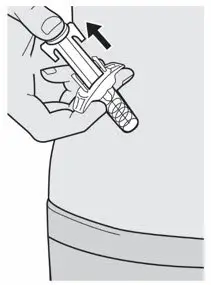
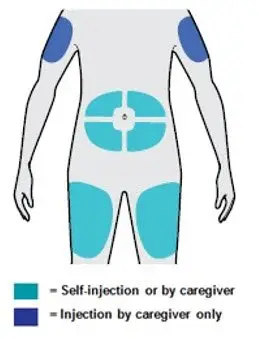
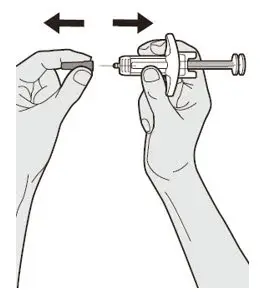
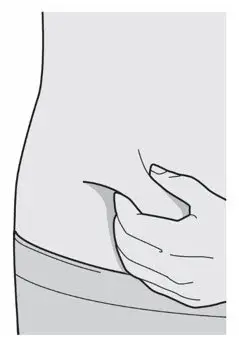
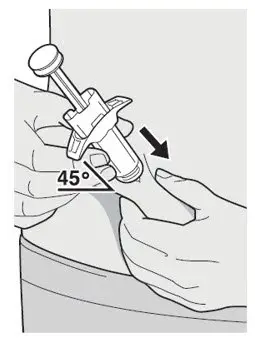
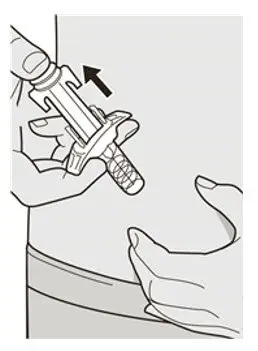
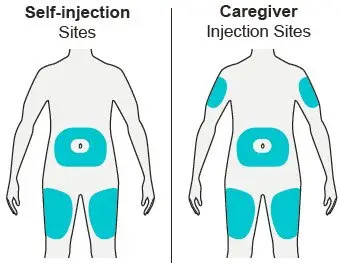
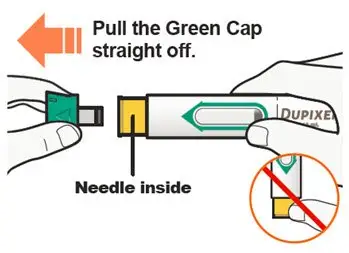
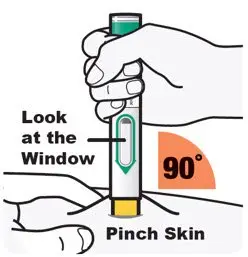
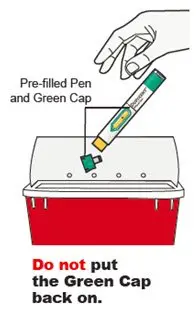
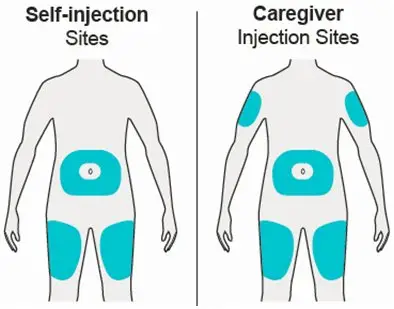
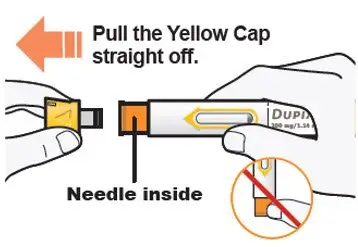
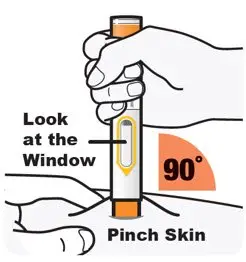
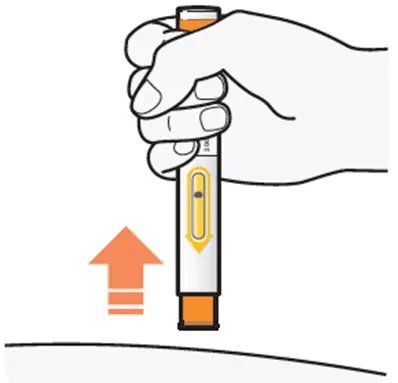
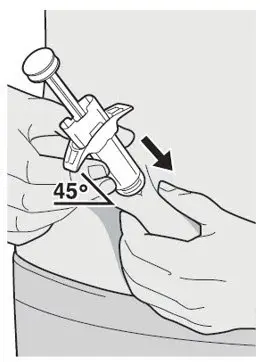
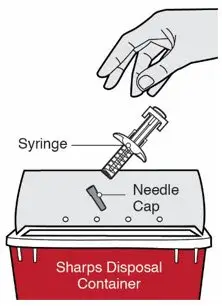
2.1 Important Administration Instructions
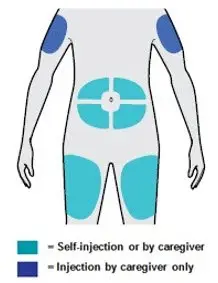
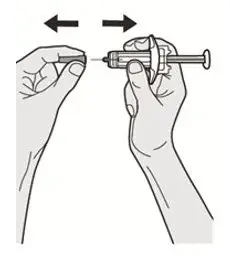
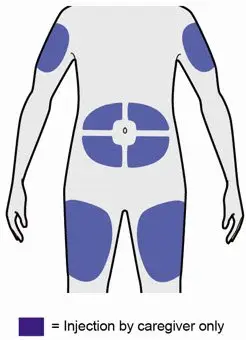
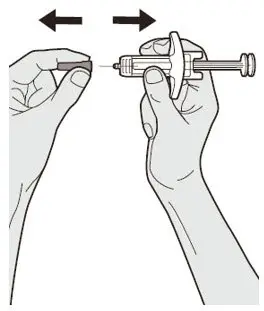
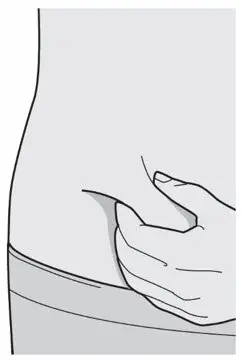
DUPIXENT is administered by subcutaneous injection.
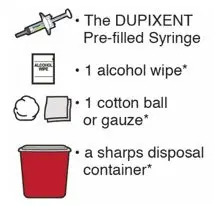
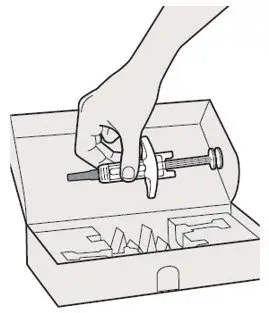
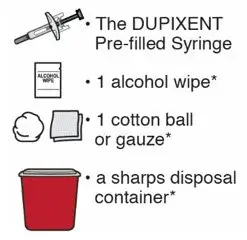
DUPIXENT is intended for use under the guidance of a healthcare provider. Provide proper training to patients and/or caregivers on the preparation and administration of DUPIXENT prior to use according to the "Instructions for Use".
2.2 Vaccination Prior to Treatment
Consider completing all age-appropriate vaccinations as recommended by current immunization guidelines prior to initiating treatment with DUPIXENT [see Warnings and Precautions (5.9)].
2.3 Recommended Dosage for Atopic Dermatitis
Dosage in Pediatric Patients 6 Months to 5 Years of Age
The recommended dosage of DUPIXENT for pediatric patients 6 months to 5 years of age is specified in Table 1.
| Body Weight | Initial* and Subsequent Dosage |
|---|---|
|
|
| 5 to less than 15 kg | 200 mg (one 200 mg injection) every 4 weeks (Q4W) |
| 15 to less than 30 kg | 300 mg (one 300 mg injection) every 4 weeks (Q4W) |
Dosage in Pediatric Patients 6 Years to 17 Years of Age
The recommended dosage of DUPIXENT for pediatric patients 6 years to 17 years of age is specified in Table 2.
| Body Weight | Initial Loading Dose | Subsequent Dosage |
|---|---|---|
| 15 to less than 30 kg | 600 mg (two 300 mg injections) | 300 mg every 4 weeks (Q4W) |
| 30 to less than 60 kg | 400 mg (two 200 mg injections) | 200 mg every other week (Q2W) |
| 60 kg or more | 600 mg (two 300 mg injections) | 300 mg every other week (Q2W) |
2.4 Recommended Dosage for Asthma
Dosage in Adult and Pediatric Patients 12 Years and Older
The recommended dosage of DUPIXENT for adult and pediatric patients 12 years of age and older is specified in Table 3.
| Initial Loading Dose | Subsequent Dosage |
|---|---|
| 400 mg (two 200 mg injections) | 200 mg every 2 weeks (Q2W) |
| or | |
| 600 mg (two 300 mg injections) | 300 mg every 2 weeks (Q2W) |
| Dosage for patients with oral corticosteroid-dependent asthma or with co-morbid moderate-to-severe atopic dermatitis or adults with co-morbid chronic rhinosinusitis with nasal polyposis | |
| 600 mg (two 300 mg injections) | 300 mg every 2 weeks (Q2W) |
Dosage in Pediatric Patients 6 to 11 Years of Age
The recommended dosage of DUPIXENT for pediatric patients 6 to 11 years of age is specified in Table 4.
| Body Weight | Initial* and Subsequent Dosage |
|---|---|
|
|
| 15 to less than 30 kg | 100 mg every other week (Q2W) or 300 mg every four weeks (Q4W) |
| ≥30 kg | 200 mg every other week (Q2W) |
For pediatric patients 6 to 11 years of age with asthma and co-morbid moderate-to-severe AD, follow the recommended dosage as per Table 2 which includes an initial loading dose [see Dosage and Administration (2.3)].
2.5 Recommended Dosage for Chronic Rhinosinusitis with Nasal Polyposis
The recommended dosage of DUPIXENT for adult patients is 300 mg given every other week.
2.6 Recommended Dosage for Eosinophilic Esophagitis
The recommended dosage of DUPIXENT for adult and pediatric patients 12 years of age and older, weighing at least 40 kg, is 300 mg given every week (QW).
2.7 Recommended Dosage for Prurigo Nodularis
The recommended dosage of DUPIXENT for adult patients is an initial dose of 600 mg (two 300 mg injections) followed by 300 mg given every other week (Q2W).
2.8 Missed Doses
If a weekly dose is missed, administer the dose as soon as possible, and start a new weekly schedule from the date of the last administered dose.
If an every other week dose is missed, administer the injection within 7 days from the missed dose and then resume the patient's original schedule. If the missed dose is not administered within 7 days, wait until the next dose on the original schedule.
If an every 4 week dose is missed, administer the injection within 7 days from the missed dose and then resume the patient's original schedule. If the missed dose is not administered within 7 days, administer the dose, starting a new schedule based on this date.
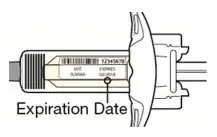
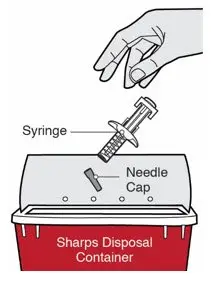
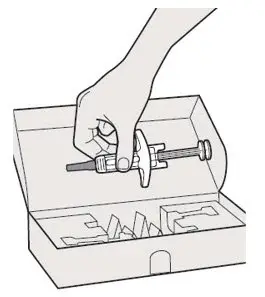
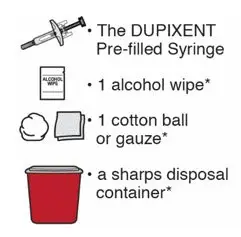
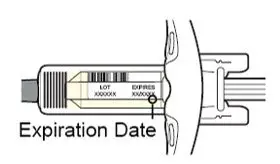
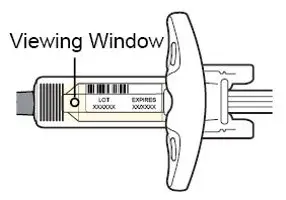
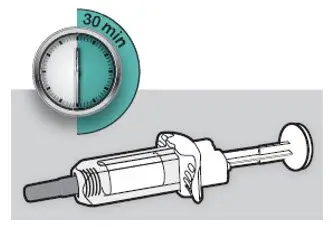
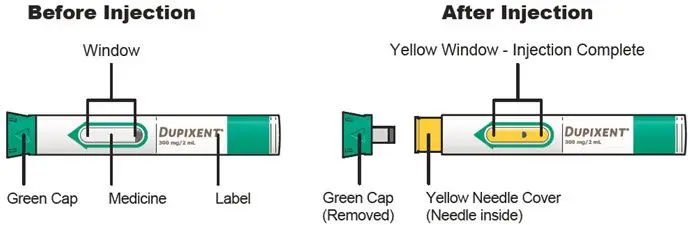
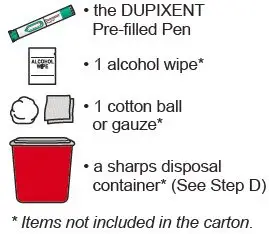
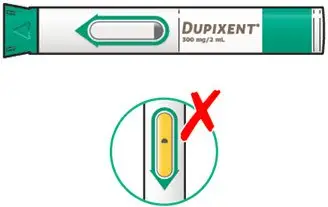
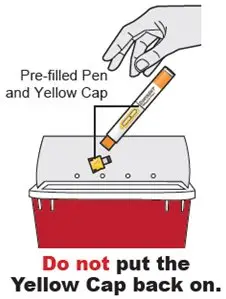
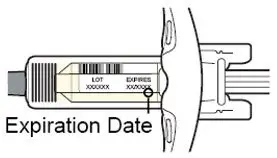
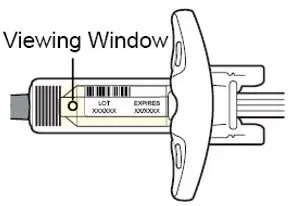
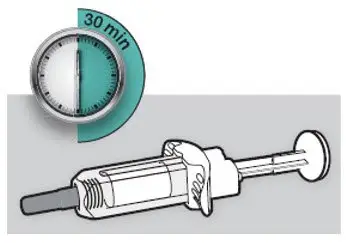
2.9 Preparation for Use
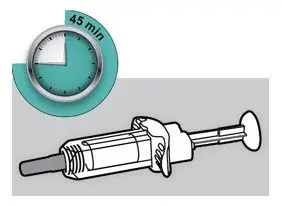
Before injection, remove DUPIXENT from the refrigerator and allow DUPIXENT to reach room temperature (45 minutes for the 300 mg/2 mL pre-filled syringe or pre-filled pen, 30 minutes for the 200 mg/1.14 mL pre-filled syringe or pre-filled pen, and 100 mg/0.67 mL pre-filled syringe) without removing the needle cap. After removal from the refrigerator, DUPIXENT must be used within 14 days or discarded.
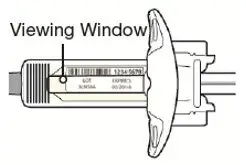
Inspect DUPIXENT visually for particulate matter and discoloration prior to administration. DUPIXENT is a clear to slightly opalescent, colorless to pale yellow solution. Do not use if the liquid contains visible particulate matter, is discolored or cloudy (other than clear to slightly opalescent, colorless to pale yellow). DUPIXENT does not contain preservatives; therefore, discard any unused product remaining in the pre-filled syringe or pre-filled pen.
3. Dosage Forms and Strengths
DUPIXENT is a clear to slightly opalescent, colorless to pale yellow solution in a:
Single-dose pre-filled syringe with needle shield as:
- Injection: 300 mg/2 mL
- Injection: 200 mg/1.14 mL
- Injection: 100 mg/0.67 mL
Single-dose pre-filled pen as:
- Injection: 300 mg/2 mL
- Injection: 200 mg/1.14 mL
4. Contraindications
DUPIXENT is contraindicated in patients who have known hypersensitivity to dupilumab or any excipients of DUPIXENT [see Warnings and Precautions (5.1)].
5. Warnings and Precautions
5.1 Hypersensitivity
Hypersensitivity reactions, including anaphylaxis, serum sickness or serum sickness-like reactions, angioedema, generalized urticaria, rash, erythema nodosum, and erythema multiforme have been reported. If a clinically significant hypersensitivity reaction occurs, institute appropriate therapy and discontinue DUPIXENT [see Adverse Reactions (6.1, 6.2, 6.3)].
5.2 Conjunctivitis and Keratitis
Conjunctivitis and keratitis adverse reactions have been reported in clinical trials.
Conjunctivitis and keratitis occurred more frequently in AD subjects who received DUPIXENT compared to those who received placebo. Conjunctivitis was the most frequently reported eye disorder. Most subjects with conjunctivitis or keratitis recovered or were recovering during the treatment period [see Adverse Reactions (6.1)].
In subjects with CRSwNP, the frequency of conjunctivitis was 2% in the DUPIXENT group compared to 1% in the placebo group in the 24-week safety pool; these subjects recovered. There were no cases of keratitis reported in the CRSwNP development program [see Adverse Reactions (6.1)].
Among subjects with asthma, the frequencies of conjunctivitis and keratitis were similar between DUPIXENT and placebo [see Adverse Reactions (6.1)].
Among subjects with EoE, the frequency of conjunctivitis and keratitis was 0% and 0% in the DUPIXENT group and 2% and 0% in the placebo group, respectively [see Adverse Reactions (6.1)].
In subjects with PN, the frequency of conjunctivitis was 4% in the DUPIXENT group compared to 1% in the placebo group; these subjects recovered or were recovering during the treatment period. There were no cases of keratitis reported in the PN development program [see Adverse Reactions (6.1)].
Conjunctivitis and keratitis adverse events have also been reported with DUPIXENT in postmarketing settings, predominantly in AD patients. Some patients reported visual disturbances (e.g., blurred vision) associated with conjunctivitis or keratitis.
Advise patients to report new onset or worsening eye symptoms to their healthcare provider. Consider ophthalmological examination for patients who develop conjunctivitis that does not resolve following standard treatment or signs and symptoms suggestive of keratitis, as appropriate [see Adverse Reactions (6.1)].
5.3 Eosinophilic Conditions
Patients being treated for asthma may present with serious systemic eosinophilia sometimes presenting with clinical features of eosinophilic pneumonia or vasculitis consistent with eosinophilic granulomatosis with polyangiitis, conditions which are often treated with systemic corticosteroid therapy. These events may be associated with the reduction of oral corticosteroid therapy. Healthcare providers should be alert to vasculitic rash, worsening pulmonary symptoms, cardiac complications, and/or neuropathy presenting in their patients with eosinophilia. Cases of eosinophilic pneumonia were reported in adult subjects who participated in the asthma development program and cases of vasculitis consistent with eosinophilic granulomatosis with polyangiitis have been reported with DUPIXENT in adult subjects who participated in the asthma development program as well as in adult subjects with co-morbid asthma in the CRSwNP development program. A causal association between DUPIXENT and these conditions has not been established.
5.4 Acute Asthma Symptoms or Deteriorating Disease
DUPIXENT should not be used to treat acute asthma symptoms or acute exacerbations. Do not use DUPIXENT to treat acute bronchospasm or status asthmaticus. Patients should seek medical advice if their asthma remains uncontrolled or worsens after initiation of treatment with DUPIXENT.
5.5 Risk Associated with Abrupt Reduction of Corticosteroid Dosage
Do not discontinue systemic, topical, or inhaled corticosteroids abruptly upon initiation of therapy with DUPIXENT. Reductions in corticosteroid dose, if appropriate, should be gradual and performed under the direct supervision of a healthcare provider. Reduction in corticosteroid dose may be associated with systemic withdrawal symptoms and/or unmask conditions previously suppressed by systemic corticosteroid therapy.
5.6 Patients with Co-morbid Asthma
Advise patients with co-morbid asthma not to adjust or stop their asthma treatments without consultation with their physicians.
5.7 Arthralgia
Arthralgia has been reported with the use of DUPIXENT with some patients reporting gait disturbances or decreased mobility associated with joint symptoms; some cases resulted in hospitalization [see Adverse Reactions (6.1)]. In postmarketing reports, onset of arthralgia was variable, ranging from days to months after the first dose of DUPIXENT. Some patients' symptoms resolved while continuing treatment with DUPIXENT and other patients recovered or were recovering following discontinuation of DUPIXENT.
Advise patients to report new onset or worsening joint symptoms to their healthcare provider. If symptoms persist or worsen, consider rheumatological evaluation and/or discontinuation of DUPIXENT.
5.8 Parasitic (Helminth) Infections
Patients with known helminth infections were excluded from participation in clinical studies. It is unknown if DUPIXENT will influence the immune response against helminth infections.
Treat patients with pre-existing helminth infections before initiating therapy with DUPIXENT. If patients become infected while receiving treatment with DUPIXENT and do not respond to anti-helminth treatment, discontinue treatment with DUPIXENT until the infection resolves. Adverse reactions of helminth infections (5 cases of enterobiasis and 1 case of ascariasis) were reported in pediatric patients 6 to 11 years old who participated in the pediatric asthma development program [see Adverse Reactions (6.1)].
5.9 Vaccinations
Consider completing all age-appropriate vaccinations as recommended by current immunization guidelines prior to initiating treatment with DUPIXENT. Avoid use of live vaccines in patients treated with DUPIXENT. It is unknown if administration of live vaccines during DUPIXENT treatment will impact the safety or effectiveness of these vaccines. Limited data are available regarding coadministration of DUPIXENT with non-live vaccines [see Clinical Pharmacology (12.2)].
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Hypersensitivity [see Warnings and Precautions (5.1)]
- Conjunctivitis and Keratitis [see Warnings and Precautions (5.2)]
- Arthralgia [see Warnings and Precautions (5.7)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Weeks 0 to 16 (SOLO 1, SOLO 2, CHRONOS, and AD-1021)
In DUPIXENT monotherapy trials (SOLO 1, SOLO 2, and AD-1021) through Week 16, the proportion of subjects who discontinued treatment because of adverse events was 1.9% in both the DUPIXENT 300 mg Q2W and placebo groups. Table 5 summarizes the adverse reactions that occurred at a rate of at least 1% in the DUPIXENT 300 mg Q2W monotherapy groups, and in the DUPIXENT + TCS group, all at a higher rate than in their respective comparator groups during the first 16 weeks of treatment.
| Adverse Reaction | DUPIXENT Monotherapy* | DUPIXENT + TCS† | ||
|---|---|---|---|---|
| DUPIXENT 300 mg Q2W‡ | Placebo | DUPIXENT 300 mg Q2W‡ + TCS | Placebo + TCS | |
| N=529 n (%) | N=517 n (%) | N=110 n (%) | N=315 n (%) |
|
|
||||
| Injection site reaction | 51 (10) | 28 (5) | 11 (10) | 18 (6) |
| Conjunctivitis§ | 51 (10) | 12 (2) | 10 (9) | 15 (5) |
| Blepharitis | 2 (<1) | 1 (<1) | 5 (5) | 2 (1) |
| Oral herpes | 20 (4) | 8 (2) | 3 (3) | 5 (2) |
| Keratitis¶ | 1 (<1) | 0 | 4 (4) | 0 |
| Eye pruritus | 3 (1) | 1 (<1) | 2 (2) | 2 (1) |
| Other herpes simplex virus infection# | 10 (2) | 6 (1) | 1 (1) | 1 (<1) |
| Dry eye | 1 (<1) | 0 | 2 (2) | 1 (<1) |
Asthma
Adults and Pediatric Subjects 12 Years of Age and Older with Asthma
A total of 2888 adult and pediatric subjects 12 to 17 years of age with moderate-to-severe asthma (AS) were evaluated in 3 randomized, placebo-controlled, multicenter trials of 24 to 52 weeks duration (DRI12544, QUEST, and VENTURE). Of these, 2678 had a history of 1 or more severe exacerbations in the year prior to enrollment despite regular use of medium to high-dose inhaled corticosteroids plus an additional controller(s) (DRI12544 and QUEST). A total of 210 subjects with oral corticosteroid-dependent asthma receiving high-dose inhaled corticosteroids plus up to two additional controllers were enrolled (VENTURE). The safety population (DRI12544 and QUEST) was 12-87 years of age, of which 63% were female, and 82% were White. DUPIXENT 200 mg or 300 mg was administered subcutaneously Q2W, following an initial dose of 400 mg or 600 mg, respectively.
In DRI12544 and QUEST, the proportion of subjects who discontinued treatment due to adverse events was 4% of the placebo group, 3% of the DUPIXENT 200 mg Q2W group, and 6% of the DUPIXENT 300 mg Q2W group.
Table 6 summarizes the adverse reactions that occurred at a rate of at least 1% in subjects treated with DUPIXENT and at a higher rate than in their respective comparator groups in DRI12544 and QUEST.
| Adverse Reaction | DRI12544 and QUEST | ||
|---|---|---|---|
| DUPIXENT 200 mg Q2W | DUPIXENT 300 mg Q2W | Placebo | |
| N=779 n (%) | N=788 n (%) | N=792 n (%) |
|
|
|||
| Injection site reactions* | 111 (14%) | 144 (18%) | 50 (6%) |
| Oropharyngeal pain | 13 (2%) | 19 (2%) | 7 (1%) |
| Eosinophilia† | 17 (2%) | 16 (2%) | 2 (<1%) |
Injection site reactions were most common with the loading (initial) dose.
The safety profile of DUPIXENT through Week 52 was generally consistent with the safety profile observed at Week 24.
Chronic Rhinosinusitis with Nasal Polyposis
A total of 722 adult subjects with chronic rhinosinusitis with nasal polyposis (CRSwNP) were evaluated in 2 randomized, placebo-controlled, multicenter trials of 24 to 52 weeks duration (SINUS-24 and SINUS-52). The safety pool consisted of data from the first 24 weeks of treatment from both studies.
In the safety pool, the proportion of subjects who discontinued treatment due to adverse events was 5% of the placebo group and 2% of the DUPIXENT 300 mg Q2W group.
Table 7 summarizes the adverse reactions that occurred at a rate of at least 1% in subjects treated with DUPIXENT and at a higher rate than in their respective comparator group in SINUS-24 and SINUS-52.
| Adverse Reaction | SINUS-24 and SINUS-52 | |
|---|---|---|
| DUPIXENT 300 mg Q2W | Placebo | |
| N=440 n (%) | N=282 n (%) |
|
|
||
| Injection site reactions* | 28 (6%) | 12 (4%) |
| Conjunctivitis† | 7 (2%) | 2 (1%) |
| Arthralgia | 14 (3%) | 5 (2%) |
| Gastritis | 7 (2%) | 2 (1%) |
| Insomnia | 6 (1%) | 0 (<1%) |
| Eosinophilia | 5 (1%) | 1 (<1%) |
| Toothache | 5 (1%) | 1 (<1%) |
The safety profile of DUPIXENT through Week 52 was generally consistent with the safety profile observed at Week 24.
6.2 Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors, including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies to dupilumab in the studies described below with the incidence of antibodies in other studies or to other products may be misleading.
6.3 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of DUPIXENT. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Immune system disorders: angioedema [see Warnings and Precautions (5.1)]
Skin and subcutaneous tissue disorders: Facial skin reactions, including erythema, rash, scaling, edema, papules, pruritus, burning, and pain
8. Use In Specific Populations
8.5 Geriatric Use
Of the 1472 subjects with AD exposed to DUPIXENT in a dose-ranging study and placebo-controlled trials, 67 subjects were 65 years or older. Clinical trials of DUPIXENT in AD did not include sufficient numbers of subjects aged 65 years and over to determine whether they respond differently from younger subjects [see Clinical Pharmacology (12.3)].
Of the 1977 subjects with asthma exposed to DUPIXENT, a total of 240 subjects were 65 years or older. Efficacy and safety in this age group was similar to the overall study population.
Of the 440 subjects with CRSwNP exposed to DUPIXENT, a total of 79 subjects were 65 years or older. Efficacy and safety in this age group were similar to the overall study population.
Clinical studies of DUPIXENT in EoE did not include sufficient numbers of subjects aged 65 years and over to determine whether they respond differently from younger adult subjects.
Of the 152 subjects with PN exposed to DUPIXENT, a total of 37 were 65 years or older including 8 subjects 75 years or older. Clinical trials did not include a sufficient number of subjects 65 years of age and older to determine whether they respond differently from younger adult subjects.
10. Overdosage
There is no specific treatment for DUPIXENT overdose. In the event of overdosage, contact Poison Control (1-800-222-1222) for the latest recommendations and monitor the patient for any signs or symptoms of adverse reactions and institute appropriate symptomatic treatment immediately.
11. Dupixent Description
Dupilumab, an interleukin-4 receptor alpha antagonist, is a human monoclonal antibody of the IgG4 subclass that binds to the IL-4Rα subunit and inhibits IL-4 and IL-13 signaling. Dupilumab has an approximate molecular weight of 147 kDa.
Dupilumab is produced by recombinant DNA technology in Chinese Hamster Ovary cell suspension culture.
DUPIXENT (dupilumab) Injection is supplied as a sterile, preservative-free, clear to slightly opalescent, colorless to pale yellow solution for subcutaneous injection. DUPIXENT is provided as either a single-dose pre-filled syringe with needle shield or a single-dose pre-filled pen in a siliconized Type-1 clear glass syringe. The needle cap is not made with natural rubber latex.
Each 300 mg pre-filled syringe or pre-filled pen delivers 300 mg dupilumab in 2 mL which also contains L-arginine hydrochloride (10.5 mg), L-histidine (6.2 mg), polysorbate 80 (4 mg), sodium acetate (2 mg), sucrose (100 mg), and water for injection, pH 5.9.
Each 200 mg pre-filled syringe or pre-filled pen delivers 200 mg dupilumab in 1.14 mL which also contains L-arginine hydrochloride (12 mg), L-histidine (3.5 mg), polysorbate 80 (2.3 mg), sodium acetate (1.2 mg), sucrose (57 mg), and water for injection, pH 5.9.
Each 100 mg pre-filled syringe delivers 100 mg dupilumab in 0.67 mL which also contains L-arginine hydrochloride (3.5 mg), L-histidine (2.1 mg), polysorbate 80 (1.3 mg), sodium acetate (0.7 mg), sucrose (34 mg), and water for injection, pH 5.9.
12. Dupixent - Clinical Pharmacology
12.1 Mechanism of Action
Dupilumab is a human monoclonal IgG4 antibody that inhibits interleukin-4 (IL-4) and interleukin-13 (IL-13) signaling by specifically binding to the IL-4Rα subunit shared by the IL-4 and IL-13 receptor complexes. Dupilumab inhibits IL-4 signaling via the Type I receptor and both IL-4 and IL-13 signaling through the Type II receptor.
Inflammation driven by IL-4 and IL-13 is an important component in the pathogenesis of asthma, AD, CRSwNP, EoE, and PN. Multiple cell types that express IL-4Rα (e.g., mast cells, eosinophils, macrophages, lymphocytes, epithelial cells, goblet cells) and inflammatory mediators (e.g., histamine, eicosanoids, leukotrienes, cytokines, chemokines) are involved in inflammation. Blocking IL-4Rα with dupilumab inhibits IL-4 and IL-13 cytokine-induced inflammatory responses, including the release of proinflammatory cytokines, chemokines, nitric oxide, and IgE. The mechanism of dupilumab action has not been definitively established.
12.2 Pharmacodynamics
Consistent with inhibition of IL-4 and IL-13 signaling, dupilumab treatment decreased certain biomarkers of inflammation. In asthma subjects, fractional exhaled nitric oxide (FeNO) and circulating concentrations of eotaxin-3, total IgE, allergen specific IgE, TARC, and periostin were decreased relative to placebo. Reductions in these biomarkers were comparable for the 300 mg Q2W and 200 mg Q2W regimens. These markers were near maximal suppression after 2 weeks of treatment, except for IgE which declined more slowly. These effects were sustained throughout treatment. The median percent reduction from baseline in total IgE concentrations with dupilumab treatments was 52% at Week 24 (DRI12544) and 70% at Week 52 (QUEST). For FeNO, the mean percent reduction from baseline at Week 2 was 35% and 24% in DRI12544 and QUEST, respectively, and in the overall safety population, the mean FeNO level decreased to 20 ppb.
12.3 Pharmacokinetics
The pharmacokinetics of dupilumab is similar in subjects with AD, asthma, CRSwNP, EoE and PN.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Animal studies have not been conducted to evaluate the carcinogenic or mutagenic potential of dupilumab.
No effects on fertility parameters such as reproductive organs, menstrual cycle length, or sperm analysis were observed in sexually mature mice that were subcutaneously administered a homologous antibody against IL-4Rα at doses up to 200 mg/kg/week.
14. Clinical Studies
14.1 Atopic Dermatitis
Clinical Response at Week 16 (SOLO 1, SOLO 2, and CHRONOS)
The results of the DUPIXENT monotherapy trials (SOLO 1 and SOLO 2) and the DUPIXENT with concomitant TCS trial (CHRONOS) are presented in Table 10.
| SOLO 1 | SOLO 2 | CHRONOS | ||||
|---|---|---|---|---|---|---|
| DUPIXENT 300 mg Q2W | Placebo | DUPIXENT 300 mg Q2W | Placebo | DUPIXENT 300 mg Q2W + TCS | Placebo + TCS | |
|
||||||
| Number of subjects randomized (FAS)* | 224 | 224 | 233 | 236 | 106 | 315 |
| IGA 0 or 1†,‡ | 38% | 10% | 36% | 9% | 39% | 12% |
| EASI-75‡ | 51% | 15% | 44% | 12% | 69% | 23% |
| EASI-90‡ | 36% | 8% | 30% | 7% | 40% | 11% |
| Number of subjects with baseline Peak Pruritus NRS score ≥4 | 213 | 212 | 225 | 221 | 102 | 299 |
| Peak Pruritus NRS (≥4-point improvement)‡ | 41% | 12% | 36% | 10% | 59% | 20% |
| Figure 1: Proportion of Adult Subjects 18 Years of Age and Older with Moderate-to-Severe AD with ≥4-point Improvement on the Peak Pruritus NRS in SOLO 1* and SOLO 2* Studies (FAS)† | |
|---|---|
| SOLO 1 | SOLO 2 |
|
|
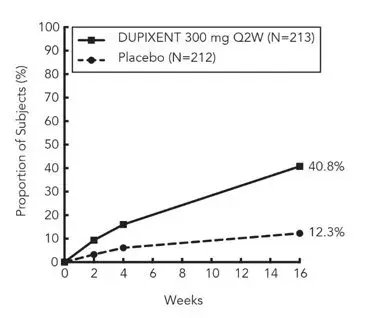 | 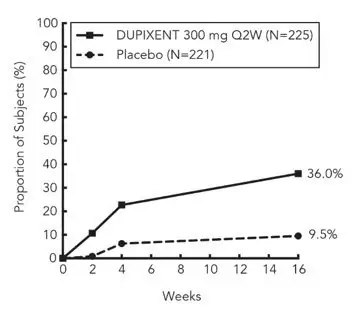 |
In CHRONOS, of the 421 subjects, 353 had been on study for 52 weeks at the time of data analysis. Of these 353 subjects, responders at Week 52 represent a mixture of subjects who maintained their efficacy from Week 16 (e.g., 53% of DUPIXENT IGA 0 or 1 responders at Week 16 remained responders at Week 52) and subjects who were non-responders at Week 16 who later responded to treatment (e.g., 24% of DUPIXENT IGA 0 or 1 non-responders at Week 16 became responders at Week 52). Results of supportive analyses of the 353 subjects in the DUPIXENT with concomitant TCS trial (CHRONOS) are presented in Table 11.
| DUPIXENT 300 mg Q2W + TCS | Placebo + TCS | |
|---|---|---|
|
||
| Number of Subjects* | 89 | 264 |
| Responder†,‡ at Week 16 and 52 | 22% | 7% |
| Responder at Week 16 but Non-responder at Week 52 | 20% | 7% |
| Non-responder at Week 16 and Responder at Week 52 | 13% | 6% |
| Non-responder at Week 16 and 52 | 44% | 80% |
| Overall Responder†,‡ Rate at Week 52 | 36% | 13% |
Treatment effects in subgroups (weight, age, gender, race, and prior treatment, including immunosuppressants) in SOLO 1, SOLO 2, and CHRONOS were generally consistent with the results in the overall study population.
In SOLO 1, SOLO 2, and CHRONOS, a third randomized treatment arm of DUPIXENT 300 mg QW did not demonstrate additional treatment benefit over DUPIXENT 300 mg Q2W.
Subjects in SOLO 1 and SOLO 2 who had an IGA 0 or 1 with a reduction of ≥2 points were re-randomized into SOLO CONTINUE (NCT02395133). SOLO CONTINUE evaluated multiple DUPIXENT monotherapy dose regimens for maintaining treatment response. The study included subjects randomized to continue with DUPIXENT 300 mg Q2W (62 subjects) or switch to placebo (31 subjects) for 36 weeks. IGA 0 or 1 responses at Week 36 were as follows: 33 (53%) in the Q2W group and 3 (10%) in the placebo group.
Pediatric Subjects 12 to 17 Years of Age with Atopic Dermatitis
The efficacy of DUPIXENT monotherapy in pediatric subjects 12 to 17 years of age was evaluated in a multicenter, randomized, double-blind, placebo-controlled trial (AD-1526; NCT03054428) in 251 pediatric subjects 12 to 17 years of age, with moderate-to-severe AD defined by an IGA score ≥3 (scale of 0 to 4), an EASI score ≥16 (scale of 0 to 72), and a minimum BSA involvement of ≥10%. Eligible subjects enrolled into this trial had previous inadequate response to topical medication.
Subjects in the DUPIXENT group with baseline weight of <60 kg received an initial dose of 400 mg at Week 0, followed by 200 mg Q2W for 16 weeks. Subjects with baseline weight of ≥60 kg received an initial dose of 600 mg at Week 0, followed by 300 mg Q2W for 16 weeks. Subjects were permitted to receive rescue treatment at the discretion of the investigator. Subjects who received rescue treatment were considered non-responders.
In AD-1526, the mean age was 14.5 years, the median weight was 59.4 kg, 41% of subjects were female, 63% were White, 15% were Asian, and 12% were Black. At baseline, 46% of subjects had an IGA score of 3 (moderate AD), 54% had an IGA score of 4 (severe AD), the mean BSA involvement was 57%, and 42% had received prior systemic immunosuppressants. Also, at baseline, the mean EASI score was 36, and the weekly averaged Peak Pruritus NRS was 8 on a scale of 0-10. Overall, 92% of subjects had at least one co-morbid allergic condition; 66% had allergic rhinitis, 54% had asthma, and 61% had food allergies.
The primary endpoint was the proportion of subjects with an IGA 0 (clear) or 1 (almost clear) and at least a 2-point improvement from baseline to Week 16. Other evaluated outcomes included the proportion of subjects with EASI-75 or EASI-90 (improvement of at least 75% or 90% in EASI from baseline, respectively), and reduction in itch as measured by the Peak Pruritus NRS (≥4-point improvement).
The efficacy results at Week 16 for AD-1526 are presented in Table 12.
| DUPIXENT†
200 mg (<60 kg) or 300 mg (≥60 kg) Q2W N=82* | Placebo N=85* |
|
|---|---|---|
|
||
| IGA 0 or 1‡,§ | 24% | 2% |
| EASI-75§ | 42% | 8% |
| EASI-90§ | 23% | 2% |
| Peak Pruritus NRS (≥4-point improvement)§ | 37% | 5% |
A greater proportion of subjects randomized to DUPIXENT achieved an improvement in the Peak Pruritus NRS compared to placebo (defined as ≥4-point improvement at Week 4). See Figure 2.
| Figure 2: Proportion of Pediatric Subjects 12 to 17 Years of Age with Moderate-to-Severe AD with ≥4-point Improvement on the Peak Pruritus NRS in AD-1526* (FAS)† |
|---|
|
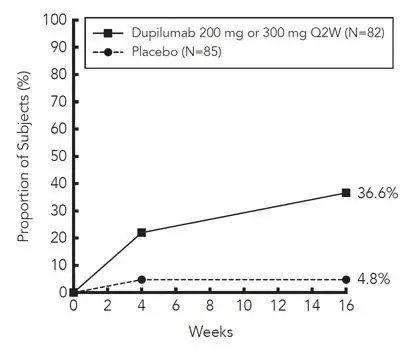 |
Pediatric Subjects 6 to 11 Years of Age with Atopic Dermatitis
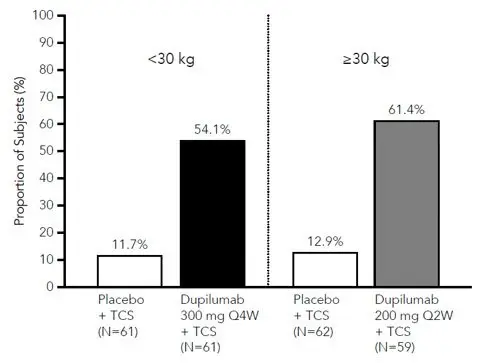
The efficacy and safety of DUPIXENT use concomitantly with TCS in pediatric subjects was evaluated in a multicenter, randomized, double-blind, placebo-controlled trial (AD-1652; NCT03345914) in 367 subjects 6 to 11 years of age, with AD defined by an IGA score of 4 (scale of 0 to 4), an EASI score ≥21 (scale of 0 to 72), and a minimum BSA involvement of ≥15%. Eligible subjects enrolled into this trial had previous inadequate response to topical medication. Enrollment was stratified by baseline weight (<30 kg; ≥30 kg).
Subjects in the DUPIXENT Q4W + TCS group received an initial dose of 600 mg on Day 1, followed by 300 mg Q4W from Week 4 to Week 12, regardless of weight. Subjects in the DUPIXENT Q2W + TCS group with baseline weight of <30 kg received an initial dose of 200 mg on Day 1, followed by 100 mg Q2W from Week 2 to Week 14, and subjects with baseline weight of ≥30 kg received an initial dose of 400 mg on Day 1, followed by 200 mg Q2W from Week 2 to Week 14. Subjects were permitted to receive rescue treatment at the discretion of the investigator. Subjects who received rescue treatment were considered non-responders.
In AD-1652, the mean age was 8.5 years, the median weight was 29.8 kg, 50% of subjects were female, 69% were White, 17% were Black, and 8% were Asian. At baseline, the mean BSA involvement was 58%, and 17% had received prior systemic non-steroidal immunosuppressants. Also, at baseline the mean EASI score was 37.9, and the weekly average of daily worst itch score was 7.8 on a scale of 0-10. Overall, 92% of subjects had at least one co-morbid allergic condition; 64% had food allergies, 63% had other allergies, 60% had allergic rhinitis, and 47% had asthma.
The primary endpoint was the proportion of subjects with an IGA 0 (clear) or 1 (almost clear) at Week 16. Other evaluated outcomes included the proportion of subjects with EASI-75 or EASI-90 (improvement of at least 75% or 90% in EASI from baseline, respectively), and reduction in itch as measured by the Peak Pruritus NRS (≥4-point improvement).
Table 13 presents the results by baseline weight strata for the approved dose regimens.
| DUPIXENT 300 mg Q4W† + TCS | Placebo + TCS | DUPIXENT 200 mg Q2W‡ + TCS | Placebo + TCS | |
|---|---|---|---|---|
| (N=61) | (N=61) | (N=59) | (N=62) | |
| <30 kg | <30 kg | ≥30 kg | ≥30 kg | |
|
||||
| IGA 0 or 1§,¶ | 30% | 13% | 39% | 10% |
| EASI-75¶ | 75% | 28% | 75% | 26% |
| EASI-90¶ | 46% | 7% | 36% | 8% |
| Peak Pruritus NRS (≥4-point improvement)¶ | 54% | 12% | 61% | 13% |
A greater proportion of subjects randomized to DUPIXENT + TCS achieved an improvement in the Peak Pruritus NRS compared to placebo + TCS (defined as ≥4-point improvement at Week 16). See Figure 3.
| Figure 3: Proportion of Pediatric Subjects 6 to 11 Years of Age with AD with ≥4-point Improvement on the Peak Pruritus NRS at Week 16 in AD-1652* (FAS)† |
|---|
|
 |
14.2 Asthma
The asthma development program for patients aged 12 years and older included three randomized, double-blind, placebo-controlled, parallel-group, multicenter trials (DRI12544 (NCT01854047), QUEST (NCT02414854), and VENTURE (NCT02528214)) of 24 to 52 weeks in treatment duration which enrolled a total of 2888 subjects. Subjects enrolled in DRI12544 and QUEST were required to have a history of 1 or more asthma exacerbations that required treatment with systemic corticosteroids or emergency department visit or hospitalization for the treatment of asthma in the year prior to trial entry. Subjects enrolled in VENTURE required dependence on daily oral corticosteroids in addition to regular use of high-dose inhaled corticosteroids plus an additional controller(s). In all 3 trials, subjects were enrolled without requiring a minimum baseline blood eosinophil count. In QUEST and VENTURE, subjects with screening blood eosinophil level of >1500 cells/mcL (<1.3%) were excluded. DUPIXENT was administered as add-on to background asthma treatment. Subjects continued background asthma therapy throughout the duration of the studies, except in VENTURE in which OCS dose was tapered as described below.
VENTURE
VENTURE was a 24-week oral corticosteroid-reduction study in 210 adult and pediatric subjects 15 years of age and older with asthma who required daily oral corticosteroids in addition to regular use of high dose inhaled corticosteroids plus an additional controller. After optimizing the OCS dose during the screening period, subjects received 300 mg DUPIXENT (N=103) or placebo (N=107) once Q2W for 24 weeks following an initial dose of 600 mg or placebo. Subjects continued to receive their existing asthma medicine during the study; however, their OCS dose was reduced every 4 weeks during the OCS reduction phase (Week 4-20), as long as asthma control was maintained. The primary endpoint was the percent reduction of oral corticosteroid dose at Weeks 20 to 24 compared with the baseline dose, while maintaining asthma control in the overall population (unrestricted by minimum baseline blood eosinophils count). Additional secondary endpoints included the annualized rate of severe exacerbation events during treatment period and responder rate in the ACQ-5 and AQLQ(S) scores.
The demographics and baseline characteristics of these 3 trials are provided in Table 15 below.
| Parameter | DRI12544 (N=776) | QUEST (N=1902) | VENTURE (N=210) |
|---|---|---|---|
| ICS = inhaled corticosteroid; FEV1 = Forced expiratory volume in 1 second; AD = atopic dermatitis; NP = nasal polyposis; AR = allergic rhinitis; FeNO = fraction of exhaled nitric oxide | |||
| Mean age (years) (SD) | 49 (13) | 48 (15) | 51 (13) |
| % Female | 63 | 63 | 61 |
| % White | 78 | 83 | 94 |
| Duration of Asthma (years), mean (± SD) | 22 (15) | 21 (15) | 20 (14) |
| Never smoked (%) | 77 | 81 | 81 |
| Mean exacerbations in previous year (± SD) | 2.2 (2.1) | 2.1 (2.2) | 2.1 (2.2) |
| High dose ICS use (%) | 50 | 52 | 89 |
| Pre-dose FEV1 (L) at baseline (± SD) | 1.84 (0.54) | 1.78 (0.60) | 1.58 (0.57) |
| Mean percent predicted FEV1 at baseline (%) (± SD) | 61 (11) | 58 (14) | 52 (15) |
| % Reversibility (± SD) | 27 (15) | 26 (22) | 19 (23) |
| Atopic Medical History % Overall (AD %, NP %, AR %) | 73 (8, 11, 62) | 78 (10, 13, 69) | 72 (8, 21, 56) |
| Mean FeNO ppb (± SD) | 39 (35) | 35 (33) | 38 (31) |
| Mean total IgE IU/mL (± SD) | 435 (754) | 432 (747) | 431 (776) |
| Mean baseline blood Eosinophil count (± SD) cells/mcL | 350 (430) | 360 (370) | 350 (310) |
Exacerbations
DRI12544 and QUEST evaluated the frequency of severe asthma exacerbations defined as deterioration of asthma requiring the use of systemic corticosteroids for at least 3 days or hospitalization or emergency room visit due to asthma that required systemic corticosteroids. In the primary analysis population (subjects with baseline blood eosinophil count of ≥300 cells/mcL in DRI12544 and the overall population in QUEST), subjects receiving either DUPIXENT 200 mg or 300 mg Q2W had significant reductions in the rate of asthma exacerbations compared to placebo. In the overall population in QUEST, the rate of severe exacerbations was 0.46 and 0.52 for DUPIXENT 200 mg Q2W and 300 mg Q2W, respectively, compared to matched placebo rates of 0.87 and 0.97. The rate ratio of severe exacerbations compared to placebo was 0.52 (95% CI: 0.41, 0.66) and 0.54 (95% CI: 0.43, 0.68) for DUPIXENT 200 mg Q2W and 300 mg Q2W, respectively. Results in subjects with baseline blood eosinophil counts ≥300 cells/mcL in DRI12544 and QUEST are shown in Table 16.
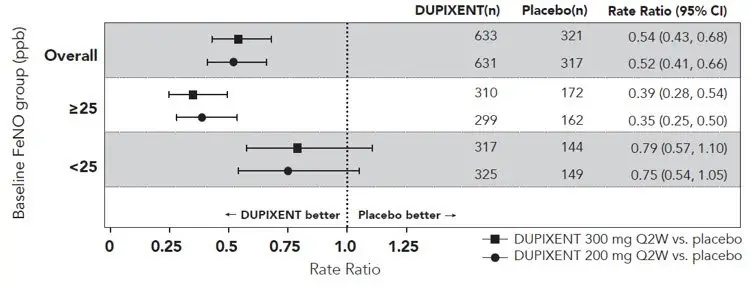
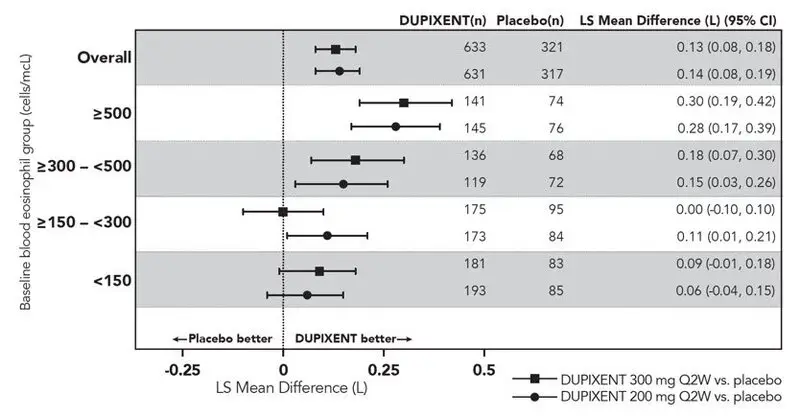
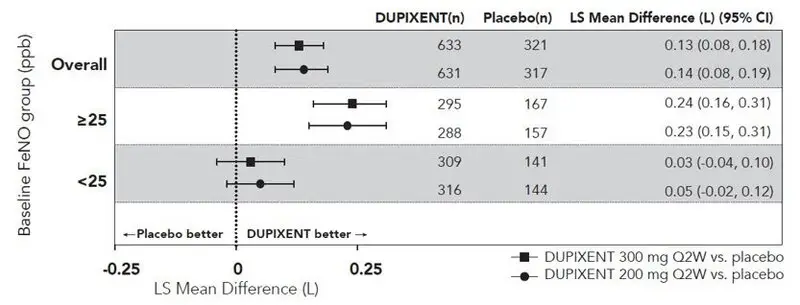
Response rates by baseline blood eosinophils and baseline FeNO for QUEST are shown for the overall population in Figure 4 and Figure 5, respectively. Elevation of FeNO can be a marker of the eosinophilic asthma phenotype when supported by clinical data. Pre-specified subgroup analyses of DRI12544 and QUEST demonstrated that there were greater reductions in severe exacerbations in subjects with higher baseline blood eosinophil levels (≥150 cells/mcL) or FeNO (≥25 ppb). In QUEST, reductions in exacerbations were significant in the subgroup of subjects with baseline blood eosinophils ≥150 cells/mcL. In subjects with baseline blood eosinophil count <150 cells/mcL and FeNO <25 ppb, similar severe exacerbation rates were observed between DUPIXENT and placebo.
In QUEST, the estimated rate ratio of exacerbations leading to hospitalizations and/or emergency room visits versus placebo was 0.53 (95% CI: 0.28, 1.03) and 0.74 (95% CI: 0.32, 1.70) with DUPIXENT 200 mg or 300 mg Q2W, respectively.
| Trial | Treatment | Baseline Blood EOS ≥300 cells/mcL (primary analysis population, DRI12544) |
||
|---|---|---|---|---|
| N | Rate (95% CI) | Rate Ratio (95% CI) |
||
| DRI12544 | DUPIXENT 200 mg Q2W | 65 | 0.30 (0.13, 0.68) | 0.29 (0.11, 0.76) |
| DUPIXENT 300 mg Q2W | 64 | 0.20 (0.08, 0.52) | 0.19 (0.07, 0.56) |
|
| Placebo | 68 | 1.04 (0.57, 1.90) | ||
| QUEST | DUPIXENT 200 mg Q2W | 264 | 0.37 (0.29, 0.48) | 0.34 (0.24, 0.48) |
| Placebo | 148 | 1.08 (0.85, 1.38) | ||
| DUPIXENT 300 mg Q2W | 277 | 0.40 (0.32, 0.51) | 0.33 (0.23, 0.45) |
|
| Placebo | 142 | 1.24 (0.97, 1.57) | ||
Figure 4: Relative Risk in Annualized Event Rate of Severe Exacerbations across Baseline Blood Eosinophil Count (cells/mcL) in Subjects with Moderate-to-Severe Asthma (QUEST)
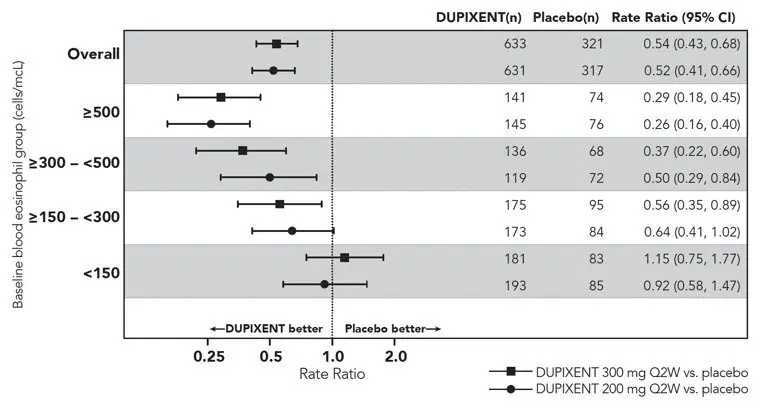
Figure 5: Relative Risk in Annualized Event Rate of Severe Exacerbations across Baseline FeNO Group (ppb) in Subjects with Moderate-to-Severe Asthma (QUEST)
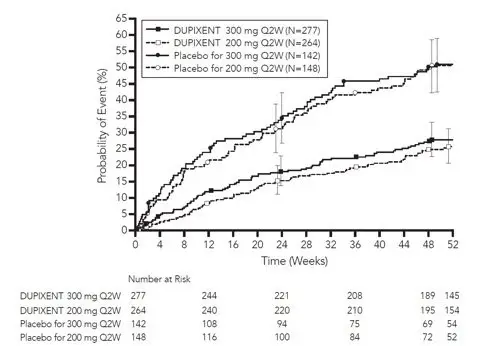
The time to first exacerbation was longer for the subjects receiving DUPIXENT compared to placebo in QUEST (Figure 6).
| Figure 6: Kaplan Meier Incidence Curve for Time to First Severe Exacerbation in Subjects with Moderate-to-Severe Asthma with Baseline Blood Eosinophils ≥300 cells/mcL (QUEST)* |
|---|
|
 |
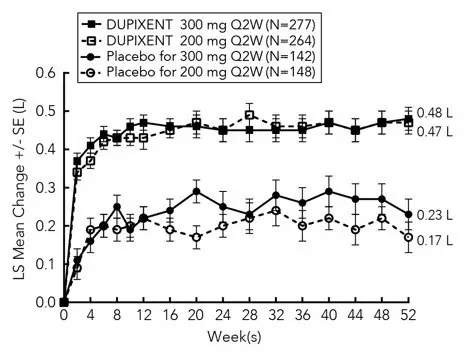
Lung Function
Significant increases in pre-bronchodilator FEV1 were observed at Week 12 for DRI12544 and QUEST in the primary analysis populations (subjects with baseline blood eosinophil count of ≥300 cells/mcL in DRI12544 and the overall population in QUEST). In the overall population in QUEST, the FEV1 LS mean change from baseline was 0.32 L (21%) and 0.34 L (23%) for DUPIXENT 200 mg Q2W and 300 mg Q2W, respectively, compared to matched placebo means of 0.18 L (12%) and 0.21 L (14%). The mean treatment difference versus placebo was 0.14 L (95% CI: 0.08, 0.19) and 0.13 L (95% CI: 0.08, 0.18) for DUPIXENT 200 mg Q2W and 300 mg Q2W, respectively. Results in subjects with baseline blood eosinophil counts ≥300 cells/mcL in DRI12544 and QUEST are shown in Table 17.
Improvements in FEV1 by baseline blood eosinophils and baseline FeNO for QUEST are shown in Figure 7 and 8, respectively. Subgroup analysis of DRI12544 and QUEST demonstrated greater improvement in subjects with higher baseline blood eosinophils (≥150 cells/mcL) or FeNO (≥25 ppb). In subjects with baseline blood eosinophil count <150 cells/mcL and FeNO <25 ppb, similar differences in FEV1 were observed between DUPIXENT and placebo.
Mean changes in FEV1 over time in QUEST are shown in Figure 9.
| Trial | Treatment | Baseline Blood EOS ≥300 cells/mcL (primary analysis population, DRI12544) |
||
|---|---|---|---|---|
| N | LS Mean Change from baseline L (%) | LS Mean Difference vs. placebo (95% CI) |
||
| DRI12544 | DUPIXENT 200 mg Q2W | 65 | 0.43 (25.9) | 0.26 (0.11, 0.40) |
| DUPIXENT 300 mg Q2W | 64 | 0.39 (25.8) | 0.21 (0.06, 0.36) |
|
| Placebo | 68 | 0.18 (10.2) | ||
| QUEST | DUPIXENT 200 mg Q2W | 264 | 0.43 (29.0) | 0.21 (0.13, 0.29) |
| Placebo | 148 | 0.21 (15.6) | ||
| DUPIXENT 300 mg Q2W | 277 | 0.47 (32.5) | 0.24 (0.16, 0.32) |
|
| Placebo | 142 | 0.22 (14.4) | ||
Pediatric Subjects 6 to 11 Years of Age with Asthma
The efficacy and safety of DUPIXENT in pediatric subjects was evaluated in a 52-week multicenter, randomized, double-blind, placebo-controlled study (VOYAGE; NCT02948959) in 408 subjects 6 to 11 years of age, with moderate-to-severe asthma on a medium or high-dose ICS and a second controller medication or high-dose ICS alone. Subjects were required to have a history of 1 or more asthma exacerbation(s) that required treatment with systemic corticosteroids or emergency department visit or hospitalization for the treatment of asthma in the year prior to trial entry. Subjects were randomized to DUPIXENT (N=273) or matching placebo (N=135) every other week based on body weight <30 kg (100 mg Q2W) or ≥30 kg (200 mg Q2W). The effectiveness of DUPIXENT 300 mg Q4W was extrapolated from efficacy of 100 mg Q2W in VOYAGE with support from population pharmacokinetic analyses showing higher drug exposure levels with 300 mg Q4W [see Pediatric Use (8.4) and Pharmacokinetics (12.3)].
The primary endpoint was the annualized rate of severe asthma exacerbation events during the 52-week placebo-controlled period. Severe asthma exacerbations were defined as deterioration of asthma requiring the use of systemic corticosteroids for at least 3 days or hospitalization or emergency room visit due to asthma that required systemic corticosteroids. The key secondary endpoint was the change from baseline in pre-bronchodilator FEV1 percent predicted at Week 12. Additional secondary endpoints included mean change from baseline and responder rates in the ACQ-7-IA (Asthma Control Questionnaire-7-Interviewer Administered) and PAQLQ(S)-IA (Pediatric Asthma Quality of Life Questionnaire with Standardized Activities Interviewer Administered) scores.
The demographics and baseline characteristics for VOYAGE are provided in Table 18 below.
| Parameter | VOYAGE (N=408) |
|---|---|
| ICS = inhaled corticosteroid; FEV1 = Forced expiratory volume in 1 second; AD = atopic dermatitis; AR = allergic rhinitis; FeNO = fraction of exhaled nitric oxide | |
| Mean age (years) (SD) | 9 (2) |
| % Female | 36 |
| % White | 88 |
| Mean body weight (kg) | 36 |
| Mean exacerbations in previous year (± SD) | 2.4 (2.2) |
| High dose ICS use (%) | 44 |
| Pre-dose FEV1 (L) at baseline (± SD) | 1.48 (0.41) |
| Mean percent predicted FEV1 (%) (±SD) | 78 (15) |
| Mean % Reversibility (± SD) | 20 (21) |
| Atopic Medical History % Overall (AD %, AR %) | 92 (36, 82) |
| Mean FeNO ppb (± SD) | 28 (24) |
| % subjects with FeNO ppb ≥20 | 50 |
| Median total IgE IU/mL (±SD) | 792 (1093) |
| Mean baseline Eosinophil count (± SD) cells/mcL | 502 (395) |
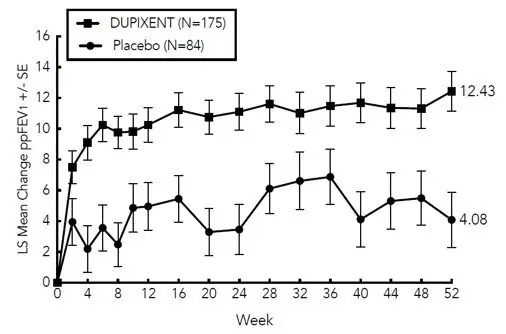
DUPIXENT significantly reduced the annualized rate of severe asthma exacerbation events during the 52-week treatment period compared to placebo in populations with an eosinophilic phenotype as indicated by elevated blood eosinophils and/or the population with elevated FeNO. Subgroup analyses for results of DUPIXENT treatment based upon either baseline eosinophil level or baseline FeNO level were similar to the pediatric (12 to 17 years of age) and adult trials and are described for the adult and pediatric (12 to 17 years of age) asthma population above. In subjects with baseline blood eosinophil count <150 cells/mcL and FeNO <20 ppb, similar severe asthma exacerbation rates were observed between DUPIXENT and placebo.
Significant improvements in percent predicted pre-bronchodilator FEV1 were observed at Week 12. Significant improvements in percent predicted FEV1 were observed as early as Week 2 and were maintained through Week 52 in VOYAGE (Figure 10).
The efficacy results for VOYAGE are presented in Table 19.
| Treatment | EOS ≥300 cells/mcL* | ||
|---|---|---|---|
|
|||
| Annualized Severe Exacerbations Rate over 52 Weeks | |||
| N | Rate (95% CI) | Rate Ratio (95% CI) |
|
| DUPIXENT 100 mg Q2W (<30 kg)/ 200 mg Q2W (≥30 kg) | 175 | 0.24 (0.16, 0.35) | 0.35 (0.22, 0.56) |
| Placebo | 84 | 0.67 (0.47, 0.95) | |
| Mean Change from Baseline in Percent Predicted FEV1 at Week 12 | |||
| N | LS mean Δ from Baseline | LS mean difference vs. Placebo (95% CI) | |
| DUPIXENT 100 mg Q2W (<30 kg)/ 200 mg Q2W (≥30 kg) | 168 | 10.15 | 5.32 (1.76, 8.88) |
| Placebo | 80 | 4.83 | |
Figure 10: Mean Change from Baseline in Percent Predicted Pre-bronchodilator FEV1 (L) Over Time in Pediatric Subjects 6 to 11 Years of Age in VOYAGE (Baseline Blood Eosinophils ≥300 cells/mcL)
Improvements were also observed for ACQ-7-IA and PAQLQ(S)-IA at Week 24 and were sustained at Week 52. Greater responder rates were observed for ACQ-7-IA and PAQLQ(S)-IA compared to placebo at Week 24. The responder rate was defined as an improvement in score of 0.5 or more (scale range 0-6 for ACQ-7-IA and 1-7 for PAQLQ(S)-IA). In the subgroup of subjects with baseline blood eosinophil count ≥300 cells/mcL, DUPIXENT led to a higher proportion of subjects with a response in ACQ-7-IA (80.6% versus 64.3% for placebo) with an OR of 2.79 (95% CI: 1.43, 5.44), and in PAQLQ(S)-IA (72.8% versus 63.0% for placebo) with an OR of 1.84 (95% CI: 0.92, 3.65) at Week 24.
14.3 Chronic Rhinosinusitis with Nasal Polyposis
The chronic rhinosinusitis with nasal polyposis (CRSwNP) development program included two randomized, double-blind, parallel-group, multicenter, placebo-controlled studies (SINUS-24 (NCT02912468) and SINUS-52 (NCT02898454)) in 724 adult subjects 18 years of age and older on background intranasal corticosteroids (INCS). These studies included subjects with CRSwNP despite prior sino-nasal surgery or treatment with, or who were ineligible to receive or were intolerant to, systemic corticosteroids in the past 2 years. Subjects with chronic rhinosinusitis without nasal polyposis were not included in these trials. Rescue with systemic corticosteroids or surgery was allowed during the studies at the investigator's discretion. In SINUS-24, a total of 276 subjects were randomized to receive either 300 mg DUPIXENT (N=143) or placebo (N=133) every other week for 24 weeks. In SINUS-52, 448 subjects were randomized to receive either 300 mg DUPIXENT (N=150) every other week for 52 weeks, 300 mg DUPIXENT (N=145) every other week until Week 24 followed by 300 mg DUPIXENT every 4 weeks until Week 52, or placebo (N=153). All subjects had evidence of sinus opacification on the Lund Mackay (LMK) sinus CT scan and 73% to 90% of subjects had opacification of all sinuses. Subjects were stratified based on their histories of prior surgery and co-morbid asthma/nonsteroidal anti-inflammatory drug exacerbated respiratory disease (NSAID-ERD). A total of 63% of subjects reported previous sinus surgery, with a mean number of 2.0 prior surgeries, 74% used systemic corticosteroids in the previous 2 years with a mean number of 1.6 systemic corticosteroid courses in the previous 2 years, 59% had co-morbid asthma, and 28% had NSAID-ERD.
The co-primary efficacy endpoints were change from baseline to Week 24 in bilateral endoscopic nasal polyps score (NPS; 0-8 scale) as graded by central blinded readers, and change from baseline to Week 24 in nasal congestion/obstruction score averaged over 28 days (NC; 0-3 scale), as determined by subjects using a daily diary. For NPS, polyps on each side of the nose were graded on a categorical scale (0=no polyps; 1=small polyps in the middle meatus not reaching below the inferior border of the middle turbinate; 2=polyps reaching below the lower border of the middle turbinate; 3=large polyps reaching the lower border of the inferior turbinate or polyps medial to the middle turbinate; 4=large polyps causing complete obstruction of the inferior nasal cavity). The total score was the sum of the right and left scores. Nasal congestion was rated daily by the subjects on a 0 to 3 categorical severity scale (0=no symptoms; 1=mild symptoms; 2=moderate symptoms; 3=severe symptoms).
In both studies, key secondary end-points at Week 24 included change from baseline in: LMK sinus CT scan score, daily loss of smell, and 22-item sino-nasal outcome test (SNOT-22). The LMK sinus CT scan score evaluated the opacification of each sinus using a 0 to 2 scale (0=normal; 1=partial opacification; 2=total opacification) deriving a maximum score of 12 per side and a total maximum score of 24 (higher scores indicate more opacification). Loss of smell was scored reflectively by the subject every morning on a 0-3 scale (0=no symptoms, 1=mild symptoms, 2=moderate symptoms, 3=severe symptoms). SNOT-22 includes 22 items assessing symptoms and symptom impact associated with CRSwNP with each item scored from 0 (no problem) to 5 (problem as bad as it can be) with a global score ranging from 0 to 110. SNOT-22 had a 2 week recall period. In the pooled efficacy results, the reduction in the proportion of subjects rescued with systemic corticosteroids and/or sino-nasal surgery (up to Week 52) were evaluated.
The demographics and baseline characteristics of these 2 trials are provided in Table 20 below.
| Parameter | SINUS-24 (N=276) | SINUS-52 (N=448) |
|---|---|---|
| SD = standard deviation; AM = morning; NPS = nasal polyps score; SNOT-22 = 22-item sino-nasal outcome test; NSAID-ERD = asthma/nonsteroidal anti-inflammatory drug exacerbated respiratory disease | ||
|
||
| Mean age (years) (SD) | 50 (13) | 52 (12) |
| % Male | 57 | 62 |
| Mean CRSwNP duration (years) (SD) | 11 (9) | 11 (10) |
| Subjects with ≥1 prior surgery (%) | 72 | 58 |
| Subjects with systemic corticosteroid use in the previous 2 years (%) | 65 | 80 |
| Mean Bilateral endoscopic NPS* (SD), range 0-8 | 5.8 (1.3) | 6.1 (1.2) |
| Mean Nasal congestion (NC) score* (SD), range 0-3 | 2.4 (0.6) | 2.4 (0.6) |
| Mean LMK sinus CT total score* (SD), range 0-24 | 19 (4.4) | 18 (3.8) |
| Mean loss of smell score *(AM), (SD) range 0-3 | 2.7 (0.5) | 2.8 (0.5) |
| Mean SNOT-22 total score* (SD), range 0-110 | 49.4 (20.2) | 51.9 (20.9) |
| Mean blood eosinophils (cells/mcL) (SD) | 440 (330) | 430 (350) |
| Mean total IgE IU/mL (SD) | 212 (276) | 240 (342) |
| Atopic Medical History % Overall | 75 | 82 |
| Asthma (%) | 58 | 60 |
| NSAID-ERD (%) | 30 | 27 |
Clinical Response (SINUS-24 and SINUS-52)
The results for primary endpoints in CRSwNP studies are presented in Table 21.
| SINUS-24 | SINUS-52 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Placebo (n=133) | DUPIXENT 300 mg Q2W (n=143) | LS mean difference vs. Placebo (95% CI) | Placebo (n=153) | DUPIXENT 300 mg Q2W (n=295) | LS mean difference vs. Placebo (95% CI) | |||||
| Primary Endpoints at Week 24 | ||||||||||
| Scores | Baseline mean | LS mean change | Baseline mean | LS mean change | Baseline mean | LS mean change | Baseline mean | LS mean change | ||
| A reduction in score indicates improvement. NPS = nasal polyps score; NC = nasal congestion/obstruction |
||||||||||
| NPS | 5.86 | 0.17 | 5.64 | -1.89 | -2.06 (-2.43, -1.69) | 5.96 | 0.10 | 6.18 | -1.71 | -1.80 (-2.10, -1.51) |
| NC | 2.45 | -0.45 | 2.26 | -1.34 | -0.89 (-1.07, -0.71) | 2.38 | -0.38 | 2.46 | -1.25 | -0.87 (-1.03, -0.71) |
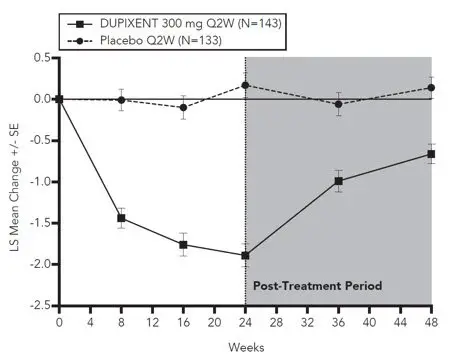
Statistically significant efficacy was observed in SINUS-52 with regard to improvement in bilateral endoscopic NPS score at week 24 and week 52 (see Figure 11).
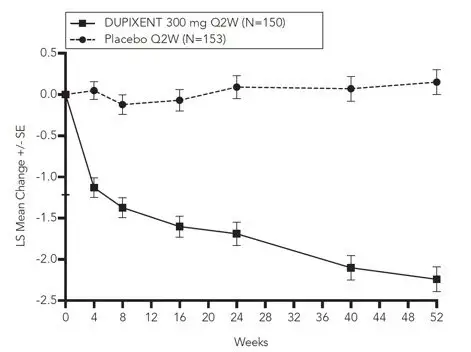
Similar results were seen in SINUS-24 at Week 24. In the post-treatment period when subjects were off DUPIXENT, the treatment effect diminished over time (see Figure 12).
At Week 52, the LS mean difference for nasal congestion in the DUPIXENT group versus placebo was -0.98 (95% CI -1.17, -0.79). In both studies, significant improvements in nasal congestion were observed as early as the first assessment at Week 4. The LS mean difference for nasal congestion at Week 4 in the DUPIXENT group versus placebo was -0.41 (95% CI: -0.52, -0.30) in SINUS-24 and -0.37 (95% CI: -0.46, -0.27) in SINUS-52.
A significant decrease in the LMK sinus CT scan score was observed. The LS mean difference for LMK sinus CT scan score at Week 24 in the DUPIXENT group versus placebo was -7.44 (95% CI: -8.35, -6.53) in SINUS-24 and -5.13 (95% CI: -5.80, -4.46) in SINUS-52. At Week 52, in SINUS-52 the LS mean difference for LMK sinus CT scan score in the DUPIXENT group versus placebo was -6.94 (95% CI: -7.87, -6.01).
Dupilumab significantly improved the loss of smell compared to placebo. The LS mean difference for loss of smell at Week 24 in the DUPIXENT group versus placebo was -1.12 (95% CI: -1.31, -0.93) in SINUS-24 and -0.98 (95% CI: -1.15, -0.81) in SINUS-52. At Week 52, the LS mean difference for loss of smell in the DUPIXENT group versus placebo was -1.10 (95% CI -1.31, -0.89). In both studies, significant improvements in daily loss of smell severity were observed as early as the first assessment at Week 4.
Dupilumab significantly decreased sino-nasal symptoms as measured by SNOT-22 compared to placebo. The LS mean difference for SNOT-22 at Week 24 in the DUPIXENT group versus placebo was -21.12 (95% CI: -25.17, -17.06) in SINUS-24 and -17.36 (95% CI: -20.87, -13.85) in SINUS-52. At Week 52, the LS mean difference in the DUPIXENT group versus placebo was -20.96 (95% CI -25.03, -16.89).
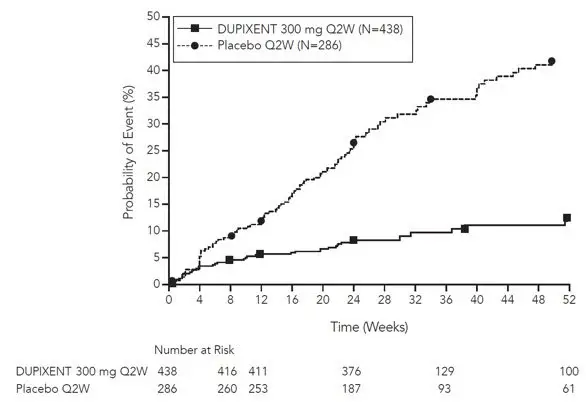
In the pre-specified multiplicity-adjusted pooled analysis of two studies, treatment with DUPIXENT resulted in significant reduction of systemic corticosteroid use and need for sino-nasal surgery versus placebo (HR of 0.24; 95% CI: 0.17, 0.35) (see Figure 13). The proportion of subjects who required systemic corticosteroids was reduced by 74% (HR of 0.26; 95% CI: 0.18, 0.38). The total number of systemic corticosteroid courses per year was reduced by 75% (RR of 0.25; 95% CI: 0.17, 0.37). The proportion of subjects who required surgery was reduced by 83% (HR of 0.17; 95% CI: 0.07, 0.46).
The effects of DUPIXENT on the primary endpoints of NPS and nasal congestion and the key secondary endpoint of LMK sinus CT scan score were consistent in subjects with prior surgery and without prior surgery.
In subjects with co-morbid asthma, improvements in pre-bronchodilator FEV1 were similar to subjects in the asthma program.
14.4 Eosinophilic Esophagitis
A single randomized, double-blind, parallel-group, multicenter, placebo-controlled trial, including two 24-week treatment periods (Parts A and B), was conducted in adult and pediatric subjects 12 to 17 years of age, weighing at least 40 kg, with EoE (NCT03633617). In both parts, subjects were randomized to receive 300 mg DUPIXENT every week or placebo. Eligible subjects had ≥15 intraepithelial eosinophils per high-power field (eos/hpf) following a treatment course of a proton pump inhibitor (PPI) either prior to or during the screening period and symptoms of dysphagia as measured by the Dysphagia Symptom Questionnaire (DSQ). At baseline, 43% of subjects in Part A and 37% of subjects in Part B had a history of prior esophageal dilations.
Demographics and baseline characteristics were similar in Parts A and B. A total of 81 subjects (61 adults and 20 pediatric subjects) were enrolled in Part A and 159 subjects (107 adults and 52 pediatric subjects) were enrolled in Part B. The mean age in years was 32 years (range 13 to 62 years) in Part A and 28 years (range 12 to 66 years) in Part B. The majority of subjects were male (60% in Part A and 68% in Part B) and White (96% in Part A and 90% in Part B). The mean baseline DSQ score (SD) was 33.6 (12.4) in Part A and 37.2 (10.7) in Part B.
The coprimary efficacy endpoints in Parts A and B were the (1) proportion of subjects achieving histological remission defined as peak esophageal intraepithelial eosinophil count of ≤6 eos/hpf at Week 24; and (2) the absolute change in the subject-reported DSQ score from baseline to Week 24.
Efficacy results for Parts A and B are presented in Table 22.
| Part A | Part B | |||||
|---|---|---|---|---|---|---|
| DUPIXENT 300 mg QW* | Placebo* | Difference vs. Placebo (95% CI)* | DUPIXENT 300 mg QW* | Placebo* | Difference vs. Placebo (95% CI)* |
|
| N = 42 | N = 39 | N = 80 | N = 79 | |||
|
||||||
| Co-primary Endpoints | ||||||
| Proportion of subjects achieving histological remission (peak esophageal intraepithelial eosinophil count ≤6 eos/hpf), n (%) | 25 (59.5) | 2 (5.1) | 57.0 (40.9, 73.1) | 47 (58.8) | 5 (6.3) | 53.5 (41.2, 65.8) |
| Absolute change from baseline in DSQ score (0-84†), LS mean (SE) | -21.9 (2.5) | -9.6 (2.8) | -12.3 (-19.1, -5.5) | -23.8 (1.9) | -13.9 (1.9) | -9.9 (-14.8, -5.0) |
In Parts A and B, a greater proportion of subjects randomized to DUPIXENT achieved histological remission (peak esophageal intraepithelial eosinophil count ≤6 eos/hpf) compared to placebo. Treatment with DUPIXENT also resulted in a significant improvement in LS mean change in DSQ score compared to placebo at Week 24. The results of the anchor-based analyses that incorporated the subjects' perspectives indicated that the observed improvement in dysphagia from Parts A and B is representative of a clinically meaningful within-subject improvement.
14.5 Prurigo Nodularis
The prurigo nodularis (PN) development program included two 24-week randomized, double-blind, placebo-controlled, multicenter, parallel-group trials (PRIME (NCT04183335) and PRIME 2 (NCT04202679)) in 311 adult subjects 18 years of age and older with pruritus (WI-NRS ≥ 7 on a scale of 0 to 10) and greater than or equal to 20 nodular lesions. PRIME and PRIME 2 assessed the effect of DUPIXENT on pruritus improvement as well as its effect on PN lesions.
In these two trials, subjects received either subcutaneous DUPIXENT 600 mg (two 300 mg injections) on day 1, followed by 300 mg once every other week (Q2W) for 24 weeks, or matching placebo.
In these trials, the mean age was 49.5 years, the median weight was 71 kg, 65% of subjects were female, 57% were White, 6% were Black, and 34% were Asian. At baseline, the mean Worst Itch-Numeric Rating Scale (WI-NRS) was 8.5, 66% had 20 to 100 nodules (moderate), and 34% had greater than 100 nodules (severe). Eleven percent (11%) of subjects were taking stable doses of antidepressants at baseline and were instructed to continue taking these medications during the trial. Forty-three percent (43%) had a history of atopy (defined as having a medical history of AD, allergic rhinitis/rhinoconjunctivitis, asthma, or food allergy).
The WI-NRS is comprised of a single item, rated on a scale from 0 ("no itch") to 10 ("worst imaginable itch"). Subjects were asked to rate the intensity of their worst pruritus (itch) over the past 24 hours using this scale. The Investigator's Global Assessment for Prurigo Nodularis-Stage (IGA PN-S) is a scale that measures the approximate number of nodules using a 5-point scale from 0 (clear) to 4 (severe).
Efficacy was assessed with the proportion of subjects with improvement (reduction) in WI-NRS by ≥4 points, the proportion of subjects with IGA PN-S 0 or 1 (the equivalent of 0-5 nodules), and the proportion of subjects who achieved a response in both WI-NRS and IGA PN-S per the criteria described above.
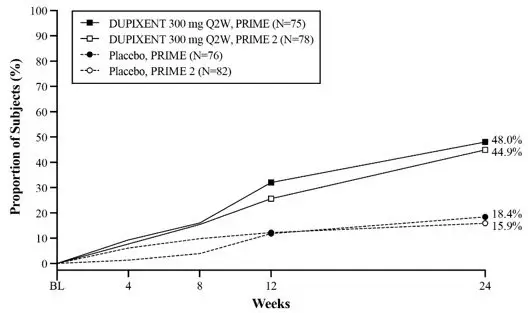
The efficacy results for PRIME and PRIME2 are presented in Table 23 and Figures 14, 15 and 16.
| PRIME | PRIME2 | |||||
|---|---|---|---|---|---|---|
| Placebo (N=76) | DUPIXENT 300 mg Q2W (N=75) | Difference (95% CI) for DUPIXENT vs. Placebo | Placebo (N=82) | DUPIXENT 300 mg Q2W (N=78) | Difference (95% CI) for DUPIXENT vs. Placebo | |
|
||||||
| Proportion of subjects with both an improvement (reduction) in WI-NRS by ≥4 points from baseline to Week 24 and an IGA PN-S 0 or 1 at Week 24 * | 9.2% | 38.7% | 29.6% (16.4, 42.8) | 8.5% | 32.1% | 25.5% (13.1, 37.9) |
| Proportion of subjects with improvement (reduction) in WI-NRS by ≥4 points from baseline at Week 24* | 18.4% | 60.0% | 42.7% (27.8, 57.7) | 19.5% | 57.7% | 42.6% (29.1, 56.1) |
| Proportion of subjects with IGA PN-S 0 or 1 at Week 24 * | 18.4% | 48.0% | 28.3% (13.4, 43. 2) | 15.9% | 44.9% | 30.8% (16. 4, 45.2) |
| Proportion of subjects with improvement (reduction) in WI-NRS by ≥4 points from baseline at Week 12 * | 15.8%† | 44.0%† | 29.2% (14.5, 43.8)† | 22.0% | 37.2% | 16.8% (2.3, 31.2) |
Figure 14: Proportion of Adult Subjects with PN with Both WI-NRS ≥4-point Improvement and IGA PN-S 0 or 1 Over Time in PRIME and PRIME 2
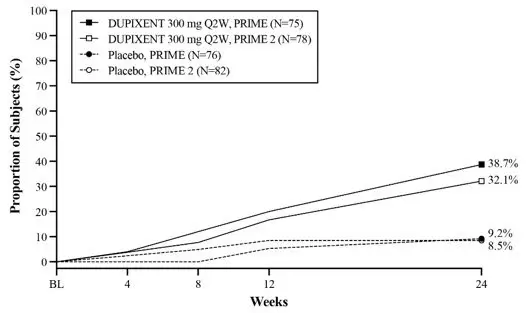
Figure 15: Proportion of Adult Subjects with PN with WI-NRS ≥4-point Improvement Over Time in PRIME and PRIME2
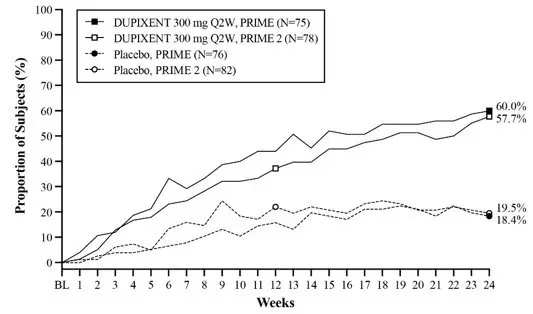
Figure 16: Proportion of Adult Subjects with IGA PN-S 0 or 1 Over Time in PRIME and PRIME 2
The efficacy data did not show differential treatment effect across demographic subgroups.
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information and Instructions for Use).
| This Patient Information has been approved by the U.S. Food and Drug Administration. | Revised: October 2022 | |||
| Patient Information DUPIXENT® (DU-pix-ent) (dupilumab) injection, for subcutaneous use |
||||
| What is DUPIXENT?
DUPIXENT is a prescription medicine used: |
||||
|
||||
|
||||
| Do not use DUPIXENT if you are allergic to dupilumab or to any of the ingredients in DUPIXENT. See the end of this leaflet for a complete list of ingredients in DUPIXENT. | ||||
Before using DUPIXENT, tell your healthcare provider about all your medical conditions, including if you:
Especially tell your healthcare provider if you:
|
||||
How should I use DUPIXENT?
|
||||
| What are the possible side effects of DUPIXENT? DUPIXENT can cause serious side effects, including:
|
||||
|
|
|
||
|
||||
|
| |||
|
||||
|
|
|||
The following additional side effects have been reported with DUPIXENT:
These are not all of the possible side effects of DUPIXENT. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||||
How should I store DUPIXENT?
|
||||
| General information about the safe and effective use of DUPIXENT.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use DUPIXENT for a condition for which it was not prescribed. Do not give DUPIXENT to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider for information about DUPIXENT that is written for health professionals. |
||||
| What are the ingredients in DUPIXENT?
Active ingredient: dupilumab Inactive ingredients: L-arginine hydrochloride, L-histidine, polysorbate 80, sodium acetate, sucrose, and water for injection. Manufactured by: Regeneron Pharmaceuticals, Inc., Tarrytown, NY 10591 U.S. License No. 1760 Marketed by: sanofi-aventis U.S. LLC (Bridgewater, NJ 08807) and Regeneron Pharmaceuticals, Inc. (Tarrytown, NY 10591) DUPIXENT® is a registered trademark of Sanofi Biotechnology / © 2022 Regeneron Pharmaceuticals, Inc. / sanofi-aventis U.S. LLC. All rights reserved. For more information about DUPIXENT, go to www.DUPIXENT.com or call 1-844-DUPIXENT (1-844-387-4936). |
||||
| DUPIXENT
dupilumab injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| DUPIXENT
dupilumab injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| DUPIXENT
dupilumab injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| DUPIXENT
dupilumab injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| DUPIXENT
dupilumab injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - sanofi-aventis U.S. LLC (824676584) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Regeneron Pharmaceuticals, Inc. | 945589711 | API MANUFACTURE(0024-5914, 0024-5918, 0024-5915, 0024-5919, 0024-5911) , ANALYSIS(0024-5914, 0024-5918, 0024-5915, 0024-5919, 0024-5911) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Sanofi-Winthrop Industrie | 297730488 | ANALYSIS(0024-5914, 0024-5918, 0024-5915, 0024-5919, 0024-5911) , MANUFACTURE(0024-5914, 0024-5918, 0024-5915, 0024-5919, 0024-5911) , LABEL(0024-5914, 0024-5918, 0024-5915, 0024-5919, 0024-5911) , PACK(0024-5914, 0024-5918, 0024-5915, 0024-5919, 0024-5911) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Sanofi-Aventis Deutschland GmbH | 313218430 | ANALYSIS(0024-5914, 0024-5918, 0024-5915, 0024-5919, 0024-5911) , MANUFACTURE(0024-5915, 0024-5919) , LABEL(0024-5915, 0024-5919) , PACK(0024-5915, 0024-5919) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Regeneron Ireland Designated Activity Company | 986063166 | API MANUFACTURE(0024-5914, 0024-5918, 0024-5915, 0024-5919, 0024-5911) , ANALYSIS(0024-5914, 0024-5918, 0024-5915, 0024-5919, 0024-5911) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Genzyme Ireland Limited | 985127419 | ANALYSIS(0024-5914, 0024-5919, 0024-5918, 0024-5915) , MANUFACTURE(0024-5914, 0024-5919, 0024-5918, 0024-5915) , LABEL(0024-5914) , PACK(0024-5914) | |