Drug Detail:Gazyva (Obinutuzumab [ oh-bi-nue-tooz-ue-mab ])
Drug Class: CD20 monoclonal antibodies
Highlights of Prescribing Information
GAZYVA® (obinutuzumab) injection, for intravenous use
Initial U.S. Approval: 2013
WARNING: HEPATITIS B VIRUS REACTIVATION and PROGRESSIVE MULTIFOCAL LEUKOENCEPHALOPATHY
See full prescribing information for complete boxed warning.
- Hepatitis B Virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure, and death. (5.1)
- Progressive Multifocal Leukoencephalopathy (PML) resulting in death. (5.2)
Recent Major Changes
| Dosage and Administration, Recommended Dosage for Follicular Lymphoma (2.3) | 2/2022 |
| Dosage Modifications for Adverse Reactions (2.5) | 2/2022 |
| Dosage and Administration, Preparation and Administration (2.6) | 2/2022 |
| Warnings and Precautions, Thrombocytopenia (5.8) and Disseminated Intravascular Coagulation (5.9) | 7/2022 |
Indications and Usage for Gazyva
GAZYVA is a CD20-directed cytolytic antibody indicated:
- in combination with chlorambucil, for the treatment of patients with previously untreated chronic lymphocytic leukemia. (1, 14)
- in combination with bendamustine followed by GAZYVA monotherapy, for the treatment of patients with follicular lymphoma who relapsed after, or are refractory to, a rituximab-containing regimen. (1, 14)
- in combination with chemotherapy followed by GAZYVA monotherapy in patients achieving at least a partial remission, for the treatment of adult patients with previously untreated stage II bulky, III or IV follicular lymphoma. (1, 14)
Gazyva Dosage and Administration
- Premedicate for infusion-related reactions and tumor lysis syndrome. (2.1, 5.3, 5.4)
- Administer only as intravenous infusion. Do not administer as an intravenous push or bolus. (2.1)
- The recommended dosage for chronic lymphocytic leukemia is 100 mg on day 1 and 900 mg on day 2 of Cycle 1, 1,000 mg on day 8 and 15 of Cycle 1, and 1,000 mg on day 1 of Cycles 2–6. (2.2)
- The recommended dosage for follicular lymphoma is 1,000 mg on day 1, 8 and 15 of Cycle 1, 1,000 mg on day 1 of Cycles 2-6 or Cycles 2-8, and then 1,000 mg every 2 months for up to 2 years. (2.3)
Dosage Forms and Strengths
Injection: 1,000 mg/40 mL (25 mg/mL) single-dose vial. (3)
Contraindications
GAZYVA is contraindicated in patients with known hypersensitivity reactions (e.g., anaphylaxis) to obinutuzumab or any of the excipients, including serum sickness with prior obinutuzumab use. (4)
Warnings and Precautions
- Infusion-Related Reactions: Premedicate patients with glucocorticoid, acetaminophen, and anti-histamine. Monitor patients closely during infusions. Interrupt, reduce rate, or discontinue for infusion-related reactions based on severity. (2.1, 5.3)
- Hypersensitivity Reactions Including Serum Sickness: Discontinue GAZYVA permanently. (5.4)
- Tumor Lysis Syndrome: Premedicate with anti-hyperuricemics and adequate hydration, especially for patients with high tumor burden, high circulating lymphocyte count or renal impairment. Correct electrolyte abnormalities, provide supportive care, and monitor renal function and fluid balance. (5.5)
- Infections: Do not administer GAZYVA to patients with an active infection. Patients with a history of recurring or chronic infections may be at increased risk of infection. (5.6)
- Neutropenia: In patients with Grade 3 to 4 neutropenia, monitor laboratory tests until resolution and for infection. Consider dose delays and infection prophylaxis, as appropriate. (5.7)
- Thrombocytopenia: Monitor for decreased platelet counts and bleeding. Transfusion may be necessary. (5.8)
- Disseminated Intravascular Coagulation: Evaluate cause and monitor for bleeding, thrombosis, and need for supportive care. (5.9)
- Immunization: Avoid administration of live virus vaccines during GAZYVA treatment and until B-cell recovery. (5.10)
- Embryo-Fetal Toxicity: Can cause fetal harm. Advise females of reproductive potential of the potential risk to a fetus and use effective contraception. (5.11)
Adverse Reactions/Side Effects
The most common adverse reactions (incidence ≥ 20% and ≥ 2% greater in the GAZYVA treated arm) were:
- Previously untreated CLL: infusion-related reactions and neutropenia. (6)
- Relapsed or refractory NHL: infusion-related reactions, fatigue, neutropenia, cough, upper respiratory tract infections, and musculoskeletal pain. (6)
- Previously untreated NHL: infusion-related reactions, neutropenia, upper respiratory tract infections, cough, constipation, and diarrhea. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Genentech at 1-888-835-2555 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Use In Specific Populations
- Lactation: Advise not to breastfeed. (8.1)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 7/2022
Related/similar drugs
Venclexta, rituximab, cyclophosphamide, Revlimid, Rituxan, Imbruvica, lenalidomideFull Prescribing Information
WARNING: HEPATITIS B VIRUS REACTIVATION and PROGRESSIVE MULTIFOCAL LEUKOENCEPHALOPATHY
- Hepatitis B Virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure, and death, can occur in patients receiving CD20-directed cytolytic antibodies, including GAZYVA. Screen all patients for HBV infection before treatment initiation. Monitor HBV-positive patients during and after treatment with GAZYVA. Discontinue GAZYVA and concomitant medications in the event of HBV reactivation [see Warnings and Precautions (5.1)].
- Progressive Multifocal Leukoencephalopathy (PML) including fatal PML, can occur in patients receiving GAZYVA [see Warnings and Precautions (5.2)].
1. Indications and Usage for Gazyva
1.1 Chronic Lymphocytic Leukemia (CLL)
GAZYVA, in combination with chlorambucil, is indicated for the treatment of patients with previously untreated chronic lymphocytic leukemia.
1.2 Follicular Lymphoma (FL)
GAZYVA, in combination with bendamustine followed by GAZYVA monotherapy, is indicated for the treatment of patients with follicular lymphoma who relapsed after, or are refractory to, a rituximab-containing regimen.
GAZYVA, in combination with chemotherapy followed by GAZYVA monotherapy in patients achieving at least a partial remission, is indicated for the treatment of adult patients with previously untreated stage II bulky, III or IV follicular lymphoma.
2. Gazyva Dosage and Administration
2.1 Important Dosing Information
- Premedicate before each infusion [see Dosage and Administration (2.4)].
- Provide prophylactic hydration and anti-hyperuricemics to patients at high risk of tumor lysis syndrome [see Dosage and Administration (2.4) and Warnings and Precautions (5.4)].
- Administer only as an intravenous infusion through a dedicated line [see Dosage and Administration (2.6)].
- Do not administer as an intravenous push or bolus.
- Monitor blood counts at regular intervals.
- GAZYVA should only be administered by a healthcare professional with appropriate medical support to manage severe infusion-related reactions that can be fatal if they occur [see Warnings and Precautions (5.3)].
2.2 Recommended Dosage for Chronic Lymphocytic Leukemia
Each dose of GAZYVA is 1,000 mg administered intravenously with the exception of the first infusions in Cycle 1, which are administered on day 1 (100 mg) and day 2 (900 mg) according to Table 1.
| Day of treatment cycle | Dose of GAZYVA | Rate of infusion | |
|---|---|---|---|
| Cycle 1 (loading doses) | Day 1 | 100 mg | Administer at 25 mg/hr over 4 hours. Do not increase the infusion rate. |
| Day 2 | 900 mg | If no infusion-related reaction (IRR) occurred during the previous infusion, administer at 50 mg/hr. The rate of the infusion can be escalated in increments of 50 mg/hr every 30 minutes to a maximum rate of 400 mg/hr. If an IRR occurred during the previous infusion, administer at 25 mg/hr. The rate of infusion can be escalated in increments of up to 50 mg/hr every 30 minutes to a maximum rate of 400 mg/hr. |
|
| Day 8 | 1,000 mg | If no IRR occurred during the previous infusion and the final infusion rate was 100 mg/hr or faster, infusions can be started at a rate of 100 mg/hr and increased by 100 mg/hr increments every 30 minutes to a maximum of 400 mg/hr. If an infusion-related reaction occurred during the previous infusion, administer at 50 mg/hr. The rate of infusion can be escalated in increments of 50 mg/hr every 30 minutes to a maximum rate of 400 mg/hr. |
|
| Day 15 | 1,000 mg | ||
| Cycles 2–6 | Day 1 | 1,000 mg | |
If a planned dose of GAZYVA is missed, administer the missed dose as soon as possible and adjust dosing schedule to maintain the time interval between doses. If appropriate, patients who do not complete the Day 1 Cycle 1 dose may proceed to the Day 2 Cycle 1 dose.
2.3 Recommended Dosage for Follicular Lymphoma
Each dose of GAZYVA is 1,000 mg administered intravenously according to Table 2.
For patients with relapsed or refractory FL, administer GAZYVA in combination with bendamustine in six 28-day cycles. Patients who achieve stable disease, complete response, or partial response to the initial 6 cycles should continue on GAZYVA 1,000 mg as monotherapy for up to two years.
For patients with previously untreated FL, administer GAZYVA with one of the following chemotherapy regimens:
- Six 28-day cycles in combination with bendamustine
- Six 21-day cycles in combination with CHOP, followed by 2 additional 21-day cycles of GAZYVA alone
- Eight 21-day cycles in combination with CVP
Patients with previously untreated FL who achieve a complete response or partial response to the initial 6 or 8 cycles should continue on GAZYVA 1,000 mg as monotherapy for up to two years.
GAZYVA should be administered at the standard infusion rate in Cycle 1 (see Table 2). In patients with FL who do not experience a Grade 3 or higher IRR during Cycle 1, GAZYVA may be administered as a shorter, approximately 90-minute infusion from Cycle 2 onwards (see Table 3) with continued premedication.
| Day of treatment cycle | Dose of GAZYVA | Rate of infusion | |
|---|---|---|---|
| Cycle 1 (loading doses) | Day 1 | 1,000 mg | Administer at 50 mg/hr. The rate of the infusion can be escalated in 50 mg/hr increments every 30 minutes to a maximum of 400 mg/hr. |
| Day 8 | 1,000 mg | If no infusion-related reaction or an infusion-related reaction of Grade 1 occurred during the previous infusion and the final infusion rate was 100 mg/hr or faster, infusions can be started at a rate of 100 mg/hr and increased by 100 mg/hr increments every 30 minutes to a maximum of 400 mg/hr. If an infusion-related reaction of Grade 2 or higher occurred during the previous infusion, administer at 50 mg/hr. The rate of infusion can be escalated in increments of 50 mg/hr every 30 minutes to a maximum rate of 400 mg/hr. |
|
| Day 15 | 1,000 mg | ||
| Cycles 2–6 or 2–8 | Day 1 | 1,000 mg | |
| Monotherapy | Every two months for up to two years | 1,000 mg | |
| Day of treatment cycle | Dose of GAZYVA | Rate of infusion | |
|---|---|---|---|
|
|||
| Cycle 1 | Days 1, 8, 15 | 1,000 mg | See Table 2 |
| Cycles 2–6* or 2-8* | Day 1 | 1,000 mg | If no Grade 3 or higher IRR occurred during Cycle 1: 100 mg/hr for 30 minutes, then 900 mg/hr for approximately 60 minutes. If an IRR of Grade 1-2 with ongoing symptoms or a Grade 3 or higher IRR occurred during the previous approximately 90-minute infusion, administer all subsequent GAZYVA infusions at the standard infusion rate (see Table 2). |
| Monotherapy* | Every two months for up to two years | 1,000 mg | |
If a planned dose of GAZYVA is missed, administer the missed dose as soon as possible. During GAZYVA and chemotherapy treatment, adjust the dosing schedule accordingly to maintain the time interval between chemotherapy cycles. During monotherapy, maintain the original dosing schedule for subsequent doses. Initiate monotherapy approximately two months after the last dose of GAZYVA administered during the induction phase.
2.4 Recommended Premedication and Prophylactic Medications
Infusion-Related Reactions
Premedication to reduce the risk of IRRs is outlined in Table 4 [see Warnings and Precautions (5.3)].
Hypotension may occur during GAZYVA intravenous infusions. Consider withholding antihypertensive treatments for 12 hours prior to and throughout each GAZYVA infusion and for the first hour after administration [see Warnings and Precautions (5.3)].
| Day of Treatment Cycle | Patients requiring premedication | Premedication | Administration |
|---|---|---|---|
| Premedication applies to both standard and approximately 90-minute infusions. | |||
|
|||
| Cycle 1: CLL Day 1, Day 2 FL Day 1 | All patients | Intravenous glucocorticoid: 20 mg dexamethasone or 80 mg methylprednisolone*,† | Completed at least 1 hour prior to GAZYVA infusion. |
| 650–1,000 mg acetaminophen | At least 30 minutes before GAZYVA infusion. | ||
| anti-histamine (e.g., 50 mg diphenhydramine) | |||
| All subsequent infusions, CLL or FL | All patients | 650–1,000 mg acetaminophen | At least 30 minutes before GAZYVA infusion. |
| Patients with an IRR (Grade 1-2) with the previous infusion | 650–1,000 mg acetaminophen | At least 30 minutes before GAZYVA infusion. | |
| anti-histamine (e.g., 50 mg diphenhydramine) | |||
| Patients with a Grade 3 IRR with the previous infusion OR with a lymphocyte count > 25 × 109/L prior to next treatment | Intravenous glucocorticoid: 20 mg dexamethasone or 80 mg methylprednisolone* | Completed at least 1 hour prior to GAZYVA infusion. | |
| 650–1,000 mg acetaminophen | At least 30 minutes before GAZYVA infusion. | ||
| anti-histamine (e.g., 50 mg diphenhydramine) | |||
3. Dosage Forms and Strengths
Injection: 1,000 mg/40 mL (25 mg/mL) clear, colorless to slightly brown solution in single-dose vial.
4. Contraindications
GAZYVA is contraindicated in patients with known hypersensitivity reactions (e.g., anaphylaxis) to obinutuzumab or to any of the excipients, or serum sickness with prior obinutuzumab use [see Warnings and Precautions (5.4)].
5. Warnings and Precautions
5.1 Hepatitis B Virus Reactivation
Hepatitis B virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure, and death, can occur in patients treated with anti-CD20 antibodies such as GAZYVA. HBV reactivation has been reported in patients who are hepatitis B surface antigen (HBsAg) positive and also in patients who are HBsAg negative but are hepatitis B core antibody (anti-HBc) positive. Reactivation has also occurred in patients who appear to have resolved hepatitis B infection (i.e., HBsAg negative, anti-HBc positive, and hepatitis B surface antibody [anti-HBs] positive).
HBV reactivation is defined as an abrupt increase in HBV replication manifesting as a rapid increase in serum HBV DNA level or detection of HBsAg in a person who was previously HBsAg negative and anti-HBc positive. Reactivation of HBV replication is often followed by hepatitis, i.e., increase in transaminase levels and, in severe cases, increase in bilirubin levels, liver failure, and death.
Screen all patients for HBV infection by measuring HBsAg and anti-HBc before initiating treatment with GAZYVA. For patients who show evidence of hepatitis B infection (HBsAg positive [regardless of antibody status] or HBsAg negative but anti-HBc positive), consult healthcare providers with expertise in managing hepatitis B regarding monitoring and consideration for HBV antiviral therapy.
Monitor patients with evidence of current or prior HBV infection for clinical and laboratory signs of hepatitis or HBV reactivation during and for several months following treatment with GAZYVA. HBV reactivation has been reported for other CD20-directed cytolytic antibodies following completion of therapy.
In patients who develop reactivation of HBV while receiving GAZYVA, immediately discontinue GAZYVA and any concomitant chemotherapy and institute appropriate treatment. Resumption of GAZYVA in patients whose HBV reactivation resolves should be discussed with healthcare providers with expertise in managing hepatitis B. Insufficient data exist regarding the safety of resuming GAZYVA in patients who develop HBV reactivation.
5.2 Progressive Multifocal Leukoencephalopathy
John Cunningham (JC) virus infection resulting in progressive multifocal leukoencephalopathy (PML), which can be fatal, occurred in patients treated with GAZYVA. Consider the diagnosis of PML in any patient presenting with new onset or changes to preexisting neurologic manifestations. Evaluation of PML includes, but is not limited to, consultation with a neurologist, brain MRI, and lumbar puncture. Discontinue GAZYVA therapy and consider discontinuation or reduction of any concomitant chemotherapy or immunosuppressive therapy in patients who develop PML.
5.3 Infusion-Related Reactions
GAZYVA can cause severe and life-threatening infusion-related reactions (IRRs). Sixty-five percent of patients with CLL experienced a reaction to the first 1,000 mg of GAZYVA infused. Thirty-seven percent of patients with relapsed or refractory NHL and 60% of patients with previously untreated NHL experienced a reaction on Day 1 of GAZYVA infusion. IRRs have occurred within 24 hours of receiving GAZYVA. IRRs can also occur with subsequent infusions. Symptoms may include hypotension, tachycardia, dyspnea, and respiratory symptoms (e.g., bronchospasm, larynx and throat irritation, wheezing, laryngeal edema). The most frequently reported symptoms include nausea, fatigue, chest discomfort, dyspnea, dizziness, vomiting, diarrhea, rash, hypertension, hypotension, flushing, headache, pyrexia, and chills [see Adverse Reactions (6.1)].
Premedicate patients with acetaminophen, anti-histamine, and a glucocorticoid [see Dosage and Administration (2.4)]. Closely monitor patients during the entire infusion. Reduce infusion rate, interrupt infusion or permanently discontinue GAZYVA for IRRs based on severity [see Dosage and Administration (2.5)]. Institute medical management (e.g., glucocorticoids, epinephrine, bronchodilators, and/or oxygen) for IRRs as needed.
For patients with preexisting cardiac or pulmonary conditions, monitor more frequently throughout the infusion and the post-infusion period since they may be at greater risk of experiencing more severe reactions. Hypotension may occur as part of the IRR to GAZYVA. Consider withholding antihypertensive treatments for 12 hours prior to, during each GAZYVA infusion, and for the first hour after administration until blood pressure is stable. For patients at increased risk of hypertensive crisis, consider the benefits versus the risks of withholding their antihypertensive medication as is suggested here.
5.4 Hypersensitivity Reactions Including Serum Sickness
Hypersensitivity reactions have been reported in patients treated with GAZYVA. Signs of immediate-onset hypersensitivity included dyspnea, bronchospasm, hypotension, urticaria and tachycardia. Late-onset hypersensitivity diagnosed as serum sickness has also been reported, with symptoms that include chest pain, diffuse arthralgia and fever. Hypersensitivity reactions may be difficult to clinically distinguish from IRRs. However, hypersensitivity very rarely occurs with the first infusion and, when observed, often occurs after previous exposure.
If a hypersensitivity reaction is suspected during or after an infusion, stop the infusion and permanently discontinue treatment. GAZYVA is contraindicated in patients with known hypersensitivity reactions to GAZYVA, including serum sickness with prior GAZYVA use [see Contraindications (4)].
5.5 Tumor Lysis Syndrome
Tumor lysis syndrome (TLS), including fatal cases, has been reported in patients receiving GAZYVA. Patients with high tumor burden, high circulating lymphocyte count (> 25 × 109/L) or renal impairment are at greater risk for TLS.
Administer appropriate tumor lysis prophylaxis with anti-hyperuricemics (e.g., allopurinol or rasburicase) and hydration prior to the infusion of GAZYVA for patients at risk for TLS [see Dosage and Administration (2.4)]. During the initial days of GAZYVA treatment, monitor the laboratory parameters of patients considered at risk for TLS. For treatment of TLS, correct electrolyte abnormalities, monitor renal function and fluid balance, and administer supportive care, including dialysis as indicated.
5.6 Infections
Fatal and serious bacterial, fungal, and new or reactivated viral infections can occur during and following GAZYVA therapy. When GAZYVA is administered with chemotherapy followed by GAZYVA monotherapy as in the GALLIUM study, Grade 3 to 5 infections have been reported in up to 8% of patients during combination therapy, up to 13% of patients during monotherapy, and up to 8% of patients after treatment [see Adverse Reactions (6.1)].
In GALLIUM, more Grade 3 to 5 infections were reported in the recipients of GAZYVA and bendamustine (117/410 patients, 29%) as compared to GAZYVA plus CHOP or CVP (43/281 patients, 15%). More fatal infections were reported in patients treated with GAZYVA and bendamustine (3%), as compared to GAZYVA plus CHOP or CVP (< 1%), including during the monotherapy phase and after completion of treatment.
Do not administer GAZYVA to patients with an active infection. Patients with a history of recurring or chronic infections may be at increased risk of infection.
5.7 Neutropenia
Severe and life-threatening neutropenia, including febrile neutropenia, has been reported during treatment with GAZYVA. Monitor patients with Grade 3 to 4 neutropenia frequently with regular laboratory tests until resolution. Anticipate, evaluate, and treat any symptoms or signs of developing infection. Consider dose delays for Grade 3 or 4 neutropenia. Consider administration of granulocyte colony-stimulating factors (GCSF) in patients with Grade 3 or 4 neutropenia.
Neutropenia can also be of late onset (occurring more than 28 days after completion of treatment) and/or prolonged (lasting longer than 28 days). Patients with severe and long lasting (> 1 week) neutropenia are strongly recommended to receive antimicrobial prophylaxis until resolution of neutropenia to Grade 1 or 2. Consider antiviral and antifungal prophylaxis.
5.8 Thrombocytopenia
Severe and life-threatening thrombocytopenia has been reported during treatment with GAZYVA in combination with chemotherapy. Fatal hemorrhagic events have been reported in patients with NHL and CLL treated with GAZYVA in combination with chemotherapy, including during Cycle 1.
Monitor all patients frequently for thrombocytopenia and hemorrhagic events, especially during the first cycle and if clinically indicated, evaluate laboratory coagulation parameters [see Warnings and Precautions (5.9)]. In patients with Grade 3 or 4 thrombocytopenia, monitor platelet counts more frequently until resolution and consider dose delays of GAZYVA and chemotherapy or dose reductions of chemotherapy. Transfusion of blood products (i.e., platelet transfusion) may be necessary. Consider withholding concomitant medications that may increase bleeding risk (platelet inhibitors, anticoagulants), especially during the first cycle.
5.9 Disseminated Intravascular Coagulation (DIC)
Fatal and severe DIC has been reported in patients receiving GAZYVA for treatment of follicular lymphoma and chronic lymphocytic leukemia. The majority of DIC cases have involved changes in platelets and laboratory coagulation parameters following the first infusion, with spontaneous resolution usually occurring by Day 8. In some cases, DIC was associated with IRRs, TLS, or both [see Adverse Reactions (6.1)]. In patients with suspected DIC, evaluate potential causes, and monitor coagulation parameters, platelet counts, and for signs and symptoms of bleeding or thrombosis. Manage according to standard guidelines for DIC. Supportive care, including transfusion of blood products and other medical management, may be necessary.
5.10 Immunization
The safety and efficacy of immunization with live or attenuated viral vaccines during or following GAZYVA therapy have not been studied. Immunization with live virus vaccines is not recommended during treatment and until B-cell recovery.
5.11 Embryo-Fetal Toxicity
Based on its mechanism of action and findings in animals, GAZYVA can cause B-cell depletion in infants exposed to obinutuzumab in-utero. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception while receiving GAZYVA and for 6 months after the last dose [see Use in Specific Populations (8.1, 8.3)].
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Hepatitis B virus reactivation [see Warnings and Precautions (5.1)]
- Progressive multifocal leukoencephalopathy [see Warnings and Precautions (5.2)]
- Infusion-related reactions [see Warnings and Precautions (5.3)]
- Hypersensitivity reactions including serum sickness [see Warnings and Precautions (5.4)]
- Tumor lysis syndrome [see Warnings and Precautions (5.5)]
- Infections [see Warnings and Precautions (5.6)]
- Neutropenia [see Warnings and Precautions (5.7)]
- Thrombocytopenia [see Warnings and Precautions (5.8)]
- Disseminated intravascular coagulation [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Chronic Lymphocytic Leukemia
The data below are based on a safety population of 773 previously untreated patients with CLL in the CLL11 study. Patients were treated with chlorambucil alone, GAZYVA in combination with chlorambucil, or rituximab product in combination with chlorambucil. The Stage 1 analysis compared GAZYVA in combination with chlorambucil vs. chlorambucil alone and Stage 2 compared GAZYVA in combination with chlorambucil vs. rituximab product in combination with chlorambucil. Adverse reactions rates and laboratory abnormalities from the Stage 2 phase are presented below and are consistent with the rates in Stage 1. In addition to the adverse reactions observed in Stage 2, in Stage 1, back pain (5% vs. 2%), anemia (12% vs. 10%) and cough (10% vs. 7%) were observed at a higher incidence in the GAZYVA treated patients. The incidence of Grade 3 to 4 back pain (< 1% vs. 0%), cough (0% vs. < 1%) and anemia (5% vs. 4%) was similar in both treatment arms. With regard to laboratory abnormalities, in Stage 1 hyperkalemia (33% vs. 18%), creatinine increased (30% vs. 20%) and alkaline phosphatase increased (18% vs. 11%) were observed at a higher incidence in patients treated with GAZYVA with similar incidences of Grade 3 to 4 abnormalities between the two arms.
Patients received three 1,000 mg doses of GAZYVA on the first cycle and a single dose of 1,000 mg once every 28 days for 5 additional cycles in combination with chlorambucil (6 cycles of 28 days each in total). In the last 140 patients enrolled, the first dose of GAZYVA was split between day 1 (100 mg) and day 2 (900 mg) [see Dosage and Administration (2.2)]. In total, 81% of patients received all 6 cycles (of 28 days each) of GAZYVA-based therapy.
Adverse reactions in ≥ 10% of patients in the GAZYVA containing arm were infusion-related reactions, neutropenia, thrombocytopenia, and diarrhea. The most common Grade 3 to 4 adverse reactions (incidence ≥ 10%) in the GAZYVA containing arm were neutropenia, infusion-related reactions, and thrombocytopenia.
| Body System Adverse Reactions | GAZYVA + Chlorambucil n = 336 | Rituximab product + Chlorambucil n = 321 |
||
|---|---|---|---|---|
| All Grades % | Grades 3 to 4 % | All Grades % | Grades 3 to 4 % |
|
|
||||
| Injury, Poisoning and Procedural Complications | ||||
| Infusion-Related Reaction | 66 | 20 | 38 | 4 |
| Blood and Lymphatic System Disorders* | ||||
| Neutropenia | 38 | 33 | 32 | 28 |
| Thrombocytopenia | 14 | 10 | 7 | 3 |
| Gastrointestinal Disorders | ||||
| Diarrhea | 10 | 2 | 8 | < 1 |
| Constipation | 8 | 0 | 5 | 0 |
| General Disorders and Administration Site Conditions | ||||
| Pyrexia | 9 | < 1 | 7 | < 1 |
| Infections and Infestations | ||||
| Nasopharyngitis | 6 | < 1 | 3 | 0 |
| Urinary Tract Infection | 5 | 1 | 2 | < 1 |
| Laboratory Abnormalities | GAZYVA + Chlorambucil n = 336 | Rituximab product + Chlorambucil n = 321 |
||
|---|---|---|---|---|
| All Grades % | Grades 3 to 4 % | All Grades % | Grades 3 to 4 % | |
| Hematology | ||||
| Leukopenia | 84 | 35 | 62 | 16 |
| Lymphopenia | 80 | 39 | 50 | 16 |
| Neutropenia | 76 | 46 | 69 | 41 |
| Thrombocytopenia | 48 | 13 | 40 | 8 |
| Anemia | 39 | 10 | 37 | 10 |
| Chemistry | ||||
| Hypocalcemia | 37 | 3 | 32 | < 1 |
| ALT increased | 28 | 2 | 21 | 1 |
| AST increased | 27 | 2 | 21 | < 1 |
| Hyponatremia | 26 | 7 | 18 | 2 |
| Hypoalbuminemia | 23 | < 1 | 16 | < 1 |
| Hypokalemia | 14 | 1 | 10 | < 1 |
Non-Hodgkin Lymphoma
GADOLIN
The GADOLIN study evaluated safety in 407 patients with relapsed or refractory NHL, including FL (81%), small lymphocytic lymphoma and marginal zone lymphoma (a disease for which GAZYVA is not indicated), who did not respond to or progressed within 6 months of treatment with rituximab product or a rituximab product-containing regimen. In the population of patients with FL, the profile of adverse reactions was consistent with the overall NHL population. Patients received either GAZYVA in combination with bendamustine (204 patients), followed by GAZYVA monotherapy in patients that had not progressed, or bendamustine alone (203 patients).
Patients randomized to the GAZYVA + bendamustine arm received three weekly 1,000 mg doses of GAZYVA in the first cycle and a single dose of 1,000 mg once every 28 days for 5 additional cycles, in combination with bendamustine 90 mg/m2 intravenously on Days 1 and 2 in all 6 cycles. Patients who did not progress on the combination received a single 1,000 mg dose of GAZYVA monotherapy every two months until progression or for a maximum of two years. The control arm received bendamustine 120 mg/m2 on Days 1 and 2 of each cycle for 6 cycles, with a cycle length of 28 days. In the GAZYVA arm, 78% of patients received 6 cycles of bendamustine and 82% received their full 6 cycles of GAZYVA; 72 (46%) of the 158 patients who began GAZYVA monotherapy received all planned doses. In the control arm, 72% of patients received 6 cycles of bendamustine.
Serious adverse reactions occurred in 45% of the GAZYVA arm and 37% of the bendamustine-only arm. Fatal adverse reactions within 90 days of treatment occurred in 3.4% and 2.5%, respectively. During treatment and follow-up combined, fatal adverse reactions occurred in 10% of GAZYVA recipients and in 7.4% of recipients of bendamustine alone, with infection and second primary malignancies being the leading causes.
Dose modification due to adverse reactions occurred in 50% of the GAZYVA arm and 42% of the control arm, and discontinuation of any study drug due to adverse reactions occurred in 20% and 17%, respectively.
Table 7 presents selected adverse reactions in GADOLIN. The most common adverse reactions (incidence ≥ 20%) in GAZYVA recipients included infusion-related reactions, fatigue, neutropenia, cough, upper respiratory tract infections, and musculoskeletal pain.
| Body System Adverse Reactions*, † | GAZYVA + Bendamustine followed by GAZYVA monotherapy n = 204 | Bendamustine n = 203 |
||
|---|---|---|---|---|
| All Grades % | Grades 3 to 5 % | All Grades % | Grades 3 to 5 % |
|
|
||||
| Procedural Complications | ||||
| Infusion-Related Reaction‡ | 67 | 11 | 63 | 5 |
| General Disorders | ||||
| Fatigue | 40 | 3 | 36 | 3 |
| Pyrexia | 19 | 1 | 15 | 1 |
| Blood and Lymphatic System Disorders | ||||
| Neutropenia | 37 | 35§ | 29 | 27 |
| Infections and Infestations | ||||
| Upper Respiratory Tract Infection | 36 | 3 | 23 | 1 |
| Respiratory Tract Infection, Unspecified | 14 | 1 | 8 | 0 |
| Urinary Tract Infection | 13 | 3 | 7 | 0 |
| Respiratory, Thoracic and Mediastinal Disorders | ||||
| Cough | 31 | <1 | 21 | 0 |
| Musculoskeletal and Connective Tissue Disorders | ||||
| Musculoskeletal Pain | 28 | 1 | 20 | 0 |
| Arthralgia | 12 | <1 | 5 | 0 |
| Skin and Subcutaneous Tissue Disorders | ||||
| Rash | 17 | <1 | 14 | <1 |
| Pruritus | 11 | 0 | 6 | 0 |
Infusion-related reactions are defined as any related adverse reaction that occurred during or within 24 hours of infusion.
Fatigue includes fatigue, lethargy, asthenia.
Pyrexia includes pyrexia, hyperthermia, body temperature increased.
Cough includes cough, productive cough, upper-airway cough syndrome.
Neutropenia includes neutropenia, agranulocytosis, granulocytopenia, neutrophil count decreased.
Upper respiratory tract infection includes upper respiratory tract congestion, upper respiratory tract inflammation, upper respiratory fungal infection, rhinovirus infection, and all terms containing: upper respiratory tract infection, laryngitis, nasopharyngitis, pharyngitis, rhinitis, tonsillitis, and sinusitis with the exception of sinobronchitis.
Respiratory tract infection unspecified includes respiratory tract infection, respiratory tract infection viral, influenza, influenza-like illness, sinobronchitis, respiratory syncytial virus infection.
Urinary tract infection includes all terms containing: urinary tract infection, cystitis, pyelonephritis.
Musculoskeletal pain includes non-cardiac chest pain, bone pain, spinal pain, myalgia, back pain, neck pain, musculoskeletal discomfort, pain in extremity, and all terms containing "musculoskeletal pain".
Rash includes drug eruption, skin reaction, all terms containing "rash", urticaria, and selected terms containing "dermatitis".
Pruritus includes pruritus, pruritus generalized.
Other clinically relevant adverse reactions (incidence < 10% and ≥ 2% greater in the GAZYVA arm) included:
- Blood and lymphatic system disorders: febrile neutropenia (6%)
- Infection: sepsis (7%)
During GAZYVA monotherapy (158 patients), adverse reactions in ≥ 10% of patients included upper and lower respiratory tract infections, cough, neutropenia, musculoskeletal pain, fatigue, diarrhea, rash, and urinary tract infection.
Table 8 presents selected new or worsening laboratory abnormalities in the GADOLIN trial.
| Laboratory Abnormalities | GAZYVA + Bendamustine followed by GAZYVA monotherapy n = 204 | Bendamustine n = 203 |
||
|---|---|---|---|---|
| All Grades % | Grades 3 to 4 % | All Grades % | Grades 3 to 4 % | |
|
||||
| Hematology | ||||
| Lymphopenia | 97 | 92 | 96 | 84 |
| Leukopenia | 84 | 47 | 87 | 34 |
| Neutropenia | 76 | 53 | 75 | 42 |
| Chemistry | ||||
| Hypophosphatemia | 41 | 8 | 38 | 7 |
| Hypocalcemia | 39 | 3 | 24 | 1 |
| ALT/SGPT increased | 36 | 2 | 31 | 3 |
| Alkaline phosphatase increased | 27 | 0 | 23 | 0 |
| Hyperbilirubinemia | 21 | 2 | 17 | 2 |
| Hyperkalemia | 20 | 3 | 18 | 0 |
In the GAZYVA monotherapy phase, new or worsening grade 3 or 4 abnormalities included neutropenia in 25% of patients (Grade 4, 10%) and lymphopenia in 23% (Grade 4, 5%).
GALLIUM
A randomized, open-label multicenter trial (GALLIUM) evaluated the safety of GAZYVA as compared to rituximab product in 1385 patients with previously untreated follicular lymphoma (86%) or marginal zone lymphoma (14%). Patients received chemotherapy (bendamustine, CHOP, or CVP) combined with either GAZYVA (691 patients) or rituximab product (694 patients), followed in responding patients by GAZYVA or rituximab product monotherapy every two months until disease progression or for a maximum of two years. The study excluded patients having an absolute neutrophil count (ANC) < 1500 / µL, platelets < 75,000 / µL, CLcr < 40 mL/min and, unless attributable to lymphoma, hepatic transaminases > 2.5 × upper limit of normal.
The median age was 60 (range: 23-88), 47% were male, 82% were white, and 97% had an ECOG performance status of 0 or 1. The chemotherapy was bendamustine in 59%, CHOP in 31% and CVP in 10% of patients. Following combination therapy, 624 patients (90%) in the GAZYVA arm and 612 patients (88%) in the rituximab product arm received monotherapy.
Serious adverse reactions occurred in 50% of patients on the GAZYVA arm and 43% of patients on the rituximab product arm. Fatal adverse reactions were reported during treatment in 3% in the GAZYVA arm and 2% in the rituximab product arm, most often from infections in the GAZYVA arm. During treatment and follow-up combined, fatal adverse reactions were reported in 5% of the GAZYVA arm and 4% of the rituximab product arm, with infections and second malignancies being leading causes. In the GAZYVA arm, fatal infections occurred in 2% of patients compared to < 1% in the rituximab product arm.
During combination therapy, 93% of patients received all treatment cycles in the GAZYVA arm, and 92% received all treatment cycles in the rituximab product arm. Of the responding patients who began monotherapy with GAZYVA or rituximab product, 76% and 73%, respectively, completed the full course. Dose modification due to adverse reactions occurred in 74% of the GAZYVA arm and 63% of the rituximab product arm throughout study treatment, and discontinuation of any study drug due to adverse reactions occurred in 18% and 15%, respectively.
Throughout treatment and follow-up, the most common adverse reactions (incidence ≥ 20%) observed at least 2% more in the GAZYVA arm included infusion-related reactions, neutropenia, upper respiratory tract infections, constipation and diarrhea (Table 9). Neutropenia, infusion-related reactions, febrile neutropenia and thrombocytopenia were the most common Grade 3 to 5 adverse reactions (incidence ≥ 5%) observed more frequently in the GAZYVA arm.
| Body System Adverse Reactions *, † | GAZYVA + chemotherapy followed by GAZYVA monotherapy n = 691 | Rituximab product + chemotherapy followed by rituximab product monotherapy n = 694 |
||
|---|---|---|---|---|
| All Grades % | Grades 3 to 5 % | All Grades % | Grades 3 to 5 % |
|
|
||||
| Injury, Poisoning and Procedural Complications | ||||
| Infusion-Related Reaction ‡ | 72 | 12 | 60 | 8 |
| Blood and Lymphatic System Disorders | ||||
| Neutropenia § | 53 | 49 | 47 | 41 |
| Thrombocytopenia § | 14 | 7 | 8 | 3 |
| Infections and Infestations | ||||
| Upper Respiratory Tract Infection | 50 | 3 | 43 | 1 |
| Herpesvirus Infection | 18 | 3 | 14 | 1 |
| Pneumonia | 14 | 7 | 12 | 6 |
| Respiratory, Thoracic and Mediastinal Disorders | ||||
| Cough | 35 | < 1 | 28 | < 1 |
| Gastrointestinal Disorders | ||||
| Constipation | 32 | < 1 | 29 | < 1 |
| Diarrhea | 30 | 3 | 26 | 2 |
| Nervous System Disorders | ||||
| Headache | 18 | < 1 | 15 | < 1 |
| Musculoskeletal and Connective Tissue Disorders | ||||
| Arthralgia | 16 | 0 | 14 | < 1 |
| Psychiatric Disorders | ||||
| Insomnia | 15 | < 1 | 12 | < 1 |
| Metabolism and Nutrition Disorders | ||||
| Decreased Appetite | 14 | < 1 | 12 | < 1 |
| Skin and Subcutaneous Tissue Disorders | ||||
| Pruritus | 11 | < 1 | 9 | 0 |
Infusion-related reactions are defined as any related adverse reaction that occurred during or within 24 hours of infusion.
Neutropenia includes neutropenia, agranulocytosis, granulocytopenia, and neutrophil count decreased.
Febrile neutropenia includes febrile neutropenia, neutropenic infection, neutropenic sepsis, and febrile bone marrow aplasia.
Thrombocytopenia includes thrombocytopenia and platelet count decreased.
Upper respiratory tract infection includes upper respiratory tract congestion, upper respiratory tract inflammation, upper respiratory tract infection, rhinovirus infection, and all terms containing: laryngitis, nasopharyngitis, pharyngitis, rhinitis, tonsillitis, and sinusitis with the exception of sinobronchitis.
Herpesvirus infection includes all terms containing "herpes" or "varicella."
Pneumonia includes all terms containing "pneumonia," bacterial, pneumonia haemophilus, pneumonia pneumococcal, pneumonia fungal, pneumocystis jirovecii infection, lung infection, and lung infiltration.
Diarrhea includes diarrhea, defecation urgency, frequent bowel movement, and all terms containing "gastroenteritis".
Headache includes all terms containing "headache" and migraine.
Insomnia includes all terms containing "insomnia" and sleep disorder.
Pruritus includes pruritus and pruritus generalized.
During the monotherapy period, the common adverse reactions (incidence ≥ 10%) observed at least 2% more with GAZYVA were upper respiratory tract infection (40%), cough (23%), musculoskeletal pain (20%), neutropenia (19%), and herpesvirus infection (13%).
Table 10 summarizes treatment-emergent laboratory abnormalities during treatment and follow-up. The Grade 3 to 4 abnormalities reported at least 2% more in the GAZYVA arm were lymphopenia, leukopenia, neutropenia, thrombocytopenia, and hyperuricemia. Patients in the GAZYVA arm, as compared to the rituximab product arm, had higher incidences of Grade 4 neutropenia (38% vs. 30%, respectively), Grade 4 lymphopenia (33% vs. 22%), and Grade 4 leukopenia (17% vs. 12%).
| Laboratory Abnormalities * | GAZYVA+ chemotherapy followed by GAZYVA monotherapy n = 691 | Rituximab product + chemotherapy followed by rituximab product monotherapy n = 694 |
||
|---|---|---|---|---|
| All Grades % | Grades 3 to 4 % | All Grades % | Grades 3 to 4 % | |
|
||||
| Hematology | ||||
| Lymphopenia | 97 | 83 | 95 | 67 |
| Leukopenia | 92 | 49 | 89 | 39 |
| Neutropenia | 84 | 59 | 76 | 50 |
| Thrombocytopenia | 68 | 11 | 50 | 4 |
| Chemistry | ||||
| ALT increased | 50 | 3 | 43 | 2 |
| AST increased | 44 | 1 | 41 | 1 |
| Hypophosphatemia | 36 | 5 | 33 | 5 |
| Hypoalbuminemia | 33 | 1 | 25 | 1 |
| Hypoproteinemia | 32 | 0 | 30 | 0 |
| Hypocalcemia | 32 | 1 | 26 | 1 |
| Hyperuricemia | 28 | 28 | 22 | 22 |
| Hyponatremia | 26 | 4 | 20 | 3 |
| Hyperkalemia | 23 | 1 | 17 | 1 |
| Hypernatremia | 16 | < 1 | 13 | 0 |
In the monotherapy phase, new-onset Grade 3 or 4 neutropenia was reported in 21% of patients in the GAZYVA arm (Grade 4, 10%) and 17% of patients in the rituximab product arm (Grade 4, 9%).
6.2 Immunogenicity
As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other products may be misleading.
Seven percent (18/271) of patients with CLL tested positive for anti-GAZYVA antibodies at one or more time points in CLL11. No patients developed anti-GAZYVA antibodies during or following GAZYVA treatment in GADOLIN, while 1 patient (1/564, 0.2%) developed anti-GAZYVA antibodies in GALLIUM. Neutralizing activity of anti-GAZYVA antibodies has not been assessed.
6.3 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of GAZYVA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
- Immune/Autoimmune Events: Serum sickness
8. Use In Specific Populations
8.4 Pediatric Use
The safety and effectiveness of GAZYVA in pediatric patients have not been established.
10. Overdosage
There has been no experience with overdose in human clinical trials. For patients who experience overdose, treatment should consist of immediate interruption or reduction of GAZYVA and supportive therapy.
11. Gazyva Description
Obinutuzumab is a humanized anti-CD20 monoclonal antibody of the IgG1 subclass. It recognizes a specific epitope of the CD20 molecule found on B cells. The molecular mass of the antibody is approximately 150 kDa.
GAZYVA (obinutuzumab) injection is produced by mammalian cell (CHO) suspension culture. GAZYVA was engineered for reduced fucose content as compared to a typical IgG1 produced in CHO cells. GAZYVA is a sterile, clear, colorless to slightly brown, preservative-free liquid concentrate for intravenous use. GAZYVA is supplied at a concentration of 25 mg/mL in 1,000 mg single-dose vials. The product is formulated in 20 mM L-histidine/L-histidine hydrochloride, 240 mM trehalose, 0.02% poloxamer 188. The pH is 6.0.
12. Gazyva - Clinical Pharmacology
12.1 Mechanism of Action
Obinutuzumab is a monoclonal antibody that targets the CD20 antigen expressed on the surface of pre-B and mature B lymphocytes. Upon binding to CD20, obinutuzumab mediates B-cell lysis through (1) engagement of immune effector cells, (2) by directly activating intracellular death signaling pathways (direct cell death), and/or (3) activation of the complement cascade. The immune effector cell mechanisms include antibody-dependent cellular cytotoxicity (ADCC) and antibody-dependent cellular phagocytosis.
As an antibody with reduced fucose content, obinutuzumab induces greater ADCC activity than rituximab in vitro using human cancer cell lines. Obinutuzumab also demonstrated an increased ability to induce direct cell death when compared to rituximab. Obinutuzumab binds to FcγRIII using purified proteins with a higher affinity than rituximab. Obinutuzumab and rituximab bind with similar affinity to overlapping epitopes on CD20.
12.2 Pharmacodynamics
In patients with CLL, GAZYVA caused CD19 B-cell depletion (defined as CD19 B cell counts < 0.07 × 109/L). Initial CD19 B cell recovery was observed in some patients approximately 9 months after the last GAZYVA dose. At 18 months of follow-up, some patients remain B cell depleted.
Although the depletion of B cells in the peripheral blood is a measurable pharmacodynamic effect, it is not directly correlated with the depletion of B-cells in solid organs or in malignant deposits. B cell depletion has not been shown to be directly correlated to clinical response.
12.3 Pharmacokinetics
The pharmacokinetic parameters of obinutuzumab after 100 mg on day 1 and 900 mg on day 2 of Cycle 1, 1,000 mg on day 8 and 15 of Cycle 1, and 1,000 mg on day 1 of Cycles 2–6 for CLL and after 1,000 mg on day 1, 8 and 15 of Cycle 1, 1,000 mg on day 1 of Cycles 2-6 or Cycles 2-8, and then 1,000 mg every 2 months for up to 2 years for NHL are provided in Table 11. The dosing regimen is within the linear pharmacokinetic behavior of obinutuzumab.
| PK Measure | CLL* | Relapsed or refractory FL* | First line FL in combination with chemotherapy | |
|---|---|---|---|---|
| GAZYVA + Bendamustine* | GAZYVA + CHOP or CVP† | |||
| Results are presented as geometric mean (% Coefficient of Variation). | ||||
|
||||
| Cmax, µg/mL | 466.3 (35) | 553.5 (32) | 513.4 (28) | 676.4 (30) |
| Ctrough, µg/mL | 192.5 (78) | 295 (56) | 255 (46) | 395 (44) |
| AUC, µg/mL*day | 8701 (51) | 11362 (41) | 10088 (35) | 10723 (37) |
Distribution and Elimination
The elimination of obinutuzumab is comprised of a linear clearance pathway and a time-dependent non-linear clearance pathway. As GAZYVA treatment progresses, the impact of the time-dependent pathway diminishes in a manner suggesting target-mediated drug disposition (TMDD) and saturation of the TMDD at the end of the treatment cycle at the proposed clinical dose regimen. The pharmacokinetic properties of obinutuzumab in patients with CLL and NHL are provided in Table 12.
| CLL | NHL | |
|---|---|---|
| Parameters are presented as geometric mean (% Coefficient of Variation). | ||
|
||
| Distribution | ||
| Volume of Distribution*, L | 4.1 (20) | 4.3 (21) |
| Elimination | ||
| Terminal Half-life, days | 25.5 (48) | 35.3 (35) |
| Clearance, L/day | 0.11 (53) | 0.08 (41) |
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No carcinogenicity or genotoxicity studies have been conducted with obinutuzumab.
No specific studies have been conducted to evaluate potential effects on fertility; however, no adverse effects on male or female reproductive organs were observed in the 26-week repeat-dose toxicity study in cynomolgus monkeys.
14. Clinical Studies
14.1 Chronic Lymphocytic Leukemia
The efficacy of GAZYVA was evaluated in a three-arm, open-label, active-controlled, randomized, multicenter trial (CLL11; NCT01010061) in 781 patients with previously untreated CD20+ CLL requiring treatment who had coexisting medical conditions or reduced renal function as measured by creatinine clearance (CLcr) < 70 mL/min. Patients with CLcr < 30 mL/min, active infections, positive hepatitis B (HBsAg or anti-HBc positive; patients positive for anti-HBc could be included if hepatitis B viral DNA was not detectable) and hepatitis C serology, or immunization with live virus vaccine within 28 days prior to randomization were excluded from the trial. Patients were treated with chlorambucil control (Arm 1), GAZYVA in combination with chlorambucil (Arm 2), or rituximab product in combination with chlorambucil (Arm 3). The safety and efficacy of GAZYVA was evaluated in a Stage 1 comparison of Arm 1 vs. Arm 2 in 356 patients and a Stage 2 comparison of Arm 2 vs. Arm 3 in 663 patients.
The majority of patients received 1,000 mg of GAZYVA on days 1, 8 and 15 of the first cycle, followed by treatment on the first day of 5 subsequent cycles (total of 6 cycles, 28 days each). The first dose of GAZYVA was divided between day 1 (100 mg) and day 2 (900 mg) [see Dosage and Administration (2.2)], which was implemented in 140 patients. Chlorambucil was given orally at 0.5 mg/kg on day 1 and day 15 of all treatment cycles (1 to 6).
In CLL11, the median age was 73 years, 62% were male, and 95% were White. Sixty-five percent had a CLcr < 70 mL/min and 76% had multiple coexisting medical conditions. Twenty-two percent of patients were Binet stage A, 42% were stage B, and 36% were stage C. The median estimated CLcr was 62 mL/min. Eighty-one percent of patients treated with GAZYVA in combination with chlorambucil received all 6 cycles compared to 89% of patients in the rituximab product treated arm and 67% in the chlorambucil alone arm.
In the Stage 1 analysis of CLL11, the median progression-free survival (PFS) in the GAZYVA in combination with chlorambucil arm was 27.2 months and 11.2 months in the chlorambucil alone arm (median observation time 22.8 months) as assessed by independent review and is consistent with investigator-assessed PFS. The median overall survival (OS) was not yet reached with a total of 46 deaths: 22 (9%) in the GAZYVA in combination with chlorambucil arm and 24 (20%) in the chlorambucil arm. The hazard ratio for OS was 0.41 (95% CI: 0.23-0.74).
In the Stage 2 analysis of CLL11, the median PFS was 26.7 months in the GAZYVA arm and 14.9 months in the rituximab product arm with a median observation time of 18.7 months (HR: 0.42, 95% CI: 0.33-0.54, p-value < 0.0001). These results were assessed by independent review and are consistent with investigator-assessed PFS. Minimal residual disease (MRD) was evaluated using allele-specific oligonucleotide polymerase chain reaction (ASO-PCR). The cutoff for a negative status was one CLL cell per 104 leukocytes in the sample (i.e., an MRD value of < 10-4 was considered negative). Among patients who achieved complete response (CR) and complete response with incomplete marrow recovery (CRi; 94 patients in the GAZYVA arm and 34 patients in the rituximab product arm), 18 patients (19%) had negative MRD in the bone marrow in the GAZYVA arm compared to 2 patients (6%) in the rituximab product arm. Out of the patients who achieved CR and CRi, 39 patients (41%) in the GAZYVA arm, and 4 patients (12%) in the rituximab product arm were MRD negative in peripheral blood samples collected at least 3 months after the end of treatment.
Efficacy results are shown in Table 13 and Figures 1 and 2.
| Endpoint | Stage 1 of CLL11 | Stage 2 of CLL11 | ||
|---|---|---|---|---|
| GAZYVA + Chlorambucil* | Chlorambucil | GAZYVA + Chlorambucil* | Rituximab product + Chlorambucil | |
| n = 238 | n = 118 | n = 333 | n = 330 | |
|
||||
| Median Progression-Free Survival† | 27.2 months | 11.2 months | 26.7 months | 14.9 months |
| (HR 0.19 [0.14; 0.27], p-value < 0.0001 stratified log-rank test) | (HR 0.42 [0.33; 0.54], p-value < 0.0001 stratified log-rank test) | |||
| Overall Response Rate‡ | 78.2% | 33.1% | 79.6% | 66.3% |
| Complete Response | 28.2% | 0 | 26.1% | 8.8% |
| Complete Response with Incomplete Marrow Recovery | 2.5% | 1.7% | 2.1% | 1.5% |
| Partial Response | 45.0% | 30.5% | 48.6% | 54.1% |
| Nodular Partial Response | 2.5% | 0.8% | 2.7% | 1.8% |
| Median Duration of Response | 22.4 months | 4.7 months | 19.6 months | 9.7 months |
| Overall Survival | HR 0.41 [0.23; 0.74] | Not Yet Mature | ||
| Figure 1 Kaplan-Meier Curve of Overall Survival in Patients with CLL in CLL11 (Stage 1) |
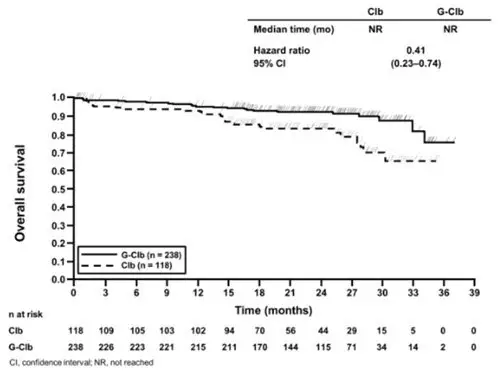 |
| Figure 2 Kaplan-Meier Curve of Progression-Free Survival in Patients with CLL in CLL11 (Stage 2) |
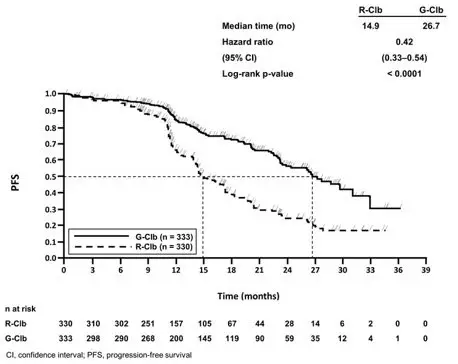 |
14.2 Follicular Lymphoma
GADOLIN
The efficacy of GAZYVA was evaluated in GADOLIN (NCT01059630), an open-label, multicenter, randomized study that included 335 patients with follicular lymphoma (FL) who had no response to or have progressed during or within 6 months of rituximab product or a rituximab product-containing regimen. These patients were randomized to receive either bendamustine alone (n = 171) or GAZYVA in combination with bendamustine (n = 164) for 6 cycles, each of 28 days duration. Patients in the GAZYVA plus bendamustine arm who did not have disease progression [patients with a complete response (CR), partial response (PR) or stable disease (SD)] at the end of the 6 cycles continued receiving GAZYVA monotherapy for 2 years. Patients were stratified according to the type of refractoriness to rituximab product (refractory to rituximab product monotherapy versus rituximab product in combination with chemotherapy), the number of prior therapies (≤ 2 versus > 2), and geographic region.
GAZYVA was given by intravenous infusion as a flat dose of 1,000 mg on Days 1, 8 and 15 of Cycle 1, on Day 1 of Cycles 2–6, and then every 2 months until disease progression for up to 2 years. Bendamustine was given intravenously on Days 1 and 2 for all treatment cycles (1–6) at 90 mg/m2/day when given in combination with GAZYVA or 120 mg/m2/day when given alone.
The primary analysis included 321 FL patients, including 166 patients randomized to bendamustine alone and 155 patients randomized to GAZYVA in combination with bendamustine. In the primary analysis, patients had a median age of 63 years, 88% were White and 56% were male. Thirty-four percent had bulky disease (> 6 cm), 15% had at least one B-symptom at baseline and 95% had an ECOG performance status of 0–1 at baseline. The median time since initial diagnosis was 3 years and the median number of prior therapies was 2 (range 1 to 10). Forty-six percent of patients received 1 prior therapy and 33% of patients received 2 prior therapies. Twenty percent of patients were refractory to prior rituximab product monotherapy, 37% of patients were refractory to prior rituximab product plus chemotherapy induction treatment, and 41% of patients were refractory to rituximab product maintenance treatment received following rituximab product plus chemotherapy induction. Seventy-nine percent of patients were refractory to both rituximab product and an alkylating agent during any prior regimen (double refractory).
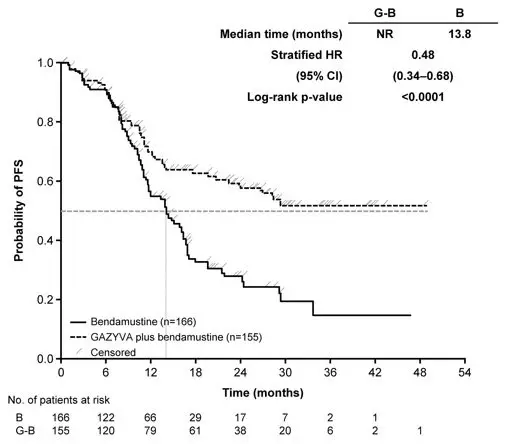
The major efficacy outcome measure was PFS as determined by an independent review committee (IRC). At the time of the primary analysis, median observation time was 21.1 months. The median PFS in the bendamustine arm was 13.8 months. Median PFS was not reached in the GAZYVA plus bendamustine arm (PFS HR = 0.48, 95% CI: 0.34-0.68; stratified log-rank test p-value < 0.0001). The investigator assessed PFS result was consistent with the IRC-assessed PFS. The median investigator-assessed PFS in the bendamustine arm was 13.7 months and the median in the GAZYVA containing arm was 29.2 months (PFS HR = 0.48, 95% CI: 0.35-0.67; stratified log-rank test p-value < 0.0001).
Efficacy results are summarized in Table 14. The Kaplan-Meier curve for IRC-PFS is shown in Figure 3.
| Endpoint | GADOLIN | |
|---|---|---|
| GAZYVA + Bendamustine followed by GAZYVA monotherapy n = 155 | Bendamustine n = 166 |
|
|
||
| Median Progression-Free Survival (months) | Not Reached | 13.8 |
| (HR = 0.48 [0.34; 0.68], p-value < 0.0001 by stratified log-rank test) | ||
| Best Overall Response‡ | 78.7% | 74.7% |
| Complete Response | 15.5% | 18.7% |
| Partial Response | 63.2% | 56.0% |
| Median duration of response (months) | Not Reached | 11.6 |
| Figure 3 Kaplan-Meier Curve of IRC-Assessed Progression-Free Survival in Patients with FL |
 |
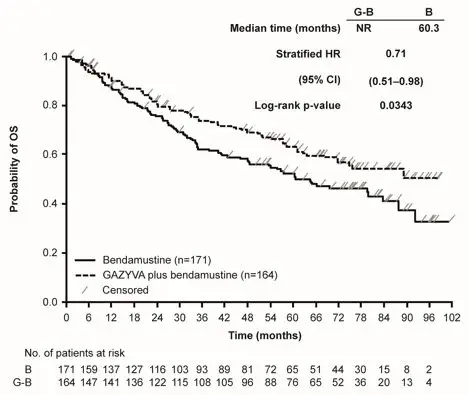
The final analysis included a total of 335 patients with 171 randomized to bendamustine alone and 164 to GAZYVA in combination with bendamustine. With an overall median observation time of 52.2 months (range: 0-100.9 months), there were 66 deaths (40.2%) in the GAZYVA arm and 85 deaths (51.3%) in the bendamustine-alone arm (OS HR = 0.71, 95% CI: 0.51, 0.98). The Kaplan-Meier curve for OS is presented in Figure 4.
| Figure 4 Kaplan-Meier Curve of Overall Survival in Patients with FL |
 |
GALLIUM
The efficacy of GAZYVA was evaluated in GALLIUM (NCT01332968), a multicenter, open-label, randomized study that included 1202 patients with previously untreated, stage II bulky, III or IV FL. Patients were randomized 1:1 to receive either GAZYVA (n = 601) or rituximab product (n = 601) in combination with chemotherapy (CHOP, CVP, or bendamustine) for 6–8 cycles. Patients were stratified by chemotherapy (selected by each site; all patients at that site received the chosen chemotherapy regimen), FLIPI (Follicular Lymphoma International Prognostic Index) risk group and geographic region. Patients with at least PR to combination therapy received monotherapy with GAZYVA (1,000 mg) or rituximab product every two months until disease progression or for a maximum of two years. The study excluded patients with follicular lymphoma grade 3b or transformed disease; patients having an ANC < 1500 / µL, platelets < 75,000 / µL, or CLcr < 40 mL/min; and patients with hepatic transaminases > 2.5 × upper limit of normal unless attributable to lymphoma.
GAZYVA was given by intravenous infusion as a flat dose of 1,000 mg on Days 1, 8 and 15 of Cycle 1 and Day 1 of subsequent treatment cycles.
GAZYVA and bendamustine were given in six 28-day cycles. Bendamustine was administered at 90 mg/m2/day on Days 1 and 2 of each cycle, with prednisone 100 mg orally or equivalent on Day 1 of Cycle 1.
GAZYVA and CHOP were given in six 21-day cycles. Subsequently, two additional cycles of GAZYVA were given for a total of 8 GAZYVA cycles. CHOP consisted of cyclophosphamide 750 mg/m2 intravenously, doxorubicin 50 mg/m2, and vincristine 1.4 mg/m2 (maximum dose, 2 mg) on Day 1 and prednisone 100 mg orally on Days 1-5.
GAZYVA and CVP were given in eight 21-day cycles. CVP consisted of cyclophosphamide 750 mg/m2 intravenously and vincristine 1.4 mg/m2 (maximum dose, 2 mg) on Day 1 and prednisone 100 mg orally on Days 1-5.
Patients had a median age of 59 years, 81% were White and 53% were female; 7% had Stage II, 35% had Stage III, and 56% had Stage IV disease, with 44% having bulky disease (≥ 7 cm) overall; 79% had a FLIPI score of > 2; and 97% had an ECOG performance status of 0–1. The chemotherapy was bendamustine in 57%, CHOP in 33%, and CVP in 10% of patients.
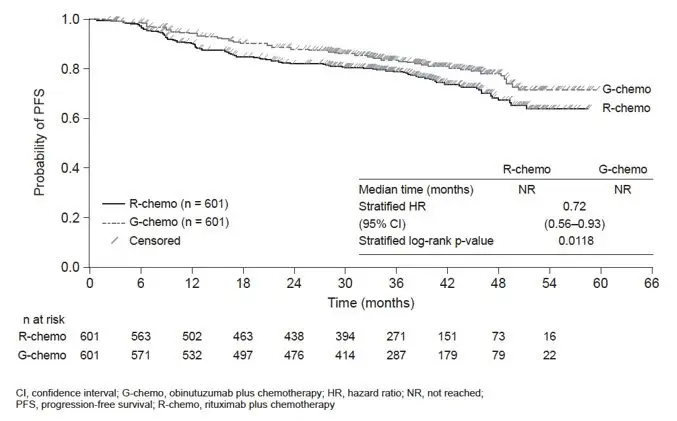
Efficacy was based on PFS per IRC, with a median observation time of 38 months. Upon interim analysis, the risk of progression or death was significantly reduced in the GAZYVA containing arm compared to the rituximab product containing arm (Table 15). Kaplan-Meier curves for PFS are shown in Figure 5. Overall response and complete remission rates were similar.
| Endpoint per IRC | GAZYVA + chemotherapy followed by GAZYVA monotherapy n = 601 | Rituximab product + chemotherapy followed by rituximab product monotherapy n = 601 |
|---|---|---|
|
||
| Progression-Free Survival *
Number of events (%) | 108 (18%) | 141 (23%) |
| HR = 0.72 [95% CI: 0.56, 0.93], p-value = 0.0118 † | ||
| Overall Response Rate ‡ | 91% | 88% |
| Complete Remission Rate ‡ | 28% | 27% |
| Figure 5 Kaplan-Meier Curves of Progression Free Survival in Patients with Previously Untreated FL |
|
|
16. How is Gazyva supplied
GAZYVA is a clear, colorless to slightly brown, preservative-free solution for intravenous use supplied as 1,000 mg/40 mL (25 mg/mL) in single-dose vials (NDC 50242-070-01).
17. Patient Counseling Information
Advise patients to seek immediate medical attention for any of the following:
- Signs and symptoms of infusion-related reactions including dizziness, nausea, chills, fever, vomiting, diarrhea, breathing problems, or chest pain [see Warnings and Precautions (5.3) and Adverse Reactions (6.1)].
- Symptoms of tumor lysis syndrome such as nausea, vomiting, diarrhea, and lethargy [see Warnings and Precautions (5.5) and Adverse Reactions (6.1)].
- Signs of infections including fever and cough [see Warnings and Precautions (5.6) and Adverse Reactions (6.1)].
- Symptoms of hepatitis including worsening fatigue or yellow discoloration of skin or eyes [see Warnings and Precautions (5.1)].
- New or changes in neurological symptoms such as confusion, dizziness or loss of balance, difficulty talking or walking, or vision problems [see Warnings and Precautions (5.2)].
- Signs and symptoms of bleeding or thrombosis [see Warnings and Precautions (5.8 and 5.9)].
Advise patients of the need for:
- Periodic monitoring of blood counts [see Warnings and Precautions (5.7, 5.8 and 5.9) and Adverse Reactions (6.1)].
- Avoid vaccinations with live viral vaccines [see Warnings and Precautions (5.10)].
- Patients with a history of hepatitis B infection (based on the blood test) should be monitored and sometimes treated for their hepatitis [see Warnings and Precautions (5.1)].
Advise pregnant women of potential fetal B-cell depletion. Advise females of reproductive potential to inform their healthcare provider of a known or suspected pregnancy [see Warnings and Precautions (5.11), Use in Specific Populations (8.1)].
Advise females of reproductive potential to use effective contraception during treatment with GAZYVA and for 6 months after the last dose [see Use in Specific Populations (8.3)].
Advise women not to breastfeed during treatment with GAZYVA and for 6 months after the last dose [see Use in Specific Populations (8.2)].
| GAZYVA
obinutuzumab injection, solution, concentrate |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Genentech, Inc. (080129000) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Roche Diagnostics GmbH | 315028860 | ANALYSIS(50242-070) , MANUFACTURE(50242-070) , PACK(50242-070) , LABEL(50242-070) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| F. Hoffmann-La Roche Ltd | 485244961 | LABEL(50242-070) , PACK(50242-070) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Roche Diagnostics GmbH | 323105205 | API MANUFACTURE(50242-070) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Genentech, Inc. | 080129000 | ANALYSIS(50242-070) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Genentech, Inc. | 146373191 | ANALYSIS(50242-070) | |