Drug Detail:Gleevec (Imatinib)
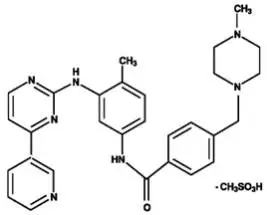
Drug Class: BCR-ABL tyrosine kinase inhibitors
Highlights of Prescribing Information
GLEEVEC® (imatinib mesylate) tablets, for oral use
Initial U.S. Approval: 2001
Indications and Usage for Gleevec
Gleevec is a kinase inhibitor indicated for the treatment of:
- Newly diagnosed adult and pediatric patients with Philadelphia chromosome positive chronic myeloid leukemia (Ph+ CML) in chronic phase. (1.1)
- Patients with Philadelphia chromosome positive chronic myeloid leukemia (Ph+ CML) in blast crisis (BC), accelerated phase (AP), or in chronic phase (CP) after failure of interferon-alpha therapy. (1.2)
- Adult patients with relapsed or refractory Philadelphia chromosome positive acute lymphoblastic leukemia (Ph+ ALL). (1.3)
- Pediatric patients with newly diagnosed Philadelphia chromosome positive acute lymphoblastic leukemia (Ph+ ALL) in combination with chemotherapy. (1.4)
- Adult patients with myelodysplastic/myeloproliferative diseases (MDS/MPD) associated with platelet-derived growth factor receptor (PDGFR) gene re-arrangements. (1.5)
- Adult patients with aggressive systemic mastocytosis (ASM) without the D816V c-Kit mutation or with c-Kit mutational status unknown. (1.6)
- Adult patients with hypereosinophilic syndrome (HES) and/or chronic eosinophilic leukemia (CEL) who have the FIP1L1-PDGFRα fusion kinase (mutational analysis or fluorescence in situ hybridization [FISH] demonstration of CHIC2 allele deletion) and for patients with HES and/or CEL who are FIP1L1-PDGFRα fusion kinase negative or unknown. (1.7)
- Adult patients with unresectable, recurrent and/or metastatic dermatofibrosarcoma protuberans (DFSP). (1.8)
- Patients with Kit (CD117) positive unresectable and/or metastatic malignant gastrointestinal stromal tumors (GIST). (1.9)
- Adjuvant treatment of adult patients following resection of Kit (CD117) positive GIST. (1.10)
Gleevec Dosage and Administration
- Adults with Ph+ CML CP (2.2):
400 mg/day
- Adults with Ph+ CML AP or BC (2.2):
600 mg/day
- Pediatrics with Ph+ CML CP (2.3):
340 mg/m2/day
- Adults with Ph+ ALL (2.4):
600 mg/day
- Pediatrics with Ph+ ALL (2.5):
340 mg/m2/day
- Adults with MDS/MPD (2.6):
400 mg/day
- Adults with ASM (2.7):
100 mg/day or 400 mg/day
- Adults with HES/CEL (2.8):
100 mg/day or 400 mg/day
- Adults with DFSP (2.9):
800 mg/day
- Adults with metastatic and/or unresectable GIST (2.10):
400 mg/day
- Adjuvant treatment of adults with GIST (2.11):
400 mg/day
- Patients with mild to moderate hepatic impairment (2.12):
400 mg/day
- Patients with severe hepatic impairment (2.12): 300 mg/day
All doses of Gleevec should be taken with a meal and a large glass of water. Doses of 400 mg or 600 mg should be administered once daily, whereas a dose of 800 mg should be administered as 400 mg twice a day. Gleevec can be dissolved in water or apple juice for patients having difficulty swallowing. Daily dosing of 800 mg and above should be accomplished using the 400-mg tablet to reduce exposure to iron.
Dosage Forms and Strengths
Tablets (scored): 100 mg and 400 mg (3)
Contraindications
None. (4)
Warnings and Precautions
- Edema and severe fluid retention have occurred. Weigh patients regularly and manage unexpected rapid weight gain by drug interruption and diuretics. (5.1, 6.1)
- Cytopenias, particularly anemia, neutropenia, and thrombocytopenia, have occurred. Manage with dose reduction, dose interruption, or discontinuation of treatment. Perform complete blood counts weekly for the first month, biweekly for the second month, and periodically thereafter. (5.2)
- Severe congestive heart failure and left ventricular dysfunction have been reported, particularly in patients with comorbidities and risk factors. Monitor and treat patients with cardiac disease or risk factors for cardiac failure. (5.3)
- Severe hepatotoxicity, including fatalities may occur. Assess liver function before initiation of treatment and monthly thereafter or as clinically indicated. Monitor liver function when combined with chemotherapy known to be associated with liver dysfunction. (5.4)
- Grade 3/4 hemorrhage has been reported in clinical studies in patients with newly diagnosed CML and with GIST. GI tumor sites may be the source of GI bleeds in GIST. (5.5)
- Gastrointestinal (GI) perforations, some fatal, have been reported. (5.6)
- Cardiogenic shock/left ventricular dysfunction has been associated with the initiation of Gleevec in patients with conditions associated with high eosinophil levels (e.g., HES, MDS/MPD, and ASM). (5.7)
- Bullous dermatologic reactions (e.g., erythema multiforme and Stevens-Johnson syndrome) have been reported with the use of Gleevec. (5.8)
- Hypothyroidism has been reported in thyroidectomy patients undergoing levothyroxine replacement. Closely monitor TSH levels in such patients. (5.9)
- Fetal harm can occur when administered to a pregnant woman. Apprise women of the potential harm to the fetus, and to avoid pregnancy when taking Gleevec. (5.10, 8.1)
- Growth retardation occurring in children and pre-adolescents receiving Gleevec has been reported. Close monitoring of growth in children under Gleevec treatment is recommended. (5.11, 6.2)
- Tumor Lysis Syndrome. Close monitoring is recommended. (5.12)
- Reports of motor vehicle accidents have been received in patients receiving Gleevec. Caution patients about driving a car or operating machinery. (5.13)
- Renal Toxicity. A decline in renal function may occur in patients receiving Gleevec. Evaluate renal function at baseline and during therapy, with attention to risk factors for renal dysfunction. (5.14)
Adverse Reactions/Side Effects
The most frequently reported adverse reactions (greater than or equal to 30%) were edema, nausea, vomiting, muscle cramps, musculoskeletal pain, diarrhea, rash, fatigue, and abdominal pain. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Novartis Pharmaceuticals Corporation at 1-888-669-6682 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- CYP3A4 inducers may decrease Gleevec Cmax and area under curve (AUC). (2.12, 7.1, 12.3)
- CYP3A4 inhibitors may increase Gleevec Cmax and AUC. (7.2, 12.3)
- Gleevec is an inhibitor of CYP3A4 and CYP2D6 which may increase the Cmax and AUC of other drugs. (7.3, 7.4, 12.3)
- Patients who require anticoagulation should receive low-molecular weight or standard heparin and not warfarin. (7.3)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 3/2022
Full Prescribing Information
1. Indications and Usage for Gleevec
1.1 Newly Diagnosed Philadelphia Positive Chronic Myeloid Leukemia (Ph+ CML)
Newly diagnosed adult and pediatric patients with Philadelphia chromosome positive chronic myeloid leukemia (Ph+ CML) in chronic phase.
1.2 Ph+ CML in Blast Crisis (BC), Accelerated Phase (AP) or Chronic Phase (CP) After Interferon-alpha (IFN) Therapy
Patients with Philadelphia chromosome positive chronic myeloid leukemia in blast crisis, accelerated phase, or in chronic phase after failure of interferon-alpha therapy.
1.3 Adult Patients With Ph+ Acute Lymphoblastic Leukemia (ALL)
Adult patients with relapsed or refractory Philadelphia chromosome positive acute lymphoblastic leukemia (Ph+ ALL).
1.4 Pediatric Patients With Ph+ Acute Lymphoblastic Leukemia (ALL)
Pediatric patients with newly diagnosed Philadelphia chromosome positive acute lymphoblastic leukemia (Ph+ ALL) in combination with chemotherapy.
1.5 Myelodysplastic/Myeloproliferative Diseases (MDS/MPD)
Adult patients with myelodysplastic/myeloproliferative diseases associated with platelet-derived growth factor receptor (PDGFR) gene re-arrangements.
1.6 Aggressive Systemic Mastocytosis (ASM)
Adult patients with aggressive systemic mastocytosis without the D816V c-Kit mutation or with c-Kit mutational status unknown.
1.7 Hypereosinophilic Syndrome (HES) and/or Chronic Eosinophilic Leukemia (CEL)
Adult patients with hypereosinophilic syndrome and/or chronic eosinophilic leukemia who have the FIP1L1-PDGFRα fusion kinase (mutational analysis or fluorescence in situ hybridization [FISH] demonstration of CHIC2 allele deletion) and for patients with HES and/or CEL who are FIP1L1-PDGFRα fusion kinase negative or unknown.
1.8 Dermatofibrosarcoma Protuberans (DFSP)
Adult patients with unresectable, recurrent and/or metastatic dermatofibrosarcoma protuberans.
2. Gleevec Dosage and Administration
2.1 Drug Administration
The prescribed dose should be administered orally, with a meal and a large glass of water. Doses of 400 mg or 600 mg should be administered once daily, whereas a dose of 800 mg should be administered as 400 mg twice a day.
For patients unable to swallow the film-coated tablets, the tablets may be dispersed in a glass of water or apple juice. The required number of tablets should be placed in the appropriate volume of beverage (approximately 50 mL for a 100-mg tablet, and 200 mL for a 400-mg tablet) and stirred with a spoon. The suspension should be administered immediately after complete disintegration of the tablet(s).
For daily dosing of 800 mg and above, dosing should be accomplished using the 400-mg tablet to reduce exposure to iron.
Treatment may be continued as long as there is no evidence of progressive disease or unacceptable toxicity.
2.2 Adult Patients With Ph+ CML CP, AP, or BC
The recommended dose of Gleevec is 400 mg/day for adult patients in chronic phase CML and 600 mg/day for adult patients in accelerated phase or blast crisis.
In CML, a dose increase from 400 mg to 600 mg in adult patients with chronic phase disease, or from 600 mg to 800 mg (given as 400 mg twice daily) in adult patients in accelerated phase or blast crisis may be considered in the absence of severe adverse drug reaction and severe non-leukemia related neutropenia or thrombocytopenia in the following circumstances: disease progression (at any time), failure to achieve a satisfactory hematologic response after at least 3 months of treatment, failure to achieve a cytogenetic response after 6 to 12 months of treatment, or loss of a previously achieved hematologic or cytogenetic response.
2.3 Pediatric Patients With Ph+ CML CP
The recommended dose of Gleevec for children with newly diagnosed Ph+ CML is 340 mg/m2/day (not to exceed 600 mg). Gleevec treatment can be given as a once daily dose or the daily dose may be split into two–one portion dosed in the morning and one portion in the evening. There is no experience with Gleevec treatment in children under 1 year of age.
2.4 Adult Patients With Ph+ ALL
The recommended dose of Gleevec is 600 mg/day for adult patients with relapsed/refractory Ph+ ALL.
2.5 Pediatric Patients With Ph+ ALL
The recommended dose of Gleevec to be given in combination with chemotherapy to children with newly diagnosed Ph+ ALL is 340 mg/m2/day (not to exceed 600 mg). Gleevec treatment can be given as a once daily dose.
2.6 Adult Patients With MDS/MPD
Determine PDGFRb gene rearrangements status prior to initiating treatment.
The recommended dose of Gleevec is 400 mg/day for adult patients with MDS/MPD.
2.7 Adult Patients With ASM
Determine D816V c-Kit mutation status prior to initiating treatment.
The recommended dose of Gleevec is 400 mg/day for adult patients with ASM without the D816V c-Kit mutation. If c-Kit mutational status is not known or unavailable, treatment with Gleevec 400 mg/day may be considered for patients with ASM not responding satisfactorily to other therapies. For patients with ASM associated with eosinophilia, a clonal hematological disease related to the fusion kinase FIP1L1-PDGFRα, a starting dose of 100 mg/day is recommended. Dose increase from 100 mg to 400 mg for these patients may be considered in the absence of adverse drug reactions if assessments demonstrate an insufficient response to therapy.
2.8 Adult Patients With HES/CEL
The recommended dose of Gleevec is 400 mg/day for adult patients with HES/CEL. For HES/CEL patients with demonstrated FIP1L1-PDGFRα fusion kinase, a starting dose of 100 mg/day is recommended. Dose increase from 100 mg to 400 mg for these patients may be considered in the absence of adverse drug reactions if assessments demonstrate an insufficient response to therapy.
2.9 Adult Patients With DFSP
The recommended dose of Gleevec is 800 mg/day for adult patients with DFSP.
2.10 Adult Patients With Metastatic and/or Unresectable GIST
The recommended dose of Gleevec is 400 mg/day for adult patients with unresectable and/or metastatic, malignant GIST. A dose increase up to 800 mg daily (given as 400 mg twice daily) may be considered, as clinically indicated, in patients showing clear signs or symptoms of disease progression at a lower dose and in the absence of severe adverse drug reactions.
2.11 Adult Patients With Adjuvant GIST
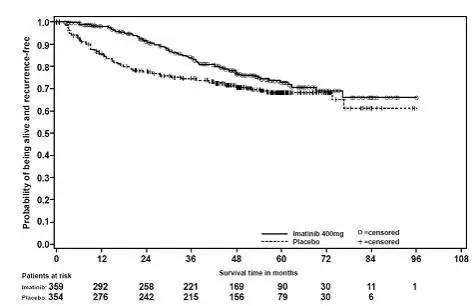
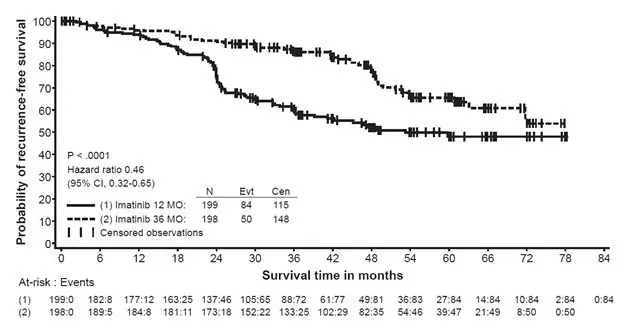
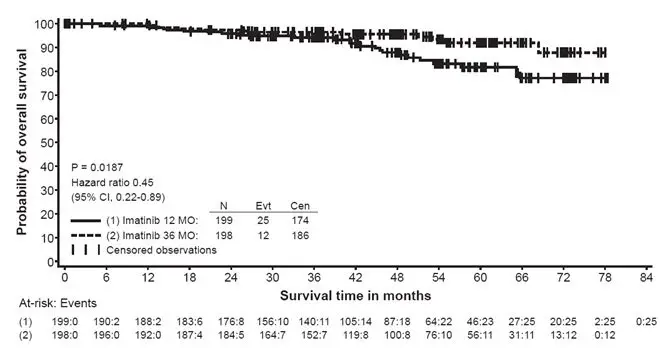
The recommended dose of Gleevec is 400 mg/day for the adjuvant treatment of adult patients following complete gross resection of GIST. In clinical trials, one year of Gleevec and three years of Gleevec were studied. In the patient population defined in Study 2, three years of Gleevec is recommended [see Clinical Studies (14.8)]. The optimal treatment duration with Gleevec is not known.
2.12 Dose Modification Guidelines
Concomitant Strong CYP3A4 inducers: The use of concomitant strong CYP3A4 inducers should be avoided (e.g., dexamethasone, phenytoin, carbamazepine, rifampin, rifabutin, rifampacin, phenobarbital). If patients must be coadministered a strong CYP3A4 inducer, based on pharmacokinetic studies, the dosage of Gleevec should be increased by at least 50%, and clinical response should be carefully monitored [see Drug Interactions (7.1)].
Hepatic Impairment: Patients with mild and moderate hepatic impairment do not require a dose adjustment and should be treated per the recommended dose. A 25% decrease in the recommended dose should be used for patients with severe hepatic impairment [see Use in Specific Populations (8.6)].
Renal Impairment: Patients with moderate renal impairment (creatinine clearance [CrCL] = 20-39 mL/min) should receive a 50% decrease in the recommended starting dose and future doses can be increased as tolerated. Doses greater than 600 mg are not recommended in patients with mild renal impairment (CrCL = 40-59 mL/min). For patients with moderate renal impairment doses greater than 400 mg are not recommended.
Imatinib should be used with caution in patients with severe renal impairment. A dose of 100 mg/day was tolerated in two patients with severe renal impairment [see Warnings and Precautions (5.3), Use in Specific Populations (8.7)].
5. Warnings and Precautions
5.1 Fluid Retention and Edema
Gleevec is often associated with edema and occasionally serious fluid retention [see Adverse Reactions (6.1)]. Weigh and monitor patients regularly for signs and symptoms of fluid retention. Investigate unexpected rapid weight gain carefully and provide appropriate treatment. The probability of edema was increased with higher Gleevec dose and age greater than 65 years in the CML studies. Severe superficial edema was reported in 1.5% of newly diagnosed CML patients taking Gleevec, and in 2% to 6% of other adult CML patients taking Gleevec. In addition, other severe fluid retention (e.g., pleural effusion, pericardial effusion, pulmonary edema, and ascites) reactions were reported in 1.3% of newly diagnosed CML patients taking Gleevec, and in 2% to 6% of other adult CML patients taking Gleevec. Severe fluid retention was reported in 9% to 13.1% of patients taking Gleevec for GIST [see Adverse Reactions (6.1)]. In a randomized trial in patients with newly diagnosed Ph+ CML in chronic phase comparing Gleevec and nilotinib, severe (Grade 3 or 4) fluid retention occurred in 2.5% of patients receiving Gleevec and in 3.9% of patients receiving nilotinib 300 mg twice daily. Effusions (including pleural effusion, pericardial effusion, ascites) or pulmonary edema were observed in 2.1% (none were Grade 3 or 4) of patients in the Gleevec arm and 2.2% (0.7% Grade 3 or 4) of patients in the nilotinib 300 mg twice daily arm.
5.2 Hematologic Toxicity
Treatment with Gleevec is associated with anemia, neutropenia, and thrombocytopenia. Perform complete blood counts weekly for the first month, biweekly for the second month, and periodically thereafter as clinically indicated (for example, every 2 to 3 months). In CML, the occurrence of these cytopenias is dependent on the stage of disease and is more frequent in patients with accelerated phase CML or blast crisis than in patients with chronic phase CML. In pediatric CML patients the most frequent toxicities observed were Grade 3 or 4 cytopenias, including neutropenia, thrombocytopenia, and anemia. These generally occur within the first several months of therapy [see Dosage and Administration (2.14)].
5.3 Congestive Heart Failure and Left Ventricular Dysfunction
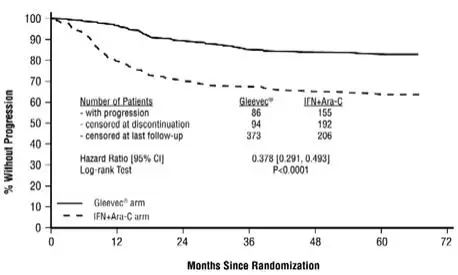
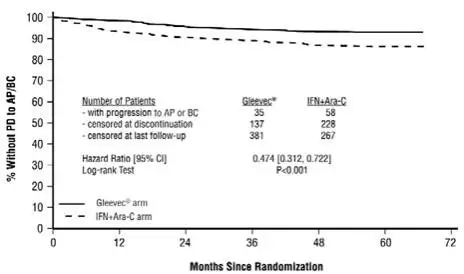
Congestive heart failure and left ventricular dysfunction have been reported in patients taking Gleevec. Cardiac adverse reactions were more frequent in patients with advanced age or co-morbidities, including previous medical history of cardiac disease. In an international randomized Phase 3 study in 1106 patients with newly diagnosed Ph+ CML in chronic phase, severe cardiac failure and left ventricular dysfunction were observed in 0.7% of patients taking Gleevec compared to 0.9% of patients taking IFN + Ara-C. In another randomized trial with newly diagnosed Ph+ CML patients in chronic phase that compared Gleevec and nilotinib, cardiac failure was observed in 1.1% of patients in the Gleevec arm and 2.2% of patients in the nilotinib 300 mg twice daily arm and severe (Grade 3 or 4) cardiac failure occurred in 0.7% of patients in each group. Carefully monitor patients with cardiac disease or risk factors for cardiac or history of renal failure. Evaluate and treat any patient with signs or symptoms consistent with cardiac or renal failure.
5.4 Hepatotoxicity
Hepatotoxicity, occasionally severe, may occur with Gleevec [see Adverse Reactions (6.1)]. Cases of fatal liver failure and severe liver injury requiring liver transplants have been reported with both short-term and long-term use of Gleevec. Monitor liver function (transaminases, bilirubin, and alkaline phosphatase) before initiation of treatment and monthly, or as clinically indicated. Manage laboratory abnormalities with Gleevec interruption and/or dose reduction [see Dosage and Administration (2.13)]. When Gleevec is combined with chemotherapy, liver toxicity in the form of transaminase elevation and hyperbilirubinemia has been observed. Additionally, there have been reports of acute liver failure. Monitoring of hepatic function is recommended.
5.5 Hemorrhage
In a trial of Gleevec versus IFN+Ara-C in patients with the newly diagnosed CML, 1.8% of patients had Grade 3/4 hemorrhage. In the Phase 3 unresectable or metastatic GIST studies, 211 patients (12.9%) reported Grade 3/4 hemorrhage at any site. In the Phase 2 unresectable or metastatic GIST study, 7 patients (5%) had a total of 8 CTC Grade 3/4 hemorrhages; gastrointestinal (GI) (3 patients), intra-tumoral (3 patients) or both (1 patient). Gastrointestinal tumor sites may have been the source of GI hemorrhages. In a randomized trial in patients with newly diagnosed Ph+ CML in chronic phase comparing Gleevec and nilotinib, GI hemorrhage occurred in 1.4% of patients in the Gleevec arm, and in 2.9% of patients in the nilotinib 300 mg twice daily arm. None of these events were Grade 3 or 4 in the Gleevec arm; 0.7% were Grade 3 or 4 in the nilotinib 300 mg twice daily arm. In addition, gastric antral vascular ectasia has been reported in postmarketing experience.
5.6 Gastrointestinal Disorders
Gleevec is sometimes associated with GI irritation. Gleevec should be taken with food and a large glass of water to minimize this problem. There have been rare reports, including fatalities, of GI perforation.
5.7 Hypereosinophilic Cardiac Toxicity
In patients with hypereosinophilic syndrome with occult infiltration of HES cells within the myocardium, cases of cardiogenic shock/left ventricular dysfunction have been associated with HES cell degranulation upon the initiation of Gleevec therapy. The condition was reported to be reversible with the administration of systemic steroids, circulatory support measures and temporarily withholding Gleevec.
Myelodysplastic/myeloproliferative disease and systemic mastocytosis may be associated with high eosinophil levels. Consider performing an echocardiogram and determining serum troponin in patients with HES/CEL, and in patients with MDS/MPD or ASM associated with high eosinophil levels. If either is abnormal, consider prophylactic use of systemic steroids (1-2 mg/kg) for one to two weeks concomitantly with Gleevec at the initiation of therapy.
5.8 Dermatologic Toxicities
Bullous dermatologic reactions, including erythema multiforme and Stevens-Johnson syndrome, have been reported with use of Gleevec. In some cases of bullous dermatologic reactions, including erythema multiforme and Stevens-Johnson syndrome reported during postmarketing surveillance, a recurrent dermatologic reaction was observed upon rechallenge. Several foreign postmarketing reports have described cases in which patients tolerated the reintroduction of Gleevec therapy after resolution or improvement of the bullous reaction. In these instances, Gleevec was resumed at a dose lower than that at which the reaction occurred and some patients also received concomitant treatment with corticosteroids or antihistamines.
5.9 Hypothyroidism
Clinical cases of hypothyroidism have been reported in thyroidectomy patients undergoing levothyroxine replacement during treatment with Gleevec. Monitor TSH levels in such patients.
5.10 Embryo-Fetal Toxicity
Gleevec can cause fetal harm when administered to a pregnant woman. Imatinib mesylate was teratogenic in rats when administered during organogenesis at doses approximately equal to the maximum human dose of 800 mg/day based on body surface area (BSA). Significant post-implantation loss was seen in female rats administered imatinib mesylate at doses approximately one-half the maximum human dose of 800 mg/day based on BSA. Advise sexually active female patients of reproductive potential to use effective contraception (methods that result in less than 1% pregnancy rates) when using Gleevec and for 14 days after stopping Gleevec. If this drug is used during pregnancy or if the patient becomes pregnant while taking this drug, apprise the patient of the potential hazard to a fetus [see Use in Specific Populations (8.1)].
5.11 Growth Retardation in Children and Adolescents
Growth retardation has been reported in children and pre-adolescents receiving Gleevec. The long-term effects of prolonged treatment with Gleevec on growth in children are unknown. Therefore, monitor growth in children under Gleevec treatment [see Adverse Reactions (6.1)].
5.12 Tumor Lysis Syndrome
Cases of Tumor Lysis Syndrome (TLS), including fatal cases, have been reported in patients with CML, GIST, ALL, and eosinophilic leukemia receiving Gleevec. The patients at risk of TLS are those with tumors having a high proliferative rate or high tumor burden prior to treatment. Monitor these patients closely and take appropriate precautions. Due to possible occurrence of TLS, correct clinically significant dehydration and treat high uric acid levels prior to initiation of Gleevec.
5.13 Impairments Related to Driving and Using Machinery
Motor vehicle accidents have been reported in patients receiving Gleevec. Advise patients that they may experience side effects, such as dizziness, blurred vision, or somnolence during treatment with Gleevec. Recommend caution when driving a car or operating machinery.
5.14 Renal Toxicity
A decline in renal function may occur in patients receiving Gleevec. Median estimated glomerular filtration rate (eGFR) values in patients on Gleevec 400 mg daily for newly-diagnosed CML (four randomized trials) and malignant GIST (one single-arm trial) declined from a baseline value of 85 mL/min/1.73 m2 (N = 1190) to 75 mL/min/1.73 m2 at 12 months (N = 1082) and 69 mL/min/1.73 m2 at 60 months (N = 549). Evaluate renal function prior to initiating Gleevec and monitor during therapy, with attention to risk factors for renal dysfunction, such as preexisting renal impairment, diabetes mellitus, hypertension, and congestive heart failure.
6. Adverse Reactions/Side Effects
The following serious adverse reactions are described elsewhere in the labeling:
- Fluid Retention and Edema [see Warnings and Precautions (5.1)]
- Hematologic Toxicity [see Warnings and Precautions (5.2)]
- Congestive Heart Failure and Left Ventricular Dysfunction [see Warnings and Precautions (5.3)]
- Hepatotoxicity [see Warnings and Precautions (5.4)]
- Hemorrhage [see Warnings and Precautions (5.5)]
- Gastrointestinal Disorders [see Warnings and Precautions (5.6)]
- Hypereosinophilic Cardiac Toxicity [see Warnings and Precautions (5.7)]
- Dermatologic Toxicities [see Warnings and Precautions (5.8)]
- Hypothyroidism [see Warnings and Precautions (5.9)]
- Growth Retardation in Children and Adolescents [see Warnings and Precautions (5.11)]
- Tumor Lysis Syndrome [see Warnings and Precautions (5.12)]
- Impairments Related to Driving and Using Machinery [see Warnings and Precautions (5.13)]
- Renal Toxicity [see Warnings and Precautions (5.14)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Chronic Myeloid Leukemia
The majority of Gleevec-treated patients experienced adverse reactions at some time. Gleevec was discontinued due to drug-related adverse reactions in 2.4% of patients receiving Gleevec in the randomized trial of newly diagnosed patients with Ph+ CML in chronic phase comparing Gleevec versus IFN+Ara-C, and in 12.5% of patients receiving Gleevec in the randomized trial of newly diagnosed patients with Ph+ CML in chronic phase comparing Gleevec and nilotinib. Gleevec was discontinued due to drug-related adverse reactions in 4% of patients in chronic phase after failure of interferon-alpha therapy, in 4% of patients in accelerated phase and in 5% of patients in blast crisis.
The most frequently reported drug-related adverse reactions were edema, nausea and vomiting, muscle cramps, musculoskeletal pain, diarrhea and rash (Table 2 and Table 3 for newly diagnosed CML, Table 4 for other CML patients). Edema was most frequently periorbital or in lower limbs and was managed with diuretics, other supportive measures, or by reducing the dose of Gleevec [see Dosage and Administration (2.13)]. The frequency of severe superficial edema was 1.5%-6%.
A variety of adverse reactions represent local or general fluid retention, including pleural effusion, ascites, pulmonary edema, and rapid weight gain with or without superficial edema. These reactions appear to be dose related, were more common in the blast crisis and accelerated phase studies (where the dose was 600 mg/day), and are more common in the elderly. These reactions were usually managed by interrupting Gleevec treatment and using diuretics or other appropriate supportive care measures. These reactions may be serious or life threatening.
Adverse reactions, regardless of relationship to study drug, that were reported in at least 10% of the Gleevec-treated patients are shown in Tables 2, 3, and 4.
| Abbreviations: CML, chronic myeloid leukemia; CNS, central nervous system; CTC, common terminology criteria; GI, gastrointestinal; IFN, Interferon-alpha. *NCI Common Terminology Criteria for Adverse Events, version 3.0. (1)All adverse reactions occurring in greater than or equal to10% of Gleevec-treated patients are listed regardless of suspected relationship to treatment. (2)Other fluid retention reactions include pleural effusion, ascites, pulmonary edema, pericardial effusion, anasarca, edema aggravated, and fluid retention not otherwise specified. |
||||
| All Grades | CTC Grades* 3/4 | |||
| Gleevec | IFN+Ara−C | Gleevec | IFN+Ara−C | |
| Preferred Term | N = 551 (%) | N = 533 (%) | N = 551 (%) | N = 533 (%) |
| Fluid retention | 61.7 | 11.1 | 2.5 | 0.9 |
| − Superficial edema | 59.9 | 9.6 | 1.5 | 0.4 |
| − Other fluid retention reactions2 | 6.9 | 1.9 | 1.3 | 0.6 |
| Nausea | 49.5 | 61.5 | 1.3 | 5.1 |
| Muscle cramps | 49.2 | 11.8 | 2.2 | 0.2 |
| Musculoskeletal pain | 47.0 | 44.8 | 5.4 | 8.6 |
| Diarrhea | 45.4 | 43.3 | 3.3 | 3.2 |
| Rash and related terms | 40.1 | 26.1 | 2.9 | 2.4 |
| Fatigue | 38.8 | 67.0 | 1.8 | 25.1 |
| Headache | 37.0 | 43.3 | 0.5 | 3.8 |
| Joint pain | 31.4 | 38.1 | 2.5 | 7.7 |
| Abdominal pain | 36.5 | 25.9 | 4.2 | 3.9 |
| Nasopharyngitis | 30.5 | 8.8 | 0 | 0.4 |
| Hemorrhage | 28.9 | 21.2 | 1.8 | 1.7 |
| - GI hemorrhage | 1.6 | 1.1 | 0.5 | 0.2 |
| - CNS hemorrhage | 0.2 | 0.4 | 0 | 0.4 |
| Myalgia | 24.1 | 38.8 | 1.5 | 8.3 |
| Vomiting | 22.5 | 27.8 | 2.0 | 3.4 |
| Dyspepsia | 18.9 | 8.3 | 0 | 0.8 |
| Cough | 20.0 | 23.1 | 0.2 | 0.6 |
| Pharyngolaryngeal pain | 18.1 | 11.4 | 0.2 | 0 |
| Upper respiratory tract infection | 21.2 | 8.4 | 0.2 | 0.4 |
| Dizziness | 19.4 | 24.4 | 0.9 | 3.8 |
| Pyrexia | 17.8 | 42.6 | 0.9 | 3.0 |
| Weight increased | 15.6 | 2.6 | 2.0 | 0.4 |
| Insomnia | 14.7 | 18.6 | 0 | 2.3 |
| Depression | 14.9 | 35.8 | 0.5 | 13.1 |
| Influenza | 13.8 | 6.2 | 0.2 | 0.2 |
| Bone pain | 11.3 | 15.6 | 1.6 | 3.4 |
| Constipation | 11.4 | 14.4 | 0.7 | 0.2 |
| Sinusitis | 11.4 | 6.0 | 0.2 | 0.2 |
| Abbreviation: Ph+ CML-CP, Philadelphia chromosome positive chronic myeloid leukemia-chronic phase. aExcluding laboratory abnormalities. bNCI Common Terminology Criteria for Adverse Events, version 3.0. |
|||||
| Patients With Newly Diagnosed Ph+ CML-CP | |||||
| Gleevec
400 mg once daily | nilotinib
300 mg twice daily | Gleevec
400 mg once daily | nilotinib
300 mg twice daily |
||
| N = 280 | N = 279 | N = 280 | N = 279 | ||
| Body System and Preferred Term | All Grades (%) | CTC Gradesb 3/4 (%) | |||
| Skin and subcutaneous tissue disorders |
Rash |
19 |
38 |
2 |
< 1 |
| Pruritus | 7 | 21 | 0 | < 1 | |
| Alopecia | 7 | 13 | 0 | 0 | |
| Dry skin | 6 | 12 | 0 | 0 | |
| Gastrointestinal disorders | Nausea | 41 | 22 | 2 | 2 |
| Constipation | 8 | 20 | 0 | < 1 | |
| Diarrhea | 46 | 19 | 4 | 1 | |
| Vomiting | 27 | 15 | < 1 | < 1 | |
| Abdominal pain upper | 14 | 18 | < 1 | 1 | |
| Abdominal pain | 12 | 15 | 0 | 2 | |
| Dyspepsia | 12 | 10 | 0 | 0 | |
| Nervous system disorders | Headache | 23 | 32 | < 1 | 3 |
| Dizziness | 11 | 12 | < 1 | < 1 | |
| General disorders and administration-site conditions |
Fatigue |
20 |
23 |
1 |
1 |
| Pyrexia | 13 | 14 | 0 | < 1 | |
| Asthenia | 12 | 14 | 0 | < 1 | |
| Peripheral edema | 20 | 9 | 0 | < 1 | |
| Face edema | 14 | < 1 | < 1 | 0 | |
| Musculoskeletal and connective tissue disorders |
Myalgia |
19 |
19 |
< 1 |
< 1 |
| Arthralgia | 17 | 22 | < 1 | < 1 | |
| Muscle spasms | 34 | 12 | 1 | 0 | |
| Pain in extremity | 16 | 15 | < 1 | < 1 | |
| Back pain | 17 | 19 | 1 | 1 | |
| Respiratory, thoracic and mediastinal disorders |
Cough |
13 |
17 |
0 |
0 |
| Oropharyngeal pain | 6 | 12 | 0 | 0 | |
| Dyspnea | 6 | 11 | < 1 | 2 | |
| Infections and infestations | Nasopharyngitis | 21 | 27 | 0 | 0 |
| Upper respiratory tract infection |
14 |
17 |
0 |
< 1 |
|
| Influenza | 9 | 13 | 0 | 0 | |
| Gastroenteritis | 10 | 7 | < 1 | 0 | |
| Eye disorders | Eyelid edema | 19 | 1 | < 1 | 0 |
| Periorbital edema | 15 | < 1 | 0 | 0 | |
| Psychiatric disorders | Insomnia | 9 | 11 | 0 | 0 |
| Vascular disorder | Hypertension | 4 | 10 | < 1 | 1 |
| Abbreviations: CML, chronic myeloid leukemia; IFN, Interferon-alpha. (1)All adverse reactions occurring in greater than or equal to 10% of patients are listed regardless of suspected relationship to treatment. (2)Other fluid retention reactions include pleural effusion, ascites, pulmonary edema, pericardial effusion, anasarca, edema aggravated, and fluid retention not otherwise specified. |
||||||
| Myeloid Blast Crisis
(n = 260) | Accelerated Phase
(n = 235) | Chronic Phase, IFN Failure
(n = 532) |
||||
| % | % | % | ||||
| Preferred Term | All Grades | Grade 3/4 | All Grades | Grade 3/4 | All Grades | Grade 3/4 |
| Fluid Retention | 72 | 11 | 76 | 6 | 69 | 4 |
| -Superficial edema | 66 | 6 | 74 | 3 | 67 | 2 |
| -Other Fluid Retention Reactions (2) | 22 | 6 | 15 | 4 | 7 | 2 |
| Nausea | 71 | 5 | 73 | 5 | 63 | 3 |
| Muscle cramps | 28 | 1 | 47 | 0.4 | 62 | 2 |
| Vomiting | 54 | 4 | 58 | 3 | 36 | 2 |
| Diarrhea | 43 | 4 | 57 | 5 | 48 | 3 |
| Hemorrhage | 53 | 19 | 49 | 11 | 30 | 2 |
| - CNS hemorrhage | 9 | 7 | 3 | 3 | 2 | 1 |
| - GI hemorrhage | 8 | 4 | 6 | 5 | 2 | 0.4 |
| Musculoskeletal pain | 42 | 9 | 49 | 9 | 38 | 2 |
| Fatigue | 30 | 4 | 46 | 4 | 48 | 1 |
| Skin rash | 36 | 5 | 47 | 5 | 47 | 3 |
| Pyrexia | 41 | 7 | 41 | 8 | 21 | 2 |
| Arthralgia | 25 | 5 | 34 | 6 | 40 | 1 |
| Headache | 27 | 5 | 32 | 2 | 36 | 0.6 |
| Abdominal pain | 30 | 6 | 33 | 4 | 32 | 1 |
| Weight increased | 5 | 1 | 17 | 5 | 32 | 7 |
| Cough | 14 | 0.8 | 27 | 0.9 | 20 | 0 |
| Dyspepsia | 12 | 0 | 22 | 0 | 27 | 0 |
| Myalgia | 9 | 0 | 24 | 2 | 27 | 0.2 |
| Nasopharyngitis | 10 | 0 | 17 | 0 | 22 | 0.2 |
| Asthenia | 18 | 5 | 21 | 5 | 15 | 0.2 |
| Dyspnea | 15 | 4 | 21 | 7 | 12 | 0.9 |
| Upper respiratory tract infection | 3 | 0 | 12 | 0.4 | 19 | 0 |
| Anorexia | 14 | 2 | 17 | 2 | 7 | 0 |
| Night Sweats | 13 | 0.8 | 17 | 1 | 14 | 0.2 |
| Constipation | 16 | 2 | 16 | 0.9 | 9 | 0.4 |
| Dizziness | 12 | 0.4 | 13 | 0 | 16 | 0.2 |
| Pharyngitis | 10 | 0 | 12 | 0 | 15 | 0 |
| Insomnia | 10 | 0 | 14 | 0 | 14 | 0.2 |
| Pruritus | 8 | 1 | 14 | 0.9 | 14 | 0.8 |
| Hypokalemia | 13 | 4 | 9 | 2 | 6 | 0.8 |
| Pneumonia | 13 | 7 | 10 | 7 | 4 | 1 |
| Anxiety | 8 | 0.8 | 12 | 0 | 8 | 0.4 |
| Liver toxicity | 10 | 5 | 12 | 6 | 6 | 3 |
| Rigors | 10 | 0 | 12 | 0.4 | 10 | 0 |
| Chest pain | 7 | 2 | 10 | 0.4 | 11 | 0.8 |
| Influenza | 0.8 | 0.4 | 6 | 0 | 11 | 0.2 |
| Sinusitis | 4 | 0.4 | 11 | 0.4 | 9 | 0.4 |
Hematologic and Biochemistry Laboratory Abnormalities
Cytopenias, and particularly neutropenia and thrombocytopenia, were a consistent finding in all studies, with a higher frequency at doses greater than or equal to 750 mg (Phase 1 study). The occurrence of cytopenias in CML patients was also dependent on the stage of the disease.
In patients with newly diagnosed CML, cytopenias were less frequent than in the other CML patients (see Tables 5, 6, and 7). The frequency of Grade 3 or 4 neutropenia and thrombocytopenia was between 2- and 3-fold higher in blast crisis and accelerated phase compared to chronic phase (see Tables 4 and 5). The median duration of the neutropenic and thrombocytopenic episodes varied from 2 to 3 weeks, and from 2 to 4 weeks, respectively.
These reactions can usually be managed with either a reduction of the dose or an interruption of treatment with Gleevec, but may require permanent discontinuation of treatment.
| Abbreviations: CML, chronic myeloid leukemia; IFN, Interferon-alpha; SGOT, serum glutamic-oxaloacetic transaminase is now referred to as aspartate aminotransferase (AST); SGPT, serum glutamic-pyruvic transaminase is now referred to as alanine aminotransferase (ALT). *p less than 0.001 (difference in Grade 3 plus 4 abnormalities between the two treatment groups). |
||||
| Gleevec
N = 551 | IFN+Ara−C
N = 533 |
|||
| % | % | |||
| CTC Grades | Grade 3 | Grade 4 | Grade 3 | Grade 4 |
| Hematology Parameters* | ||||
| − Neutropenia* | 13.1 | 3.6 | 20.8 | 4.5 |
| − Thrombocytopenia* | 8.5 | 0.4 | 15.9 | 0.6 |
| − Anemia | 3.3 | 1.1 | 4.1 | 0.2 |
| Biochemistry Parameters | ||||
| − Elevated creatinine | 0 | 0 | 0.4 | 0 |
| − Elevated bilirubin | 0.9 | 0.2 | 0.2 | 0 |
| − Elevated alkaline phosphatase | 0.2 | 0 | 0.8 | 0 |
| − Elevated SGOT (AST)/SGPT (ALT) | 4.7 | 0.5 | 7.1 | 0.4 |
| Abbreviations: CML, chronic myeloid leukemia; SGOT, serum glutamic-oxaloacetic transaminase is now referred to as aspartate aminotransferase (AST); SGPT, serum glutamic-pyruvic transaminase is now referred to as alanine aminotransferase (ALT). *NCI Common Terminology Criteria for Adverse Events, version 3.0. |
||
| Gleevec 400 mg
once daily N = 280 (%) | nilotinib 300 mg
twice daily N = 279 (%) |
|
| Hematologic Parameters | ||
| Thrombocytopenia | 9 | 10 |
| Neutropenia | 22 | 12 |
| Anemia | 6 | 4 |
| Biochemistry Parameters | ||
| Elevated lipase | 4 | 9 |
| Hyperglycemia | < 1 | 7 |
| Hypophosphatemia | 10 | 8 |
| Elevated bilirubin (total) | < 1 | 4 |
| Elevated SGPT (ALT) | 3 | 4 |
| Hyperkalemia | 1 | 2 |
| Hyponatremia | < 1 | 1 |
| Hypokalemia | 2 | < 1 |
| Elevated SGOT (AST) | 1 | 1 |
| Decreased albumin | < 1 | 0 |
| Hypocalcemia | < 1 | < 1 |
| Elevated alkaline phosphatase | < 1 | 0 |
| Elevated creatinine | < 1 | 0 |
| Abbreviations: CML, chronic myeloid leukemia; CTC, common terminology criteria; IFN, Interferon-alpha; SGOT, serum glutamic-oxaloacetic transaminase is now referred to as aspartate aminotransferase (AST); SGPT, serum glutamic-pyruvic transaminase is now referred to as alanine aminotransferase (ALT). (1)CTC Grades: neutropenia (Grade 3 greater than or equal to 0.5–1.0 x 109/L, Grade 4 less than 0.5 x 109/L), thrombocytopenia (Grade 3 greater than or equal to 10–50 x 109/L, Grade 4 less than 10 x 109/L), anemia (hemoglobin greater than or equal to 65–80 g/L, Grade 4 less than 65 g/L), elevated creatinine (Grade 3 greater than 3–6 x upper limit normal range [ULN], Grade 4 greater than 6 x ULN), elevated bilirubin (Grade 3 greater than 3–10 x ULN, Grade 4 greater than 10 x ULN), elevated alkaline phosphatase (Grade 3 greater than 5–20 x ULN, Grade 4 greater than 20 x ULN), elevated SGOT or SGPT (Grade 3 greater than 5–20 x ULN, Grade 4 greater than 20 x ULN). |
||||||
| Myeloid Blast Crisis
(n = 260) | Accelerated Phase
(n = 235) | Chronic Phase, IFN Failure
(n = 532) |
||||
| 600 mg n = 223
400 mg n = 37 | 600 mg n = 158
400 mg n = 77 | 400 mg | ||||
| % | % | % | ||||
| CTC Grades(1) | Grade 3 | Grade 4 | Grade 3 | Grade 4 | Grade 3 | Grade 4 |
| Hematology Parameters | ||||||
| − Neutropenia | 16 | 48 | 23 | 36 | 27 | 9 |
| − Thrombocytopenia | 30 | 33 | 31 | 13 | 21 | < 1 |
| − Anemia | 42 | 11 | 34 | 7 | 6 | 1 |
| Biochemistry Parameters | ||||||
| − Elevated creatinine | 1.5 | 0 | 1.3 | 0 | 0.2 | 0 |
| − Elevated bilirubin | 3.8 | 0 | 2.1 | 0 | 0.6 | 0 |
| − Elevated alkaline phosphatase | 4.6 | 0 | 5.5 | 0.4 | 0.2 | 0 |
| − Elevated SGOT (AST) | 1.9 | 0 | 3.0 | 0 | 2.3 | 0 |
| − Elevated SGPT (ALT) | 2.3 | 0.4 | 4.3 | 0 | 2.1 | 0 |
Hepatotoxicity
Severe elevation of transaminases or bilirubin occurred in approximately 5% of CML patients (see Tables 6 and 7) and were usually managed with dose reduction or interruption (the median duration of these episodes was approximately 1 week). Treatment was discontinued permanently because of liver laboratory abnormalities in less than 1.0% of CML patients. One patient, who was taking acetaminophen regularly for fever, died of acute liver failure. In the Phase 2 GIST trial, Grade 3 or 4 SGPT (ALT) elevations were observed in 6.8% of patients and Grade 3 or 4 SGOT (AST) elevations were observed in 4.8% of patients. Bilirubin elevation was observed in 2.7% of patients.
Adverse Reactions in Pediatric Population
Single-Agent Therapy
The overall safety profile of pediatric patients treated with Gleevec in 93 children studied was similar to that found in studies with adult patients, except that musculoskeletal pain was less frequent (20.5%) and peripheral edema was not reported. Nausea and vomiting were the most commonly reported individual adverse reactions with an incidence similar to that seen in adult patients. Most patients experienced adverse reactions at some time during the study. The incidence of Grade 3/4 events across all types of adverse reactions was 75%; the events with the highest Grade 3/4 incidence in CML pediatric patients were mainly related to myelosuppression.
In Combination with Multi-Agent Chemotherapy
Pediatric and young adult patients with very high risk ALL, defined as those with an expected 5 year event-free survival (EFS) less than 45%, were enrolled after induction therapy on a multicenter, non-randomized cooperative group pilot protocol. The study population included patients with a median age of 10 years (1 to 21 years), 61% of whom were male, 75% were white, 7% were black, and 6% were Asian/Pacific Islander. Patients with Ph+ ALL (n = 92) were assigned to receive Gleevec and treated in 5 successive cohorts. Gleevec exposure was systematically increased in successive cohorts by earlier introduction and more prolonged duration.
The safety of Gleevec given in combination with intensive chemotherapy was evaluated by comparing the incidence of Grade 3 and 4 adverse events, neutropenia (less than 750/mcL) and thrombocytopenia (less than 75,000/mcL) in the 92 patients with Ph+ ALL compared to 65 patients with Ph- ALL enrolled on the trial who did not receive Gleevec. The safety was also evaluated comparing the incidence of adverse events in cycles of therapy administered with or without Gleevec. The protocol included up to 18 cycles of therapy. Patients were exposed to a cumulative total of 1425 cycles of therapy, 778 with Gleevec, and 647 without Gleevec. The adverse events that were reported with a 5% or greater incidence in patients with Ph+ ALL compared to Ph- ALL or with a 1% or greater incidence in cycles of therapy that included Gleevec are presented in Table 8.
| Abbreviations: Ph+ ALL, Philadelphia chromosome positive acute lymphoblastic leukemia; Ph- ALL, Philadelphia chromosome negative acute lymphoblastic leukemia. *Defined as the frequency of adverse events (AEs) per patient per treatment cycles that included Gleevec (includes patients with Ph+ ALL that received cycles with Gleevec). **Defined as the frequency of AEs per patient per treatment cycles that did not include Gleevec (includes patients with Ph+ ALL that received cycles without Gleevec as well as all patients with Ph- ALL who did not receive Gleevec in any treatment cycle). |
||||
| Adverse Event | Per Patient
Incidence Ph+ ALL With Gleevec N = 92 n (%) | Per Patient
Incidence Ph- ALL No Gleevec N = 65 n (%) | Per Patient
Per Cycle Incidence With Gleevec* N = 778 n (%) | Per Patient
Per Cycle Incidence No Gleevec** N = 647 n (%) |
| Grade 3 and 4 Adverse Events | ||||
| Nausea and/or Vomiting | 15 (16) | 6 (9) | 28 (4) | 8 (1) |
| Hypokalemia | 31 (34) | 16 (25) | 72 (9) | 32 (5) |
| Pneumonitis | 7 (8) | 1 (1) | 7 (1) | 1 (< 1) |
| Pleural effusion | 6 (7) | 0 | 6 (1) | 0 |
| Abdominal pain | 8 (9) | 2 (3) | 9 (1) | 3 (< 1) |
| Anorexia | 10 (11) | 3 (5) | 19 (2) | 4 (1) |
| Hemorrhage | 11 (12) | 4 (6) | 17 (2) | 8 (1) |
| Hypoxia | 8 (9) | 2 (3) | 12 (2) | 2 (< 1) |
| Myalgia | 5 (5) | 0 | 4 (1) | 1 (< 1) |
| Stomatitis | 15 (16) | 8 (12) | 22 (3) | 14 (2) |
| Diarrhea | 8 (9) | 3 (5) | 12 (2) | 3 (< 1) |
| Rash/Skin Disorder | 4 (4) | 0 | 5 (1) | 0 |
| Infection | 49 (53) | 32 (49) | 131 (17) | 92 (14) |
| Hepatic (transaminase and/or bilirubin) | 52 (57) | 38 (58) | 172 (22) | 113 (17) |
| Hypotension | 10 (11) | 5 (8) | 16 (2) | 6 (1) |
| Myelosuppression | ||||
| Neutropenia (< 750/mcL) | 92 (100) | 63 (97) | 556 (71) | 218 (34) |
| Thrombocytopenia (< 75,000/mcL) | 90 (92) | 63 (97) | 431 (55) | 329 (51) |
Adverse Reactions in Other Subpopulations
In older patients (greater than or equal to 65 years old), with the exception of edema, where it was more frequent, there was no evidence of an increase in the incidence or severity of adverse reactions. In women there was an increase in the frequency of neutropenia, as well as Grade 1/2 superficial edema, headache, nausea, rigors, vomiting, rash, and fatigue. No differences were seen that were related to race but the subsets were too small for proper evaluation.
Acute Lymphoblastic Leukemia
The adverse reactions were similar for Ph+ ALL as for Ph+ CML. The most frequently reported drug-related adverse reactions reported in the Ph+ ALL studies were mild nausea and vomiting, diarrhea, myalgia, muscle cramps, and rash. Superficial edema was a common finding in all studies and were described primarily as periorbital or lower limb edemas. These edemas were reported as Grade 3/4 events in 6.3% of the patients and may be managed with diuretics, other supportive measures, or in some patients by reducing the dose of Gleevec.
Myelodysplastic/Myeloproliferative Diseases
Adverse reactions, regardless of relationship to study drug, that were reported in at least 10% of the patients treated with Gleevec for MDS/MPD in the Phase 2 study, are shown in Table 9.
| Abbreviation: MPD, Myeloproliferative Disease. | |
| Preferred Term | N = 7
n (%) |
| Nausea | 4 (57.1) |
| Diarrhea | 3 (42.9) |
| Anemia | 2 (28.6) |
| Fatigue | 2 (28.6) |
| Muscle cramp | 3 (42.9) |
| Arthralgia | 2 (28.6) |
| Periorbital edema | 2 (28.6) |
Aggressive Systemic Mastocytosis
All aggressive systemic mastocytosis (ASM) patients experienced at least one adverse reaction at some time. The most frequently reported adverse reactions were diarrhea, nausea, ascites, muscle cramps, dyspnea, fatigue, peripheral edema, anemia, pruritus, rash, and lower respiratory tract infection. None of the 5 patients in the Phase 2 study with ASM discontinued Gleevec due to drug-related adverse reactions or abnormal laboratory values.
Hypereosinophilic Syndrome and Chronic Eosinophilic Leukemia
The safety profile in the HES/CEL patient population does not appear to be different from the safety profile of Gleevec observed in other hematologic malignancy populations, such as Ph+ CML. All patients experienced at least one adverse reaction, the most common being GI, cutaneous and musculoskeletal disorders. Hematological abnormalities were also frequent, with instances of CTC Grade 3 leukopenia, neutropenia, lymphopenia, and anemia.
Dermatofibrosarcoma Protuberans
Adverse reactions, regardless of relationship to study drug, that were reported in at least 10% of the 12 patients treated with Gleevec for DFSP in the Phase 2 study are shown in Table 10.
| Abbreviation: DFSP, dermatofibrosarcoma protuberans. | |
| Preferred Term | N = 12
n (%) |
| Nausea | 5 (41.7) |
| Diarrhea | 3 (25.0) |
| Vomiting | 3 (25.0) |
| Periorbital edema | 4 (33.3) |
| Face edema | 2 (16.7) |
| Rash | 3 (25.0) |
| Fatigue | 5 (41.7) |
| Peripheral edema | 4 (33.3) |
| Pyrexia | 2 (16.7) |
| Eye edema | 4 (33.3) |
| Lacrimation increased | 3 (25.0) |
| Dyspnea exertional | 2 (16.7) |
| Anemia | 3 (25.0) |
| Rhinitis | 2 (16.7) |
| Anorexia | 2 (16.7) |
Clinically relevant or severe laboratory abnormalities in the 12 patients treated with Gleevec for DFSP in the Phase 2 study are presented in Table 11.
| Abbreviation: CTC, common terminology criteria. (1)CTC Grades: neutropenia (Grade 3 greater than or equal to 0.5–1.0 x 109/L, Grade 4 less than 0.5 x 109/L), thrombocytopenia (Grade 3 greater than or equal to 10–50 x 109/L, Grade 4 less than 10 x 109/L), anemia (Grade 3 greater than or equal to 65–80 g/L, Grade 4 less than 65 g/L), elevated creatinine (Grade 3 greater than 3–6 x upper limit normal range [ULN], Grade 4 greater than 6 x ULN). |
||
| N = 12 | ||
| CTC Grades(1) | Grade 3
% | Grade 4
% |
| Hematology Parameters | ||
| - Anemia | 17 | 0 |
| - Thrombocytopenia | 17 | 0 |
| - Neutropenia | 0 | 8 |
| Biochemistry Parameters | ||
| - Elevated Creatinine | 0 | 8 |
Gastrointestinal Stromal Tumors
Unresectable and/or Malignant Metastatic GIST
In the Phase 3 trials, the majority of Gleevec-treated patients experienced adverse reactions at some time. The most frequently reported adverse reactions were edema, fatigue, nausea, abdominal pain, diarrhea, rash, vomiting, myalgia, anemia, and anorexia. Drug was discontinued for adverse reactions in a total of 89 patients (5.4%). Superficial edema, most frequently periorbital or lower extremity edema was managed with diuretics, other supportive measures, or by reducing the dose of Gleevec [see Dosage and Administration (2.13)]. Severe (CTC Grade 3/4) edema was observed in 182 patients (11.1%).
Adverse reactions, regardless of relationship to study drug, that were reported in at least 10% of the patients treated with Gleevec are shown in Table 12.
Overall the incidence of all grades of adverse reactions and the incidence of severe adverse reactions (CTC Grade 3 and above) were similar between the two treatment arms except for edema, which was reported more frequently in the 800 mg group.
| Abbreviations: ANC, absolute neutrophil count; GI, gastrointestinal; GIST, gastrointestinal stromal tumors. | ||||
| Reported or Specified Term | Imatinib 400 mg
N = 818 | Imatinib 800 mg
N = 822 |
||
| All Grades
% | Grades 3/4/5
% | All Grades
% | Grades 3/4/5
% |
|
| Edema | 76.7 | 9.0 | 86.1 | 13.1 |
| Fatigue/lethargy, malaise, asthenia | 69.3 | 11.7 | 74.9 | 12.2 |
| Nausea | 58.1 | 9.0 | 64.5 | 7.8 |
| Abdominal pain/cramping | 57.2 | 13.8 | 55.2 | 11.8 |
| Diarrhea | 56.2 | 8.1 | 58.2 | 8.6 |
| Rash/desquamation | 38.1 | 7.6 | 49.8 | 8.9 |
| Vomiting | 37.4 | 9.2 | 40.6 | 7.5 |
| Myalgia | 32.2 | 5.6 | 30.2 | 3.8 |
| Anemia | 32.0 | 4.9 | 34.8 | 6.4 |
| Anorexia | 31.1 | 6.6 | 35.8 | 4.7 |
| Other GI toxicity | 25.2 | 8.1 | 28.1 | 6.6 |
| Headache | 22.0 | 5.7 | 19.7 | 3.6 |
| Other pain (excluding tumor related pain) | 20.4 | 5.9 | 20.8 | 5.0 |
| Other dermatology/skin toxicity | 17.6 | 5.9 | 20.1 | 5.7 |
| Leukopenia | 17.0 | 0.7 | 19.6 | 1.6 |
| Other constitutional symptoms | 16.7 | 6.4 | 15.2 | 4.4 |
| Cough | 16.1 | 4.5 | 14.5 | 3.2 |
| Infection (without neutropenia) | 15.5 | 6.6 | 16.5 | 5.6 |
| Pruritus | 15.4 | 5.4 | 18.9 | 4.3 |
| Other neurological toxicity | 15.0 | 6.4 | 15.2 | 4.9 |
| Constipation | 14.8 | 5.1 | 14.4 | 4.1 |
| Other renal/genitourinary toxicity | 14.2 | 6.5 | 13.6 | 5.2 |
| Arthralgia (joint pain) | 13.6 | 4.8 | 12.3 | 3.0 |
| Dyspnea (shortness of breath) | 13.6 | 6.8 | 14.2 | 5.6 |
| Fever in absence of neutropenia (ANC < 1.0 x 109/L) | 13.2 | 4.9 | 12.9 | 3.4 |
| Sweating | 12.7 | 4.6 | 8.5 | 2.8 |
| Other hemorrhage | 12.3 | 6.7 | 13.3 | 6.1 |
| Weight gain | 12.0 | 1.0 | 10.6 | 0.6 |
| Alopecia | 11.9 | 4.3 | 14.8 | 3.2 |
| Dyspepsia/heartburn | 11.5 | 0.6 | 10.9 | 0.5 |
| Neutropenia/granulocytopenia | 11.5 | 3.1 | 16.1 | 4.1 |
| Rigors/chills | 11.0 | 4.6 | 10.2 | 3.0 |
| Dizziness/lightheadedness | 11.0 | 4.8 | 10.0 | 2.8 |
| Creatinine increase | 10.8 | 0.4 | 10.1 | 0.6 |
| Flatulence | 10.0 | 0.2 | 10.1 | 0.1 |
| Stomatitis/pharyngitis (oral/pharyngeal mucositis) | 9.2 | 5.4 | 10.0 | 4.3 |
| Lymphopenia | 6.0 | 0.7 | 10.1 | 1.9 |
Clinically relevant or severe abnormalities of routine hematologic or biochemistry laboratory values were not reported or evaluated in the Phase 3 GIST trials. Severe abnormal laboratory values reported in the Phase 2 GIST trial are presented in Table 13.
| Abbreviations: CTC, common terminology criteria; GIST, gastrointestinal stromal tumors; SGOT, serum glutamic-oxaloacetic transaminase is now referred to as aspartate aminotransferase (AST); SGPT, serum glutamic-pyruvic transaminase is now referred to as alanine aminotransferase (ALT). 1CTC Grades: neutropenia (Grade 3 greater than or equal to 0.5–1.0 x 109/L, Grade 4 less than 0.5 x 109/L), thrombocytopenia (Grade 3 greater than or equal to 10–50 x 109/L, Grade 4 less than 10 x 109/L), anemia (Grade 3 greater than or equal to 65–80 g/L, Grade 4 less than 65 g/L), elevated creatinine (Grade 3 greater than 3–6 x upper limit normal range [ULN], Grade 4 greater than 6 x ULN), elevated bilirubin (Grade 3 greater than 3–10 x ULN, Grade 4 greater than 10 x ULN), elevated alkaline phosphatase, SGOT or SGPT (Grade 3 greater than 5–20 x ULN, Grade 4 greater than 20 x ULN), albumin (Grade 3 less than 20 g/L). |
||||
| 400 mg
(n = 73) | 600 mg
(n = 74) |
|||
| % | % | |||
| CTC Grades1 | Grade 3 | Grade 4 | Grade 3 | Grade 4 |
| Hematology Parameters | ||||
| − Anemia | 3 | 0 | 8 | 1 |
| − Thrombocytopenia | 0 | 0 | 1 | 0 |
| − Neutropenia | 7 | 3 | 8 | 3 |
| Biochemistry Parameters | ||||
| − Elevated creatinine | 0 | 0 | 3 | 0 |
| − Reduced albumin | 3 | 0 | 4 | 0 |
| − Elevated bilirubin | 1 | 0 | 1 | 3 |
| − Elevated alkaline phosphatase | 0 | 0 | 3 | 0 |
| − Elevated SGOT (AST) | 4 | 0 | 3 | 3 |
| − Elevated SGPT (ALT) | 6 | 0 | 7 | 1 |
Adjuvant Treatment of GIST
In Study 1, the majority of both Gleevec and placebo-treated patients experienced at least one adverse reaction at some time. The most frequently reported adverse reactions were similar to those reported in other clinical studies in other patient populations and include diarrhea, fatigue, nausea, edema, decreased hemoglobin, rash, vomiting, and abdominal pain. No new adverse reactions were reported in the adjuvant GIST-treatment setting that had not been previously reported in other patient populations, including patients with unresectable and/or malignant metastatic GIST. Drug was discontinued for adverse reactions in 57 patients (17%) and 11 patients (3%) of the Gleevec and placebo-treated patients, respectively. Edema, GI disturbances (nausea, vomiting, abdominal distention, and diarrhea), fatigue, low hemoglobin, and rash were the most frequently reported adverse reactions at the time of discontinuation.
In Study 2, discontinuation of therapy due to adverse reactions occurred in 15 patients (8%) and 27 patients (14%) of the Gleevec 12-month, and 36-month treatment arms, respectively. As in previous trials the most common adverse reactions were diarrhea, fatigue, nausea, edema, decreased hemoglobin, rash, vomiting, and abdominal pain.
Adverse reactions, regardless of relationship to study drug, that were reported in at least 5% of the patients treated with Gleevec are shown in Table 14 (Study 1) and Table 15 (Study 2). There were no deaths attributable to Gleevec treatment in either trial.
| Abbreviations: CTC, common terminology criteria; GIST, gastrointestinal stromal tumors; SGOT, serum glutamic-oxaloacetic transaminase is now referred to as aspartate aminotransferase (AST); SGPT, serum glutamic-pyruvic transaminase is now referred to as alanine aminotransferase (ALT). *NCI Common Terminology Criteria for Adverse Events, version 3.0. (1)All adverse reactions occurring in greater than or equal to 5% of patients are listed regardless of suspected relationship to treatment. A patient with multiple occurrences of an adverse reaction is counted only once in the adverse reaction category. |
||||
| All CTC Grades | CTC Grade 3* and Above | |||
| Gleevec
(n = 337) | Placebo
(n = 345) | Gleevec
(n = 337) | Placebo
(n = 345) |
|
| Preferred Term | % | % | % | % |
| Diarrhea | 59.3 | 29.3 | 3.0 | 1.4 |
| Fatigue | 57.0 | 40.9 | 2.1 | 1.2 |
| Nausea | 53.1 | 27.8 | 2.4 | 1.2 |
| Periorbital edema | 47.2 | 14.5 | 1.2 | 0 |
| Hemoglobin Decreased | 46.9 | 27.0 | 0.6 | 0 |
| Peripheral edema | 26.7 | 14.8 | 0.3 | 0 |
| Rash (Exfoliative) | 26.1 | 12.8 | 2.7 | 0 |
| Vomiting | 25.5 | 13.9 | 2.4 | 0.6 |
| Abdominal pain | 21.1 | 22.3 | 3.0 | 1.4 |
| Headache | 19.3 | 20.3 | 0.6 | 0 |
| Dyspepsia | 17.2 | 13.0 | 0.9 | 0 |
| Anorexia | 16.9 | 8.7 | 0.3 | 0 |
| Weight increased | 16.9 | 11.6 | 0.3 | 0 |
| Liver enzymes (ALT) increased | 16.6 | 13.0 | 2.7 | 0 |
| Muscle spasms | 16.3 | 3.3 | 0 | 0 |
| Neutrophil count decreased | 16.0 | 6.1 | 3.3 | 0.9 |
| Arthralgia | 15.1 | 14.5 | 0 | 0.3 |
| White blood cell count decreased | 14.5 | 4.3 | 0.6 | 0.3 |
| Constipation | 12.8 | 17.7 | 0 | 0.3 |
| Dizziness | 12.5 | 10.7 | 0 | 0.3 |
| Liver enzymes (AST) increased | 12.2 | 7.5 | 2.1 | 0 |
| Myalgia | 12.2 | 11.6 | 0 | 0.3 |
| Blood creatinine increased | 11.6 | 5.8 | 0 | 0.3 |
| Cough | 11.0 | 11.3 | 0 | 0 |
| Pruritus | 11.0 | 7.8 | 0.9 | 0 |
| Weight decreased | 10.1 | 5.2 | 0 | 0 |
| Hyperglycemia | 9.8 | 11.3 | 0.6 | 1.7 |
| Insomnia | 9.8 | 7.2 | 0.9 | 0 |
| Lacrimation increased | 9.8 | 3.8 | 0 | 0 |
| Alopecia | 9.5 | 6.7 | 0 | 0 |
| Flatulence | 8.9 | 9.6 | 0 | 0 |
| Rash | 8.9 | 5.2 | 0.9 | 0 |
| Abdominal distension | 7.4 | 6.4 | 0.3 | 0.3 |
| Back pain | 7.4 | 8.1 | 0.6 | 0 |
| Pain in extremity | 7.4 | 7.2 | 0.3 | 0 |
| Hypokalemia | 7.1 | 2.0 | 0.9 | 0.6 |
| Depression | 6.8 | 6.4 | 0.9 | 0.6 |
| Facial edema | 6.8 | 1.2 | 0.3 | 0 |
| Blood alkaline phosphatase increased | 6.5 | 7.5 | 0 | 0 |
| Dry skin | 6.5 | 5.2 | 0 | 0 |
| Dysgeusia | 6.5 | 2.9 | 0 | 0 |
| Abdominal pain upper | 6.2 | 6.4 | 0.3 | 0 |
| Neuropathy peripheral | 5.9 | 6.4 | 0 | 0 |
| Hypocalcemia | 5.6 | 1.7 | 0.3 | 0 |
| Leukopenia | 5.0 | 2.6 | 0.3 | 0 |
| Platelet count decreased | 5.0 | 3.5 | 0 | 0 |
| Stomatitis | 5.0 | 1.7 | 0.6 | 0 |
| Upper respiratory tract infection | 5.0 | 3.5 | 0 | 0 |
| Vision Blurred | 5.0 | 2.3 | 0 | 0 |
| Abbreviations: AE, adverse event; CTC, common terminology criteria. (1)All adverse reactions occurring in greater than or equal to 5% of patients are listed regardless of suspected relationship to treatment. A patient with multiple occurrences of an adverse reaction is counted only once in the adverse reaction category. |
||||
| Preferred Term | All CTC Grades | CTC Grades 3 and Above | ||
| Gleevec
12 Months (N = 194) % | Gleevec
36 Months (N = 198) % | Gleevec
12 Months (N = 194) % | Gleevec
36 Months (N = 198) % |
|
| Patients with at least one AE | 99.0 | 100.0 | 20.1 | 32.8 |
| Hemoglobin decreased | 72.2 | 80.3 | 0.5 | 0.5 |
| Periorbital edema | 59.3 | 74.2 | 0.5 | 1.0 |
| Blood lactate dehydrogenase increased | 43.3 | 60.1 | 0 | 0 |
| Diarrhea | 43.8 | 54.0 | 0.5 | 2.0 |
| Nausea | 44.8 | 51.0 | 1.5 | 0.5 |
| Muscle spasms | 30.9 | 49.0 | 0.5 | 1.0 |
| Fatigue | 48.5 | 48.5 | 1.0 | 0.5 |
| White blood cell count decreased | 34.5 | 47.0 | 2.1 | 3.0 |
| Pain | 25.8 | 45.5 | 1.0 | 3.0 |
| Blood creatinine increased | 30.4 | 44.4 | 0 | 0 |
| peripheral edema | 33.0 | 40.9 | 0.5 | 1.0 |
| Dermatitis | 29.4 | 38.9 | 2.1 | 1.5 |
| Aspartate aminotransferase increased | 30.9 | 37.9 | 1.5 | 3.0 |
| Alanine aminotransferase increased | 28.9 | 34.3 | 2.1 | 3.0 |
| Neutrophil count decreased | 24.2 | 33.3 | 4.6 | 5.1 |
| Hypoproteinemia | 23.7 | 31.8 | 0 | 0 |
| Infection | 13.9 | 27.8 | 1.5 | 2.5 |
| Weight increased | 13.4 | 26.8 | 0 | 0.5 |
| Pruritus | 12.9 | 25.8 | 0 | 0 |
| Flatulence | 19.1 | 24.7 | 1.0 | 0.5 |
| Vomiting | 10.8 | 22.2 | 0.5 | 1.0 |
| Dyspepsia | 17.5 | 21.7 | 0.5 | 1.0 |
| Hypoalbuminemia | 11.9 | 21.2 | 0 | 0 |
| Edema | 10.8 | 19.7 | 0 | 0.5 |
| Abdominal distension | 11.9 | 19.2 | 0.5 | 0 |
| Headache | 8.2 | 18.2 | 0 | 0 |
| Lacrimation increased | 18.0 | 17.7 | 0 | 0 |
| Arthralgia | 8.8 | 17.2 | 0 | 1.0 |
| Blood alkaline phosphatase increased | 10.8 | 16.7 | 0 | 0.5 |
| Dyspnea | 6.2 | 16.2 | 0.5 | 1.5 |
| Myalgia | 9.3 | 15.2 | 0 | 1.0 |
| Platelet count decreased | 11.3 | 14.1 | 0 | 0 |
| Blood bilirubin increased | 11.3 | 13.1 | 0 | 0 |
| Dysgeusia | 9.3 | 12.6 | 0 | 0 |
| Paresthesia | 5.2 | 12.1 | 0 | 0.5 |
| Vision blurred | 10.8 | 11.1 | 1.0 | 0.5 |
| Alopecia | 11.3 | 10.6 | 0 | 0 |
| Decreased appetite | 9.8 | 10.1 | 0 | 0 |
| Constipation | 8.8 | 9.6 | 0 | 0 |
| Pyrexia | 6.2 | 9.6 | 0 | 0 |
| Depression | 3.1 | 8.1 | 0 | 0 |
| Abdominal pain | 2.6 | 7.6 | 0 | 0 |
| Conjunctivitis | 5.2 | 7.6 | 0 | 0 |
| Photosensitivity reaction | 3.6 | 7.1 | 0 | 0 |
| Dizziness | 4.6 | 6.6 | 0.5 | 0 |
| Hemorrhage | 3.1 | 6.6 | 0 | 0 |
| Dry skin | 6.7 | 6.1 | 0.5 | 0 |
| Nasopharyngitis | 1.0 | 6.1 | 0 | 0.5 |
| Palpitations | 5.2 | 5.1 | 0 | 0 |
Adverse Reactions from Multiple Clinical Trials
Cardiac Disorders:
Estimated 1%-10%: palpitations, pericardial effusion
Estimated 0.1%-1%: congestive cardiac failure, tachycardia, pulmonary edema
Estimated 0.01%-0.1%: arrhythmia, atrial fibrillation, cardiac arrest, myocardial infarction, angina pectoris
Vascular Disorders:
Estimated 1%-10%: flushing, hemorrhage
Estimated 0.1%-1%: hypertension, hypotension, peripheral coldness, Raynaud’s phenomenon, hematoma, subdural hematoma
Investigations:
Estimated 1%-10%: blood creatine phosphokinase (CPK) increased, blood amylase increased
Estimated 0.1%-1%: blood lactate dehydrogenase (LDH) increased
Skin and Subcutaneous Tissue Disorders:
Estimated 1%-10%: dry skin, alopecia, face edema, erythema, photosensitivity reaction, nail disorder, purpura
Estimated 0.1%-1%: exfoliative dermatitis, bullous eruption, psoriasis, rash pustular, contusion, sweating increased, urticaria, ecchymosis, increased tendency to bruise, hypotrichosis, skin hypopigmentation, skin hyperpigmentation, onychoclasis, folliculitis, petechiae, erythema multiforme
Estimated 0.01%-0.1%: vesicular rash, Stevens-Johnson syndrome, acute generalized exanthematous pustulosis, acute febrile neutrophilic dermatosis (Sweet’s syndrome), nail discoloration, angioneurotic edema, leucocytoclastic vasculitis
Gastrointestinal Disorders:
Estimated 1%-10%: abdominal distention, gastroesophageal reflux, dry mouth, gastritis
Estimated 0.1%-1%: gastric ulcer, stomatitis, mouth ulceration, eructation, melena, esophagitis, ascites, hematemesis, chelitis, dysphagia, pancreatitis
Estimated 0.01%-0.1%: colitis, ileus, inflammatory bowel disease
General Disorders and Administration-Site Conditions:
Estimated 1%-10%: weakness, anasarca, chills
Estimated 0.1%-1%: malaise
Blood and Lymphatic System Disorders:
Estimated 1%-10%: pancytopenia, febrile neutropenia, lymphopenia, eosinophilia
Estimated 0.1%-1%: thrombocythemia, bone marrow depression, lymphadenopathy
Estimated 0.01%-0.1%: hemolytic anemia, aplastic anemia
Hepatobiliary Disorders:
Estimated 0.1%-1%: hepatitis, jaundice
Estimated 0.01%-0.1%: hepatic failure and hepatic necrosis1
Immune System Disorders:
Estimated 0.01%-0.1%: angioedema
Infections and Infestations:
Estimated 0.1%-1%: sepsis, herpes simplex, herpes zoster, cellulitis, urinary tract infection, gastroenteritis
Estimated 0.01%-0.1%: fungal infection
Metabolism and Nutrition Disorders:
Estimated 1%-10%: weight decreased, decreased appetite
Estimated 0.1%-1%: dehydration, gout, increased appetite, hyperuricemia, hypercalcemia, hyperglycemia, hyponatremia, hyperkalemia, hypomagnesemia
Musculoskeletal and Connective Tissue Disorders:
Estimated 1%-10%: joint swelling
Estimated 0.1%-1%: joint and muscle stiffness, muscular weakness, arthritis
Nervous System/Psychiatric Disorders:
Estimated 1%-10%: paresthesia, hypesthesia
Estimated 0.1%-1%: syncope, peripheral neuropathy, somnolence, migraine, memory impairment, libido decreased, sciatica, restless leg syndrome, tremor
Estimated 0.01%-0.1%: increased intracranial pressure1, confusional state, convulsions, optic neuritis
Renal and Urinary Disorders:
Estimated 0.1%-1%: renal failure acute, urinary frequency increased, hematuria, renal pain
Reproductive System and Breast Disorders:
Estimated 0.1%-1%: breast enlargement, menorrhagia, sexual dysfunction, gynecomastia, erectile dysfunction, menstruation irregular, nipple pain, scrotal edema
Respiratory, Thoracic and Mediastinal Disorders:
Estimated 1%-10%: epistaxis
Estimated 0.1%-1%: pleural effusion
Estimated 0.01%-0.1%: interstitial pneumonitis, pulmonary fibrosis, pleuritic pain, pulmonary hypertension, pulmonary hemorrhage
Endocrine Disorders:
Estimated 0.1%-1%: hypothyroidism, hyperthyroidism
Eye, Ear, and Labyrinth Disorders:
Estimated 1%-10%: conjunctivitis, vision blurred, orbital edema, conjunctival hemorrhage, dry eye
Estimated 0.1%-1%: vertigo, tinnitus, eye irritation, eye pain, scleral hemorrhage, retinal hemorrhage, blepharitis, macular edema, hearing loss, cataract
Estimated 0.01%-0.1%: papilledema1, glaucoma
1Including some fatalities.
6.2 Postmarketing Experience
The following additional adverse reactions have been identified during post approval use of Gleevec. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
Blood and Lymphatic System Disorders: thrombotic microangiopathy
Cardiac Disorders: pericarditis, cardiac tamponade1
Eye Disorders: vitreous hemorrhage
Gastrointestinal Disorders: ileus/intestinal obstruction, tumor hemorrhage/tumor necrosis, GI perforation1 [see Warnings and Precautions (5.6)], diverticulitis, gastric antral vascular ectasia
Infections: hepatitis B virus reactivation1
Musculoskeletal and Connective Tissue Disorders: osteonecrosis, rhabdomyolysis/myopathy, growth retardation in children, musculoskeletal pain upon treatment discontinuation (including myalgia, pain in extremity, arthalgia, bone pain)
Nervous System Disorders: cerebral edema1
Reproduction Disorders: hemorrhagic corpus luteum/hemorrhagic ovarian cyst
Respiratory, Thoracic and Mediastinal Disorders: acute respiratory failure1, interstitial lung disease
Skin and Subcutaneous Tissue Disorders: lichenoid keratosis, lichen planus, toxic epidermal necrolysis, palmar-plantar erythrodysesthesia syndrome, drug rash with eosinophilia and systemic symptoms (DRESS), pseudoporphyria, pemphigus
Vascular Disorders: thrombosis/embolism, anaphylactic shock
1Including some fatalities.
7. Drug Interactions
7.1 Agents Inducing CYP3A Metabolism
Concomitant administration of Gleevec and strong CYP3A4 inducers may reduce total exposure of imatinib; consider alternative agents [see Clinical Pharmacology (12.3)].
7.2 Agents Inhibiting CYP3A Metabolism
Concomitant administration of Gleevec and strong CYP3A4 inhibitors may result in a significant imatinib exposure increase. Grapefruit juice may also increase plasma concentrations of imatinib; avoid grapefruit juice [see Clinical Pharmacology (12.3)].
7.3 Interactions With Drugs Metabolized by CYP3A4
Gleevec will increase plasma concentration of CYP3A4 metabolized drugs (e.g., triazolo-benzodiazepines, dihydropyridine calcium channel blockers, certain HMG-CoA reductase inhibitors, etc.). Use caution when administering Gleevec with CYP3A4 substrates that have a narrow therapeutic window.
Because warfarin is metabolized by CYP2C9 and CYP3A4, use low-molecular weight or standard heparin instead of warfarin in patients who require anticoagulation [see Clinical Pharmacology (12.3)].
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
Gleevec can cause fetal harm when administered to a pregnant woman based on human and animal data. There are no clinical studies regarding use of Gleevec in pregnant women. There have been postmarket reports of spontaneous abortions and congenital anomalies from women who have been exposed to Gleevec during pregnancy. Reproductive studies in rats have demonstrated that imatinib mesylate induced teratogenicity and increased incidence of congenital abnormalities following prenatal exposure to imatinib mesylate at doses equal to the highest recommended human dose of 800 mg/day based on BSA. Advise women to avoid pregnancy when taking Gleevec. If this drug is used during pregnancy, or if the patient becomes pregnant while taking this drug, apprise the patient of the potential hazard to the fetus.
The background risk of major birth defects and miscarriage for the indicated population is not known; however, in the U.S. general population, the estimated background risk of major birth defects of clinically recognized pregnancies is 2% to 4% and of miscarriage is 15% to 20%.
Data
Animal Data
In embryo-fetal development studies in rats and rabbits, pregnant animals received oral doses of imatinib mesylate up to 100 mg/kg/day and 60 mg/kg/day, respectively, during the period of organogenesis.
In rats, imatinib mesylate was teratogenic at 100 mg/kg/day (approximately equal to the maximum human dose of 800 mg/day based on BSA), the number of fetuses with encephalocoele and exencephaly was higher than historical control values and these findings were associated with missing or underdeveloped cranial bones. Lower mean fetal body weights were associated with retarded skeletal ossifications.
In rabbits, at doses 1.5 times higher than the maximum human dose of 800 mg/day based on BSA, no effects on the reproductive parameters with respect to implantation sites, number of live fetuses, sex ratio or fetal weight were observed. The examinations of the fetuses did not reveal any drug related morphological changes.
In a pre- and postnatal development study in rats, pregnant rats received oral doses of imatinib mesylate during gestation (organogenesis) and lactation up to 45 mg/kg/day. Five animals developed a red vaginal discharge in the 45 mg/kg/day group on Days 14 or 15 of gestation, the significance of which is unknown since all females produced viable litters and none had increased post-implantation loss. Other maternal effects noted only at the dose of 45 mg/kg/day (approximately one-half the maximum human dose of 800 mg/day based on BSA) included an increased number of stillborn pups and pups dying between postpartum Days 0 and 4. In the F1 offspring at this same dose level, mean body weights were reduced from birth until terminal sacrifice and the number of litters achieving criterion for preputial separation was slightly decreased. There were no other significant effects in developmental parameters or behavioral testing. F1 fertility was not affected but reproductive effects were noted at 45 mg/kg/day, including an increased number of resorptions and a decreased number of viable fetuses. The no-observed-effect level (NOEL) for both maternal animals and the F1 generation was 15 mg/kg/day.
12. Gleevec - Clinical Pharmacology
12.3 Pharmacokinetics
The pharmacokinetics of Gleevec have been evaluated in studies in healthy subjects and in population pharmacokinetic studies in over 900 patients. The pharmacokinetics of Gleevec are similar in CML and GIST patients.
Absorption and Distribution
Imatinib is well absorbed after oral administration with Cmax achieved within 2-4 hours post-dose. Mean absolute bioavailability is 98%. Mean imatinib AUC increases proportionally with increasing doses ranging from 25 mg to 1,000 mg. There is no significant change in the pharmacokinetics of imatinib on repeated dosing, and accumulation is 1.5- to 2.5-fold at steady state when Gleevec is dosed once daily. At clinically relevant concentrations of imatinib, binding to plasma proteins in in vitro experiments is approximately 95%, mostly to albumin and α1-acid glycoprotein.
Elimination
Metabolism
CYP3A4 is the major enzyme responsible for metabolism of imatinib. Other cytochrome P450 enzymes, such as CYP1A2, CYP2D6, CYP2C9, and CYP2C19, play a minor role in its metabolism. The main circulating active metabolite in humans is the N-demethylated piperazine derivative, formed predominantly by CYP3A4. It shows in vitro potency similar to the parent imatinib. The plasma AUC for this metabolite is about 15% of the AUC for imatinib. The plasma protein binding of N-demethylated metabolite CGP74588 is similar to that of the parent compound. Human liver microsome studies demonstrated that Gleevec is a potent competitive inhibitor of CYP2C9, CYP2D6, and CYP3A4/5 with Ki values of 27, 7.5, and 8 µM, respectively.
Excretion
Imatinib elimination is predominately in the feces, mostly as metabolites. Based on the recovery of compound(s) after an oral 14C-labeled dose of imatinib, approximately 81% of the dose was eliminated within 7 days, in feces (68% of dose) and urine (13% of dose). Unchanged imatinib accounted for 25% of the dose (5% urine, 20% feces), the remainder being metabolites.
Following oral administration in healthy volunteers, the elimination half-lives of imatinib and its major active metabolite, the N-demethyl derivative (CGP74588), are approximately 18 and 40 hours, respectively.
Typically, clearance of imatinib in a 50-year-old patient weighing 50 kg is expected to be 8 L/h, while for a 50-year-old patient weighing 100 kg the clearance will increase to 14 L/h. The inter-patient variability of 40% in clearance does not warrant initial dose adjustment based on body weight and/or age but indicates the need for close monitoring for treatment-related toxicity.
Specific Populations
Hepatic Impairment
The effect of hepatic impairment on the pharmacokinetics of both imatinib and its major metabolite, CGP74588, was assessed in 84 patients with cancer and varying degrees of hepatic impairment [see Use in Specific Populations (8.6)] at imatinib doses ranging from 100 mg to 800 mg. Exposure to both imatinib and CGP74588 was comparable between each of the mildly and moderately hepatically-impaired groups and the normal group. Patients with severe hepatic impairment tend to have higher exposure to both imatinib and its metabolite than patients with normal hepatic function. At steady state, the mean Cmax/dose and AUC/dose for imatinib increased by about 63% and 45%, respectively, in patients with severe hepatic impairment compared to patients with normal hepatic function. The mean Cmax/dose and AUC/dose for CGP74588 increased by about 56% and 55%, respectively, in patients with severe hepatic impairment compared to patients with normal hepatic function. Dose reductions are necessary for patients with severe hepatic impairment [see Dosage and Administration (2.12)].
Renal Impairment
The effect of renal impairment on the pharmacokinetics of imatinib was assessed in 59 cancer patients with varying degrees of renal impairment [see Use in Specific Populations (8.7)] at single and steady state imatinib doses ranging from 100 to 800 mg/day. The mean exposure to imatinib (dose normalized AUC) in patients with mild and moderate renal impairment increased 1.5- to 2-fold compared to patients with normal renal function. The AUCs did not increase for doses greater than 600 mg in patients with mild renal impairment. The AUCs did not increase for doses greater than 400 mg in patients with moderate renal impairment. Two patients with severe renal impairment were dosed with 100 mg/day and their exposures were similar to those seen in patients with normal renal function receiving 400 mg/day. Dose reductions are necessary for patients with moderate and severe renal impairment [see Dosage and Administration (2.12)].
Pediatric Use
As in adult patients, imatinib was rapidly absorbed after oral administration in pediatric patients, with a Cmax of 2–4 hours. Apparent oral clearance was similar to adult values (11.0 L/hr/m2 in children vs 10.0 L/hr/m2 in adults), as was the half-life (14.8 hours in children vs 17.1 hours in adults). Dosing in children at both 260 mg/m2 and 340 mg/m2 achieved an AUC similar to the 400 mg dose in adults. The comparison of AUC on Day 8 vs Day 1 at 260 mg/m2 and 340 mg/m2 dose levels revealed a 1.5- and 2.2-fold drug accumulation, respectively, after repeated once-daily dosing. Mean imatinib AUC did not increase proportionally with increasing dose.
Based on pooled population pharmacokinetic analysis in pediatric patients with hematological disorders (CML, Ph+ ALL, or other hematological disorders treated with imatinib), clearance of imatinib increases with increasing BSA. After correcting for the BSA effect, other demographics, such as age, body weight, and body mass index did not have clinically significant effects on the exposure of imatinib. The analysis confirmed that exposure of imatinib in pediatric patients receiving 260 mg/m2 once daily (not exceeding 400 mg once daily) or 340 mg/m2 once daily (not exceeding 600 mg once daily) were similar to those in adult patients who received imatinib 400 mg or 600 mg once daily.
Drug Interactions
Agents Inducing CYP3A Metabolism
Pretreatment of healthy volunteers with multiple doses of rifampin followed by a single dose of Gleevec, increased Gleevec oral-dose clearance by 3.8-fold, which significantly (p less than 0.05) decreased mean Cmax and AUC.
Similar findings were observed in patients receiving 400 to 1200 mg/day Gleevec concomitantly with enzyme-inducing anti-epileptic drugs (EIAED) (e.g., carbamazepine, oxcarbamazepine, phenytoin, fosphenytoin, phenobarbital, and primidone). The mean dose normalized AUC for imatinib in the patients receiving EIAED’s decreased by 73% compared to patients not receiving EIAED.
Concomitant administration of Gleevec and St. John’s Wort led to a 30% reduction in the AUC of imatinib.
Consider alternative therapeutic agents with less enzyme induction potential in patients when rifampin or other CYP3A4 inducers are indicated. Gleevec doses up to 1,200 mg/day (600 mg twice daily) have been given to patients receiving concomitant strong CYP3A4 inducers [see Dosage and Administration (2.12)].
Agents Inhibiting CYP3A Metabolism
There was a significant increase in exposure to imatinib (mean Cmax and AUC increased by 26% and 40%, respectively) in healthy subjects when Gleevec was coadministered with a single dose of ketoconazole (a CYP3A4 inhibitor). Caution is recommended when administering Gleevec with strong CYP3A4 inhibitors (e.g., ketoconazole, itraconazole, clarithromycin, atazanavir, indinavir, nefazodone, nelfinavir, ritonavir, saquinavir, telithromycin, and voriconazole). Grapefruit juice may also increase plasma concentrations of imatinib and should be avoided.
Interactions with Drugs Metabolized by CYP3A4
Gleevec increases the mean Cmax and AUC of simvastatin (CYP3A4 substrate) 2- and 3.5-fold, respectively, suggesting an inhibition of the CYP3A4 by Gleevec. Particular caution is recommended when administering Gleevec with CYP3A4 substrates that have a narrow therapeutic window (e.g., alfentanil, cyclosporine, diergotamine, ergotamine, fentanyl, pimozide, quinidine, sirolimus, or tacrolimus).
Gleevec will increase plasma concentration of other CYP3A4 metabolized drugs (e.g., triazolo-benzodiazepines, dihydropyridine calcium channel blockers, certain HMG-CoA reductase inhibitors, etc.).
Because warfarin is metabolized by CYP2C9 and CYP3A4, patients who require anticoagulation should receive low-molecular weight or standard heparin instead of warfarin.
Interactions with Drugs Metabolized by CYP2D6
Gleevec increased the mean Cmax and AUC of metoprolol by approximately 23% suggesting that Gleevec has a weak inhibitory effect on CYP2D6-mediated metabolism. No dose adjustment is necessary, however, caution is recommended when administering Gleevec with CYP2D6 substrates that have a narrow therapeutic window.
Interactions with Acetaminophen
In vitro, Gleevec inhibits the acetaminophen O-glucuronidate pathway (Ki 58.5 µM). Coadministration of Gleevec (400 mg/day for 8 days) with acetaminophen (1,000 mg single dose on Day 8) in patients with CML did not result in any changes in the pharmacokinetics of acetaminophen. Gleevec pharmacokinetics were not altered in the presence of single-dose acetaminophen. There is no pharmacokinetic or safety data on the concomitant use of Gleevec at doses greater than 400 mg/day or the chronic use of concomitant acetaminophen and Gleevec.
| GLEEVEC
imatinib mesylate tablet |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| GLEEVEC
imatinib mesylate tablet |
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
|
||||||||||||||||||||||||
| Labeler - Novartis Pharmaceuticals Corporation (002147023) |