Drug Detail:Hizentra (Immune globulin (subcutaneous) [ im-myoon-glob-yoo-lin ])
Drug Class: Immune globulins
Highlights of Prescribing Information
HIZENTRA, Immune Globulin Subcutaneous (Human), 20% Liquid
Initial U.S. Approval: 2010
WARNING: THROMBOSIS
See full prescribing information for complete boxed warning.
- Thrombosis may occur with immune globulin products, including HIZENTRA. Risk factors may include: advanced age, prolonged immobilization, hypercoagulable conditions, history of venous or arterial thrombosis, use of estrogens, indwelling vascular catheters, hyperviscosity, and cardiovascular risk factors.
- For patients at risk of thrombosis, administer HIZENTRA at the minimum dose and infusion rate practicable. Ensure adequate hydration in patients before administration. Monitor for signs and symptoms of thrombosis and assess blood viscosity in patients at risk for hyperviscosity.
Recent Major Changes
| Dosage and Administration (2.3) | 04/2023 |
Indications and Usage for Hizentra
HIZENTRA is an Immune Globulin Subcutaneous (Human) (IGSC), 20% Liquid indicated for the treatment of:
- Primary immunodeficiency (PI) in adults and pediatric patients 2 years of age and older. (1.1)
- Maintenance therapy in adults with chronic inflammatory demyelinating polyneuropathy (CIDP). (1.2)
Hizentra Dosage and Administration
For subcutaneous infusion only.
Dose (2.2)
PI
Before switching to HIZENTRA, obtain the patient's serum IgG trough level to guide subsequent dose adjustments.
- Weekly: Start HIZENTRA 1 week after last Immune Globulin Intravenous (Human) (IGIV) infusion.
| Initial weekly dose = | Previous IGIV dose (in grams) × 1.37 |
| No. of weeks between IGIV doses |
- Biweekly (every 2 weeks): Start HIZENTRA 1 or 2 weeks after the last IGIV infusion or 1 week after the last weekly IGSC infusion. Administer twice the calculated weekly dose.
- Frequent dosing (2 to 7 times per week): Start HIZENTRA 1 week after the last IGIV or IGSC infusion. Divide the calculated weekly dose by the desired number of times per week.
- Adjust the dose based on clinical response and serum IgG trough levels.
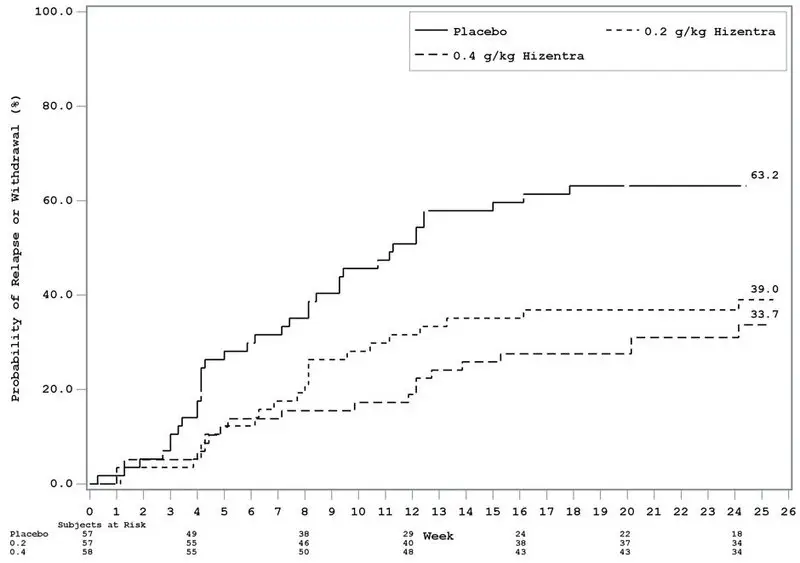
CIDP
- Initiate therapy with HIZENTRA 1 week after the last IGIV infusion.
- Recommended subcutaneous dose is 0.2 g/kg (1 mL/kg) body weight per week.
- -
- In the clinical study after transitioning from IGIV to HIZENTRA, a dose of 0.4 g/kg (2 mL/kg) body weight per week was also safe and effective to prevent CIDP relapse.
- If CIDP symptoms worsen, on 0.2 g/kg (1 mL/kg) body weight per week, consider increasing the HIZENTRA dose from 0.2 g/kg to 0.4 g/kg body weight per week.
- -
- If CIDP symptoms worsen on 0.4 g/kg body weight per week, consider re-initiating therapy with IGIV, while discontinuing HIZENTRA.
- Monitor patient's clinical response and adjust duration of therapy based on patient need.
Administration (2.3)
- PI: Administer at regular intervals from daily up to every 2 weeks.
- CIDP: Administer weekly.
- Infusion sites – Up to 8 infusion sites are allowed simultaneously, with at least 2 inches between sites.
| Infusion Parameters* | 1st Infusion | Subsequent Infusions |
|---|---|---|
|
||
| Volume (mL/site) | ≤15 | ≤25 |
| Rate (mL/hr/site) | ≤15 | ≤25 |
| Infusion Parameters* | 1st Infusion | Subsequent Infusions |
|---|---|---|
|
||
| Volume (mL/site) | ≤20 | ≤50 |
| Rate (mL/hr/site) | ≤20 | ≤50 |
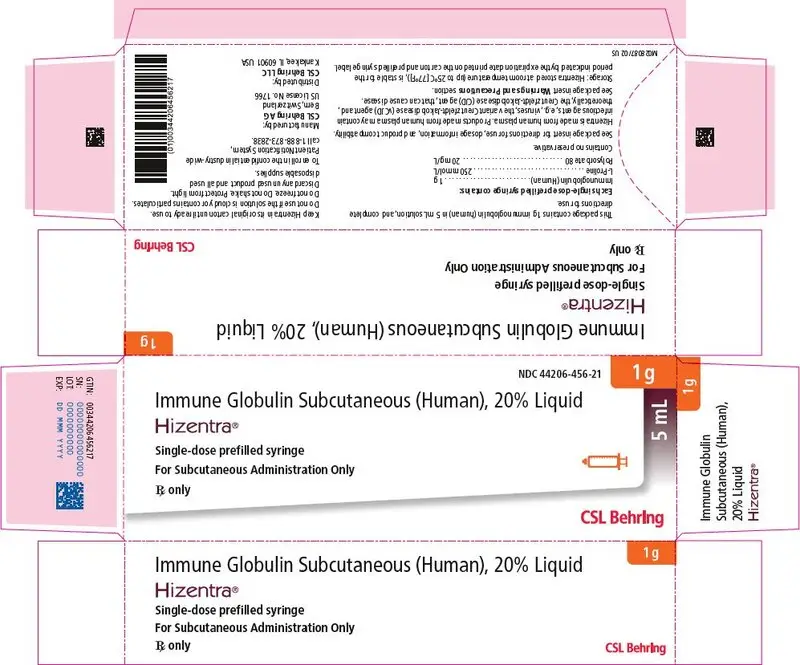
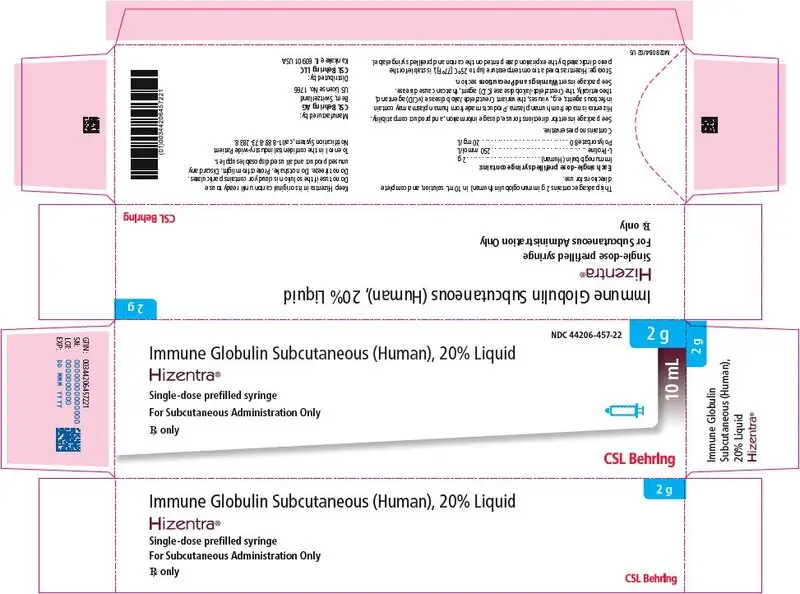
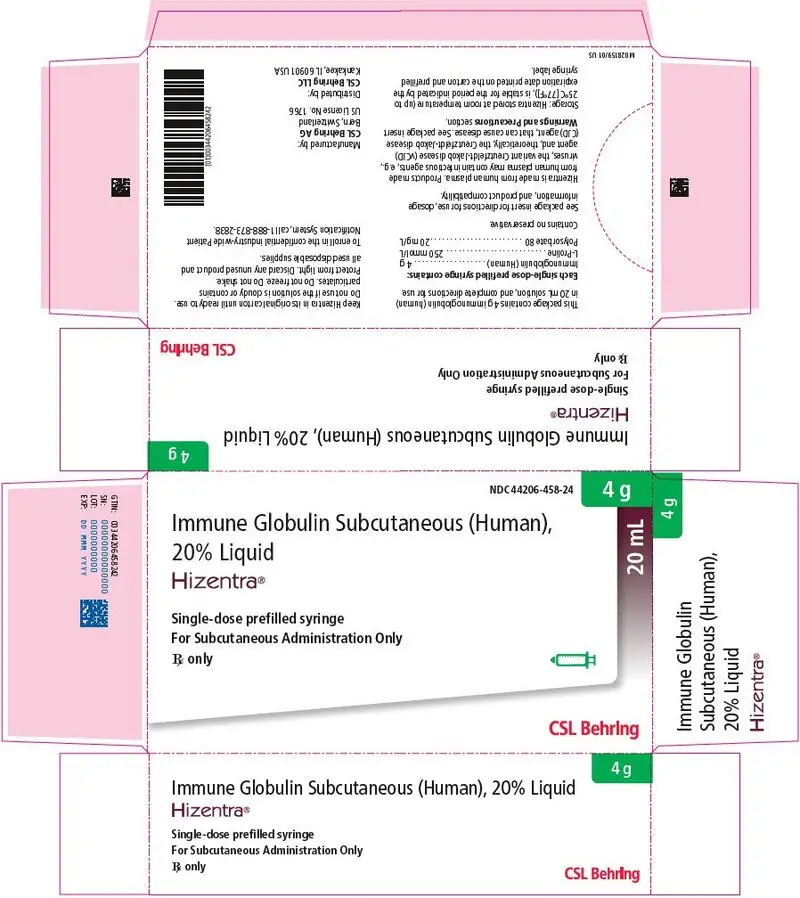
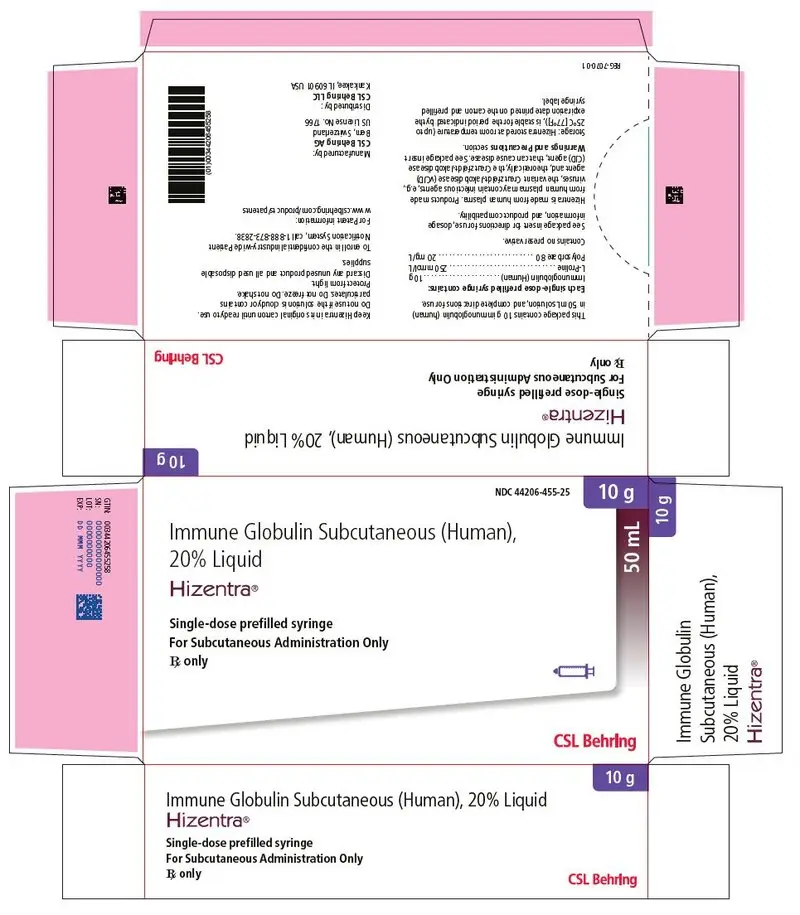
Dosage Forms and Strengths
0.2 g per mL (20%) protein solution for subcutaneous infusion available in a single-dose prefilled syringe (5 mL, 10 mL, 20 mL, and 50 mL) or tamper-evident vial (5 mL, 10 mL, 20 mL and 50 mL). (3)
Contraindications
- Anaphylactic or severe systemic reaction to human immune globulin or inactive ingredients of HIZENTRA, such as polysorbate 80. (4)
- Hyperprolinemia Type I or II (HIZENTRA contains stabilizer L-proline). (4)
- IgA-deficient patients with antibodies against IgA and a history of hypersensitivity. (4)
Warnings and Precautions
- IgA-deficient patients with anti-IgA antibodies are at greater risk of severe hypersensitivity and anaphylactic reactions. (5.1)
- Thrombosis may occur following treatment with immune globulin products, including HIZENTRA. (5.2)
- Aseptic meningitis syndrome has been reported with IGIV or IGSC, including HIZENTRA treatment. (5.3)
- Monitor renal function, including blood urea nitrogen, serum creatinine, and urine output in patients at risk of acute renal failure. (5.4)
- Monitor for clinical signs and symptoms of hemolysis. (5.5)
- Monitor for pulmonary adverse reactions (transfusion-related acute lung injury [TRALI]). (5.6)
- HIZENTRA is made from human blood and may contain infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent. (5.7)
Adverse Reactions/Side Effects
The most common adverse reactions observed in ≥5% of study subjects were local infusion site reactions, headache, diarrhea, fatigue, back pain, nausea, pain in extremity, cough, upper respiratory tract infection, rash, pruritus, vomiting, abdominal pain (upper), migraine, arthralgia, pain, fall and nasopharyngitis. (6)
To report SUSPECTED ADVERSE REACTIONS, contact CSL Behring Pharmacovigilance at 1-866-915-6958 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
The passive transfer of antibodies may interfere with the response to live virus vaccines (7.1), and lead to misinterpretation of the results of serological testing. (5.8, 7.2)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 4/2023
Full Prescribing Information
WARNING: THROMBOSIS
- Thrombosis may occur with immune globulin products1-3, including HIZENTRA. Risk factors may include: advanced age, prolonged immobilization, hypercoagulable conditions, history of venous or arterial thrombosis, use of estrogens, indwelling central vascular catheters, hyperviscosity, and cardiovascular risk factors. Thrombosis may occur in the absence of known risk factors [see Warnings and Precautions (5.2), and Patient Counseling Information (17).
- For patients at risk of thrombosis, administer HIZENTRA at the minimum dose and infusion rate practicable. Ensure adequate hydration in patients before administration. Monitor for signs and symptoms of thrombosis and assess blood viscosity in patients at risk for hyperviscosity [see Warnings and Precautions (5.2)].
1. Indications and Usage for Hizentra
HIZENTRA is an Immune Globulin Subcutaneous (Human) (IGSC), 20% Liquid indicated for the treatment of the following conditions:
1.1 Primary Immunodeficiency (PI)
HIZENTRA is indicated as replacement therapy for primary humoral immunodeficiency (PI) in adults and pediatric patients 2 years of age and older. This includes, but is not limited to, the humoral immune defect in congenital agammaglobulinemia, common variable immunodeficiency, X-linked agammaglobulinemia, Wiskott-Aldrich syndrome, and severe combined immunodeficiencies.
2. Hizentra Dosage and Administration
For subcutaneous infusion only.
2.1 Preparation and Handling
HIZENTRA is a clear and pale yellow to light brown solution. Do not use if the solution is cloudy or contains particulates.
- Prior to administration, visually inspect each prefilled syringe or vial of HIZENTRA for particulate matter or discoloration, whenever the solution and container permit.
- Do not freeze. Do not use any solution that has been frozen.
- Check the product expiration date on the prefilled syringe or vial label. Do not use beyond the expiration date.
- Do not mix HIZENTRA with other products.
- Do not shake the prefilled syringe or vial.
- Use aseptic technique when preparing and administering this product.
- Both the HIZENTRA prefilled syringe and vial are single-dose containers. Multiple HIZENTRA prefilled syringes or vials can be administered to achieve the prescribed dose. Discard all used administration supplies and any unused product immediately after each infusion in accordance with local requirements.
2.2 Dose
Primary Immunodeficiency (PI)
- HIZENTRA can be administered at regular intervals from daily up to every 2 weeks (biweekly).
- Individualize the dose based on the patient's clinical response to HIZENTRA therapy and serum immunoglobulin G (IgG) trough levels.
- Before receiving treatment with HIZENTRA:
- Ensure that patients have received Immune Globulin Intravenous (Human) (IGIV) treatment at regular intervals for at least 3 months.
- Obtain the patient's serum IgG trough level to guide subsequent dose adjustments (see below, under Dose Adjustment).
Dose Adjustment
The dose may need to be adjusted to achieve the desired clinical response and serum IgG trough level, irrespective of the frequency of administration.
To determine if a dose adjustment should be considered, measure the patient's serum IgG trough level 2 to 3 months after switching to HIZENTRA.
2.3 Administration
HIZENTRA is for subcutaneous infusion only.
HIZENTRA is intended for subcutaneous administration using an infusion pump. Infuse HIZENTRA in the abdomen, thigh, upper arm, and/or lateral hip.
- Infusion sites – A HIZENTRA dose may be infused into multiple infusion sites. Use up to 8 infusion sites in parallel. More than one infusion device can be used simultaneously. Infusion sites should be at least 2 inches apart. Change the actual site of infusion with each administration.
- Volume (as tolerated) – For the first infusion of HIZENTRA, do not exceed a volume of 15 mL per infusion site in patients with PI or up to 20 mL per infusion site in patients with CIDP. For subsequent infusions, the volume may be increased to 25 mL per infusion site for patients with PI or to 50 mL per site for patients with CIDP.
- Rate (as tolerated) – For the first infusion of HIZENTRA, the recommended flow rate is up to 15 mL per hour per infusion site in patients with PI or up to 20 mL per hour per site in patients with CIDP. For subsequent infusions, the flow rate may be increased to 25 mL per hour per site in patients with PI or up to 50 mL per hour per site in patients with CIDP.
Follow the steps below and use aseptic technique to administer HIZENTRA, either as prefilled syringe(s) or vial(s).
- 1.
- Assemble supplies Gather the HIZENTRA prefilled syringe(s) or vial(s), all supplies, and infusion log book.
- 2.
- Clean surface Clean a table or other flat surface.
- 3.
-
Wash hands – Thoroughly wash and dry hands (Figure 1).

Figure 1
- 4.
-
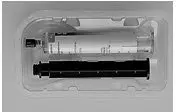
Check prefilled syringe(s) or vial(s):
-
If using prefilled syringes, carefully peel back the transparent covering from the tray and inspect the protective cap. Peel back the outer layer of the wrap-around label to allow for viewing of HIZENTRA through the fully transparent inner layer, but don't remove the label completely (Figure 2).

Figure 2
- If using vials, inspect the protective cap of the vials (Figure 3).

Figure 3
-
If using prefilled syringes, carefully peel back the transparent covering from the tray and inspect the protective cap. Peel back the outer layer of the wrap-around label to allow for viewing of HIZENTRA through the fully transparent inner layer, but don't remove the label completely (Figure 2).
Carefully inspect each prefilled syringe(s) or vial(s) of HIZENTRA. HIZENTRA is a clear and pale yellow to light brown solution. Do not use the prefilled syringe or vial if damaged, the liquid looks cloudy, contains particles, has changed color, the protective cap of the prefilled syringe or the vial is missing or defective, or the expiration date on the label has passed.
- 5.
-
Prepare HIZENTRA for infusion
If using HIZENTRA prefilled syringes, go to Step 5.1
If using HIZENTRA vials, go to Step 5.2 - 5.1
-
HIZENTRA prefilled syringe(s)
- The 5 mL, 10 mL, 20 mL, and 50 mL prefilled syringes are supplied and ready to use. The 5 mL and 10 mL prefilled syringes are fully assembled (Figure 4). For the 20 mL and 50 mL prefilled syringes, screw the plunger rod onto the prefilled syringe stopper prior to use (Figure 5).
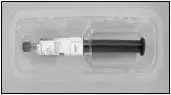
Figure 4
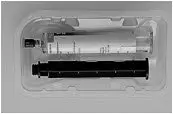
Figure 5
- HIZENTRA prefilled syringes can be placed directly in the infusion pump if the prefilled syringe size matches the pump requirements. If the prefilled syringe can be placed directly in the infusion pump, then go to Step 6.
NOTE:
An additional adapter may be required for the HIZENTRA prefilled syringes to fit properly in the infusion pump. Check with the provider of your supplies for the appropriate adapter and installation instructions. - If the HIZENTRA prefilled syringe size does not match the infusion pump requirements, transfer the contents of the prefilled syringe to another syringe of a size specific for the infusion pump by following the directions below:
- Use a syringe-to-syringe transfer device (tip-to-tip connector) (Figure 6) to transfer the contents of the prefilled syringe to the empty syringe specific for the infusion pump.
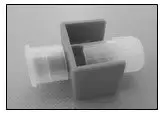
Figure 6
- Remove the protective cap from the prefilled syringe. Attach the transfer device (tip-to-tip connector) by twisting it onto the prefilled syringe. Attach the empty syringe by screwing it onto the other side of the transfer device (Figure 7).

Figure 7
- Make sure you transfer the amount needed to achieve the prescribed dose.
- Measure dose from the top of the stopper
- Push the plunger of the prefilled syringe (e.g., using your fingers, thumb or the palm of your hand) to transfer HIZENTRA from the prefilled syringe to the empty syringe.
- Repeat this step if multiple prefilled syringes are necessary to achieve the prescribed dose. Remove the emptied prefilled syringe and attach another prefilled syringe to the transfer device (tip-to-tip connector).
- After the transfer is complete, remove the emptied prefilled syringe and the transfer device (tip-to-tip connector) by unscrewing them from the syringe specific for your pump. Connect the filled syringe to the infusion tubing.
- Use a syringe-to-syringe transfer device (tip-to-tip connector) (Figure 6) to transfer the contents of the prefilled syringe to the empty syringe specific for the infusion pump.
- The 5 mL, 10 mL, 20 mL, and 50 mL prefilled syringes are supplied and ready to use. The 5 mL and 10 mL prefilled syringes are fully assembled (Figure 4). For the 20 mL and 50 mL prefilled syringes, screw the plunger rod onto the prefilled syringe stopper prior to use (Figure 5).
Go to Step 6.
- 5.2
-
Transfer HIZENTRA from vial to syringe
- Take the protective cap off the vial (Figure 8).

Figure 8
- Clean the vial stopper with an alcohol wipe (Figure 9). Let the stopper dry.

Figure 9
- If using a transfer device, follow the instructions provided by the device manufacturer.
- If using a needle and a syringe to transfer HIZENTRA, follow the instructions below:
- Attach a sterile transfer needle to a sterile syringe (Figure 10).

Figure 10
- Pull out the plunger of the syringe to fill the syringe with air. Make sure that the amount of air is the same as the amount of HIZENTRA you will transfer from the vial.
- Put the HIZENTRA vial on a flat surface. Keeping the vial upright, insert the transfer needle into the center of the rubber stopper.
- Check that the tip of the needle is not in the liquid. Then, push the plunger of the syringe down. This will inject the air from the syringe into the airspace of the vial.
- Leaving the needle in the stopper, carefully turn the vial upside down (Figure 11).

Figure 11
- Slowly pull back on the plunger of the syringe to fill the syringe with HIZENTRA.
- Take the filled syringe and needle out of the stopper.
- Take off the needle and throw it away in the sharps container.
- Attach a sterile transfer needle to a sterile syringe (Figure 10).
- Take the protective cap off the vial (Figure 8).
When using multiple vials to achieve the prescribed dose, repeat this step.
- 6.
-
Prepare infusion pump and tubing
- Prior to preparing the pump(s), make sure you have the prescribed dose in the syringe(s) and the infusion tubing is attached.
- Prepare the infusion pump following the manufacturer's instructions, including attaching any necessary adapters.
- Do not remove the needle caps until you are ready to infuse.
- Prime (fill) the infusion. To prime the tubing, connect the syringe filled with HIZENTRA to the infusion tubing and gently push on the syringe plunger (e.g., using your fingers or thumb or the palm of your hand) to fill the tubing with HIZENTRA (Figure 12).

Figure 12
- Stop priming before HIZENTRA fluid reaches the capped needle.
- Insert the syringe filled with HIZENTRA into the infusion pump.
- Prime (fill) the infusion. To prime the tubing, connect the syringe filled with HIZENTRA to the infusion tubing and gently push on the syringe plunger (e.g., using your fingers or thumb or the palm of your hand) to fill the tubing with HIZENTRA (Figure 12).
- 7.
-
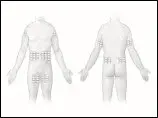
Prepare infusion site(s)
- Select an area on your abdomen, thigh, upper arm, or side of upper leg/hip for the infusion (Figure 13).The number and location of infusion sites depends on the volume of the total dose.

Figure 13
- Never infuse into areas where the skin is tender, bruised, red, or hard. Avoid infusing into scars or stretch marks.
- Infuse HIZENTRA into a maximum of 8 sites simultaneously; or up to 12 consecutively per infusion. Infusion sites should be at least 2 inches apart.
- Clean the skin at each infusion site with an antiseptic skin prep (Figure 14). Let the skin dry.

Figure 14
- Select an area on your abdomen, thigh, upper arm, or side of upper leg/hip for the infusion (Figure 13).The number and location of infusion sites depends on the volume of the total dose.
- 8.
-
Insert needle(s)
- Use just one needle per site. If injecting in more than one site, the following steps should be completed for each needle, one at a time:
- Remove the needle cap.
- Using 2 fingers, pinch together the skin around the infusion site. With a quick dart-like motion, insert the needle straight into the skin (Figure 15).

Figure 15
- Put sterile gauze and tape or a transparent dressing over the infusion site (Figure 16) to hold the needle in place.

Figure 16
- 9.
-
Start infusion
- Follow the manufacturer's instructions to turn on the infusion pump and start the infusion (Figure 17).

Figure 17
- Follow the manufacturer's instructions to turn on the infusion pump and start the infusion (Figure 17).
- 10.
-
Complete infusion and record treatment (Figure 18)
- When all the HIZENTRA has been infused, turn off the infusion pump.
- Remove the needle(s) from the skin.
- Once you have removed the needle(s), remove the empty syringe from the infusion pump.
- Disconnect the infusion set from the empty syringe.
- Cover the infusion site(s) with a protective dressing.
- Peel-off the removable part of the label for each prefilled syringe or vial used Affix it to the patient's log book with the date and time of infusion, or scan the prefilled syringe or vial if recording the infusion electronically.
Figure 18
- 11.
-
Clean up
- If applicable, remove adapter from the infusion pump following the manufacturer's instructions.
- Throw away the empty HIZENTRA prefilled syringe(s) or vial(s), along with the used disposable supplies in the sharps container (Figure 19) in accordance with local requirements.
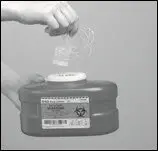
Figure 19
- Clean and store the infusion pump, following the manufacturer's instructions.
For self-administration, provide the patient with instructions and training for subcutaneous infusion in the home or other appropriate setting.
3. Dosage Forms and Strengths
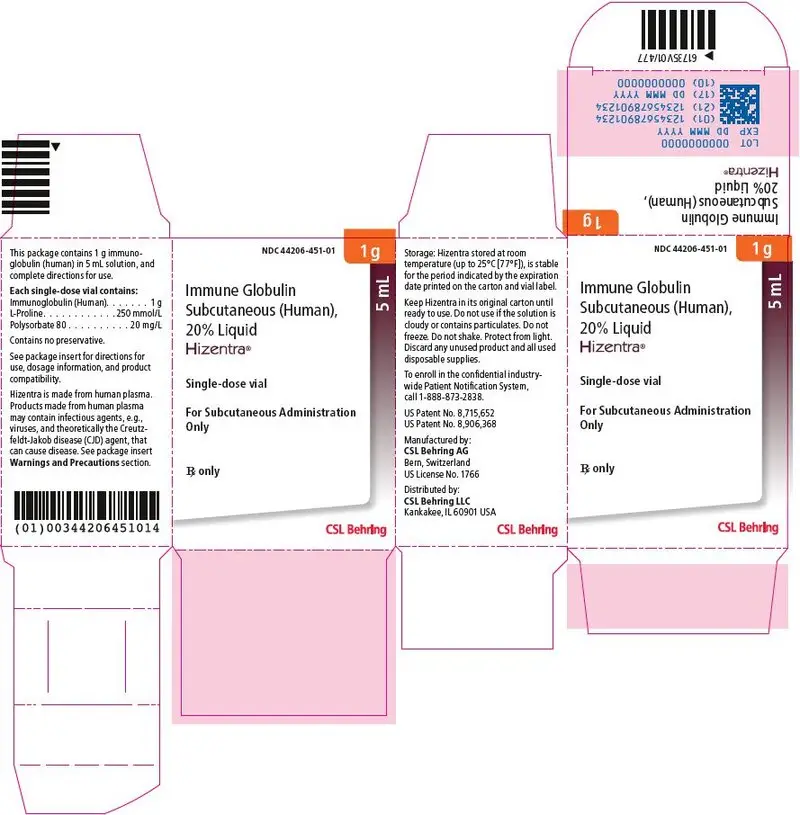
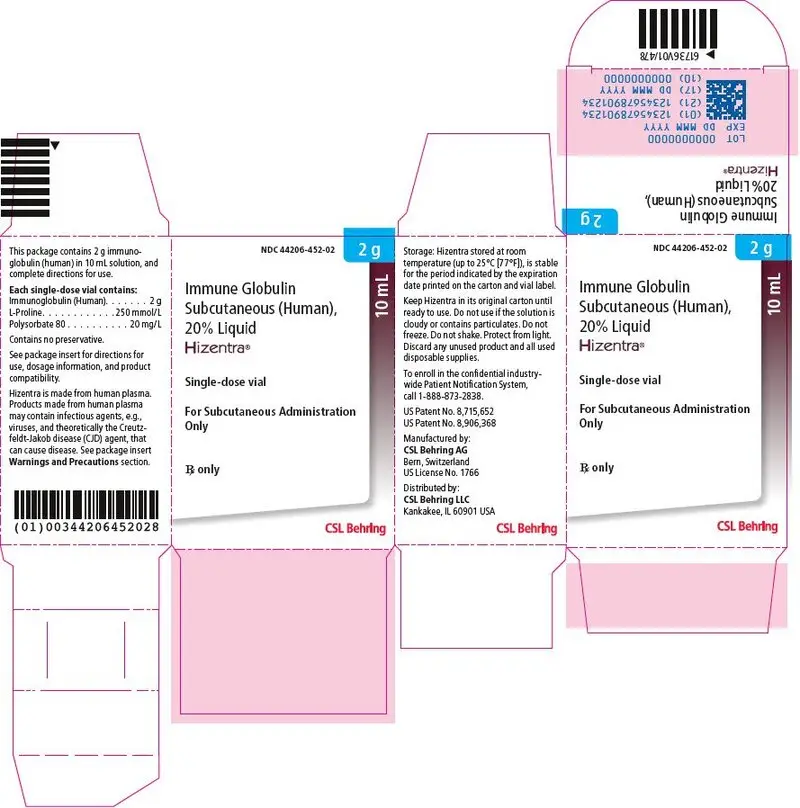
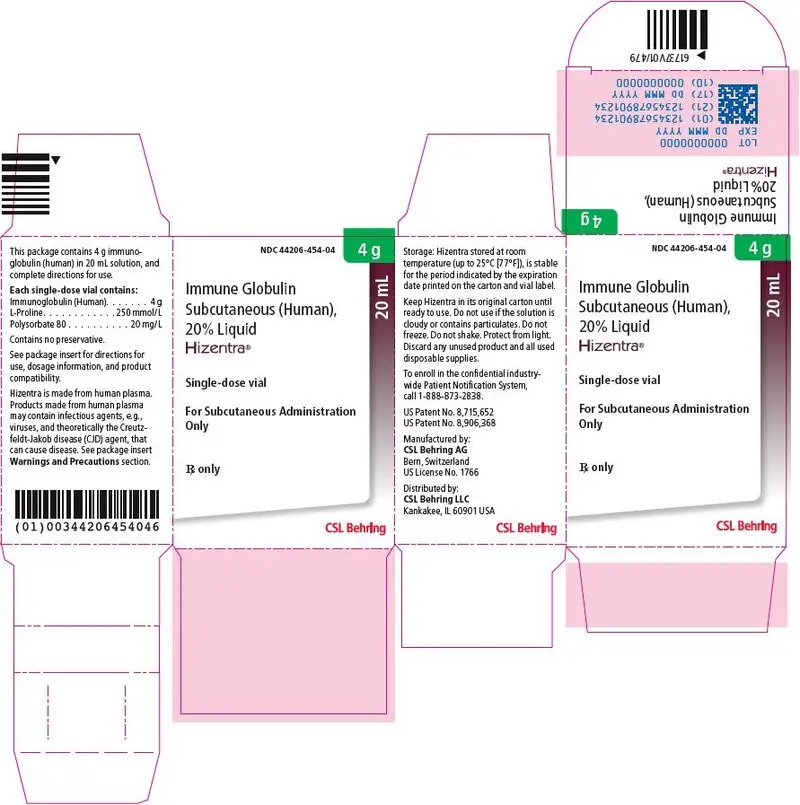
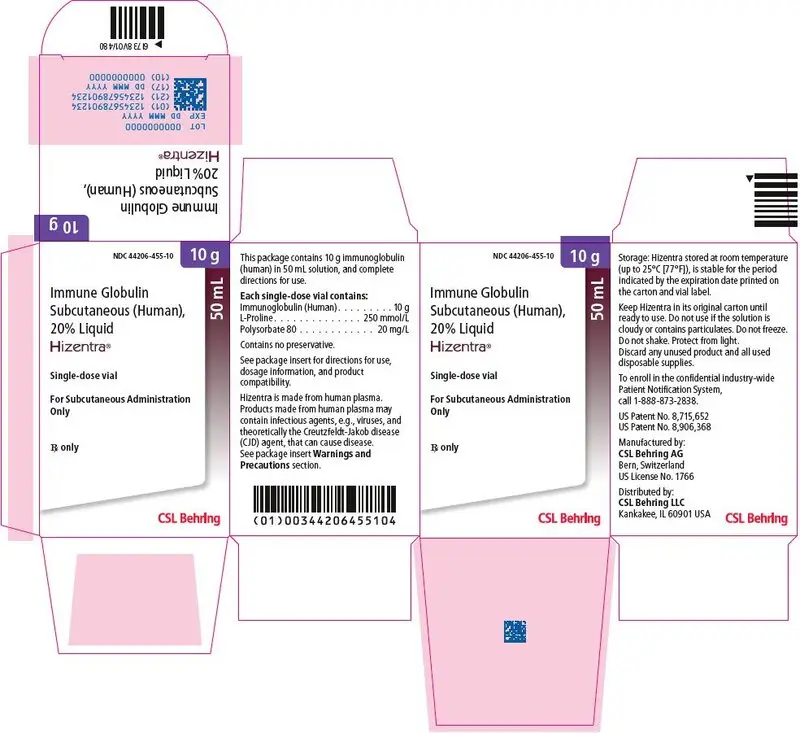
HIZENTRA is a 0.2 g/mL (20%) protein solution for subcutaneous infusion available in a single-dose, prefilled syringe (5 mL, 10 mL, 20 mL, and 50 mL) or tamper-evident vial (5 mL, 10 mL, 20 mL and 50 mL).
4. Contraindications
HIZENTRA is contraindicated in patients with:
- History of anaphylactic or severe systemic reaction to human immune globulin or inactive ingredients of HIZENTRA, such as polysorbate 80.
- Hyperprolinemia Type I or II because it contains L-proline as a stabilizer [see Description (11)].
- IgA-deficiency with antibodies against IgA and a history of hypersensitivity [see Description (11)].
5. Warnings and Precautions
5.1 Hypersensitivity
Severe hypersensitivity reactions may occur to human immune globulin or components of HIZENTRA, such as polysorbate 80. If a hypersensitivity reaction occurs, discontinue the HIZENTRA infusion immediately and institute appropriate treatment.
Individuals with IgA deficiency can develop anti-IgA antibodies and anaphylactic reactions (including anaphylaxis and shock) after administration of blood components containing IgA. Patients with known antibodies to IgA may have a greater risk of developing potentially severe hypersensitivity and anaphylactic reactions with administration of HIZENTRA. HIZENTRA contains ≤50 mcg/mL IgA [see Description (11)].
5.2 Thrombosis
Thrombosis may occur following treatment with immune globulin products1-3, including HIZENTRA. Risk factors may include: advanced age, prolonged immobilization, hypercoagulable conditions, history of venous or arterial thrombosis, use of estrogens, indwelling central vascular catheters, hyperviscosity, and cardiovascular risk factors. Thrombosis may occur in the absence of known risk factors.
Consider baseline assessment of blood viscosity in patients at risk for hyperviscosity, including those with cryoglobulins, fasting chylomicronemia/markedly high triglycerides, or monoclonal gammopathies. For patients at risk of thrombosis, administer HIZENTRA at the minimum dose and infusion rate practicable. Ensure adequate hydration in patients before administration. Monitor for signs and symptoms of thrombosis and assess blood viscosity in patients at risk for hyperviscosity [see Boxed Warning, Dosage and Administration (2) and Patient Counseling Information (17)].
5.3 Aseptic Meningitis Syndrome (AMS)
AMS has been reported with use of IGIV4 or IGSC, including HIZENTRA. The syndrome usually begins within several hours to 2 days following immune globulin treatment. AMS is characterized by the following signs and symptoms: severe headache, nuchal rigidity, drowsiness, fever, photophobia, painful eye movements, nausea, and vomiting. Cerebrospinal fluid (CSF) studies frequently show pleocytosis up to several thousand cells per cubic millimeter, predominantly from the granulocytic series, and elevated protein levels up to several hundred mg/dL. AMS may occur more frequently in association with high doses (≥2 g/kg) and/or rapid infusion of immune globulin product.
Patients exhibiting such signs and symptoms should receive a thorough neurological examination, including CSF studies, to rule out other causes of meningitis. Discontinuation of immune globulin treatment has resulted in remission of AMS within several days without sequelae.
5.4 Renal Dysfunction/Failure
Acute renal dysfunction/failure, acute tubular necrosis, proximal tubular nephropathy, osmotic nephrosis and death may occur with use of human immune globulin products, especially those containing sucrose.5 HIZENTRA does not contain sucrose. Ensure that patients are not volume depleted before administering HIZENTRA.
For patients judged to be at risk for developing renal dysfunction, including patients with any degree of pre-existing renal insufficiency, diabetes mellitus, age greater than 65, volume depletion, sepsis, paraproteinemia, or patients receiving known nephrotoxic drugs, monitor renal function and consider lower, more frequent dosing [see Dosage and Administration (2)].
Periodic monitoring of renal function and urine output is particularly important in patients judged to have a potential increased risk of developing acute renal failure.6 Assess renal function, including measurement of blood urea nitrogen (BUN) and serum creatinine, before the initial infusion of HIZENTRA and at appropriate intervals thereafter. If renal function deteriorates, consider discontinuing HIZENTRA.
5.5 Hemolysis
HIZENTRA can contain blood group antibodies that may act as hemolysins and induce in vivo coating of red blood cells (RBCs) with immunoglobulin, causing a positive direct antiglobulin (Coombs') test result and hemolysis.7,9 Delayed hemolytic anemia can develop subsequent to immune globulin therapy due to enhanced RBC sequestration, and acute hemolysis, consistent with intravascular hemolysis, has been reported.10
Monitor recipients of HIZENTRA for clinical signs and symptoms of hemolysis. If signs and/or symptoms of hemolysis are present after HIZENTRA infusion, perform appropriate confirmatory laboratory testing.
5.6 Transfusion-Related Acute Lung Injury (TRALI)
Noncardiogenic pulmonary edema may occur in patients administered human immune globulin products.11 TRALI is characterized by severe respiratory distress, pulmonary edema, hypoxemia, normal left ventricular function, and fever. Typically, it occurs within 1 to 6 hours following transfusion. Patients with TRALI may be managed using oxygen therapy with adequate ventilatory support.
Monitor HIZENTRA recipients for pulmonary adverse reactions. If TRALI is suspected, perform appropriate tests for the presence of anti-neutrophil antibodies in both the product and patient's serum.
5.7 Transmissible Infectious Agents
Because HIZENTRA is made from human blood, it may carry a risk of transmitting infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent. This also applies to unknown or emerging viruses and other pathogens. No cases of transmission of viral diseases or CJD have been associated with the use of HIZENTRA. All infections suspected by a physician possibly to have been transmitted by HIZENTRA should be reported to CSL Behring Pharmacovigilance at 1-866-915-6958.
6. Adverse Reactions/Side Effects
The most common adverse reactions (ARs) observed in ≥5% of study subjects receiving HIZENTRA were local reactions (e.g., swelling, redness, heat, pain, hematoma and itching at the infusion site), headache, diarrhea, fatigue, back pain, nausea, pain in extremity, cough, upper respiratory tract infection, rash, pruritus, vomiting, abdominal pain (upper), migraine, arthralgia, pain, fall and nasopharyngitis.
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, AR rates observed in clinical studies of a product cannot be directly compared to rates in the clinical studies of another product and may not reflect the rates observed in clinical practice.
7. Drug Interactions
8. Use In Specific Populations
11. Hizentra Description
HIZENTRA, Immune Globulin Subcutaneous (Human), 20% Liquid, is a ready-to-use, sterile 20% (0.2 g/mL) protein liquid preparation of polyvalent human immunoglobulin G (IgG) for subcutaneous administration. HIZENTRA is manufactured from large pools of human plasma by a combination of cold alcohol fractionation, octanoic acid fractionation, and anion exchange chromatography. The IgG proteins are not subjected to heating or to chemical or enzymatic modification. The Fc and Fab functions of the IgG molecule are retained. Fab functions tested include antigen binding capacities, and Fc functions tested include complement activation and Fc-receptor-mediated leukocyte activation (determined with complexed IgG). The IgG subclass distribution is similar to that of normal human plasma.
HIZENTRA has a purity of ≥98% IgG and a pH of 4.6 to 5.2. This product contains approximately 250 mmol/L (range: 210 to 290 mmol/L) L-proline (a nonessential amino acid) as a stabilizer, 8 to 30 mg/L polysorbate 80, and trace amounts of sodium. HIZENTRA contains ≤50 mcg/mL IgA, no carbohydrate stabilizers (e.g., sucrose, maltose) and no preservative.
Plasma units used in the manufacture of HIZENTRA are tested using FDA-licensed serological assays for hepatitis B surface antigen and antibodies to human immunodeficiency virus (HIV)-1/2 and hepatitis C virus (HCV) as well as FDA-licensed Nucleic Acid Testing (NAT) for HBV, HCV and HIV-1. All plasma units have been found to be nonreactive (negative) in these tests. In addition, the plasma has been tested for B19 virus (B19V) DNA by NAT. Only plasma that passes virus screening is used for production, and the limit for B19V in the fractionation pool is set not to exceed 104 IU of B19V DNA per mL.
The manufacturing process for HIZENTRA includes three steps to reduce the risk of virus transmission. Two of these are dedicated virus clearance steps: pH 4 incubation to inactivate enveloped viruses, and virus filtration to remove, by size exclusion, both enveloped and non-enveloped viruses as small as approximately 20 nanometers. In addition, a depth filtration step contributes to the virus reduction capacity.12
These steps have been independently validated in a series of in vitro experiments for their capacity to inactivate and/or remove both enveloped and non-enveloped viruses. Table 6 shows the virus clearance during the manufacturing process for HIZENTRA, expressed as the mean log10 reduction factor (LRF).
| HIV-1 | PRV | BVDV | WNV | EMCV | MVM | |
|---|---|---|---|---|---|---|
| HIV-1, human immunodeficiency virus type 1, a model for HIV-1 and HIV-2; PRV, pseudorabies virus, a nonspecific model for large enveloped DNA viruses (e.g., herpes virus); BVDV, bovine viral diarrhea virus, a model for hepatitis C virus; WNV, West Nile virus; EMCV, encephalomyocarditis virus, a model for hepatitis A virus; MVM, minute virus of mice, a model for a small highly resistant non-enveloped DNA virus (e.g., parvovirus); LRF, log10 reduction factor; nt, not tested; na, not applicable. | ||||||
|
||||||
| Virus Property | ||||||
| Genome | RNA | DNA | RNA | RNA | RNA | DNA |
| Envelope | Yes | Yes | Yes | Yes | No | No |
| Size (nm) | 80-100 | 120-200 | 50-70 | 50-70 | 25-30 | 18-24 |
| Manufacturing Step | Mean LRF | |||||
| pH 4 incubation | ≥5.6 | ≥6.1 | 4.6 | ≥7.8 | nt | nt |
| Depth filtration | ≥6.7 | ≥5.7 | 3.5±0.2 | 3.0±0.4 | 5.7±0.2 | 3.7±0.3 |
| Virus filtration | ≥4.7 | ≥5.8 | ≥4.6 | ≥6.8 | ≥6.3 | ≥6.5 |
| Overall Reduction (Log10 Units) | ≥17.0 | ≥17.6 | ≥12.7 | ≥17.6 | ≥12.0 | ≥10.2 |
12. Hizentra - Clinical Pharmacology
12.1 Mechanism of Action
HIZENTRA supplies a broad spectrum of opsonizing and neutralizing IgG antibodies against a wide variety of bacterial and viral agents. The mechanism of action has not been fully elucidated, but may include immunomodulatory effects.
12.3 Pharmacokinetics
Treatment of Primary Immunodeficiency
Pharmacokinetic Modeling and Simulation
Prediction of Trough Levels Following Regimen Changes
PK modeling and simulation also predicted changes in trough levels after switching from (a) monthly IGIV to weekly or biweekly HIZENTRA dosing, (b) weekly to biweekly HIZENTRA dosing, or (c) weekly to more frequent dosing. Table 9 (last column) shows the predicted changes in steady-state IgG trough levels after switching between the various dosing regimens.
| IgG Dosing Regimen Switch | AUC | Cmax | Cmin | Predicted Change in Trough† | |
|---|---|---|---|---|---|
| From: | To: | ||||
| AUC, area under the curve, calculated as AUC0-28days for the IGIV to HIZENTRA switches, AUC0-14days for the weekly to biweekly HIZENTRA switch, and AUC0-7days for weekly to more frequent HIZENTRA switches; Cmax, maximum IgG concentration; Cmin, minimum IgG concentration during a 28-day period (for the IGIV to HIZENTRA switches), a 14-day period (for the weekly to biweekly HIZENTRA switch), or a 7-day period (for the weekly to more frequent HIZENTRA switches). | |||||
|
|||||
| IGIV | Weekly HIZENTRA‡ | 0.97 (0.90, 1.04) | 0.68 (0.60, 0.76) | 1.16 (1.07, 1.26) | 16% increase |
| IGIV | Biweekly HIZENTRA§ | 0.97 (0.91, 1.04) | 0.71 (0.63, 0.78) | 1.10 (1.02, 1.18) | 10% increase |
| Weekly HIZENTRA | Biweekly HIZENTRA§ | 1.00 (0.98, 1.03) | 1.06 (1.02, 1.09) | 0.95 (0.92, 0.98) | 5% decrease |
| Weekly HIZENTRA | 2 times per week HIZENTRA | 1.01 (0.98, 1.03) | 0.99 (0.96, 1.02) | 1.03 (1.00, 1.06) | 3% increase |
| Weekly HIZENTRA | 3 times per week HIZENTRA | 1.01 (0.98, 1.03) | 0.99 (0.96, 1.02) | 1.04 (1.01, 1.07) | 4% increase |
| Weekly HIZENTRA | 5 times per week HIZENTRA (daily for 5 days) | 1.01 (0.98, 1.03) | 0.99 (0.97, 1.01) | 1.04 (1.01, 1.06) | 4% increase |
| Weekly HIZENTRA | Daily HIZENTRA (7 times per week) | 1.00 (0.98, 1.03) | 0.98 (0.95, 1.01) | 1.04 (1.02, 1.08) | 4% increase |
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No animal studies were conducted to evaluate the carcinogenic or mutagenic effects of HIZENTRA or its effects on fertility.
13.2 Animal Toxicology and/or Pharmacology
Long- and short-term memory loss was seen in juvenile rats in a study modeling hyperprolinemia. In this study, rats received daily subcutaneous injections with L-proline from day 6 to day 28 of life.15 The daily amounts of L-proline used in this study were more than 60 times higher than the L-proline dose that would result from the administration of 400 mg/kg body weight of HIZENTRA once weekly. In unpublished studies using the same animal model (i.e., rats) dosed with the same amount of L-proline with a dosing interval relevant to IGSC treatment (i.e., on 5 consecutive days on days 9 to 13, or once weekly on days 9, 16, and 23), no effects on learning and memory were observed. The clinical relevance of these studies is not known.
14. Clinical Studies
15. References
- Dalakas MC. High-dose intravenous immunoglobulin and serum viscosity: risk of precipitating thromboembolic events. Neurology 1994;44:223-226.
- Woodruff RK, Grigg AP, Firkin FC, Smith IL. Fatal thrombotic events during treatment of autoimmune thrombocytopenia with intravenous immunoglobulin in elderly patients. Lancet 1986;2:217-218.
- Wolberg AS, Kon RH, Monroe DM, Hoffman M. Coagulation factor XI is a contaminant in intravenous immunoglobulin preparations. Am J Hematol 2000;65:30-34.
- Gabor EP, Meningitis and skin reaction after intravenous immune globulin therapy. Ann Intern Med 1997:127:1130.
- Pierce LR, Jain N. Risks associated with the use of intravenous immunoglobulin. Trans Med Rev 2003;17:241-251.
- Cayco AV, Perazella MA, Hayslett JP. Renal insufficiency after intravenous immune globulin therapy: a report of two cases and an analysis of the literature. J Am Soc Nephrol 1997;8:1788-1793.
- Copelan EA, Strohm PL, Kennedy MS, Tutschka PJ. Hemolysis following intravenous immune globulin therapy. Transfusion 1986;26:410-412.
- Thomas MJ, Misbah SA, Chapel HM, Jones M, Elrington G, Newsom-Davis J. Hemolysis after high-dose intravenous Ig. Blood 1993;15:3789.
- Wilson JR, Bhoopalam N, Fisher M. Hemolytic anemia associated with intravenous immunoglobulin. Muscle Nerve 1997;20:1142-1145.
- Kessary-Shoham H, Levy Y, Shoenfeld Y, Lorber M, Gershon H. In vivo administration of intravenous immunoglobulin (IVIg) can lead to enhanced erythrocyte sequestration. J Autoimmun 1999;13:129-135.
- Rizk A, Gorson KC, Kenney L, Weinstein R. Transfusion-related acute lung injury after the infusion of IVIG. Transfusion 2001;41:264-268.
- Stucki M, Boschetti N, Schäfer W, et al. Investigations of prion and virus safety of a new liquid IVIG product. Biologicals 2008;36:239-247.
- Smith GN, Griffiths B, Mollison D, Mollison PL. Uptake of IgG after intramuscular and subcutaneous injection. Lancet 1972;1:1208-1212.
- Waniewski I, Gardulf A, Hammarström L. Bioavailability of γ-globulin after subcutaneous infusions in patients with common variable immunodeficiency. J Clin Immunol 1994;14:90-97.
- Bavaresco CS, Streck EL, Netto CA, et al. Chronic hyperprolinemia provokes a memory deficit in the Morris Water Maze Task. Metabolic Brain Disease 2005;20:73-80.
16. How is Hizentra supplied
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Information for Patients and Instructions for Use).
Inform patients to immediately report the following signs and symptoms to their healthcare provider:
- Hypersensitivity reactions to HIZENTRA (including hives, generalized urticaria, tightness of the chest, wheezing, hypotension, and anaphylaxis) [see Warnings and Precautions (5.1)].
- Pain and/or swelling of an arm or leg with warmth over the affected area, discoloration of an arm or leg, unexplained shortness of breath, chest pain or discomfort that worsens on deep breathing, unexplained rapid pulse, or numbness or weakness on one side of the body [see Warnings and Precautions (5.2)].
- Severe headache, neck stiffness, drowsiness, fever, sensitivity to light, painful eye movements, nausea, and vomiting [see Warnings and Precautions (5.3)].
- Decreased urine output, sudden weight gain, fluid retention/edema, and/or shortness of breath [see Warnings and Precautions (5.4)].
- Fatigue, increased heart rate, yellowing of the skin or eyes, and dark-colored urine [see Warnings and Precautions (5.5)].
- Severe breathing problems, lightheadedness, drops in blood pressure, and fever [see Warnings and Precautions (5.6)].
Inform patients that because HIZENTRA is made from human blood, it may carry a risk of transmitting infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) agent and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent [see Warnings and Precautions (5.7) and Description (11)].
Inform patients that HIZENTRA may interfere with the response to live virus vaccines (e.g., measles, mumps, rubella, and varicella) and to notify their immunizing physician of recent therapy with HIZENTRA [see Drug Interactions (7)].
| HIZENTRA
human immunoglobulin g liquid |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| HIZENTRA
human immunoglobulin g liquid |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| HIZENTRA
human immunoglobulin g liquid |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| HIZENTRA
human immunoglobulin g liquid |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| HIZENTRA
human immunoglobulin g liquid |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| HIZENTRA
human immunoglobulin g liquid |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| HIZENTRA
human immunoglobulin g liquid |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - CSL Behring AG (481152762) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| CSL Behring AG | 481152762 | MANUFACTURE | |