Drug Detail:Infliximab, infliximab-dyyb (monograph) (Inflectra)
Drug Class:
Highlights of Prescribing Information
INFLIXIMAB for injection, for intravenous use
Initial U.S. Approval: 1998
WARNING: SERIOUS INFECTIONS and MALIGNANCY
See full prescribing information for complete boxed warning.
- Increased risk of serious infections leading to hospitalization or death, including tuberculosis (TB), bacterial sepsis, invasive fungal infections (such as histoplasmosis) and infections due to other opportunistic pathogens. (5.1)
- Discontinue Infliximab if a patient develops a serious infection.
- Perform test for latent TB; if positive, start treatment for TB prior to starting Infliximab. Monitor all patients for active TB during treatment, even if initial latent TB test is negative. (5.1)
- Lymphoma and other malignancies, some fatal, have been reported in children and adolescent patients treated with tumor necrosis factor (TNF) blockers, including Infliximab. (5.2)
- Postmarketing cases of fatal hepatosplenic T-cell lymphoma (HSTCL) have been reported in patients treated with TNF blockers including Infliximab. Almost all had received azathioprine or 6-mercaptopurine concomitantly with a TNF blocker at or prior to diagnosis. The majority of Infliximab cases were reported in patients with Crohn's disease or ulcerative colitis, most of whom were adolescent or young adult males. (5.2)
Indications and Usage for Infliximab Injection
Infliximab is a tumor necrosis factor (TNF) blocker indicated for:
-
Crohn's Disease:
- reducing signs and symptoms and inducing and maintaining clinical remission in adult patients with moderately to severely active disease who have had an inadequate response to conventional therapy. (1.1)
- reducing the number of draining enterocutaneous and rectovaginal fistulas and maintaining fistula closure in adult patients with fistulizing disease. (1.1)
- Pediatric Crohn's Disease: reducing signs and symptoms and inducing and maintaining clinical remission in pediatric patients 6 years of age and older with moderately to severely active disease who have had an inadequate response to conventional therapy. (1.2)
- Ulcerative Colitis: reducing signs and symptoms, inducing and maintaining clinical remission and mucosal healing, and eliminating corticosteroid use in adult patients with moderately to severely active disease who have had an inadequate response to conventional therapy. (1.3)
- Pediatric Ulcerative Colitis: reducing signs and symptoms and inducing and maintaining clinical remission in pediatric patients 6 years of age and older with moderately to severely active disease who have had an inadequate response to conventional therapy. (1.4)
- Rheumatoid Arthritis in combination with methotrexate: reducing signs and symptoms, inhibiting the progression of structural damage, and improving physical function in adult patients with moderately to severely active disease. (1.5)
- Ankylosing Spondylitis: reducing signs and symptoms in adult patients with active disease. (1.6)
- Psoriatic Arthritis: reducing signs and symptoms of active arthritis, inhibiting the progression of structural damage, and improving physical function in adult patients. (1.7)
- Plaque Psoriasis: treatment of adult patients with chronic severe (i.e., extensive and/or disabling) plaque psoriasis who are candidates for systemic therapy and when other systemic therapies are medically less appropriate. (1.8)
Infliximab Injection Dosage and Administration
- Prior to treatment, ensure appropriate personnel and medication are available to treat reactions (e.g., hypersensitivity) that occur during infusion and shortly after infusion (2.11)
- Infliximab is administered by intravenous infusion for at least 2 hours with an in-line filter (2.11)
- Crohn's Disease: 5 mg/kg at 0, 2 and 6 weeks, then every 8 weeks. Some adult patients who initially respond to treatment may benefit from increasing the dose to 10 mg/kg every 8 weeks if they later lose their response. (2.1)
- Pediatric Crohn's Disease (≥ 6 years old): 5 mg/kg at 0, 2 and 6 weeks, then every 8 weeks. (2.2)
- Ulcerative Colitis: 5 mg/kg at 0, 2 and 6 weeks, then every 8 weeks. (2.3)
- Pediatric Ulcerative Colitis (≥ 6 years old): 5 mg/kg at 0, 2 and 6 weeks, then every 8 weeks. (2.4)
- Rheumatoid Arthritis: In conjunction with methotrexate, 3 mg/kg at 0, 2 and 6 weeks, then every 8 weeks. Some patients may benefit from increasing the dose up to 10 mg/kg every 8 weeks or treating as often as every 4 weeks. (2.5)
- Ankylosing Spondylitis: 5 mg/kg at 0, 2 and 6 weeks, then every 6 weeks. (2.6)
- Psoriatic Arthritis and Plaque Psoriasis: 5 mg/kg at 0, 2 and 6 weeks, then every 8 weeks. (2.7, 2.8)
Dosage Forms and Strengths
For injection: 100 mg of infliximab as a lyophilized powder in a single-dose vial for reconstitution and dilution. (2.11, 3)
Contraindications
- Infliximab doses >5 mg/kg in moderate or severe heart failure. (4)
- Previous severe hypersensitivity reaction to infliximab or any inactive ingredients of Infliximab or to any murine proteins. (4)
Warnings and Precautions
- Serious infections – do not give Infliximab during an active infection. If an infection develops, monitor carefully and stop Infliximab if infection becomes serious. (5.1)
- Invasive fungal infections – for patients who develop a systemic illness on Infliximab, consider empiric antifungal therapy for those who reside or travel to regions where mycoses are endemic (5.1)
- Malignancies – the incidence of malignancies, including invasive cervical cancer and lymphoma, was greater in Infliximab treated patients than in controls. Due to the risk of HSTCL carefully assess the risk/benefit especially if the patient has Crohn's disease or ulcerative colitis, is male, and is receiving azathioprine or 6-mercaptopurine treatment. (5.2)
- Hepatitis B virus reactivation – test for HBV infection before starting Infliximab. Monitor HBV carriers during and several months after therapy. If reactivation occurs, stop Infliximab and begin anti-viral therapy. (5.3)
- Hepatotoxicity – severe hepatic reactions, some fatal or necessitating liver transplantation. Stop Infliximab in cases of jaundice and/or marked liver enzyme elevations. (5.4)
- Heart failure – new onset or worsening symptoms may occur. (4, 5.5)
- Cytopenias – advise patients to seek immediate medical attention if signs and symptoms develop, and consider stopping Infliximab. (5.6)
- Hypersensitivity – serious infusion reactions including anaphylaxis or serum sickness-like reactions may occur. (5.7)
- Cardiovascular and Cerebrovascular Reactions – Cerebrovascular accidents, myocardial infarctions (some fatal), and arrhythmias have been reported during and within 24 hours of initiation of Infliximab infusion. Monitor patients during Infliximab infusion and if serious reaction occurs, discontinue infusion. (5.8)
- Demyelinating disease – exacerbation or new onset may occur. (5.9)
- Lupus-like syndrome – stop Infliximab if syndrome develops. (5.12)
- Vaccinations and Use of Live Vaccines/Therapeutic Infectious Agents– Prior to initiating Infliximab bring pediatric and adult patients up to date with all vaccinations. Live vaccines or therapeutic infectious agents should not be given with Infliximab. At least a six month waiting period following birth is recommended before the administration of live vaccines to infants exposed in utero to infliximab (5.13).
Adverse Reactions/Side Effects
Most common adverse reactions (>10%) – infections (e.g. upper respiratory, sinusitis, and pharyngitis), infusion-related reactions, headache, and abdominal pain. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Janssen Biotech, Inc. at 1-800-JANSSEN (1-800-526-7736) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
Other Biological Products– increased risk of serious infections (7.1)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 10/2021
Related/similar drugs
Kenalog, Kenalog-40, Dovonex, Bryhali, Impoyz, Trianex, SpevigoFull Prescribing Information
1. Indications and Usage for Infliximab Injection
1.1 Crohn's Disease
Infliximab is indicated for:
- reducing signs and symptoms and inducing and maintaining clinical remission in adult patients with moderately to severely active Crohn's disease (CD) who have had an inadequate response to conventional therapy.
- reducing the number of draining enterocutaneous and rectovaginal fistulas and maintaining fistula closure in adult patients with fistulizing CD.
1.2 Pediatric Crohn's Disease
Infliximab is indicated for reducing signs and symptoms and inducing and maintaining clinical remission in pediatric patients 6 years of age and older with moderately to severely active CD who have had an inadequate response to conventional therapy.
1.3 Ulcerative Colitis
Infliximab is indicated for reducing signs and symptoms, inducing and maintaining clinical remission and mucosal healing, and eliminating corticosteroid use in adult patients with moderately to severely active ulcerative colitis (UC) who have had an inadequate response to conventional therapy.
1.4 Pediatric Ulcerative Colitis
Infliximab is indicated for reducing signs and symptoms and inducing and maintaining clinical remission in pediatric patients 6 years of age and older with moderately to severely active UC who have had an inadequate response to conventional therapy.
1.5 Rheumatoid Arthritis
Infliximab, in combination with methotrexate, is indicated for reducing signs and symptoms, inhibiting the progression of structural damage, and improving physical function in adult patients with moderately to severely active rheumatoid arthritis (RA).
1.6 Ankylosing Spondylitis
Infliximab is indicated for reducing signs and symptoms in adult patients with active ankylosing spondylitis (AS).
1.7 Psoriatic Arthritis
Infliximab is indicated for reducing signs and symptoms of active arthritis, inhibiting the progression of structural damage, and improving physical function in adult patients with psoriatic arthritis (PsA).
1.8 Plaque Psoriasis
Infliximab is indicated for the treatment of adult patients with chronic severe (i.e., extensive and/or disabling) plaque psoriasis (Ps) who are candidates for systemic therapy and when other systemic therapies are medically less appropriate. Infliximab should only be administered to patients who will be closely monitored and have regular follow-up visits with a physician [see Boxed Warning, Warnings and Precautions (5)].
2. Infliximab Injection Dosage and Administration
2.1 Dosage in Adult Crohn's Disease
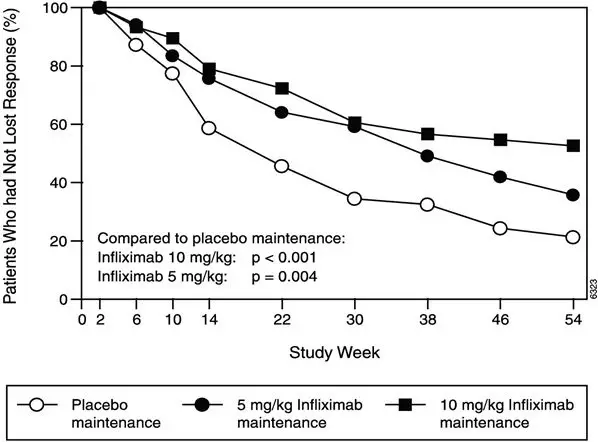
The recommended dosage of Infliximab is 5 mg/kg given as an intravenous induction regimen at 0, 2 and 6 weeks followed by a maintenance regimen of 5 mg/kg every 8 weeks thereafter for the treatment of adults with moderately to severely active CD or fistulizing CD. For adult patients who respond and then lose their response, consideration may be given to treatment with 10 mg/kg every 8 weeks. Patients who do not respond by Week 14 are unlikely to respond with continued dosing and consideration should be given to discontinue Infliximab in these patients.
2.2 Dosage in Pediatric Crohn's Disease
The recommended dosage of Infliximab for pediatric patients 6 years and older with moderately to severely active CD is 5 mg/kg given as an intravenous induction regimen at 0, 2 and 6 weeks followed by a maintenance regimen of 5 mg/kg every 8 weeks.
2.3 Dosage in Adult Ulcerative Colitis
The recommended dosage of Infliximab is 5 mg/kg given as an intravenous induction regimen at 0, 2 and 6 weeks followed by a maintenance regimen of 5 mg/kg every 8 weeks thereafter for the treatment of adult patients with moderately to severely active UC.
2.4 Dosage in Pediatric Ulcerative Colitis
The recommended dosage of Infliximab for pediatric patients 6 years and older with moderately to severely active UC is 5 mg/kg given as an intravenous induction regimen at 0, 2 and 6 weeks followed by a maintenance regimen of 5 mg/kg every 8 weeks.
2.5 Dosage in Rheumatoid Arthritis
The recommended dosage of Infliximab is 3 mg/kg given as an intravenous induction regimen at 0, 2 and 6 weeks followed by a maintenance regimen of 3 mg/kg every 8 weeks thereafter for the treatment of moderately to severely active RA. Infliximab should be given in combination with methotrexate. For patients who have an incomplete response, consideration may be given to adjusting the dosage up to 10 mg/kg every 8 weeks or treating as often as every 4 weeks bearing in mind that risk of serious infections is increased at higher doses per infusion or more frequent dosing [see Adverse Reactions (6.1)].
2.6 Dosage in Ankylosing Spondylitis
The recommended dosage of Infliximab is 5 mg/kg given as an intravenous induction regimen at 0, 2 and 6 weeks followed by a maintenance regimen of 5 mg/kg every 6 weeks thereafter for the treatment of active AS.
2.7 Dosage in Psoriatic Arthritis
The recommended dosage of Infliximab is 5 mg/kg given as an intravenous induction regimen at 0, 2 and 6 weeks followed by a maintenance regimen of 5 mg/kg every 8 weeks thereafter for the treatment of PsA. Infliximab can be used with or without methotrexate.
2.8 Dosage in Plaque Psoriasis
The recommended dosage of Infliximab in adult patients is 5 mg/kg given as an intravenous induction regimen at 0, 2 and 6 weeks followed by a maintenance regimen of 5 mg/kg every 8 weeks thereafter for the treatment of chronic severe (i.e., extensive and/or disabling) Ps.
2.9 Assessment for Latent and Active Tuberculosis
Prior to initiating Infliximab and periodically during therapy, patients should be evaluated for active tuberculosis and tested for latent infection [see Warnings and Precautions (5.1)].
2.10 Administration Instructions Regarding Infusion Reactions
Prior to treatment, ensure appropriate personnel and medication are available to treat reactions (e.g., hypersensitivity, other reactions) that occur during infusion and shortly after infusion. Prior to infusion with Infliximab, patients may be premedicated with histamine-1 receptor antagonists, histamine-2 receptor antagonists, acetaminophen, and/or corticosteroids [see Warnings and Precautions (5.7)].
For mild to moderate reactions during the infusion, consider slowing or stopping the infusion. Upon resolution of these reactions, may reinitiate at a lower infusion rate and/or with histamine-1 receptor antagonists, histamine-2 receptor antagonists, acetaminophen, and/or corticosteroids. Discontinue the infusion if the mild to moderate reactions reoccur.
Discontinue the infusion if severe hypersensitivity reactions occur during the infusion.
2.11 Reconstitution, Dilution, and Administration Instructions
Infliximab is intended for use under the guidance and supervision of a healthcare provider. The supplied lyophilized powder must be reconstituted and diluted prior to administration. The infusion solution should be prepared and administered by a trained medical professional using aseptic technique by the following procedure:
- Calculate the dose, total volume of reconstituted Infliximab solution required and the number of Infliximab vials needed. More than one vial may be needed for a full dose.
- Reconstitute each 100 mg Infliximab vial with 10 mL of Sterile Water for Injection, USP, to obtain a concentration of 10 mg/mL, using a syringe equipped with a 21-gauge or smaller needle as follows:
- Remove the flip-top from the vial and wipe the top with an alcohol swab.
- Insert the syringe needle into the vial through the center of the rubber stopper and direct the stream of Sterile Water for Injection, USP, to the glass wall of the vial. Gently swirl the solution by rotating the vial to dissolve the lyophilized powder, which has a cake-like appearance. Avoid prolonged or vigorous agitation. DO NOT SHAKE. Foaming of the solution on reconstitution is not unusual.
- Allow the reconstituted solution to stand for 5 minutes. Visually inspect the reconstituted solution for particulate matter and discoloration. The reconstituted solution should be colorless to light yellow and opalescent, and the solution may develop a few translucent particles as infliximab is a protein. Do not use if the lyophilized powder has not fully dissolved or if opaque particles, discoloration, or other foreign particles are present. Do not store unused reconstituted Infliximab solution.
- Dilute the total volume of the reconstituted Infliximab solution to 250 mL1 with sterile 0.9% Sodium Chloride Injection, USP, (do not dilute with any other diluent) as follows:
- Withdraw a volume from the 0.9% Sodium Chloride Injection, USP, 250 mL bottle or bag equal to the total volume of reconstituted Infliximab required for a dose. Slowly add the total volume of reconstituted Infliximab solution from the vial(s) to the 250 mL infusion bottle or bag.
- Discard any unused portion of the reconstituted Infliximab solution remaining in the vial(s).
- Gently invert the bag to mix the solution. The resulting infusion concentration should range between 0.4 mg/mL (minimum recommended concentration) and 4 mg/mL (maximum recommended concentration) of infliximab.
- The Infliximab infusion should begin within 3 hours of reconstitution and dilution. The infusion must be administered intravenously for at least 2 hours with an infusion set with an in-line, sterile, non-pyrogenic, low-protein-binding filter (pore size of 1.2 µm or less).
- Given that the vials do not contain antibacterial preservatives, discard any unused portion of the infusion solution (do not store for reuse).
No physical biochemical compatibility studies have been conducted to evaluate the co-administration of Infliximab with other agents. Infliximab should not be infused concomitantly in the same intravenous line with other agents.
- 1
- For volumes greater than 250 mL, either use a larger infusion bag (e.g. 500 mL) or multiple 250 mL infusion bags to ensure that the concentration of the infusion solution does not exceed 4 mg/mL.
3. Dosage Forms and Strengths
For injection: 100 mg of infliximab as a white lyophilized powder in a single-dose vial for reconstitution and dilution.
4. Contraindications
The use of Infliximab at doses >5 mg/kg is contraindicated in patients with moderate or severe heart failure [see Warnings and Precautions (5.5) and Adverse Reactions (6.1)].
Infliximab is contraindicated in patients with a previous severe hypersensitivity reaction to infliximab or any of the inactive ingredients of Infliximab or any murine proteins [severe hypersensitivity reactions have included anaphylaxis, hypotension, and serum sickness] [see Warnings and Precautions (5.7) and Adverse Reactions (6.1)].
5. Warnings and Precautions
5.1 Serious Infections
Patients treated with Infliximab are at increased risk for developing serious infections involving various organ systems and sites that may lead to hospitalization or death.
Opportunistic infections due to bacterial, mycobacterial, invasive fungal, viral, or parasitic organisms including aspergillosis, blastomycosis, candidiasis, coccidioidomycosis, cryptococcosis, histoplasmosis, legionellosis, listeriosis, pneumocystosis, salmonellosis and tuberculosis have been reported with TNF blockers. Patients have frequently presented with disseminated rather than localized disease.
Treatment with Infliximab should not be initiated in patients with an active infection, including clinically important localized infections. Patients greater than 65 years of age, patients with co-morbid conditions and/or patients taking concomitant immunosuppressants such as corticosteroids or methotrexate may be at greater risk of infection. The risks and benefits of treatment should be considered prior to initiating therapy in patients:
- with chronic or recurrent infection;
- who have been exposed to tuberculosis;
- with a history of an opportunistic infection;
- who have resided or traveled in areas of endemic tuberculosis or endemic mycoses, such as histoplasmosis, coccidioidomycosis, or blastomycosis; or
- with underlying conditions that may predispose them to infection.
5.2 Malignancies
Malignancies, some fatal, have been reported among children, adolescents and young adults who received treatment with TNF blockers (initiation of therapy ≤18 years of age), including Infliximab. Approximately half of these cases were lymphomas, including Hodgkin's and non-Hodgkin's lymphoma. The other cases represented a variety of malignancies, including rare malignancies that are usually associated with immunosuppression and malignancies that are not usually observed in children and adolescents. The malignancies occurred after a median of 30 months (range 1 to 84 months) after the first dose of TNF blocker therapy. Most of the patients were receiving concomitant immunosuppressants. These cases were reported post-marketing and are derived from a variety of sources, including registries and spontaneous postmarketing reports.
5.3 Hepatitis B Virus Reactivation
Use of TNF blockers, including Infliximab, has been associated with reactivation of hepatitis B virus (HBV) in patients who are chronic carriers of this virus. In some instances, HBV reactivation occurring in conjunction with TNF blocker therapy has been fatal. The majority of these reports have occurred in patients concomitantly receiving other medications that suppress the immune system, which may also contribute to HBV reactivation. Patients should be tested for HBV infection before initiating TNF blocker therapy, including Infliximab. For patients who test positive for hepatitis B surface antigen, consultation with a physician with expertise in the treatment of hepatitis B is recommended. Adequate data are not available on the safety or efficacy of treating patients who are carriers of HBV with anti-viral therapy in conjunction with TNF blocker therapy to prevent HBV reactivation. Patients who are carriers of HBV and require treatment with TNF blockers should be closely monitored for clinical and laboratory signs of active HBV infection throughout therapy and for several months following termination of therapy. In patients who develop HBV reactivation, TNF blockers should be stopped and antiviral therapy with appropriate supportive treatment should be initiated. The safety of resuming TNF blocker therapy after HBV reactivation is controlled is not known. Therefore, prescribers should exercise caution when considering resumption of TNF blocker therapy in this situation and monitor patients closely.
5.4 Hepatotoxicity
Severe hepatic reactions, including acute liver failure, jaundice, hepatitis and cholestasis, have been reported in postmarketing data in patients receiving Infliximab. Autoimmune hepatitis has been diagnosed in some of these cases. Severe hepatic reactions occurred between 2 weeks to more than 1 year after initiation of Infliximab; elevations in hepatic aminotransferase levels were not noted prior to discovery of the liver injury in many of these cases. Some of these cases were fatal or necessitated liver transplantation. Patients with symptoms or signs of liver dysfunction should be evaluated for evidence of liver injury. If jaundice and/or marked liver enzyme elevations (e.g., ≥5 times the upper limit of normal) develop, Infliximab should be discontinued, and a thorough investigation of the abnormality should be undertaken. In clinical trials, mild or moderate elevations of ALT and AST have been observed in patients receiving Infliximab without progression to severe hepatic injury [see Adverse Reactions (6.1)].
5.5 Heart Failure
The use of Infliximab at doses >5 mg/kg is contraindicated in patients with moderate or severe heart failure. A randomized, double-blind, placebo-controlled study evaluated the use of Infliximab (5 mg/kg or 10 mg/kg at Weeks 0, 2, and 6) in patients with moderate or severe heart failure [New York Heart Association (NYHA) Functional Class III/IV]. Compared to patients who received placebo, there was a higher rate of mortality and a higher risk of hospitalization at Week 28 due to heart failure in patients who received the 10 mg/kg Infliximab dose, and higher rates of cardiovascular adverse events in patients who received Infliximab doses of 5 mg/kg and 10 mg/kg.
There have been post-marketing reports of new onset and worsening heart failure, with and without identifiable precipitating factors (e.g., pre-existing cardiovascular disease), in Infliximab-treated patients. Some of these patients have been under 50 years of age.
If a decision is made to administer Infliximab (≤ 5 mg/kg) to patients with moderate or severe heart failure or to administer Infliximab (any approved dose) to patients with mild heart failure, they should be closely monitored during therapy, and Infliximab should be discontinued if new or worsening symptoms of heart failure appear [see Contraindications (4) and Adverse Reactions (6.1)].
5.6 Hematologic Reactions
Cases of leukopenia, neutropenia, thrombocytopenia, and pancytopenia, some with a fatal outcome, have been reported in patients receiving Infliximab. The causal relationship to Infliximab therapy remains unclear. Although no high-risk group(s) has been identified, caution should be exercised in patients being treated with Infliximab who have ongoing or a history of significant hematologic abnormalities. All patients should be advised to seek immediate medical attention if they develop signs and symptoms suggestive of blood dyscrasias or infection (e.g., persistent fever) while on Infliximab. Discontinuation of Infliximab therapy should be considered in patients who develop significant hematologic abnormalities.
5.7 Hypersensitivity
Infliximab has been associated with hypersensitivity reactions that vary in their time of onset and required hospitalization in some cases. Most hypersensitivity reactions (including anaphylaxis, urticaria, dyspnea, and/or hypotension), have occurred during or within 2 hours of Infliximab infusion.
However, in some cases, serum sickness-like reactions have been observed in patients after initial Infliximab therapy (i.e., as early as after the second dose), and when Infliximab therapy was reinstituted following an extended period without Infliximab treatment. Symptoms associated with these reactions include fever, rash, headache, sore throat, myalgias, polyarthralgias, hand and facial edema and/or dysphagia. These reactions were associated with a marked increase in antibodies to infliximab, loss of detectable serum concentrations of infliximab, and possible loss of drug efficacy.
Infliximab should be discontinued for severe hypersensitivity reactions. Medications for the treatment of hypersensitivity reactions (e.g., acetaminophen, antihistamines, corticosteroids and/or epinephrine) should be available for immediate use in the event of a reaction [see Dosage and Administration (2.10) and Adverse Reactions (6.1)].
In RA, CD and Ps clinical trials, re-administration of Infliximab after a period of no treatment resulted in a higher incidence of infusion reactions relative to regular maintenance treatment [see Adverse Reactions (6.1)]. In general, the benefit-risk of re-administration of Infliximab after a period of no-treatment, especially as a re-induction regimen given at weeks 0, 2 and 6, should be carefully considered. In the case where Infliximab maintenance therapy for Ps is interrupted, Infliximab should be reinitiated as a single dose followed by maintenance therapy.
5.8 Cardiovascular and Cerebrovascular Reactions During and After Infusion
Serious cerebrovascular accidents, myocardial ischemia/infarction (some fatal), hypotension, hypertension, and arrhythmias have been reported during and within 24 hours of initiation of Infliximab infusion. Cases of transient visual loss have been reported during or within 2 hours of infusion of Infliximab. Monitor patients during infusion and if serious reaction occurs, discontinue infusion. Further management of reactions should be dictated by signs and symptoms [see Adverse Reactions (6)].
5.9 Neurologic Reactions
Infliximab and other agents that inhibit TNF have been associated with CNS manifestation of systemic vasculitis, seizure and new onset or exacerbation of clinical symptoms and/or radiographic evidence of central nervous system demyelinating disorders, including multiple sclerosis and optic neuritis, and peripheral demyelinating disorders, including Guillain-Barré syndrome. Prescribers should exercise caution in considering the use of Infliximab in patients with these neurologic disorders and should consider discontinuation of Infliximab if these disorders develop.
5.10 Concurrent Administration with Other Biological Products
Serious infections and neutropenia were seen in clinical studies with concurrent use of anakinra and another TNF blocker, etanercept, with no added clinical benefit compared to etanercept alone. Because of the nature of the adverse reactions seen with the concurrent use of etanercept and anakinra therapy, similar toxicities may also result from the concurrent use of anakinra and other TNF blockers. Therefore, the concurrent use of Infliximab and anakinra is not recommended.
In clinical studies, concurrent administration of TNF blockers and abatacept have been associated with an increased risk of infections including serious infections compared with TNF blockers alone, without increased clinical benefit. Therefore, the concurrent use of Infliximab and abatacept is not recommended [see Drug Interactions (7.1)].
There is insufficient information regarding the concurrent use of Infliximab with other biological products used to treat the same conditions as Infliximab. The concurrent use of Infliximab with these biological products is not recommended because of the possibility of an increased risk of infection [see Drug Interactions (7.1)].
5.11 Switching Between Biological Disease-Modifying Antirheumatic Drugs (DMARDs)
Care should be taken when switching from one biologic to another, since overlapping biological activity may further increase the risk of infection.
5.12 Autoimmunity
Treatment with Infliximab may result in the formation of autoantibodies and in the development of a lupus-like syndrome. If a patient develops symptoms suggestive of a lupus-like syndrome following treatment with Infliximab, treatment should be discontinued [see Adverse Reactions (6.1)].
6. Adverse Reactions/Side Effects
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
6.2 Immunogenicity
As with all therapeutic proteins, there is potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors, including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other infliximab products may be misleading.
Treatment with Infliximab can be associated with the development of antibodies to infliximab. An enzyme immunoassay (EIA) method was originally used to measure anti-infliximab antibodies in clinical studies of Infliximab. The EIA method is subject to interference by serum infliximab, possibly resulting in an underestimation of the rate of patient antibody formation. A separate, drug-tolerant electrochemiluminescence immunoassay (ECLIA) method for detecting antibodies to infliximab was subsequently developed and validated. This method is 60-fold more sensitive than the original EIA. With the ECLIA method, all clinical samples can be classified as either positive or negative for antibodies to infliximab without the need for the inconclusive category.
The incidence of antibodies to infliximab was based on the original EIA method in all clinical studies of Infliximab except for the Phase 3 study in pediatric patients with UC where the incidence of antibodies to infliximab was detected using both the EIA and ECLIA methods.
6.3 Postmarketing Experience
Adverse reactions, some with fatal outcomes, have been identified during post approval use of Infliximab in adult and pediatric patients. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
7. Drug Interactions
7.1 Other Biological Products
The combination of Infliximab with other biological products used to treat the same conditions as Infliximab is not recommended [see Warnings and Precautions (5.10)].
An increased risk of serious infections was seen in clinical studies of other TNF blockers used in combination with anakinra or abatacept, with no added clinical benefit. Because of the nature of the adverse reactions seen with these combinations with TNF blocker therapy, similar toxicities may also result from the combination of anakinra or abatacept with other TNF blockers. Therefore, the combination of Infliximab and anakinra or abatacept is not recommended [see Warnings and Precautions (5.10)].
The concomitant use of tocilizumab with biological DMARDs such as TNF antagonists, including Infliximab, should be avoided because of the possibility of increased immunosuppression and increased risk of infection.
7.2 Methotrexate and Other Concomitant Medications
Specific drug interaction studies, including interactions with methotrexate (MTX), have not been conducted. The majority of patients in RA or CD clinical studies received one or more concomitant medications. In RA, concomitant medications besides MTX were nonsteroidal anti-inflammatory agents (NSAIDs), folic acid, corticosteroids and/or narcotics. Concomitant CD medications were antibiotics, antivirals, corticosteroids, 6-MP/AZA and aminosalicylates. In PsA clinical trials, concomitant medications included MTX in approximately half of the patients as well as NSAIDs, folic acid and corticosteroids. Concomitant MTX use may decrease the incidence of anti-infliximab antibody production and increase infliximab concentrations.
7.3 Immunosuppressants
Patients with CD who received immunosuppressants tended to experience fewer infusion reactions compared to patients on no immunosuppressants [see Adverse Reactions (6.1)]. Serum infliximab concentrations appeared to be unaffected by baseline use of medications for the treatment of CD including corticosteroids, antibiotics (metronidazole or ciprofloxacin) and aminosalicylates.
7.4 Cytochrome P450 Substrates
The formation of CYP450 enzymes may be suppressed by increased levels of cytokines (e.g., TNFα, IL-1, IL-6, IL-10, IFN) during chronic inflammation. Therefore, it is expected that for a molecule that antagonizes cytokine activity, such as infliximab, the formation of CYP450 enzymes could be normalized. Upon initiation or discontinuation of Infliximab in patients being treated with CYP450 substrates with a narrow therapeutic index, monitoring of the effect (e.g., warfarin) or drug concentration (e.g., cyclosporine or theophylline) is recommended and the individual dose of the drug product may be adjusted as needed.
7.5 Live Vaccines/Therapeutic Infectious Agents
It is recommended that live vaccines not be given concurrently with Infliximab. It is also recommended that live vaccines not be given to infants after in utero exposure to infliximab for at least 6 months following birth [see Warnings and Precautions (5.13)].
It is recommended that therapeutic infectious agents not be given concurrently with Infliximab [see Warnings and Precautions (5.13)].
8. Use In Specific Populations
8.4 Pediatric Use
The safety and effectiveness of Infliximab have been established in pediatric patients 6 to 17 years of age for induction and maintenance treatment of CD and UC [see Dosage and Administration (2.2, 2.4) and Adverse Reactions (6.1)]. However, the safety and effectiveness of Infliximab in pediatric patients <6 years of age with CD or UC have not been established. The safety and effectiveness of Infliximab in the treatment of pediatric patients with Ps and juvenile rheumatoid arthritis (JRA) have not been established.
8.5 Geriatric Use
Of the total number of Infliximab-treated patients in RA and Ps clinical studies, 256 (9.6%) were 65 years old and over, while 17 (0.6%) were 75 years old and over. In these trials, no overall differences in safety or effectiveness were observed between geriatric patients (patients ≥ 65 years old) and younger adult patients (patients 18 to 65 years old). However, the incidence of serious adverse reactions in geriatric patients was higher in both Infliximab and control groups compared to younger adult patients.
Of the total number of Infliximab-treated patients in CD, UC, AS, and PsA clinical studies, 76 (3.2%) were 65 years old and over, while 9 (0.4%) were 75 years old and over. In the CD, UC, AS, and PsA studies, there were insufficient numbers of geriatric patients to determine whether they respond differently from younger adults .
The incidence of serious infections in Infliximab-treated geriatric patients was greater than in Infliximab-treated younger adult patients; therefore close monitoring of geriatric patients for the development of serious infections is recommended [see Warnings and Precautions (5.1), and Adverse Reactions (6.1)].
10. Overdosage
Single doses up to 20 mg/kg have been administered without any direct toxic effect. In case of overdosage, it is recommended that the patient be monitored for any signs or symptoms of adverse reactions or effects [see Warnings and Precautions (5)] and appropriate symptomatic treatment instituted immediately.
11. Infliximab Injection Description
Infliximab, a tumor necrosis factor (TNF) blocker, is a chimeric IgG1κ monoclonal antibody (composed of human constant and murine variable regions). It has a molecular weight of approximately 149.1 kilodaltons. Infliximab is produced by a recombinant murine myeloma cell line, SP2/0.
Infliximab for injection is supplied as a sterile, preservative-free, white, lyophilized powder for intravenous infusion after reconstitution and dilution. Following reconstitution with 10 mL of Sterile Water for Injection, USP, the final concentration is 10 mg/mL and the resulting pH is approximately 7.2. Each single-dose vial contains 100 mg infliximab, dibasic sodium phosphate, dihydrate (6.1 mg), monobasic sodium phosphate, monohydrate (2.2 mg), polysorbate 80 (0.5 mg), and sucrose (500 mg).
12. Infliximab Injection - Clinical Pharmacology
12.1 Mechanism of Action
Infliximab neutralizes the biological activity of TNFα by binding with high affinity to the soluble and transmembrane forms of TNFα and inhibits binding of TNFα with its receptors. Infliximab does not neutralize TNFβ (lymphotoxin-α), a related cytokine that utilizes the same receptors as TNFα. Biological activities attributed to TNFα include: induction of pro-inflammatory cytokines such as interleukins (IL) 1 and 6, enhancement of leukocyte migration by increasing endothelial layer permeability and expression of adhesion molecules by endothelial cells and leukocytes, activation of neutrophil and eosinophil functional activity, induction of acute phase reactants and other liver proteins, as well as tissue degrading enzymes produced by synoviocytes and/or chondrocytes. Cells expressing transmembrane TNFα bound by infliximab can be lysed in vitro or in vivo. Infliximab inhibits the functional activity of TNFα in a wide variety of in vitro bioassays utilizing human fibroblasts, endothelial cells, neutrophils, B and T-lymphocytes and epithelial cells. The relationship of these biological response markers to the mechanism(s) by which Infliximab exerts its clinical effects is unknown. Anti-TNFα antibodies reduce disease activity in the cotton-top tamarin colitis model, and decrease synovitis and joint erosions in a murine model of collagen-induced arthritis. Infliximab prevents disease in transgenic mice that develop polyarthritis as a result of constitutive expression of human TNFα, and when administered after disease onset, allows eroded joints to heal.
12.2 Pharmacodynamics
Elevated concentrations of TNFα have been found in involved tissues and fluids of patients with RA, CD, UC, AS, PsA, and Ps. In RA, treatment with Infliximab reduced infiltration of inflammatory cells into inflamed areas of the joint as well as expression of molecules mediating cellular adhesion [E-selectin, intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1 (VCAM-1)], chemoattraction [IL-8 and monocyte chemotactic protein (MCP-1)] and tissue degradation [matrix metalloproteinase (MMP) 1 and 3]. In CD, treatment with Infliximab reduced infiltration of inflammatory cells and TNFα production in inflamed areas of the intestine, and reduced the proportion of mononuclear cells from the lamina propria able to express TNFα and interferon. After treatment with Infliximab, patients with RA or CD exhibited decreased levels of serum IL-6 and C-reactive protein (CRP) compared to baseline. Peripheral blood lymphocytes from Infliximab-treated patients showed no significant decrease in number or in proliferative responses to in vitro mitogenic stimulation when compared to cells from untreated patients. In PsA, treatment with Infliximab resulted in a reduction in the number of T-cells and blood vessels in the synovium and psoriatic skin lesions as well as a reduction of macrophages in the synovium. In Ps, Infliximab treatment may reduce the epidermal thickness and infiltration of inflammatory cells. The relationship between these pharmacodynamic activities and the mechanism(s) by which Infliximab exerts its clinical effects is unknown.
12.3 Pharmacokinetics
In adults, single intravenous (IV) infusions of 3 mg/kg to 20 mg/kg (two times the maximum recommended dose for any indication) showed a linear relationship between the dose administered and the maximum serum concentration. The volume of distribution at steady state was independent of dose and indicated that infliximab was distributed primarily within the vascular compartment. Pharmacokinetic results for single doses of 3 mg/kg to 10 mg/kg in RA, 5 mg/kg in CD, and 3 mg/kg to 5 mg/kg in Ps indicate that the median terminal half-life of infliximab is 7.7 to 9.5 days.
Following an initial dose of Infliximab, repeated infusions at 2 and 6 weeks resulted in predictable concentration-time profiles following each treatment. No systemic accumulation of infliximab occurred upon continued repeated treatment with 3 mg/kg or 10 mg/kg at 4- or 8-week intervals. Development of antibodies to infliximab increased infliximab clearance. At 8 weeks after a maintenance dose of 3 to 10 mg/kg of Infliximab, median infliximab serum concentrations ranged from approximately 0.5 to 6 mcg/mL; however, infliximab concentrations were not detectable (<0.1 mcg/mL) in patients who became positive for antibodies to infliximab. No major differences in clearance or volume of distribution were observed in patient subgroups defined by age, weight, or gender. It is not known if there are differences in clearance or volume of distribution in patients with marked impairment of hepatic or renal function.
Infliximab pharmacokinetic characteristics (including peak and trough concentrations and terminal half-life) were similar in pediatric (aged 6 to 17 years) and adult patients with CD or UC following the administration of 5 mg/kg of Infliximab.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
A 6-month study in CD-1 mice was conducted to assess the tumorigenic potential of cV1q anti-mouse TNFα, an analogous antibody. No evidence of tumorigenicity was observed in mice that received intravenous doses of 10 mg/kg or 40 mg/kg cV1q given weekly. The relevance of this study for human risk is unknown. No impairment of fertility or reproductive performance indices were observed in male or female mice that received cV1q, an analogous mouse antibody, at intravenous doses up to 40 mg/kg given weekly.
14. Clinical Studies
14.2 Pediatric Crohn's Disease
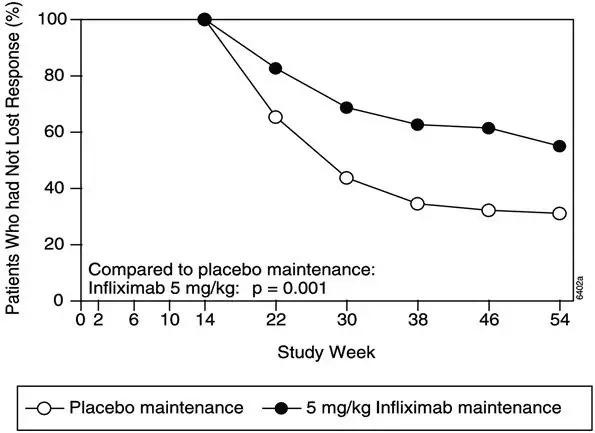
The safety and efficacy of Infliximab were assessed in a randomized, open-label study (Study Peds Crohn's) in 112 pediatric patients aged 6 to 17 years old with moderately to severely active CD and an inadequate response to conventional therapies. The median age was 13 years and the median Pediatric Crohn's Disease Activity Index (PCDAI) was 40 (on a scale of 0 to 100). All patients were required to be on a stable dose of 6-MP, AZA, or MTX; 35% were also receiving corticosteroids at baseline.
All patients received induction dosing of 5 mg/kg Infliximab at Weeks 0, 2, and 6. At Week 10, 103 patients were randomized to a maintenance regimen of 5 mg/kg Infliximab given either every 8 weeks or every 12 weeks.
At Week 10, 88% of patients were in clinical response (defined as a decrease from baseline in the PCDAI score of ≥15 points and total PCDAI score of ≤30 points), and 59% were in clinical remission (defined as PCDAI score of ≤10 points).
The proportion of pediatric patients achieving clinical response at Week 10 compared favorably with the proportion of adults achieving a clinical response in Study Crohn's I. The study definition of clinical response in Study Peds Crohn's was based on the PCDAI score, whereas the CDAI score was used in the adult Study Crohn's I.
At both Week 30 and Week 54, the proportion of patients in clinical response was greater in the every 8-week treatment group than in the every 12-week treatment group (73% vs. 47% at Week 30, and 64% vs. 33% at Week 54). At both Week 30 and Week 54, the proportion of patients in clinical remission was also greater in the every 8-week treatment group than in the every 12-week treatment group (60% vs. 35% at Week 30, and 56% vs. 24% at Week 54), (Table 4).
For patients in Study Peds Crohn's receiving corticosteroids at baseline, the proportion of patients able to discontinue corticosteroids while in remission at Week 30 was 46% for the every 8-week maintenance group and 33% for the every 12-week maintenance group. At Week 54, the proportion of patients able to discontinue corticosteroids while in remission was 46% for the every 8-week maintenance group and 17% for the every 12-week maintenance group.
| 5 mg/kg Infliximab | ||
|---|---|---|
| Every 8 Week | Every 12 Week | |
| Treatment Group | Treatment Group | |
|
||
| Patients randomized | 52 | 51 |
| Clinical Response* | ||
| Week 30 | 73%† | 47% |
| Week 54 | 64%† | 33% |
| Clinical Remission‡ | ||
| Week 30 | 60%§ | 35% |
| Week 54 | 56%† | 24% |
14.3 Adult Ulcerative Colitis
The safety and efficacy of Infliximab were assessed in 2 randomized, double-blind, placebo-controlled clinical studies in 728 adult patients with moderately to severely active UC (Mayo score 6 to 12 [of possible range 0 to 12], Endoscopy subscore ≥2) with an inadequate response to conventional oral therapies (Studies UC I and UC II). Concomitant treatment with stable doses of aminosalicylates, corticosteroids and/or immunomodulatory agents was permitted. Corticosteroid taper was permitted after Week 8. Patients were randomized at week 0 to receive either placebo, 5 mg/kg Infliximab or 10 mg/kg Infliximab at Weeks 0, 2, 6, and every 8 weeks thereafter through Week 46 in Study UC I, and at Weeks 0, 2, 6, and every 8 weeks thereafter through Week 22 in Study UC II. In Study UC II, patients were allowed to continue blinded therapy to Week 46 at the investigator's discretion.
Adult patients in Study UC I had failed to respond or were intolerant to oral corticosteroids, 6-MP, or AZA. Adult patients in Study UC II had failed to respond or were intolerant to the above treatments and/or aminosalicylates. Similar proportions of patients in Studies UC I and UC II were receiving corticosteroids (61% and 51%, respectively), 6-MP/AZA (49% and 43%) and aminosalicylates (70% and 75%) at baseline. More patients in Study UC II than UC I were taking solely aminosalicylates for UC (26% vs. 11%, respectively). Clinical response was defined as a decrease from baseline in the Mayo score by ≥30% and ≥3 points, accompanied by a decrease in the rectal bleeding subscore of ≥1 or a rectal bleeding subscore of 0 or 1.
14.4 Pediatric Ulcerative Colitis
The safety and effectiveness of Infliximab for reducing signs and symptoms and inducing and maintaining clinical remission in pediatric patients aged 6 years and older with moderately to severely active UC who have had an inadequate response to conventional therapy are supported by evidence from adequate and well-controlled studies of Infliximab in adults. Additional safety and pharmacokinetic data were collected in an open-label pediatric UC trial in 60 pediatric patients aged 6 through 17 years (median age 14.5 years) with moderately to severely active UC (Mayo score of 6 to 12; Endoscopic subscore ≥2) and an inadequate response to conventional therapies. At baseline, the median Mayo score was 8, 53% of patients were receiving immunomodulator therapy (6-MP/AZA/MTX), and 62% of patients were receiving corticosteroids (median dose 0.5 mg/kg/day in prednisone equivalents). Discontinuation of immunomodulators and corticosteroid taper were permitted after Week 0.
All patients received induction dosing of 5 mg/kg Infliximab at Weeks 0, 2, and 6. Patients who did not respond to Infliximab at Week 8 received no further Infliximab and returned for safety follow-up. At Week 8, 45 patients were randomized to a maintenance regimen of 5 mg/kg Infliximab given either every 8 weeks through Week 46 or every 12 weeks through Week 42. Patients were allowed to change to a higher dose and/or more frequent administration schedule if they experienced loss of response.
Clinical response at Week 8 was defined as a decrease from baseline in the Mayo score by ≥30% and ≥3 points, including a decrease in the rectal bleeding subscore by ≥1 points or achievement of a rectal bleeding subscore of 0 or 1.
Clinical remission at Week 8 was measured by the Mayo score, defined as a Mayo score of ≤2 points with no individual subscore >1. Clinical remission was also assessed at Week 8 and Week 54 using the Pediatric Ulcerative Colitis Activity Index (PUCAI)1 score and was defined by a PUCAI score of <10 points.
Endoscopies were performed at baseline and at Week 8. A Mayo endoscopy subscore of 0 indicated normal or inactive disease and a subscore of 1 indicated mild disease (erythema, decreased vascular pattern, or mild friability).
Of the 60 patients treated, 44 were in clinical response at Week 8. Of 32 patients taking concomitant immunomodulators at baseline, 23 achieved clinical response at Week 8, compared to 21 of 28 of those not taking concomitant immunomodulators at baseline. At Week 8, 24 of 60 patients were in clinical remission as measured by the Mayo score and 17 of 51 patients were in remission as measured by the PUCAI score.
At Week 54, 8 of 21 patients in the every 8-week maintenance group and 4 of 22 patients in the every 12-week maintenance group achieved remission as measured by the PUCAI score.
During maintenance phase, 23 of 45 randomized patients (9 in the every 8-week group and 14 in the every 12-week group) required an increase in their dose and/or increase in frequency of Infliximab administration due to loss of response. Nine of the 23 patients who required a change in dose had achieved remission at Week 54. Seven of those patients received the 10 mg/kg every 8-week dosing.
14.5 Rheumatoid Arthritis
The safety and efficacy of Infliximab in adult patients with RA were assessed in 2 multicenter, randomized, double-blind, pivotal trials: ATTRACT (Study RA I) and ASPIRE (Study RA II). Concurrent use of stable doses of folic acid, oral corticosteroids (≤10 mg/day) and/or non-steroidal anti-inflammatory drugs (NSAIDs) was permitted.
Study RA I was a placebo-controlled study of 428 patients with active RA despite treatment with MTX. Patients enrolled had a median age of 54 years, median disease duration of 8.4 years, median swollen and tender joint count of 20 and 31 respectively, and were on a median dose of 15 mg/wk of MTX. Patients received either placebo+MTX or one of 4 doses/schedules of Infliximab+MTX: 3 mg/kg or 10 mg/kg of Infliximab by IV infusion at Weeks 0, 2 and 6 followed by additional infusions every 4 or 8 weeks in combination with MTX.
Study RA II was a placebo-controlled study of 3 active treatment arms in 1004 MTX naive patients of 3 or fewer years' duration active RA. Patients enrolled had a median age of 51 years with a median disease duration of 0.6 years, median swollen and tender joint count of 19 and 31 , respectively, and >80% of patients had baseline joint erosions. At randomization, all patients received MTX (optimized to 20 mg/wk by Week 8) and either placebo, 3 mg/kg or 6 mg/kg Infliximab at Weeks 0, 2, and 6 and every 8 weeks thereafter.
Data on use of Infliximab without concurrent MTX are limited [see Adverse Reactions (6.1)].
14.6 Ankylosing Spondylitis
The safety and efficacy of Infliximab were assessed in a randomized, multicenter, double-blind, placebo-controlled study in 279 adult patients with active AS. Patients were between 18 and 74 years of age, and had AS, as defined by the modified New York criteria for Ankylosing Spondylitis. Patients were to have had active disease as evidenced by both a Bath Ankylosing Spondylitis Disease Activity Index (BASDAI) score >4 (possible range 0–10) and spinal pain >4 (on a Visual Analog Scale [VAS] of 0–10). Patients with complete ankylosis of the spine were excluded from study participation, and the use of Disease Modifying Anti-Rheumatic Drugs (DMARDs) and systemic corticosteroids were prohibited. Doses of Infliximab 5 mg/kg or placebo were administered intravenously at Weeks 0, 2, 6, 12 and 18.
At 24 weeks, improvement in the signs and symptoms of AS, as measured by the proportion of patients achieving a 20% improvement in ASAS response criteria (ASAS 20), was seen in 60% of patients in the Infliximab-treated group vs. 18% of patients in the placebo group (p<0.001). Improvement was observed at Week 2 and maintained through Week 24 (Figure 3 and Table 10).
Figure 3: Proportion of Adult AS Patients Who Achieved a ASAS 20 Response
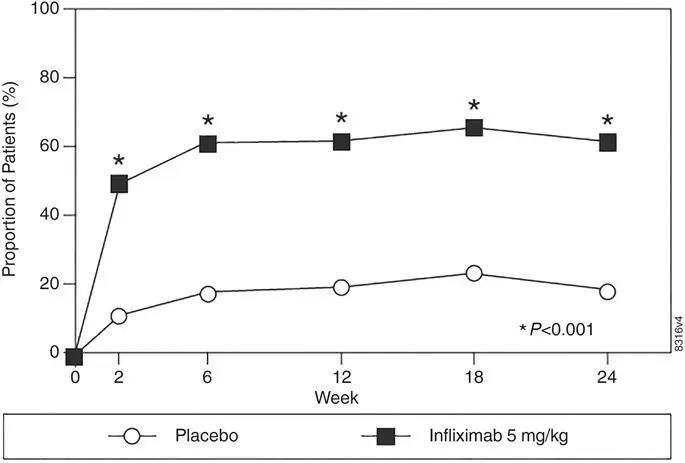
At 24 weeks, the proportions of patients achieving a 50% and a 70% improvement in the signs and symptoms of AS, as measured by ASAS response criteria (ASAS 50 and ASAS 70, respectively), were 44% and 28%, respectively, for patients receiving Infliximab, compared to 9% and 4%, respectively, for patients receiving placebo (P<0.001, Infliximab vs. placebo). A low level of disease activity (defined as a value <20 [on a scale of 0–100 mm] in each of the 4 ASAS response parameters) was achieved in 22% of Infliximab-treated patients vs. 1% in placebo-treated patients (P<0.001).
| Placebo (n=78) | Infliximab 5 mg/kg (n=201) | ||||
|---|---|---|---|---|---|
| Baseline | 24 Weeks | Baseline | 24 Weeks | P-value | |
|
|||||
| ASAS 20 response | |||||
| Criteria (Mean) | |||||
| Patient Global Assessment* | 6.6 | 6.0 | 6.8 | 3.8 | <0.001 |
| Spinal pain* | 7.3 | 6.5 | 7.6 | 4.0 | <0.001 |
| BASFI† | 5.8 | 5.6 | 5.7 | 3.6 | <0.001 |
| Inflammation‡ | 6.9 | 5.8 | 6.9 | 3.4 | <0.001 |
| Acute Phase Reactants | |||||
| Median CRP§ (mg/dL) | 1.7 | 1.5 | 1.5 | 0.4 | <0.001 |
| Spinal Mobility (cm, Mean) | |||||
| Modified Schober's test¶ | 4.0 | 5.0 | 4.3 | 4.4 | 0.75 |
| Chest expansion¶ | 3.6 | 3.7 | 3.3 | 3.9 | 0.04 |
| Tragus to wall¶ | 17.3 | 17.4 | 16.9 | 15.7 | 0.02 |
| Lateral spinal flexion¶ | 10.6 | 11.0 | 11.4 | 12.9 | 0.03 |
The median improvement from baseline in the general health-related quality-of-life questionnaire SF-36 physical component summary score at Week 24 was 10.2 for the Infliximab group vs. 0.8 for the placebo group (P<0.001). There was no change in the SF-36 mental component summary score in either the Infliximab group or the placebo group.
Results of this study were similar to those seen in a multicenter double-blind, placebo-controlled study of 70 patients with AS.
14.7 Psoriatic Arthritis
Safety and efficacy of Infliximab were assessed in a multicenter, double-blind, placebo-controlled study in 200 adult patients with active PsA despite DMARD or NSAID therapy (≥5 swollen joints and ≥5 tender joints) with 1 or more of the following subtypes: arthritis involving DIP joints (n=49), arthritis mutilans (n=3), asymmetric peripheral arthritis (n=40), polyarticular arthritis (n=100), and spondylitis with peripheral arthritis (n=8). Patients also had Ps with a qualifying target lesion ≥2 cm in diameter. Forty-six percent of patients continued on stable doses of methotrexate (≤25 mg/week). During the 24-week double-blind phase, patients received either 5 mg/kg Infliximab or placebo at Weeks 0, 2, 6, 14, and 22 (100 patients in each group). At Week 16, placebo patients with <10% improvement from baseline in both swollen and tender joint counts were switched to Infliximab induction (early escape). At Week 24, all placebo-treated patients crossed over to Infliximab induction. Dosing continued for all patients through Week 46.
14.8 Plaque Psoriasis
The safety and efficacy of Infliximab were assessed in 3 randomized, double-blind, placebo-controlled studies in patients 18 years of age and older with chronic, stable Ps involving ≥10% BSA, a minimum PASI score of 12, and who were candidates for systemic therapy or phototherapy. Patients with guttate, pustular, or erythrodermic psoriasis were excluded from these studies. No concomitant anti-psoriatic therapies were allowed during the study, with the exception of low-potency topical corticosteroids on the face and groin after Week 10 of study initiation.
Study I (EXPRESS) evaluated 378 patients who received placebo or Infliximab at a dose of 5 mg/kg at Weeks 0, 2, and 6 (induction therapy), followed by maintenance therapy every 8 weeks. At Week 24, the placebo group crossed over to Infliximab induction therapy (5 mg/kg), followed by maintenance therapy every 8 weeks. Patients originally randomized to Infliximab continued to receive Infliximab 5 mg/kg every 8 weeks through Week 46. Across all treatment groups, the median baseline PASI score was 21 and the baseline Static Physician Global Assessment (sPGA) score ranged from moderate (52% of patients) to marked (36%) to severe (2%). In addition, 75% of patients had a BSA >20%. Seventy-one percent of patients previously received systemic therapy, and 82% received phototherapy.
Study II (EXPRESS II) evaluated 835 patients who received placebo or Infliximab at doses of 3 mg/kg or 5 mg/kg at Weeks 0, 2, and 6 (induction therapy). At Week 14, within each Infliximab dose group, patients were randomized to either scheduled (every 8 weeks) or as needed (PRN) maintenance treatment through Week 46. At Week 16, the placebo group crossed over to Infliximab induction therapy (5 mg/kg), followed by maintenance therapy every 8 weeks. Across all treatment groups, the median baseline PASI score was 18, and 63% of patients had a BSA >20%. Fifty-five percent of patients previously received systemic therapy, and 64% received a phototherapy.
Study III (SPIRIT) evaluated 249 patients who had previously received either psoralen plus ultraviolet A treatment (PUVA) or other systemic therapy for their psoriasis. These patients were randomized to receive either placebo or Infliximab at doses of 3 mg/kg or 5 mg/kg at Weeks 0, 2, and 6. At Week 26, patients with a sPGA score of moderate or worse (greater than or equal to 3 on a scale of 0 to 5) received an additional dose of the randomized treatment. Across all treatment groups, the median baseline PASI score was 19, and the baseline sPGA score ranged from moderate (62% of patients) to marked (22%) to severe (3%). In addition, 75% of patients had a BSA >20%. Of the enrolled patients, 114 (46%) received the Week 26 additional dose.
In Studies I, II and III, the primary endpoint was the proportion of patients who achieved a reduction in score of at least 75% from baseline at Week 10 by the PASI (PASI 75). In Study I and Study III, another evaluated outcome included the proportion of patients who achieved a score of "cleared" or "minimal" by the sPGA. The sPGA is a 6-category scale ranging from "5 = severe" to "0 = cleared" indicating the physician's overall assessment of the psoriasis severity focusing on induration, erythema, and scaling. Treatment success, defined as "cleared" or "minimal," consisted of none or minimal elevation in plaque, up to faint red coloration in erythema, and none or minimal fine scale over <5% of the plaque.
Study II also evaluated the proportion of patients who achieved a score of "clear" or "excellent" by the relative Physician's Global Assessment (rPGA). The rPGA is a 6-category scale ranging from "6 = worse" to "1 = clear" that was assessed relative to baseline. Overall lesions were graded with consideration to the percent of body involvement as well as overall induration, scaling, and erythema. Treatment success, defined as "clear" or "excellent," consisted of some residual pinkness or pigmentation to marked improvement (nearly normal skin texture; some erythema may be present). The results of these studies are presented in Table 12.
| Placebo | Infliximab | ||
|---|---|---|---|
| 3 mg/kg | 5 mg/kg | ||
|
|||
| Psoriasis Study I - patients randomized* | 77 | — | 301 |
| PASI 75 | 2 (3%) | — | 242 (80%)† |
| sPGA | 3 (4%) | — | 242 (80%)† |
| Psoriasis Study II - patients randomized* | 208 | 313 | 314 |
| PASI 75 | 4 (2%) | 220 (70%)† | 237 (75%)† |
| rPGA | 2 (1%) | 217 (69%)† | 234 (75%)† |
| Psoriasis Study III - patients randomized‡ | 51 | 99 | 99 |
| PASI 75 | 3 (6%) | 71 (72%)† | 87 (88%)† |
| sPGA | 5 (10%) | 71 (72%)† | 89 (90%)† |
In Study I, in the subgroup of patients with more extensive Ps who had previously received phototherapy, 85% of patients on 5 mg/kg Infliximab achieved a PASI 75 at Week 10 compared with 4% of patients on placebo.
In Study II, in the subgroup of patients with more extensive Ps who had previously received phototherapy, 72% and 77% of patients on 3 mg/kg and 5 mg/kg Infliximab achieved a PASI 75 at Week 10 respectively compared with 1% on placebo. In Study II, among patients with more extensive Ps who had failed or were intolerant to phototherapy, 70% and 78% of patients on 3 mg/kg and 5 mg/kg Infliximab achieved a PASI 75 at Week 10 respectively, compared with 2% on placebo.
Maintenance of response was studied in a subset of 292 and 297 Infliximab-treated patients in the 3 mg/kg and 5 mg/kg groups; respectively, in Study II. Stratified by PASI response at Week 10 and investigational site, patients in the active treatment groups were re-randomized to either a scheduled or as needed maintenance (PRN) therapy, beginning on Week 14.
The groups that received a maintenance dose every 8 weeks appear to have a greater percentage of patients maintaining a PASI 75 through Week 50 as compared to patients who received the as-needed or PRN doses, and the best response was maintained with the 5 mg/kg every 8-week dose. These results are shown in Figure 4. At Week 46, when Infliximab serum concentrations were at trough level, in the every 8-week dose group, 54% of patients in the 5 mg/kg group compared to 36% in the 3 mg/kg group achieved PASI 75. The lower percentage of PASI 75 responders in the 3 mg/kg every 8-week dose group compared to the 5 mg/kg group was associated with a lower percentage of patients with detectable trough serum infliximab levels. This may be related in part to higher antibody rates [see Adverse Reactions (6.1)]. In addition, in a subset of patients who had achieved a response at Week 10, maintenance of response appears to be greater in patients who received Infliximab every 8 weeks at the 5 mg/kg dose. Regardless of whether the maintenance doses are PRN or every 8 weeks, there is a decline in response in a subpopulation of patients in each group over time. The results of Study I through Week 50 in the 5 mg/kg every 8 weeks maintenance dose group were similar to the results from Study II.
Figure 4: Proportion of Adult Ps Patients Who Achieved ≥75% Improvement in PASI from Baseline through Week 50 (patients randomized at Week 14)
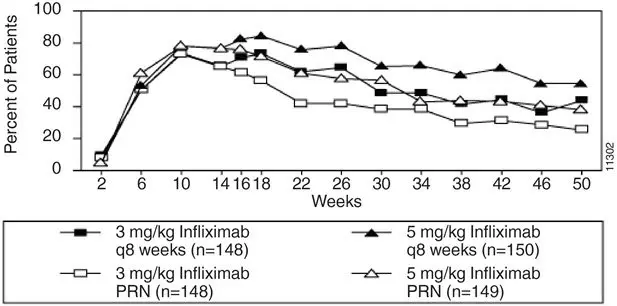
Efficacy and safety of Infliximab treatment beyond 50 weeks have not been evaluated in patients with Ps.
15. References
- Turner D, Otley AR, Mack D, et al. Development, validation, and evaluation of a pediatric ulcerative colitis activity index: A prospective multicenter study. Gastroenterology. 2007;133:423–432.
17. Patient Counseling Information
Advise the patient or their caregiver to read the FDA-approved patient labeling (Medication Guide).
Patients or their caregivers should be advised of the potential benefits and risks of Infliximab. Healthcare providers should instruct their patients or their caregivers to read the Medication Guide before starting Infliximab therapy and to reread it each time they receive an infusion.
| MEDICATION GUIDE Infliximab for injection, for intravenous use |
|||||
|---|---|---|---|---|---|
| This Medication Guide has been approved by the U.S. Food and Drug Administration | Revised: October 2021 | ||||
| Read the Medication Guide that comes with Infliximab before you receive the first treatment, and before each time you get a treatment of Infliximab. This Medication Guide does not take the place of talking with your doctor about your medical condition or treatment. | |||||
| What is the most important information I should know about Infliximab? | |||||
| Infliximab may cause serious side effects, including: | |||||
| 1. Risk of infection | |||||
| Infliximab is a medicine that affects your immune system. Infliximab can lower the ability of your immune system to fight infections. Serious infections have happened in patients receiving Infliximab. These infections include tuberculosis (TB) and infections caused by viruses, fungi or bacteria that have spread throughout the body. Some patients have died from these infections. | |||||
|
|||||
| Before starting Infliximab, tell your doctor if you: | |||||
|
|||||
| After starting Infliximab, if you have an infection, any sign of an infection including a fever, cough, flu-like symptoms, or have open cuts or sores on your body, call your doctor right away. Infliximab can make you more likely to get infections or make any infection that you have worse. | |||||
| 2. Risk of Cancer | |||||
|
|||||
| See the section "What are the possible side effects of Infliximab?" below for more information. | |||||
| What is Infliximab? | |||||
| Infliximab is a prescription medicine that is approved for patients with: | |||||
|
|||||
| Infliximab blocks the action of a protein in your body called tumor necrosis factor-alpha (TNF-alpha). TNF-alpha is made by your body's immune system. People with certain diseases have too much TNF-alpha that can cause the immune system to attack normal healthy parts of the body. Infliximab can block the damage caused by too much TNF-alpha. | |||||
| It is not known if Infliximab is safe and effective in children under 6 years of age. | |||||
| Who should not receive Infliximab? | |||||
| You should not receive Infliximab if you have: | |||||
|
|||||
| What should I tell my doctor before starting treatment with Infliximab? | |||||
| Your doctor will assess your health before each treatment. | |||||
| Tell your doctor about all of your medical conditions, including if you: | |||||
|
|||||
| If you have a baby and you were receiving Infliximab during your pregnancy, it is important to tell your baby's doctor and other health care professionals about your Infliximab use so they can decide when your baby should receive any vaccine. Certain vaccinations can cause infections. | |||||
| If you received Infliximab while you were pregnant, your baby may be at higher risk for getting an infection. If your baby receives a live vaccine within 6 months after birth, your baby may develop infections with serious complications that can lead to death. This includes live vaccines such as the BCG, rotavirus, or any other live vaccines. For other types of vaccines, talk with your doctor. | |||||
| How should I receive Infliximab? | |||||
|
|||||
| What should I avoid while receiving Infliximab? | |||||
| Do not take Infliximab together with medicines such as KINERET (anakinra), ORENCIA (abatacept), ACTEMRA (tocilizumab), or other medicines called biologics that are used to treat the same conditions as Infliximab. | |||||
| Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. These include any other medicines to treat Crohn's disease, ulcerative colitis, rheumatoid arthritis, ankylosing spondylitis, psoriatic arthritis or psoriasis. | |||||
| Know the medicines you take. Keep a list of your medicines and show them to your doctor and pharmacist when you get a new medicine. | |||||
| What are the possible side effects of Infliximab? | |||||
| Infliximab can cause serious side effects, including: | |||||
| See "What is the most important information I should know about Infliximab?" | |||||
| Serious Infections | |||||
|
|||||
|
|
||||
|
|||||
|
|
||||
| Heart Failure | |||||
| If you have a heart problem called congestive heart failure, your doctor should check you closely while you are receiving Infliximab. Your congestive heart failure may get worse while you are receiving Infliximab. Be sure to tell your doctor of any new or worse symptoms including: | |||||
|
|
||||
| Treatment with Infliximab may need to be stopped if you get new or worse congestive heart failure. | |||||
| Other Heart Problems | |||||
| Some patients have experienced a heart attack (some of which led to death), low blood flow to the heart, or abnormal heart rhythm within 24 hours of beginning their infusion of Infliximab. Symptoms may include chest discomfort or pain, arm pain, stomach pain, shortness of breath, anxiety, lightheadedness, dizziness, fainting, sweating, nausea, vomiting, fluttering or pounding in your chest, and/or a fast or a slow heartbeat. Tell your doctor right away if you have any of these symptoms. | |||||
| Liver Injury | |||||
| Some patients receiving Infliximab have developed serious liver problems. Tell your doctor if you have: | |||||
|
|
||||
| Blood Problems | |||||
| In some patients receiving Infliximab, the body may not make enough of the blood cells that help fight infections or help stop bleeding. Tell your doctor if you: | |||||
|
|
||||
| Nervous System Disorders | |||||
| Some patients receiving Infliximab have developed problems with their nervous system. Tell your doctor if you have: | |||||
|
|
||||
| Some patients have experienced a stroke within approximately 24 hours of their infusion with Infliximab. Tell your doctor right away if you have symptoms of a stroke which may include: numbness or weakness of the face, arm or leg, especially on one side of the body; sudden confusion, trouble speaking or understanding; sudden trouble seeing in one or both eyes, sudden trouble walking, dizziness, loss of balance or coordination or a sudden, severe headache. | |||||
| Allergic Reactions | |||||
| Some patients have had allergic reactions to Infliximab. Some of these reactions were severe. These reactions can happen while you are getting your Infliximab treatment or shortly afterward. Your doctor may need to stop or pause your treatment with Infliximab and may give you medicines to treat the allergic reaction. Signs of an allergic reaction can include: | |||||
|
|
||||
| Some patients treated with Infliximab have had delayed allergic reactions. The delayed reactions occurred 3 to 12 days after receiving treatment with Infliximab. Tell your doctor right away if you have any of these signs of delayed allergic reaction to Infliximab: | |||||
|
|
||||
| Lupus-like Syndrome | |||||
| Some patients have developed symptoms that are like the symptoms of Lupus. If you develop any of the following symptoms, your doctor may decide to stop your treatment with Infliximab. | |||||
|
|
||||
| Psoriasis | |||||
| Some people receiving Infliximab had new psoriasis or worsening of psoriasis they already had. Tell your doctor if you develop red scaly patches or raised bumps on the skin that are filled with pus. Your doctor may decide to stop your treatment with Infliximab. | |||||
| The most common side effects of Infliximab include: | |||||
|
|
||||
| Infusion reactions can happen up to 2 hours after your infusion of Infliximab. Symptoms of infusion reactions may include: | |||||
|
|
|
|||
| Children who received Infliximab in studies for Crohn's disease showed some differences in side effects compared with adults who received Infliximab for Crohn's disease. The side effects that happened more in children were: anemia (low red blood cells), leukopenia (low white blood cells), flushing (redness or blushing), viral infections, neutropenia (low neutrophils, the white blood cells that fight infection), bone fracture, bacterial infection and allergic reactions of the breathing tract. Among patients who received Infliximab for ulcerative colitis in clinical studies, more children had infections as compared with adults. | |||||
| Tell your doctor about any side effect that bothers you or does not go away. | |||||
| These are not all of the side effects with Infliximab. Ask your doctor or pharmacist for more information. | |||||
| Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. | |||||
| General information about Infliximab | |||||
| Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. | |||||
| You can ask your doctor or pharmacist for information about Infliximab that is written for health professionals. | |||||
| For more information call 1-800-JANSSEN (1-800-526-7736). | |||||
| What are the ingredients in Infliximab? | |||||
| The active ingredient is Infliximab. | |||||
| The inactive ingredients in Infliximab include: dibasic sodium phosphate dihydrate, monobasic sodium phosphate monohydrate, polysorbate 80, and sucrose. No preservatives are present. | |||||
| Manufactured by: Janssen Biotech, Inc. Horsham, PA 19044 U.S. License No. 1864 |
|||||
| INFLIXIMAB
infliximab injection, powder, lyophilized, for solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Janssen Biotech, Inc. (099091753) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Janssen Biologics B.V. | 409612918 | API MANUFACTURE(57894-160) , ANALYSIS(57894-160) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Janssen Biotech, Inc. | 038978363 | API MANUFACTURE(57894-160) , ANALYSIS(57894-160) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Janssen-Cilag Manufacturing, LLC | 963971374 | MANUFACTURE(57894-160) , ANALYSIS(57894-160) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Hospira, Inc. | 030606222 | MANUFACTURE(57894-160) , ANALYSIS(57894-160) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Cilag AG | 483237103 | MANUFACTURE(57894-160) , ANALYSIS(57894-160) , PACK(57894-160) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| AndersonBrecon Inc. | 053217022 | PACK(57894-160) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Janssen Ortho LLC | 084894661 | ANALYSIS(57894-160) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Patheon Italia S.p.A. | 338336589 | MANUFACTURE(57894-160) | |