Drug Detail:Keppra (Levetiracetam (oral/injection) [ lee-ve-tye-ra-se-tam ])
Drug Class: Pyrrolidine anticonvulsants
Highlights of Prescribing Information
KEPPRA (levetiracetam) tablets, for oral use
KEPPRA (levetiracetam) oral solution
Initial U.S. Approval: 1999
Indications and Usage for Keppra
KEPPRA is indicated for the treatment of partial-onset seizures in patients 1 month of age and older (1.1)
KEPPRA is indicated for adjunctive therapy for the treatment of:
- Myoclonic seizures in patients 12 years of age and older with juvenile myoclonic epilepsy (1.2)
- Primary generalized tonic-clonic seizures in patients 6 years of age and older with idiopathic generalized epilepsy (1.3)
Keppra Dosage and Administration
- Use the oral solution for pediatric patients with body weight ≤ 20 kg (2.1)
- For pediatric patients, use weight-based dosing for the oral solution with a calibrated measuring device (not a household teaspoon or tablespoon) (2.1)
Partial-Onset Seizures (monotherapy or adjunctive therapy)
- 1 Month to < 6 Months: 7 mg/kg twice daily; increase by 7 mg/kg twice daily every 2 weeks to recommended dose of 21 mg/kg twice daily (2.2)
- 6 Months to < 4 Years: 10 mg/kg twice daily; increase by 10 mg/kg twice daily every 2 weeks to recommended dose of 25 mg/kg twice daily (2.2)
- 4 Years to < 16 Years: 10 mg/kg twice daily; increase by 10 mg/kg twice daily every 2 weeks to recommended dose of 30 mg/kg twice daily (2.2)
- Adults 16 Years and Older: 500 mg twice daily; increase by 500 mg twice daily every 2 weeks to a recommended dose of 1500 mg twice daily (2.2)
Myoclonic Seizures in Adults and Pediatric Patients 12 Years and Older
- 500 mg twice daily; increase by 500 mg twice daily every 2 weeks to recommended dose of 1500 mg twice daily (2.3)
Primary Generalized Tonic-Clonic Seizures
- 6 Years to < 16 Years: 10 mg/kg twice daily, increase in increments of 10 mg/kg twice daily every 2 weeks to recommended dose of 30 mg/kg twice daily (2.4)
- Adults 16 Years and Older: 500 mg twice daily, increase by 500 mg twice daily every 2 weeks to recommended dose of 1500 mg twice daily (2.4)
Adult Patients with Impaired Renal Function
- Dose adjustment is recommended, based on the patient's estimated creatinine clearance (2.5, 8.6)
Dosage Forms and Strengths
- 250 mg, 500 mg, 750 mg, and 1000 mg film-coated, scored tablets (3)
- 100 mg/mL solution (3)
Contraindications
Known hypersensitivity to levetiracetam; angioedema and anaphylaxis have occurred (4, 5.4)
Warnings and Precautions
- Behavioral abnormalities including psychotic symptoms, suicidal ideation, irritability, and aggressive behavior have been observed; monitor patients for psychiatric signs and symptoms (5.1)
- Suicidal Behavior and Ideation: Monitor patients for new or worsening depression, suicidal thoughts/behavior, and/or unusual changes in mood or behavior (5.2)
- Monitor for somnolence and fatigue and advise patients not to drive or operate machinery until they have gained sufficient experience on KEPPRA (5.3)
- Serious Dermatological Reactions: Discontinue KEPPRA at the first sign of rash unless clearly not drug related (5.5)
- Coordination Difficulties: Monitor for ataxia, abnormal gait, and incoordination. Advise patients to not drive or operate machinery until they have gained experience on KEPPRA (5.6)
- Withdrawal Seizures: KEPPRA must be gradually withdrawn (5.7)
Adverse Reactions/Side Effects
Most common adverse reactions (incidence ≥ 5% more than placebo) include:
- Adult patients: somnolence, asthenia, infection and dizziness (6.1)
- Pediatric patients: fatigue, aggression, nasal congestion, decreased appetite, and irritability (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact UCB, Inc. at 1-844-599-2273 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Use In Specific Populations
Pregnancy: Plasma levels of levetiracetam may be decreased and therefore need to be monitored closely during pregnancy. Based on animal data, may cause fetal harm (5.10, 8.1)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 3/2023
Related/similar drugs
gabapentin, clonazepam, pregabalin, lamotrigine, diazepam, Lyrica, topiramateFull Prescribing Information
1. Indications and Usage for Keppra
1.1 Partial-Onset Seizures
KEPPRA is indicated for the treatment of partial-onset seizures in patients 1 month of age and older.
2. Keppra Dosage and Administration
2.1 Important Administration Instructions
KEPPRA is given orally with or without food. The KEPPRA dosing regimen depends on the indication, age group, dosage form (tablets or oral solution), and renal function.
Prescribe the oral solution for pediatric patients with body weight ≤ 20 kg. Prescribe the oral solution or tablets for pediatric patients with body weight above 20 kg.
When using the oral solution in pediatric patients, dosing is weight-based (mg per kg) using a calibrated measuring device (not a household teaspoon or tablespoon).
KEPPRA tablets should be swallowed whole. KEPPRA tablets should not be chewed or crushed.
2.2 Dosing for Partial-Onset Seizures
The recommended dosing for monotherapy and adjunctive therapy is the same; as outlined below.
2.3 Dosing for Myoclonic Seizures in Patients 12 Years of Age and Older with Juvenile Myoclonic Epilepsy
Initiate treatment with a dose of 1000 mg/day, given as twice-daily dosing (500 mg twice daily). Increase the dosage by 1000 mg/day every 2 weeks to the recommended daily dose of 3000 mg. The effectiveness of doses lower than 3000 mg/day has not been studied.
2.5 Dosage Adjustments in Adult Patients with Renal Impairment
KEPPRA dosing must be individualized according to the patient's renal function status. Recommended dosage adjustments for adults are shown in Table 1. In order to calculate the dose recommended for patients with renal impairment, creatinine clearance adjusted for body surface area must be calculated. To do this an estimate of the patient's creatinine clearance (CLcr) in mL/min must first be calculated using the following formula:
| CLcr= | [140-age (years)] × weight (kg) ---------------------------------------- 72 × serum creatinine (mg/dL) | (× 0.85 for female patients) |
Then CLcr is adjusted for body surface area (BSA) as follows:
| CLcr (mL/min/1.73m2)= | CLcr (mL/min) ------------------------------ BSA subject (m2) | × 1.73 |
| Group | Creatinine Clearance (mL/min/1.73m2) | Dosage (mg) | Frequency |
|---|---|---|---|
|
|||
| Normal | > 80 | 500 to 1,500 | Every 12 hours |
| Mild | 50 – 80 | 500 to 1,000 | Every 12 hours |
| Moderate | 30 – 50 | 250 to 750 | Every 12 hours |
| Severe | < 30 | 250 to 500 | Every 12 hours |
| ESRD patients using dialysis | ---- | 500 to 1,000* | Every 24 hours* |
4. Contraindications
KEPPRA is contraindicated in patients with a hypersensitivity to levetiracetam. Reactions have included anaphylaxis and angioedema [see Warnings and Precautions (5.4)].
5. Warnings and Precautions
5.1 Behavioral Abnormalities and Psychotic Symptoms
KEPPRA may cause behavioral abnormalities and psychotic symptoms. Patients treated with KEPPRA should be monitored for psychiatric signs and symptoms.
5.2 Suicidal Behavior and Ideation
Antiepileptic drugs (AEDs), including KEPPRA, increase the risk of suicidal thoughts or behavior in patients taking these drugs for any indication. Patients treated with any AED for any indication should be monitored for the emergence or worsening of depression, suicidal thoughts or behavior, and/or any unusual changes in mood or behavior.
Pooled analyses of 199 placebo-controlled clinical trials (mono- and adjunctive therapy) of 11 different AEDs showed that patients randomized to one of the AEDs had approximately twice the risk (adjusted Relative Risk 1.8, 95% CI:1.2, 2.7) of suicidal thinking or behavior compared to patients randomized to placebo. In these trials, which had a median treatment duration of 12 weeks, the estimated incidence rate of suicidal behavior or ideation among 27,863 AED-treated patients was 0.43%, compared to 0.24% among 16,029 placebo-treated patients, representing an increase of approximately one case of suicidal thinking or behavior for every 530 patients treated. There were four suicides in drug-treated patients in the trials and none in placebo-treated patients, but the number is too small to allow any conclusion about drug effect on suicide.
The increased risk of suicidal thoughts or behavior with AEDs was observed as early as one week after starting drug treatment with AEDs and persisted for the duration of treatment assessed. Because most trials included in the analysis did not extend beyond 24 weeks, the risk of suicidal thoughts or behavior beyond 24 weeks could not be assessed.
The risk of suicidal thoughts or behavior was generally consistent among drugs in the data analyzed. The finding of increased risk with AEDs of varying mechanisms of action and across a range of indications suggests that the risk applies to all AEDs used for any indication. The risk did not vary substantially by age (5-100 years) in the clinical trials analyzed. Table 2 shows absolute and relative risk by indication for all evaluated AEDs.
| Indication | Placebo Patients with Events Per 1000 Patients | Drug Patients with Events Per 1000 Patients | Relative Risk: Incidence of Events in Drug Patients/Incidence in Placebo Patients | Risk Difference: Additional Drug Patients with Events Per 1000 Patients |
|---|---|---|---|---|
| Epilepsy | 1.0 | 3.4 | 3.5 | 2.4 |
| Psychiatric | 5.7 | 8.5 | 1.5 | 2.9 |
| Other | 1.0 | 1.8 | 1.9 | 0.9 |
| Total | 2.4 | 4.3 | 1.8 | 1.9 |
The relative risk for suicidal thoughts or behavior was higher in clinical trials for epilepsy than in clinical trials for psychiatric or other conditions, but the absolute risk differences were similar for the epilepsy and psychiatric indications.
Anyone considering prescribing KEPPRA or any other AED must balance the risk of suicidal thoughts or behaviors with the risk of untreated illness. Epilepsy and many other illnesses for which AEDs are prescribed are themselves associated with morbidity and mortality and an increased risk of suicidal thoughts and behavior. Should suicidal thoughts and behavior emerge during treatment, the prescriber needs to consider whether the emergence of these symptoms in any given patient may be related to the illness being treated.
5.3 Somnolence and Fatigue
KEPPRA may cause somnolence and fatigue. Patients should be monitored for these signs and symptoms and advised not to drive or operate machinery until they have gained sufficient experience on KEPPRA to gauge whether it adversely affects their ability to drive or operate machinery.
5.4 Anaphylaxis and Angioedema
KEPPRA can cause anaphylaxis or angioedema after the first dose or at any time during treatment. Signs and symptoms in cases reported in the postmarketing setting have included hypotension, hives, rash, respiratory distress, and swelling of the face, lip, mouth, eye, tongue, throat, and feet. In some reported cases, reactions were life-threatening and required emergency treatment. If a patient develops signs or symptoms of anaphylaxis or angioedema, KEPPRA should be discontinued and the patient should seek immediate medical attention. KEPPRA should be discontinued permanently if a clear alternative etiology for the reaction cannot be established [see Contraindications (4)].
5.5 Serious Dermatological Reactions
Serious dermatological reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), have been reported in both pediatric and adult patients treated with KEPPRA. The median time of onset is reported to be 14 to 17 days, but cases have been reported at least four months after initiation of treatment. Recurrence of the serious skin reactions following rechallenge with KEPPRA has also been reported. KEPPRA should be discontinued at the first sign of a rash, unless the rash is clearly not drug-related. If signs or symptoms suggest SJS/TEN, use of this drug should not be resumed and alternative therapy should be considered.
5.6 Coordination Difficulties
KEPPRA may cause coordination difficulties.
In controlled clinical studies in adult patients with partial-onset seizure studies, 3.4% of adult KEPPRA-treated patients experienced coordination difficulties, (reported as either ataxia, abnormal gait, or incoordination) compared to 1.6% of placebo-treated patients. A total of 0.4% of patients in controlled clinical studies discontinued KEPPRA treatment due to ataxia, compared to 0% of placebo-treated patients. In 0.7% of KEPPRA-treated patients and in 0.2% of placebo-treated patients, the dose was reduced due to coordination difficulties, while one of the KEPPRA-treated patients was hospitalized due to worsening of pre-existing ataxia. These events occurred most frequently within the first 4 weeks of treatment.
Patients should be monitored for these signs and symptoms and advised not to drive or operate machinery until they have gained sufficient experience on KEPPRA to gauge whether it could adversely affect their ability to drive or operate machinery.
5.7 Withdrawal Seizures
As with most antiepileptic drugs, KEPPRA should generally be withdrawn gradually because of the risk of increased seizure frequency and status epilepticus. If withdrawal is needed because of a serious adverse reaction, rapid discontinuation can be considered.
5.8 Hematologic Abnormalities
KEPPRA can cause hematologic abnormalities. Hematologic abnormalities occurred in clinical trials and included decreases in white blood cell (WBC), neutrophil, and red blood cell (RBC) counts; decreases in hemoglobin and hematocrit; and increases in eosinophil counts. Cases of agranulocytosis, pancytopenia, and thrombocytopenia have been reported in the postmarketing setting. A complete blood count is recommended in patients experiencing significant weakness, pyrexia, recurrent infections, or coagulation disorders.
5.9 Increase in Blood Pressure
In a randomized, placebo-controlled study in patients 1 month to <4 years of age, a significantly higher risk of increased diastolic blood pressure was observed in the KEPPRA-treated patients (17%), compared to the placebo-treated patients (2%). There was no overall difference in mean diastolic blood pressure between the treatment groups. This disparity between the KEPPRA and placebo treatment groups was not observed in the studies of older children or in adults.
Monitor patients 1 month to <4 years of age for increases in diastolic blood pressure.
5.10 Seizure Control During Pregnancy
Physiological changes may gradually decrease plasma levels of levetiracetam throughout pregnancy. This decrease is more pronounced during the third trimester. It is recommended that patients be monitored carefully during pregnancy. Close monitoring should continue through the postpartum period especially if the dose was changed during pregnancy.
6. Adverse Reactions/Side Effects
The following adverse reactions are discussed in more details in other sections of labeling:
- Behavior Abnormalities and Psychotic Symptoms [see Warnings and Precautions (5.1)]
- Suicidal Behavior and Ideation [see Warnings and Precautions (5.2)]
- Somnolence and Fatigue [see Warnings and Precautions (5.3)]
- Anaphylaxis and Angioedema [see Warnings and Precautions (5.4)]
- Serious Dermatological Reactions [see Warnings and Precautions (5.5)]
- Coordination Difficulties [see Warnings and Precautions (5.6)]
- Hematologic Abnormalities [see Warnings and Precautions (5.8)]
- Increase in Blood Pressure [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Partial-Onset Seizures
Adults
In controlled clinical studies in adults with partial-onset seizures [see Clinical Studies (14.1)], the most common adverse reactions in patients receiving KEPPRA in combination with other AEDs, for events with rates greater than placebo, were somnolence, asthenia, infection, and dizziness. Of the most common adverse reactions in adults experiencing partial-onset seizures, asthenia, somnolence, and dizziness occurred predominantly during the first 4 weeks of treatment with KEPPRA.
Table 3 lists adverse reactions that occurred in at least 1% of adult epilepsy patients receiving KEPPRA in placebo-controlled studies and were numerically more common than in patients treated with placebo. In these studies, either KEPPRA or placebo was added to concurrent AED therapy.
| KEPPRA (N=769) % | Placebo (N=439) % |
|
|---|---|---|
| Asthenia | 15 | 9 |
| Somnolence | 15 | 8 |
| Headache | 14 | 13 |
| Infection | 13 | 8 |
| Dizziness | 9 | 4 |
| Pain | 7 | 6 |
| Pharyngitis | 6 | 4 |
| Depression | 4 | 2 |
| Nervousness | 4 | 2 |
| Rhinitis | 4 | 3 |
| Anorexia | 3 | 2 |
| Ataxia | 3 | 1 |
| Vertigo | 3 | 1 |
| Amnesia | 2 | 1 |
| Anxiety | 2 | 1 |
| Cough Increased | 2 | 1 |
| Diplopia | 2 | 1 |
| Emotional Lability | 2 | 0 |
| Hostility | 2 | 1 |
| Paresthesia | 2 | 1 |
| Sinusitis | 2 | 1 |
In controlled adult clinical studies, 15% of patients receiving KEPPRA and 12% receiving placebo either discontinued or had a dose reduction as a result of an adverse reaction. Table 4 lists the most common (>1%) adverse reactions that resulted in discontinuation or dose reduction and that occurred more frequently in KEPPRA-treated patients than in placebo-treated patients.
| Adverse Reaction | KEPPRA (N=769) % | Placebo (N=439) % |
|---|---|---|
| Somnolence | 4 | 2 |
| Dizziness | 1 | 0 |
Pediatric Patients 1 Month to < 4 Years
In the 7-day, controlled pediatric clinical study in children 1 month to less than 4 years of age with partial-onset seizures, the most common adverse reactions in patients receiving KEPPRA in combination with other AEDs, for events with rates greater than placebo, were somnolence and irritability. Because of the shorter exposure period, incidences of adverse reactions are expected to be lower than in other pediatric studies in older patients. Therefore, other controlled pediatric data, presented above, should also be considered to apply to this age group.
Table 6 lists adverse reactions that occurred in at least 5% of pediatric epilepsy patients (ages 1 month to < 4 years) treated with KEPPRA in the placebo-controlled study and were numerically more common than in patients treated with placebo. In this study, either KEPPRA or placebo was added to concurrent AED therapy.
| KEPPRA (N=60) % | Placebo (N=56) % |
|
|---|---|---|
| Somnolence | 13 | 2 |
| Irritability | 12 | 0 |
In the 7-day controlled pediatric clinical study in patients 1 month to < 4 years of age, 3% of patients receiving KEPPRA and 2% receiving placebo either discontinued or had a dose reduction as a result of an adverse reaction. There was no adverse reaction that resulted in discontinuation for more than one patient.
Myoclonic Seizures
Although the pattern of adverse reactions in this study seems somewhat different from that seen in patients with partial-onset seizures, this is likely due to the much smaller number of patients in this study compared to partial seizure studies. The adverse reaction pattern for patients with JME is expected to be essentially the same as for patients with partial seizures.
In the controlled clinical study in patients 12 years of age and older with myoclonic seizures [see Clinical Studies (14.2)], the most common adverse reactions in patients receiving KEPPRA in combination with other AEDs, for events with rates greater than placebo, were somnolence, neck pain, and pharyngitis.
Table 7 lists adverse reactions that occurred in at least 5% of juvenile myoclonic epilepsy patients experiencing myoclonic seizures treated with KEPPRA and were numerically more common than in patients treated with placebo. In this study, either KEPPRA or placebo was added to concurrent AED therapy.
| KEPPRA (N=60) % | Placebo (N=60) % |
|
|---|---|---|
| Somnolence | 12 | 2 |
| Neck pain | 8 | 2 |
| Pharyngitis | 7 | 0 |
| Depression | 5 | 2 |
| Influenza | 5 | 2 |
| Vertigo | 5 | 3 |
In the placebo-controlled study, 8% of patients receiving KEPPRA and 2% receiving placebo either discontinued or had a dose reduction as a result of an adverse reaction. The adverse reactions that led to discontinuation or dose reduction and that occurred more frequently in KEPPRA-treated patients than in placebo-treated patients are presented in Table 8.
| Adverse Reaction | KEPPRA (N=60) % | Placebo (N=60) % |
|---|---|---|
| Anxiety | 3 | 2 |
| Depressed mood | 2 | 0 |
| Depression | 2 | 0 |
| Diplopia | 2 | 0 |
| Hypersomnia | 2 | 0 |
| Insomnia | 2 | 0 |
| Irritability | 2 | 0 |
| Nervousness | 2 | 0 |
| Somnolence | 2 | 0 |
Primary Generalized Tonic-Clonic Seizures
Although the pattern of adverse reactions in this study seems somewhat different from that seen in patients with partial-onset seizures, this is likely due to the much smaller number of patients in this study compared to partial seizure studies. The adverse reaction pattern for patients with primary generalized tonic-clonic (PGTC) seizures is expected to be essentially the same as for patients with partial seizures.
In the controlled clinical study that included patients 4 years of age and older with PGTC seizures [see Clinical Studies (14.3)], the most common adverse reaction in patients receiving KEPPRA in combination with other AEDs, for events with rates greater than placebo, was nasopharyngitis.
Table 9 lists adverse reactions that occurred in at least 5% of idiopathic generalized epilepsy patients experiencing PGTC seizures treated with KEPPRA and were numerically more common than in patients treated with placebo. In this study, either KEPPRA or placebo was added to concurrent AED therapy.
| KEPPRA (N=79) % | Placebo (N=84) % |
|
|---|---|---|
| Nasopharyngitis | 14 | 5 |
| Fatigue | 10 | 8 |
| Diarrhea | 8 | 7 |
| Irritability | 6 | 2 |
| Mood swings | 5 | 1 |
In the placebo-controlled study, 5% of patients receiving KEPPRA and 8% receiving placebo either discontinued or had a dose reduction during the treatment period as a result of an adverse reaction.
This study was too small to adequately characterize the adverse reactions that could be expected to result in discontinuation of treatment in this population. It is expected that the adverse reactions that would lead to discontinuation in this population would be similar to those resulting in discontinuation in other epilepsy trials (see tables 4 and 8).
In addition, the following adverse reactions were seen in other controlled adult studies of KEPPRA: balance disorder, disturbance in attention, eczema, memory impairment, myalgia, and blurred vision.
6.2 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of KEPPRA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
The following adverse reactions have been reported in patients receiving marketed KEPPRA worldwide. The listing is alphabetized: abnormal liver function test, acute kidney injury, anaphylaxis, angioedema, agranulocytosis, choreoathetosis, drug reaction with eosinophilia and systemic symptoms (DRESS), dyskinesia, erythema multiforme, hepatic failure, hepatitis, hyponatremia, muscular weakness, pancreatitis, pancytopenia (with bone marrow suppression identified in some of these cases), panic attack, thrombocytopenia, weight loss, and worsening of seizures. Alopecia has been reported with KEPPRA use; recovery was observed in majority of cases where KEPPRA was discontinued.
8. Use In Specific Populations
8.1 Pregnancy
Data
Human Data
While available studies cannot definitively establish the absence of risk, data from the published literature and pregnancy registries have not established an association with levetiracetam use during pregnancy and major birth defects or miscarriage.
Animal Data
When levetiracetam (0, 400, 1200, or 3600 mg/kg/day) was administered orally to pregnant rats during the period of organogenesis, reduced fetal weights and increased incidence of fetal skeletal variations were observed at the highest dose tested. There was no evidence of maternal toxicity. The no-effect dose for adverse effects on embryofetal developmental in rats (1200 mg/kg/day) is approximately 4 times the maximum recommended human dose (MRHD) of 3000 mg on a body surface area (mg/m2) basis.
Oral administration of levetiracetam (0, 200, 600, or 1800 mg/kg/day) to pregnant rabbits during the period of organogenesis resulted in increased embryofetal mortality and incidence of fetal skeletal variations at the mid and high dose and decreased fetal weights and increased incidence of fetal malformations at the high dose, which was associated with maternal toxicity. The no-effect dose for adverse effects on embryofetal development in rabbits (200 mg/kg/day) is approximately equivalent to the MRHD on a mg/m2 basis.
Oral administration of levetiracetam (0, 70, 350, or 1800 mg/kg/day) to female rats throughout pregnancy and lactation led to an increased incidence of fetal skeletal variations, reduced fetal body weight, and decreased growth in offspring at the mid and high doses and increased pup mortality and neurobehavioral alterations in offspring at the highest dose tested. There was no evidence of maternal toxicity. The no-effect dose for adverse effects on pre- and postnatal development in rats (70 mg/kg/day) is less than the MRHD on a mg/m2 basis.
Oral administration of levetiracetam to rats during the latter part of gestation and throughout lactation produced no adverse developmental or maternal effects at doses of up to 1800 mg/kg/day (6 times the MRHD on a mg/m2 basis).
8.4 Pediatric Use
The safety and effectiveness of KEPPRA for the treatment of partial-onset seizures in patients 1 month to 16 years of age have been established [see Clinical Pharmacology (12.3) and Clinical Studies (14.1)]. The dosing recommendation in these pediatric patients varies according to age group and is weight-based [see Dosage and Administration (2.2)].
The safety and effectiveness of KEPPRA as adjunctive therapy for the treatment of myoclonic seizures in adolescents 12 years of age and older with juvenile myoclonic epilepsy have been established [see Clinical Studies (14.2)].
The safety and effectiveness of KEPPRA as adjunctive therapy for the treatment of primary generalized tonic-clonic seizures in pediatric patients 6 years of age and older with idiopathic generalized epilepsy have been established [see Clinical Studies (14.3)].
Safety and effectiveness for the treatment of partial-onset seizures in pediatric patients below the age of 1 month; adjunctive therapy for the treatment of myoclonic seizures in pediatric patients below the age of 12 years; and adjunctive therapy for the treatment of primary generalized tonic-clonic seizures in pediatric patients below the age of 6 years have not been established.
A 3-month, randomized, double-blind, placebo-controlled study was performed to assess the neurocognitive and behavioral effects of KEPPRA as adjunctive therapy in 98 (KEPPRA N=64, placebo N=34) pediatric patients, ages 4 to 16 years old, with partial seizures that were inadequately controlled. The target dose was 60 mg/kg/day. Neurocognitive effects were measured by the Leiter-R Attention and Memory (AM) Battery, which measures various aspects of a child's memory and attention. Although no substantive differences were observed between the placebo and drug treated groups in the median change from baseline in this battery, the study was not adequate to assess formal statistical non-inferiority of the drug and placebo. The Achenbach Child Behavior Checklist (CBCL/6-18), a standardized validated tool used to assess a child's competencies and behavioral/emotional problems, was also assessed in this study. An analysis of the CBCL/6-18 indicated on average a worsening in KEPPRA-treated patients in aggressive behavior, one of the eight syndrome scores [see Warnings and Precautions (5.1)].
8.5 Geriatric Use
There were 347 subjects in clinical studies of KEPPRA that were 65 and over. No overall differences in safety were observed between these subjects and younger subjects. There were insufficient numbers of elderly subjects in controlled trials of epilepsy to adequately assess the effectiveness of KEPPRA in these patients.
Levetiracetam is known to be substantially excreted by the kidney, and the risk of adverse reactions to this drug may be greater in patients with impaired renal function. Because elderly patients are more likely to have decreased renal function, care should be taken in dose selection, and it may be useful to monitor renal function [see Clinical Pharmacology (12.3)].
8.6 Renal Impairment
Clearance of levetiracetam is decreased in patients with renal impairment and is correlated with creatinine clearance [see Clinical Pharmacology (12.3)]. Dose adjustment is recommended for patients with impaired renal function and supplemental doses should be given to patients after dialysis [see Dosage and Administration (2.5)].
10. Overdosage
10.1 Signs, Symptoms and Laboratory Findings of Acute Overdosage in Humans
The highest known dose of KEPPRA received in the clinical development program was 6000 mg/day. Other than drowsiness, there were no adverse reactions in the few known cases of overdose in clinical trials. Cases of somnolence, agitation, aggression, depressed level of consciousness, respiratory depression and coma were observed with KEPPRA overdoses in postmarketing use.
10.2 Management of Overdose
There is no specific antidote for overdose with KEPPRA. If indicated, elimination of unabsorbed drug should be attempted by emesis or gastric lavage; usual precautions should be observed to maintain airway. General supportive care of the patient is indicated including monitoring of vital signs and observation of the patient's clinical status. A Certified Poison Control Center should be contacted for up to date information on the management of overdose with KEPPRA.
10.3 Hemodialysis
Standard hemodialysis procedures result in significant clearance of levetiracetam (approximately 50% in 4 hours) and should be considered in cases of overdose. Although hemodialysis has not been performed in the few known cases of overdose, it may be indicated by the patient's clinical state or in patients with significant renal impairment.
11. Keppra Description
KEPPRA is an antiepileptic drug available as 250 mg (blue), 500 mg (yellow), 750 mg (orange), and 1000 mg (white) tablets and as a clear, colorless, grape-flavored liquid (100 mg/mL) for oral administration.
The chemical name of levetiracetam, a single enantiomer, is (-)-(S)-α-ethyl-2-oxo-1-pyrrolidine acetamide, its molecular formula is C8H14N2O2 and its molecular weight is 170.21. Levetiracetam is chemically unrelated to existing antiepileptic drugs (AEDs). It has the following structural formula:
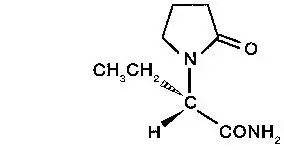
Levetiracetam is a white to off-white crystalline powder with a faint odor and a bitter taste. It is very soluble in water (104.0 g/100 mL). It is freely soluble in chloroform (65.3 g/100 mL) and in methanol (53.6 g/100 mL), soluble in ethanol (16.5 g/100 mL), sparingly soluble in acetonitrile (5.7 g/100 mL) and practically insoluble in n-hexane. (Solubility limits are expressed as g/100 mL solvent.)
KEPPRA tablets contain the labeled amount of levetiracetam. Inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, magnesium stearate, polyethylene glycol 3350, polyethylene glycol 6000, polyvinyl alcohol, talc, titanium dioxide, and additional agents listed below:
250 mg tablets: FD&C Blue #2/indigo carmine aluminum lake
500 mg tablets: iron oxide yellow
750 mg tablets: FD&C yellow #6/sunset yellow FCF aluminum lake, iron oxide red
KEPPRA oral solution contains 100 mg of levetiracetam per mL. Inactive ingredients: ammonium glycyrrhizinate, citric acid monohydrate, glycerin, maltitol solution, methylparaben, potassium acesulfame, propylparaben, purified water, sodium citrate dihydrate and natural and artificial flavor.
12. Keppra - Clinical Pharmacology
12.1 Mechanism of Action
The precise mechanism(s) by which levetiracetam exerts its antiepileptic effect is unknown.
A saturable and stereoselective neuronal binding site in rat brain tissue has been described for levetiracetam. Experimental data indicate that this binding site is the synaptic vesicle protein SV2A, thought to be involved in the regulation of vesicle exocytosis. Although the molecular significance of levetiracetam binding to SV2A is not understood, levetiracetam and related analogs showed a rank order of affinity for SV2A which correlated with the potency of their antiseizure activity in audiogenic seizure-prone mice. These findings suggest that the interaction of levetiracetam with the SV2A protein may contribute to the antiepileptic mechanism of action of the drug.
12.3 Pharmacokinetics
The pharmacokinetics of levetiracetam are similar when used as monotherapy or as adjunctive therapy for the treatment of partial-onset seizures.
14. Clinical Studies
14.1 Partial-Onset Seizures
Effectiveness in Partial-Onset Seizures in Adults
The effectiveness of KEPPRA for the treatment of partial-onset seizures in adults was established in three multicenter, randomized, double-blind, placebo-controlled clinical studies in patients who had refractory partial-onset seizures with or without secondary generalization. The tablet formulation was used in all these studies. In these studies, 904 patients were randomized to placebo, 1000 mg, 2000 mg, or 3000 mg/day. Patients enrolled in Study 1 or Study 2 had refractory partial-onset seizures for at least two years and had taken two or more classical AEDs. Patients enrolled in Study 3 had refractory partial-onset seizures for at least 1 year and had taken one classical AED. At the time of the study, patients were taking a stable dose regimen of at least one and could take a maximum of two AEDs. During the baseline period, patients had to have experienced at least two partial- onset seizures during each 4-week period.
Study 1
Study 1 was a double-blind, placebo-controlled, parallel-group study conducted at 41 sites in the United States comparing KEPPRA 1000 mg/day (N=97), KEPPRA 3000 mg/day (N=101), and placebo (N=95) given in equally divided doses twice daily. After a prospective baseline period of 12 weeks, patients were randomized to one of the three treatment groups described above. The 18-week treatment period consisted of a 6-week titration period, followed by a 12-week fixed dose evaluation period, during which concomitant AED regimens were held constant. The primary measure of effectiveness was a between group comparison of the percent reduction in weekly partial seizure frequency relative to placebo over the entire randomized treatment period (titration + evaluation period). Secondary outcome variables included the responder rate (incidence of patients with ≥50% reduction from baseline in partial-onset seizure frequency). The results of the analysis of Study 1 are displayed in Table 10.
| Placebo (N=95) | KEPPRA 1000 mg/day (N=97) | KEPPRA 3000 mg/day (N=101) |
|
|---|---|---|---|
|
|||
| Percent reduction in partial seizure frequency over placebo | – | 26.1%* | 30.1%* |
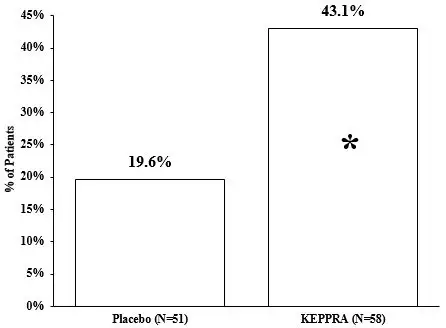
The percentage of patients (y-axis) who achieved ≥50% reduction in weekly seizure rates from baseline in partial-onset seizure frequency over the entire randomized treatment period (titration + evaluation period) within the three treatment groups (x-axis) is presented in Figure 1.
Figure 1: Responder Rate (≥50% Reduction from Baseline) in Study 1
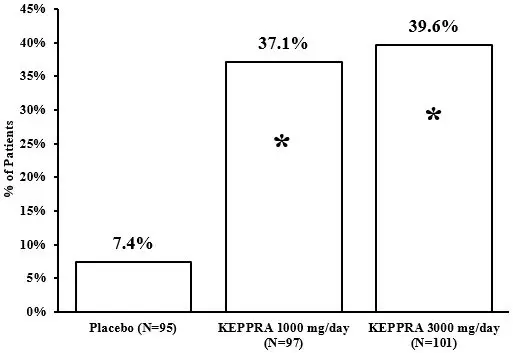
*statistically significant versus placebo
Study 2
Study 2 was a double-blind, placebo-controlled, crossover study conducted at 62 centers in Europe comparing KEPPRA 1000 mg/day (N=106), KEPPRA 2000 mg/day (N=105), and placebo (N=111) given in equally divided doses twice daily.
The first period of the study (Period A) was designed to be analyzed as a parallel-group study. After a prospective baseline period of up to 12 weeks, patients were randomized to one of the three treatment groups described above. The 16-week treatment period consisted of the 4-week titration period followed by a 12-week fixed dose evaluation period, during which concomitant AED regimens were held constant. The primary measure of effectiveness was a between group comparison of the percent reduction in weekly partial seizure frequency relative to placebo over the entire randomized treatment period (titration + evaluation period). Secondary outcome variables included the responder rate (incidence of patients with ≥50% reduction from baseline in partial-onset seizure frequency). The results of the analysis of Period A are displayed in Table 11.
| Placebo (N=111) | KEPPRA 1000 mg/day (N=106) | KEPPRA 2000 mg/day (N=105) |
|
|---|---|---|---|
|
|||
| Percent reduction in partial seizure frequency over placebo | – | 17.1%* | 21.4%* |
The percentage of patients (y-axis) who achieved ≥50% reduction in weekly seizure rates from baseline in partial-onset seizure frequency over the entire randomized treatment period (titration + evaluation period) within the three treatment groups (x-axis) is presented in Figure 2.
Figure 2: Responder Rate (≥50% Reduction from Baseline) in Study 2: Period A
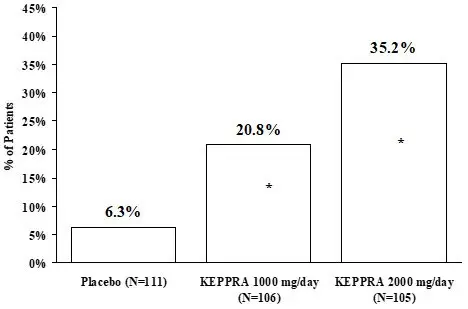
*statistically significant versus placebo
The comparison of KEPPRA 2000 mg/day to KEPPRA 1000 mg/day for responder rate was statistically significant (P=0.02). Analysis of the trial as a cross-over yielded similar results.
Study 3
Study 3 was a double-blind, placebo-controlled, parallel-group study conducted at 47 centers in Europe comparing KEPPRA 3000 mg/day (N=180) and placebo (N=104) in patients with refractory partial-onset seizures, with or without secondary generalization, receiving only one concomitant AED. Study drug was given in two divided doses. After a prospective baseline period of 12 weeks, patients were randomized to one of two treatment groups described above. The 16-week treatment period consisted of a 4-week titration period, followed by a 12-week fixed dose evaluation period, during which concomitant AED doses were held constant. The primary measure of effectiveness was a between group comparison of the percent reduction in weekly seizure frequency relative to placebo over the entire randomized treatment period (titration + evaluation period). Secondary outcome variables included the responder rate (incidence of patients with ≥50% reduction from baseline in partial-onset seizure frequency). Table 12 displays the results of the analysis of Study 3.
| Placebo (N=104) | KEPPRA 3000 mg/day (N=180) |
|
|---|---|---|
|
||
| Percent reduction in partial seizure frequency over placebo | – | 23.0%* |
The percentage of patients (y-axis) who achieved ≥50% reduction in weekly seizure rates from baseline in partial-onset seizure frequency over the entire randomized treatment period (titration + evaluation period) within the two treatment groups (x-axis) is presented in Figure 3.
Figure 3: Responder Rate (≥50% Reduction from Baseline) in Study 3
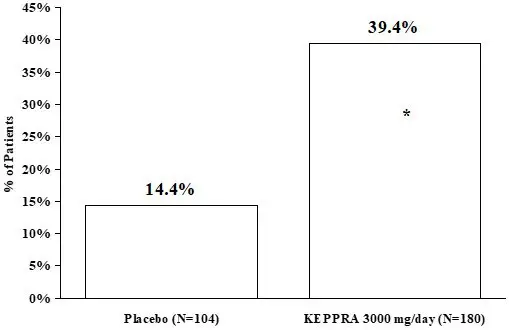
*statistically significant versus placebo
Effectiveness in Partial-Onset Seizures in Pediatric Patients 4 to 16 Years of Age
The effectiveness of KEPPRA for the treatment of partial-onset seizures in pediatric patients was established in one multicenter, randomized double-blind, placebo-controlled study (Study 4), conducted at 60 sites in North America, in pediatric patients 4 to 16 years of age with partial seizures uncontrolled by standard antiepileptic drugs (AEDs). Eligible patients on a stable dose of 1-2 AEDs, who still experienced at least 4 partial- onset seizures during the 4 weeks prior to screening, as well as at least 4 partial-onset seizures in each of the two 4-week baseline periods, were randomized to receive either KEPPRA or placebo. The enrolled population included 198 patients (KEPPRA N=101, placebo N=97) with refractory partial-onset seizures, whether or not secondarily generalized. The study consisted of an 8-week baseline period and 4-week titration period followed by a 10-week evaluation period. Dosing was initiated at a dose of 20 mg/kg/day in two divided doses. During the treatment period, KEPPRA doses were adjusted in 20 mg/kg/day increments, at 2-week intervals to the target dose of 60 mg/kg/day. The primary measure of effectiveness was a between group comparison of the percent reduction in weekly partial seizure frequency relative to placebo over the entire 14-week randomized treatment period (titration + evaluation period). Secondary outcome variables included the responder rate (incidence of patients with ≥ 50% reduction from baseline in partial-onset seizure frequency per week). Table 13 displays the results of this study.
| Placebo (N=97) | KEPPRA (N=101) |
|
|---|---|---|
|
||
| Percent reduction in partial seizure frequency over placebo | - | 26.8%* |
The percentage of patients (y-axis) who achieved ≥ 50% reduction in weekly seizure rates from baseline in partial-onset seizure frequency over the entire randomized treatment period (titration + evaluation period) within the two treatment groups (x-axis) is presented in Figure 4.
Figure 4: Responder Rate (≥ 50% Reduction from Baseline) in Study 4
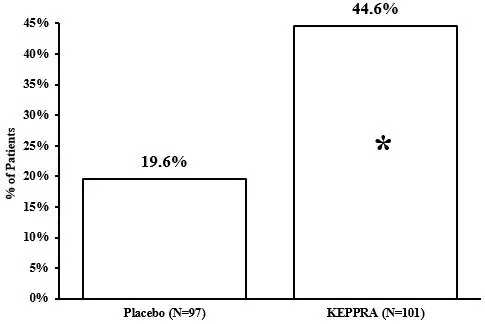
*statistically significant versus placebo
14.2 Myoclonic Seizures in Patients with Juvenile Myoclonic Epilepsy
The effectiveness of KEPPRA as adjunctive therapy in patients 12 years of age and older with juvenile myoclonic epilepsy (JME) experiencing myoclonic seizures was established in one multicenter, randomized, double-blind, placebo-controlled study (Study 6), conducted at 37 sites in 14 countries. Eligible patients on a stable dose of 1 antiepileptic drug (AED) experiencing one or more myoclonic seizures per day for at least 8 days during the prospective 8-week baseline period were randomized to either KEPPRA or placebo (KEPPRA N=60, placebo N=60). Patients were titrated over 4 weeks to a target dose of 3000 mg/day and treated at a stable dose of 3000 mg/day over 12 weeks (evaluation period). Study drug was given in 2 divided doses.
The primary measure of effectiveness was the proportion of patients with at least 50% reduction in the number of days per week with one or more myoclonic seizures during the treatment period (titration + evaluation periods) as compared to baseline. Of the 120 patients enrolled, 113 had a diagnosis of confirmed or suspected JME. Table 14 displays the results for the 113 patients with JME in this study.
| Placebo (N=59) | KEPPRA (N=54) |
|
|---|---|---|
|
||
| Percentage of responders | 23.7% | 60.4%* |
14.3 Primary Generalized Tonic-Clonic Seizures
The effectiveness of KEPPRA as adjunctive therapy in patients 6 years of age and older with idiopathic generalized epilepsy experiencing primary generalized tonic-clonic (PGTC) seizures was established in one multicenter, randomized, double-blind, placebo-controlled study (Study 7), conducted at 50 sites in 8 countries. Eligible patients on a stable dose of 1 or 2 antiepileptic drugs (AEDs) experiencing at least 3 PGTC seizures during the 8-week combined baseline period (at least one PGTC seizure during the 4 weeks prior to the prospective baseline period and at least one PGTC seizure during the 4-week prospective baseline period) were randomized to either KEPPRA or placebo. The 8-week combined baseline period is referred to as "baseline" in the remainder of this section. Patients were titrated over 4 weeks to a target dose of 3000 mg/day for adults or a pediatric target dose of 60 mg/kg/day and treated at a stable dose of 3000 mg/day (or 60 mg/kg/day for children) over 20 weeks (evaluation period). Study drug was given in 2 equally divided doses per day. The primary measure of effectiveness was the percent reduction from baseline in weekly PGTC seizure frequency for KEPPRA and placebo treatment groups over the treatment period (titration + evaluation periods). The population included 164 patients (KEPPRA N=80, placebo N=84) with idiopathic generalized epilepsy (predominately juvenile myoclonic epilepsy, juvenile absence epilepsy, childhood absence epilepsy, or epilepsy with Grand Mal seizures on awakening) experiencing primary generalized tonic-clonic seizures. Each of these syndromes of idiopathic generalized epilepsy was well represented in this patient population.
There was a statistically significant decrease from baseline in PGTC frequency in the KEPPRA-treated patients compared to the placebo-treated patients.
| Placebo (N=84) | KEPPRA (N=78) |
|
|---|---|---|
|
||
| Percent reduction in PGTC seizure frequency | 44.6% | 77.6%* |
The percentage of patients (y-axis) who achieved ≥50% reduction in weekly seizure rates from baseline in PGTC seizure frequency over the entire randomized treatment period (titration + evaluation period) within the two treatment groups (x-axis) is presented in Figure 6.
Figure 6: Responder Rate (≥50% Reduction from Baseline) in PGTC Seizure Frequency per Week in Study 7
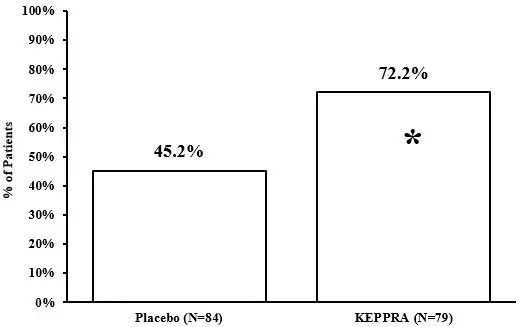
*statistically significant versus placebo
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide). The Medication Guide accompanies the product and can also be accessed on www.keppra.com or by calling 1-844-599-2273.
| This Medication Guide has been approved by the U.S. Food and Drug Administration. Revised: 1/2023 | ||
| MEDICATION GUIDE KEPPRA® (KEPP-ruh) (levetiracetam) tablets, for oral use, and oral solution |
||
| Read this Medication Guide before you start taking KEPPRA and each time you get a refill. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or treatment. | ||
| What is the most important information I should know about KEPPRA? Like other antiepileptic drugs, KEPPRA may cause suicidal thoughts or actions in a very small number of people, about 1 in 500 people taking it. Call a healthcare provider right away if you have any of these symptoms, especially if they are new, worse, or worry you:
|
||
| What is KEPPRA?
KEPPRA is a prescription medicine taken by mouth that is used to treat partial-onset seizures in people 1 month of age and older. KEPPRA is a prescription medicine taken by mouth that is used with other medicines to treat:
Before taking your medicine, make sure you have received the correct medicine. Compare the name above with the name on your bottle and the appearance of your medicine with the description of KEPPRA provided below. Tell your pharmacist immediately if you think you have been given the wrong medicine. |
||
| Who should not take KEPPRA?
Do not take KEPPRA if you are allergic to levetiracetam. |
||
| What should I tell my healthcare provider before starting KEPPRA?
Before taking KEPPRA, tell your healthcare provider about all of your medical conditions, including if you:
Know the medicines you take. Keep a list of them to show your healthcare provider and pharmacist each time you get a new medicine. |
||
How should I take KEPPRA?
|
||
| What should I avoid while taking KEPPRA?
Do not drive, operate machinery or do other dangerous activities until you know how KEPPRA affects you. KEPPRA may make you dizzy or sleepy. |
||
| What are the possible side effects of KEPPRA? KEPPRA can cause serious side effects including:
|
||
|
|
|
| The most common side effects seen in children who take KEPPRA include, in addition to those listed above include: | ||
|
|
|
| Tell your healthcare provider if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of KEPPRA. For more information, ask your healthcare provider or pharmacist. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||
How should I store KEPPRA?
|
||
| General information about the safe and effective use of KEPPRA.
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use KEPPRA for a condition for which it was not prescribed. Do not give KEPPRA to other people, even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or healthcare provider information about KEPPRA that is written for health professionals. |
||
| What are the ingredients in KEPPRA?
KEPPRA tablet active ingredient: levetiracetam Inactive ingredients: colloidal silicon dioxide, croscarmellose sodium, magnesium stearate, polyethylene glycol 3350, polyethylene glycol 6000, polyvinyl alcohol, talc, titanium dioxide, and additional agents listed below: 250 mg tablets: FD&C Blue #2/indigo carmine aluminum lake 500 mg tablets: iron oxide yellow 750 mg tablets: FD&C yellow #6/sunset yellow FCF aluminum lake, iron oxide red KEPPRA oral solution active ingredient: levetiracetam Inactive ingredients: ammonium glycyrrhizinate, citric acid monohydrate, glycerin, maltitol solution, methylparaben, potassium acesulfame, propylparaben, purified water, sodium citrate dihydrate and natural and artificial flavor. KEPPRA does not contain lactose or gluten. KEPPRA oral solution does contain carbohydrates. The liquid is dye-free. Distributed by UCB, Inc. Smyrna, GA 30080 KEPPRA is a registered trademark of the UCB Group of companies © 2023, UCB, Inc., Smyrna, GA 30080 All rights reserved. For more information, go to www.keppra.com or call 1-844-599-2273. |
||
| KEPPRA
levetiracetam tablet, film coated |
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
| KEPPRA
levetiracetam tablet, film coated |
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
|
||||||||||||||||||||||
| KEPPRA
levetiracetam tablet, film coated |
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
|
||||||||||||||||||||||||||
| KEPPRA
levetiracetam tablet, film coated |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| KEPPRA
levetiracetam solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - UCB, Inc. (028526403) |