Drug Detail:Kymriah (Tisagenlecleucel [ tis-a-jen-lek-loo-sel ])
Drug Class: Miscellaneous antineoplastics
Highlights of Prescribing Information
KYMRIAH® (tisagenlecleucel) suspension for intravenous infusion
Initial U.S. Approval: 2017
WARNING: CYTOKINE RELEASE SYNDROME and NEUROLOGICAL TOXICITIES
See full prescribing information for complete boxed warning.
- Cytokine Release Syndrome (CRS), including fatal or life-threatening reactions, occurred in patients receiving KYMRIAH. Do not administer KYMRIAH to patients with active infection or inflammatory disorders. Treat severe or life-threatening CRS with tocilizumab or tocilizumab and corticosteroids. (2.3, 2.4, 5.1)
- Neurological toxicities, which may be severe or life-threatening, can occur following treatment with KYMRIAH, including concurrently with CRS. Monitor for neurological events after treatment with KYMRIAH. Provide supportive care as needed. (5.2)
- KYMRIAH is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the KYMRIAH REMS. (5.3)
Recent Major Changes
| Indications and Usage, Adult Relapsed or Refractory (r/r) Follicular Lymphoma (FL) (1.3) | 5/2022 |
| Dosage and Administration Adult Relapsed or Refractory (r/r) Follicular Lymphoma (FL) (2.2, 2.3) | 5/2022 |
| Management of Severe Adverse Reactions (2.4) | 5/2022 |
| Warnings and Precautions (5.1, 5.2, 5.4, 5.6, 5.7, 5.8) | 5/2022 |
Indications and Usage for Kymriah
KYMRIAH is a CD19-directed genetically modified autologous T-cell immunotherapy indicated for the treatment of:
- Patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse. (1.1)
- Adult patients with relapsed or refractory (r/r) large B-cell lymphoma after two or more lines of systemic therapy, including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma and DLBCL arising from follicular lymphoma.
Limitations of Use: KYMRIAH is not indicated for treatment of patients with primary central nervous system lymphoma. (1.2) - Adult patients with relapsed or refractory follicular lymphoma (FL) after two or more lines of systemic therapy. This indication is approved under accelerated approval based on response rate and duration of response. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trial(s). (1.3)
Kymriah Dosage and Administration
For autologous use only. For intravenous use only.
- Administer a lymphodepleting regimen if needed before infusion of KYMRIAH. (2.3)
- Do NOT use a leukodepleting filter. (2.3)
- Verify the patient’s identity prior to infusion. (2.3)
- Premedicate with acetaminophen and an H1-antihistamine. (2.3)
- Confirm availability of tocilizumab prior to infusion. (2.3, 5.1)
- Dosing of KYMRIAH is based on the number of chimeric antigen receptor (CAR)-positive viable T cells.
-
Pediatric and Young Adult B-cell ALL (up to 25 years of age)
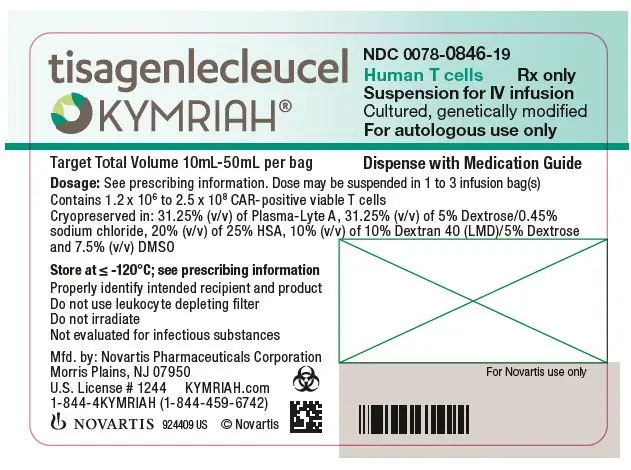
• For patients 50 kg or less, administer 0.2 to 5.0 x 106 CAR-positive viable T cells per kg body weight intravenously. (2.1)
• For patients above 50 kg, administer 0.1 to 2.5 x 108 total CAR-positive viable T cells (non-weight based) intravenously. (2.1)
-
Adult Relapsed or Refractory Diffuse Large B-cell Lymphoma and Follicular Lymphoma
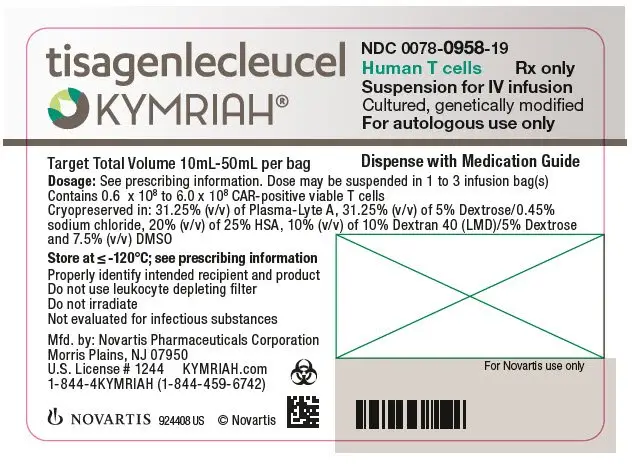
• Administer 0.6 to 6.0 x 108 CAR-positive viable T cells intravenously. (2.2)
Dosage Forms and Strengths
- Pediatric and Young Adult B-cell ALL (up to 25 years of age)
A single dose of KYMRIAH contains 0.2 to 5.0 x 106 CAR-positive viable T cells per kg of body weight for patients 50 kg or less, or 0.1 to 2.5 x 108 CAR-positive viable T cells for patients more than 50 kg, suspended in one to three patient-specific infusion bag(s) for intravenous infusion. (3)
- Adult Relapsed or Refractory Diffuse Large B-cell Lymphoma and Follicular Lymphoma
A single dose of KYMRIAH contains 0.6 to 6.0 x 108 CAR-positive viable T cells suspended in one to three patient-specific infusion bag(s) for intravenous infusion. (3)
Contraindications
None. (4)
Warnings and Precautions
-
Hypersensitivity Reactions: Monitor for hypersensitivity reactions during infusion. (5.5)
-
Serious Infections: Monitor patients for signs and symptoms of infection; treat appropriately. (5.6)
-
Prolonged Cytopenias: Patients may exhibit ≥ Grade 3 cytopenias for several weeks following KYMRIAH infusion. Prolonged neutropenia has been associated with increased risk of infection. (5.7)
-
Hypogammaglobulinemia: Monitor and provide replacement therapy until resolution. Assess immunoglobulin levels in newborns of mothers treated with KYMRIAH. (5.8)
-
Secondary Malignancies: In the event that a secondary malignancy occurs after treatment with KYMRIAH, contact Novartis Pharmaceuticals Corporation at 1-844-4KYMRIAH. (5.9)
- Effects on Ability to Drive and Use Machines: Advise patients to refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery, for at least 8 weeks after receiving KYMRIAH. (5.10)
Adverse Reactions/Side Effects
Pediatric and Young Adult B-cell ALL (up to 25 years of age): The most common adverse reactions (incidence greater than 20%) are cytokine release syndrome, infections-pathogen unspecified, hypogammaglobulinemia, fever, decreased appetite, viral infectious disorders, headache, febrile neutropenia, hemorrhage, musculoskeletal pain, vomiting, encephalopathy, diarrhea, hypotension, cough, nausea, bacterial infectious disorders, pain, hypoxia, tachycardia, edema, fatigue, and acute kidney injury. (6.1)
Adult Relapsed or Refractory Diffuse Large B-cell Lymphoma: The most common adverse reactions (incidence greater than 20%) are CRS, infections-pathogen unspecified, fever, diarrhea, nausea, fatigue, hypotension, edema, hemorrhage, dyspnea, and headache. (6.1)
Adult Relapsed or Refractory Follicular Lymphoma: The most common adverse reactions (incidence greater than 20%) are cytokine release syndrome, infections-pathogens unspecified, fatigue, musculoskeletal pain, headache, and diarrhea. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Novartis Pharmaceuticals Corporation at 1-888-669-6682 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 5/2022
Related/similar drugs
Blincyto, prednisone, methotrexate, rituximab, cyclophosphamide, Revlimid, RituxanFull Prescribing Information
1. Indications and Usage for Kymriah
KYMRIAH is a CD19-directed genetically modified autologous T cell immunotherapy indicated for the treatment of:
1.1 Pediatric and Young Adult Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)
Patients up to 25 years of age with B-cell precursor acute lymphoblastic leukemia (ALL) that is refractory or in second or later relapse.
1.2 Adult Relapsed or Refractory (r/r) Diffuse Large B-cell Lymphoma (DLBCL)
Adult patients with relapsed or refractory (r/r) large B-cell lymphoma after two or more lines of systemic therapy including diffuse large B-cell lymphoma (DLBCL) not otherwise specified, high grade B-cell lymphoma and DLBCL arising from follicular lymphoma.
Limitation of Use: KYMRIAH is not indicated for treatment of patients with primary central nervous system lymphoma.
1.3 Adult Relapsed or Refractory (r/r) Follicular Lymphoma (FL)
Adult patients with relapsed or refractory (r/r) follicular lymphoma (FL) after two or more lines of systemic therapy.
This indication is approved under accelerated approval based on response rate and duration of response [see Clinical Studies (14.3)]. Continued approval for this indication may be contingent upon verification and description of clinical benefit in confirmatory trial(s).
2. Kymriah Dosage and Administration
For autologous use only. For intravenous use only.
2.1 Dosage in Pediatric and Young Adult Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)
KYMRIAH is provided as a single-dose for infusion containing a suspension of chimeric antigen receptor (CAR)-positive viable T cells.
Based on the patient weight reported at the time of leukapheresis:
- Patients 50 kg or less: administer 0.2 to 5.0 x 106 CAR-positive viable T cells per kg body weight.
- Patients above 50 kg: administer 0.1 to 2.5 x 108 CAR-positive viable T cells.
2.2 Dosage in Adult Relapsed or Refractory (r/r) Diffuse Large B-cell Lymphoma (DLBCL) and Follicular Lymphoma (FL)
KYMRIAH is provided as a single-dose for infusion containing a suspension of chimeric antigen receptor (CAR)-positive viable T cells.
- For adult patients: administer 0.6 to 6.0 x 108 CAR-positive viable T cells.
2.3 Administration
Preparing Patient for KYMRIAH Administration with Lymphodepletion
- Confirm availability of KYMRIAH prior to starting the lymphodepleting regimen.
Pediatric and Young Adult Relapsed or Refractory (r/r) B-cell Acute Lymphoblastic Leukemia (ALL)
- Lymphodepleting chemotherapy: Fludarabine (30 mg/m2 intravenously daily for 4 days) and cyclophosphamide (500 mg/m2 intravenously daily for 2 days starting with the first dose of fludarabine).
- Infuse KYMRIAH 2 to 14 days after completion of the lymphodepleting chemotherapy.
Adult Relapsed or Refractory (r/r) Diffuse Large B-cell Lymphoma (DLBCL) and r/r Follicular Lymphoma (FL)
• Lymphodepleting chemotherapy: Fludarabine (25 mg/m2 intravenously daily for 3 days) and cyclophosphamide (250 mg/m2 intravenously daily for 3 days starting with the first dose of fludarabine).
• Alternate lymphodepleting chemotherapy: bendamustine 90 mg/m2 intravenously daily for 2 days if a patient experienced a previous Grade 4 hemorrhagic cystitis with cyclophosphamide or demonstrates resistance to a previous cyclophosphamide containing regimen.
• Infuse KYMRIAH 2 to 11 days (r/r DLBCL) or 2 to 6 days (r/r FL) after completion of the lymphodepleting chemotherapy.
• Lymphodepleting chemotherapy may be omitted if a patient is experiencing significant cytopenia, e.g., white blood cell (WBC) count is less than 1 x 109/L within 1 week prior to KYMRIAH infusion.
Preparation of KYMRIAH for Infusion and Administration
Delay the infusion of KYMRIAH if a patient has unresolved serious adverse reactions (including pulmonary reactions, cardiac reactions, or hypotension) from preceding chemotherapies, active uncontrolled infection, active graft versus host disease (GVHD), or worsening of leukemia burden following lymphodepleting chemotherapy [see Warnings and Precautions (5.1)].
A KYMRIAH dose may be contained in one to three cryopreserved patient specific infusion bag(s). Verify the number of bags received for the dose of KYMRIAH with the Certificate of Conformance (CoC) and Certificate of Analysis (CoA). Coordinate the timing of thaw of KYMRIAH and infusion in the following manner. Confirm the infusion time in advance, and adjust the start time for thaw so that KYMRIAH is available for infusion when the recipient is ready. If more than one bag has been received for the treatment dose, thaw 1 bag at a time. Wait to thaw/infuse the next bag until it is determined that the previous bag is safely administered.
Preparation of KYMRIAH for Infusion
1. Ensure tocilizumab and emergency equipment are available prior to infusion and during the recovery period.
2. Premedicate patient with acetaminophen and diphenhydramine or another H1-antihistamine approximately 30 to 60 minutes prior to KYMRIAH infusion. Avoid prophylactic use of systemic corticosteroids, as it may interfere with the activity of KYMRIAH.
3. Confirm patient identity: Prior to KYMRIAH preparation, match the patient's identity with the patient identifiers on each KYMRIAH infusion bag(s). KYMRIAH is for autologous use only. Employ universal precautions to avoid potential transmission of infectious diseases when handling the product.
Note: The patient identifier number may be preceded by the letters DIN or Aph ID.
Figure 1. KYMRIAH Infusion Bag
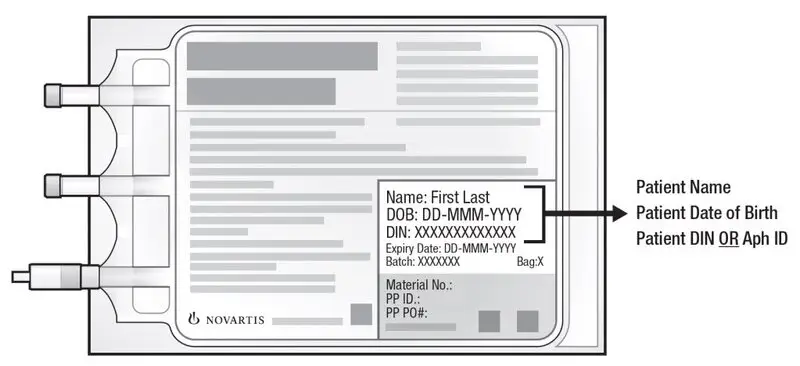
4. Inspect the infusion bag(s) for any breaks or cracks prior to thawing. If a bag is compromised, do not infuse the contents. Call Novartis at 1-844-4KYMRIAH.
5. Place the infusion bag inside a second, sterile bag in case of a leak and to protect ports from contamination.
6. Thaw each infusion bag one at a time at 37°C using either a water bath or dry thaw method until there is no visible ice in the infusion bag. Remove bag from thawing device immediately; do not store product bag at 37°C. Once the infusion bag has been thawed and is at room temperature (20°C to 25°C), it should be infused within 30 minutes. Do not wash, spin down, and/or resuspend KYMRIAH in new media prior to infusion.
7. Inspect the contents of the thawed infusion bag for any visible cell clumps. If visible cell clumps remain, gently mix the contents of the bag. Small clumps of cellular material should disperse with gentle manual mixing. Do not infuse KYMRIAH if clumps are not dispersed, the infusion bag is damaged or leaking, or otherwise appears to be compromised. Call Novartis at 1-844-4KYMRIAH.
Administration
8. Confirm the patient’s identity with the patient identifiers on the infusion bag.
9. Administer KYMRIAH as an intravenous infusion at 10 mL to 20 mL per minute, adjusted as appropriate for smaller children and smaller volumes. The volume in the infusion bag ranges from 10 mL to 50 mL. Do NOT use a leukocyte-depleting filter. If more than one bag is being infused for the treatment dose, wait to thaw/infuse the next bag until it is determined that the previous bag is safely administered.
- Prime the tubing prior to infusion with sodium chloride 9 mg/mL (0.9%) solution for injection.
- Infuse all contents of the infusion bag.
- Rinse the infusion bag with 10 mL to 30 mL sodium chloride 9 mg/mL (0.9%) solution for injection while maintaining a closed tubing system to assure as many cells as possible are infused into the patient.
- Cells from all the bag(s) must be infused to complete a single dose.
KYMRIAH contains human cells genetically modified with a lentivirus. Follow local biosafety guidelines applicable for handling and disposal of such products.
Monitoring
- Administer KYMRIAH at a REMS-certified healthcare facility.
- Monitor patients 2-3 times during the first week following KYMRIAH infusion at the certified healthcare facility for signs and symptoms of CRS and neurologic toxicities [see Warnings and Precautions (5.1, 5.2)].
- Instruct patients to remain within proximity of the certified healthcare facility for at least 4 weeks following infusion.
- Instruct patients to refrain from driving or hazardous activities for at least 8 weeks following infusion.
2.4 Management of Severe Adverse Reactions
Cytokine Release Syndrome
Identify cytokine release syndrome (CRS) based on clinical presentation [see Warnings and Precautions (5.1)]. Evaluate for and treat other causes of fever, hypoxia, and hypotension. If CRS is suspected, manage according to the recommendations in Table 1 (Lee et al 2014). Alternative CRS management strategies may be implemented based on appropriate institutional or academic guidelines.
| aLee et al. 2014.
bSantomasso et al. 2021. cRefer to tocilizumab Prescribing Information for details. dAlternative therapy includes anti-cytokine and anti-T cell therapies as per institutional policy and published guidelines such as (but not limited to) anakinra, siltuximab, ruxolitinib, cyclophosphamide, IVIG and ATG. |
|||
| CRS Grade a | Symptomatic treatment | Tocilizumab | Corticosteroids |
| Grade 1
Mild symptoms requiring symptomatic treatment only (e.g., low grade fever, fatigue, anorexia, etc.) | Exclude other causes (e.g., infection) and treat specific symptoms (e.g., with antipyretics, antiemetics, analgesics, etc.) | In patients with persistent (> 3 days) or refractory fever, consider managing as Grade 2 CRSb. | Not applicable |
| Grade 2
Symptoms require and respond to moderate intervention Oxygen requirement < 40% or Hypotension responsive to fluids or low dose of one vasopressor or Grade 2 organ toxicity | Antipyretics, oxygen, intravenous fluids and/or low dose vasopressors as needed. | Administer tocilizumabc intravenously over 1 hour: - 8 mg/kg (max. 800 mg) if body weight ≥ 30 kg - 12 mg/kg if body weight < 30 kg If no improvement after first dose, repeat every 8 hours (limit to a maximum of 3 dosages in 24 hours period; maximum total of 4 doses). | If no improvement within 24 hours of tocilizumab, administer a daily dose of 2 mg/kg/day methylprednisolone intravenously (or equivalent) until vasopressor and oxygen no longer needed, then taper. If not improving, manage as appropriate grade below. |
| Grade 3
Symptoms require and respond to aggressive intervention Oxygen requirement ≥ 40% or Hypotension requiring high dose or multiple vasopressors or Grade 3 organ toxicity or Grade 4 transaminitis | High-flow oxygen Intravenous fluids, and high-dose or multiple vasopressors Treat other organ toxicities as per local guidelines. | Per Grade 2 If not improving, consider alternative therapyd. | Per Grade 2 If not improving, manage as Grade 4. |
| Grade 4
Life-threatening symptoms Requirement for ventilator support or Grade 4 organ toxicity (excluding transaminitis) | Mechanical ventilation Intravenous fluids and high-dose vasopressor(s) Treat other organ toxicities as per local guidelines. | Per Grade 2 If not improving, consider alternative therapyd. | Administer methylprednisolone 1,000 mg intravenously one to two times per day for 3 days. If not improving, consider methylprednisolone 1,000 mg intravenously two to three times a day or alternate therapyd. Continue corticosteroids until improvement to Grade 1, and then taper as clinically appropriate. |
Neurologic Toxicities
Patients should be monitored for neurologic toxicities, including ICANS, following KYMRIAH infusion, particularly during and after resolution of CRS. Identify neurologic toxicities based on clinical presentation. Evaluate for and treat other causes of neurological symptoms. Consider non-sedating seizure prophylaxis (e.g., levetiracetam) for patients at higher risk of seizure, such as those with seizure history, CNS disease, concerning EEG findings, or neoplastic brain lesions. If neurologic toxicity is suspected, manage according to the recommendations in Table 2. Alternative neurologic toxicities management strategies may be implemented based on appropriate institutional, academic, or consensus guidelines.
| aASTCT criteria for grading NT (Lee et al. 2019); NCI CTCAE criteria for grading NT used in clinical trials.
bICE Assessment Tool: (1) Orientation: orientation to year, month, city, and hospital: 4 points. (2) Naming: ability to name three objects (e.g., point to clock, pen, and button): 3 points. (3) Following commands: ability to follow simple commands (e.g., show me 2 fingers or close your eyes and stick out your tongue): 1 point. (4) Writing: ability to write a standard sentence (e.g., Our national bird is the bald eagle): 1 point. (5) Attention: ability to count backward from 100 by 10: 1 point. cSantomasso et. al. 2021. dAlternate therapy may include anakinra, siltuximab, ruxolitinib, cyclophosphamide, antithymocyte globulin, or intrathecal hydrocortisone (50 mg) plus methotrexate (12 mg). *A patient with an ICE score of 0 may be classified as Grade 3 ICANS if awake with global aphasia, but a patient with an ICE score of 0 may be classified as Grade 4 ICANS if unarousable. |
||
| ICANS Gradea | No concurrent CRS | Concurrent CRS |
| Grade 1
ICE scoreb: 7-9 with no depressed level of consciousness | Offer supportive care with intravenous hydration and aspiration precautions. | Administer tocilizumab at any grade CRS, as per dosage recommendation in Table 1. Caution with repeated tocilizumab doses in patients with ICANS. Consider adding corticosteroids to tocilizumab past the first dose c. |
| Grade 2
ICE scoreb: 3-6 and/or Mild somnolence awaking to voice | Supportive care as above. Consider dexamethasone 10 mg intravenously every 6-12 hours or methylprednisolone equivalent (1 mg/kg intravenously every 12 hours) until the event is Grade 1 or less. If improving, taper corticosteroids. | Administer tocilizumab at any grade CRS, as per dosage recommendation in Table 1. If refractory to tocilizumab past the first dose, administer dexamethasone 10 mg intravenously every 6-12 hours or methylprednisolone equivalent (1 mg/kg intravenously every 12 hours) until the event is Grade 1 or less, then taper corticosteroids. |
| Grade 3
ICE scoreb: 0-2* and/or Depressed level of consciousness awakening only to tactile stimulus and/or Any clinical seizure focal or generalized that resolves rapidly or nonconvulsive seizures on EEG that resolve with intervention and/or Focal or local edema on neuroimaging | Administer dexamethasone 10 mg intravenously every 6-12 hours or methylprednisolone equivalent (1 mg/kg intravenously every 12 hours) | Administer tocilizumab at any grade CRS, as per dosage recommendation in Table 1. Administer dexamethasone 10 mg intravenously every 6-12 hours or methylprednisolone equivalent (1 mg/kg intravenously every 12 hours). Continue corticosteroids until the event is Grade 1 or less, then taper corticosteroids. If not improving, manage as Grade 4. |
| Grade 4
ICE scoreb: 0* (patient is unarousable and unable to perform ICE) and/or Stupor or coma and/or Life-threatening prolonged seizure (> 5 minutes) or repetitive clinical or electrical seizures without return to baseline in between and/or Diffuse cerebral edema on neuroimaging, decerebrate or decorticate posturing or papilledema, cranial nerve VI palsy, or Cushing’s triad | Consider mechanical ventilation for airway protection. Administer high-dose methylprednisolone intravenously 1,000 mg one to two times per day for 3 days. If not improving, consider 1,000 mg of methylprednisolone two to three times per day or alternate therapyd. Continue corticosteroids until improvement to Grade 1, and then taper as clinically appropriate. Treat seizures, status epilepticus, and cerebral edema as per institutional guidelines. | Administer tocilizumab at any grade CRS, as per dosage recommendation in Table 1. Administer methylprednisolone 1,000 mg intravenously one to two times per day for 3 days. If not improving, consider methylprednisolone 1,000 mg intravenously two to three times per day or alternate therapyd. Continue corticosteroids until improvement to Grade 1, and then taper as clinically appropriate. Treat seizures, status epilepticus, and cerebral edema as per institutional guidelines. |
3. Dosage Forms and Strengths
Pediatric and Young Adult r/r B-cell ALL (up to 25 years of age): A single dose of KYMRIAH contains 0.2 to 5.0 x 106 CAR-positive viable T cells per kg of body weight for patients 50 kg and below or 0.1 to 2.5 x 108 CAR-positive viable T cells for patients above 50 kg, suspended in one to three patient-specific infusion bag(s) [see How Supplied/Storage and Handling (16)].
Adult r/r DLBCL and r/r FL: A single dose of KYMRIAH contains 0.6 to 6.0 x 108 CAR-positive viable T cells, which may be suspended in one to three patient-specific infusion bag(s) [see How Supplied/Storage and Handling (16)].
See the CoA for actual cell count. The volume in the infusion bag ranges from 10 mL to 50 mL.
5. Warnings and Precautions
5.1 Cytokine Release Syndrome (CRS)
CRS, including fatal or life-threatening reactions, occurred following treatment with KYMRIAH. CRS occurred in 61 (77%) of the 79 pediatric and young adult patients with r/r ALL receiving KYMRIAH, including ≥ Grade 3 CRS (Penn grading system1) occurring in 48% of patients. The median times to onset and resolution of CRS were 3 days (range: 1-22; 1 patient with onset after Day 10) and 8 days (range: 1-36), respectively. Of the 61 patients with CRS, 31 (51%) received tocilizumab. Ten (16%) patients received two doses of tocilizumab and 3 (5%) patients received three doses of tocilizumab; 17 (28%) patients received addition of corticosteroids (e.g., methylprednisolone).
CRS occurred in 85 (74%) of the 115 adult patients with r/r DLBCL receiving KYMRIAH, including ≥ Grade 3 CRS (Penn grading system1) occurring in 23% of patients. The median times to onset and resolution of CRS were 3 days (range: 1-51; 1 patient with onset after Day 10) and 7 days (range: 2-30), respectively. Of the 85 patients with CRS, 19 (22%) received systemic tocilizumab or corticosteroids. Seven (8%) patients received a single dose of tocilizumab and 11 (13%) patients received two doses of tocilizumab; 11 (13%) patients received corticosteroids in addition to tocilizumab. One patient received corticosteroids for CRS without concomitant tocilizumab, and two patients received corticosteroids for persistent neurotoxicity after resolution of CRS.
CRS occurred in 51 (53%) of the 97 adult patients with r/r FL receiving KYMRIAH; all were Grade 1 or 2 CRS (Lee grading system2). The median times to onset and resolution of CRS were 4 days (range: 1-14) and 4 days (range: 1-13), respectively. Of the 51 patients with CRS, 15 (29%) received systemic anticytokine treatment with tocilizumab. Three (6%) patients required 3 dosages of tocilizumab, 4 (8%) patients required 2 dosages and 8 (16%) patients required single dose of tocilizumab. Two (4%) patients received corticosteroids in addition to tocilizumab.
Five deaths occurred within 30 days of KYMRIAH infusion. One patient with r/r ALL died with CRS and progressive leukemia, and one patient had resolving CRS with abdominal compartment syndrome, coagulopathy, and renal failure when an intracranial hemorrhage occurred. Of the 3 r/r DLBCL patients who died within 30 days of infusion, all had CRS in the setting of stable to progressive underlying disease, one of whom developed bowel necrosis.
Among patients with CRS, key manifestations include fever (93% in r/r ALL; 85% in r/r DLBCL; 92% in r/r FL), hypotension (69% in r/r ALL; 45% in r/r DLBCL; 40% in r/r FL), hypoxia (57% in r/r ALL; 35% in r/r DLBCL; 19% in r/r FL), and tachycardia (26% in r/r ALL; 13% in r/r DLBCL; 2% in r/r FL). CRS may be associated with hepatic, renal, and cardiac dysfunction, and coagulopathy.
Delay the infusion of KYMRIAH after lymphodepleting chemotherapy if the patient has unresolved serious adverse reactions from preceding chemotherapies (including pulmonary toxicity, cardiac toxicity, or hypotension), active uncontrolled infection, active graft versus host disease (GVHD), or worsening of leukemia burden [see Dosage and Administration (2.3)].
Risk factors for severe CRS in the pediatric and young adult r/r B-cell ALL population are high pre-infusion tumor burden (greater than 50% blasts in bone marrow), uncontrolled or accelerating tumor burden following lymphodepleting chemotherapy, active infections, and/or inflammatory processes.
Ensure that a minimum of two doses of tocilizumab are available on site prior to infusion of KYMRIAH.
Monitor patients 2-3 times during the first week following KYMRIAH infusion at the REMS-certified healthcare facility for signs and symptoms of CRS. Monitor patients for signs or symptoms of CRS for at least 4 weeks after treatment with KYMRIAH. At the first sign of CRS, immediately evaluate patient for hospitalization and institute treatment with supportive care, tocilizumab and/or corticosteroids as indicated [see Dosage and Administration (2.3, 2.4)].
Counsel patients to seek immediate medical attention should signs or symptoms of CRS occur at any time [see Patient Counseling Information (17)].
5.2 Neurological Toxicities
Neurological toxicities, including severe or life-threatening reactions, occurred following treatment with KYMRIAH. Neurologic toxicities occurred in 56 (71%) of the 79 patients with r/r ALL, including ≥ Grade 3 in 22%. The median times to the first event and duration were 6 days from infusion (range: 1-301) and 7 days, respectively.
Neurologic toxicities occurred in 69 (60%) of the 115 patients with r/r DLBCL, including ≥ Grade 3 in 19%. The median times to the first event and duration were 5 days (range: 1-368) and 17 days, respectively.
Neurologic toxicities occurred in 42 (43%) of the 97 patients with r/r FL, including ≥ Grade 3 in 6%. The median times to the first event and duration were 8 days (range: 1-345) and 5 days, respectively.
Among patients who had a neurological toxicity, 84% occurred within 8 weeks following KYMRIAH infusion. Resolution occurred within 3 weeks in 71% of patients with r/r ALL, 50% of patients with r/r DLBCL, and 74% of patients with r/r FL. Encephalopathy lasting up to 70 days was noted.
The onset of neurological toxicity can be concurrent with CRS, following resolution of CRS or in the absence of CRS.
The most common neurological toxicities observed with KYMRIAH include headache (35% in r/r ALL; 21% in r/r DLBCL; 25% in r/r FL), encephalopathy (30% in r/r ALL; 16% in r/r DLBCL; 3% in r/r FL), delirium (19% in r/r ALL; 5% in r/r DLBCL; 1% in r/r FL), anxiety (16% in r/r ALL; 10% in r/r DLBCL; 2% in r/r FL), sleep disorders (11% in r/r ALL; 10% in r/r DLBCL; 6% in r/r FL), dizziness (5% in r/r ALL; 12% in r/r DLBCL; 8% of r/r FL), tremor (8% in r/r ALL; 6% r/r DLBCL; 3% of r/r FL), and peripheral neuropathy (4% in r/r ALL; 12% in r/r DLBCL; 7% in r/r FL). Other manifestations included seizures and aphasia.
Monitor patients 2-3 times during the first week following KYMRIAH infusion at the REMS-certified healthcare facility for signs and symptoms of neurologic toxicities. Rule out other causes of neurological symptoms. Monitor patients for signs or symptoms of neurologic toxicities for at least 4 weeks after infusion and treat promptly. Neurologic toxicity should be managed with supportive care and/or corticosteroids as needed [see Dosage and Administration (2.3)].
Counsel patients to seek immediate medical attention should signs or symptoms of neurologic toxicity occur at any time [see Patient Counseling Information (17)].
5.3 KYMRIAH REMS to Mitigate Cytokine Release Syndrome and Neurological Toxicities
Because of the risk of CRS and neurological toxicities, KYMRIAH is available only through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS) called the KYMRIAH REMS [see Boxed Warning, Warnings and Precautions (5.1, 5.2)]. The required components of the KYMRIAH REMS are:
- Healthcare facilities that dispense and administer KYMRIAH must be enrolled and comply with the REMS requirements.
- Certified healthcare facilities must have on-site, immediate access to tocilizumab, and ensure that a minimum of two doses of tocilizumab are available for each patient for administration within 2 hours after KYMRIAH infusion, if needed for treatment of CRS.
- Certified healthcare facilities must ensure that healthcare providers who prescribe, dispense or administer KYMRIAH are trained about the management of CRS and neurological toxicities.
Further information is available at www.kymriah-rems.com or 1-844-4KYMRIAH.
5.4 Hemophagocytic Lymphohistiocytosis (HLH)/Macrophage Activation Syndrome (MAS)
Hemophagocytic Lymphohistiocytosis (HLH)/Macrophage Activation Syndrome (MAS), which can be life-threatening or fatal, has occurred following treatment with KYMRIAH. HLH was reported in 6% (5/79) of patients with r/r ALL (time to onset ranged from 3 to 18 days) and 2% (2/115) of patients with r/r DLBCL (times to onset were Day 7 and Day 10); all HLH events occurred during ongoing CRS and resolved. One patient (1%) with r/r FL developed HLH > 1 year after receiving KYMRIAH with a fatal outcome. The patient did not have CRS during or immediately preceding HLH. Treatment of HLH should be administered as per institutional standards.
5.5 Hypersensitivity Reactions
Allergic reactions may occur with infusion of KYMRIAH. Serious hypersensitivity reactions, including anaphylaxis, may be due to the DMSO or dextran 40 in KYMRIAH. Observe patients for hypersensitivity reactions during the infusion.
5.6 Serious Infections
Infections, including life-threatening or fatal infections, occurred following treatment with KYMRIAH. Infections occurred in 57 (72%) of the 79 patients with r/r ALL; 38 patients (48%) experienced ≥ Grade 3 infections, including fatal infections in 2 patients (3%).
Infections occurred in 67 (58%) of the 115 patients with r/r DLBCL; 38 patients (33%) experienced ≥ Grade 3 infections, including fatal infection in 1 patient (1%).
Infections occurred in 50 (52%) of the 97 patients with r/r FL; 20 patients (21%) experienced ≥ Grade 3 infections, including fatal infection in 1 patient (1%).
Prior to KYMRIAH infusion, infection prophylaxis should follow local guidelines. Patients with active uncontrolled infection should not start KYMRIAH treatment until the infection is resolved. Monitor patients for signs and symptoms of infection after treatment with KYMRIAH and treat appropriately [see Dosage and Administration (2.3)].
Febrile neutropenia (≥ Grade 3) was also observed in 34% of patients with r/r ALL, 17% of patients with r/r DLBCL, and 13% of patients with r/r FL after KYMRIAH infusion and may be concurrent with CRS. In the event of febrile neutropenia, evaluate for infection and manage with broad spectrum antibiotics, fluids and other supportive care as medically indicated.
Viral Reactivation
Hepatitis B virus (HBV) reactivation, in some cases resulting in fulminant hepatitis, hepatic failure and death, can occur in patients treated with drugs directed against B cells.
There is no experience with manufacturing KYMRIAH for patients with a positive test for HIV or with active HBV or active HCV. Perform screening for HBV, HCV, and HIV in accordance with clinical guidelines before collection of cells for manufacturing.
5.7 Prolonged Cytopenias
Patients may exhibit cytopenias for several weeks following lymphodepleting chemotherapy and KYMRIAH infusion.
In the ELIANA study (Study 1), ≥ Grade 3 cytopenias not resolved by Day 28 following KYMRIAH treatment included neutropenia (40%), and thrombocytopenia (27%) among 52 responding patients. At 56 days following KYMRIAH, 17% and 12% of responding patients had ≥ Grade 3 neutropenia or thrombocytopenia, respectively.
In the JULIET study (Study 2), ≥ Grade 3 cytopenias not resolved by Day 28 following KYMRIAH treatment included thrombocytopenia (39%) and neutropenia (25%) among 115 treated patients.
In the ELARA study (Study 3), ≥ Grade 3 cytopenias not resolved by Day 28 following KYMRIAH treatment included thrombocytopenia (17%) and neutropenia (16%) among 97 treated patients.
Prolonged neutropenia has been associated with increased risk of infection. Myeloid growth factors, particularly GM-CSF, are not recommended during the first 3 weeks after KYMRIAH infusion or until CRS has resolved.
5.8 Hypogammaglobulinemia
Hypogammaglobulinemia and agammaglobulinemia related to B-cell aplasia can occur in patients after KYMRIAH infusion.
Hypogammaglobulinemia was reported in 53% of patients treated with KYMRIAH for r/r ALL, 17% of patients with r/r DLBCL, and 18% of patients with r/r FL [see Clinical Pharmacology (12.3)].
Monitor immunoglobulin levels after treatment with KYMRIAH and manage using infection precautions, antibiotic prophylaxis, and immunoglobulin replacement standard guidelines.
Immunization with Live Vaccine
The safety of immunization with live vaccines during or following KYMRIAH treatment has not been studied. Vaccination with live vaccines is not recommended for at least 6 weeks prior to the start of lymphodepleting chemotherapy, during KYMRIAH treatment, and until immune recovery following treatment with KYMRIAH.
Pregnant women who have received KYMRIAH may have hypogammaglobulinemia. Assess immunoglobulin levels in newborns of mothers treated with KYMRIAH.
5.9 Secondary Malignancies
Patients treated with KYMRIAH may develop secondary malignancies or recurrence of their cancer. Monitor life-long for secondary malignancies. In the event that a secondary malignancy occurs, contact Novartis Pharmaceuticals Corporation at 1-844-4KYMRIAH to obtain instructions on patient samples to collect for testing.
5.10 Effects on Ability to Drive and Use Machines
Due to the potential for neurological events, including altered mental status or seizures, patients receiving KYMRIAH are at risk for altered or decreased consciousness or coordination in the 8 weeks following KYMRIAH infusion. Advise patients to refrain from driving and engaging in hazardous occupations or activities, such as operating heavy or potentially dangerous machinery, during this initial period.
6. Adverse Reactions/Side Effects
The following serious adverse reactions are discussed in greater detail in another section of the label:
- Cytokine Release Syndrome [see Warnings and Precautions (5.1)]
- Neurological Toxicities [see Warnings and Precautions (5.2)]
- Hemophagocytic Lymphohistiocytosis (HLH)/Macrophage Activation Syndrome (MAS) [see Warnings and Precautions (5.4)]
- Infections and Febrile Neutropenia [see Warnings and Precautions (5.6)]
- Prolonged Cytopenias [see Warnings and Precautions (5.7)]
- Hypogammaglobulinemia [see Warnings and Precautions (5.8)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety data described in the WARNINGS AND PRECAUTIONS and in this section reflect exposure to KYMRIAH in three non-randomized, single-arm studies in which 79 pediatric and young adult patients with relapsed/refractory (r/r) B-cell ALL (ELIANA Study), 115 adults with r/r diffuse large B-cell lymphoma (JULIET Study), and 97 adults with r/r follicular lymphoma (ELARA Study) received a single dose of CAR-positive viable T cells.
Pediatric and Young Adult r/r B-cell Acute Lymphoblastic Leukemia (ALL) (up to 25 years of age)
Based on a recommended dose which was weight-based, all 79 patients in the ELIANA study (Study 1) received a single intravenous dose of KYMRIAH [see Clinical Studies (14.1)]. The most common adverse reactions (> 20%) were cytokine release syndrome (77%), infections-pathogen unspecified (57%), hypogammaglobulinemia (53%), fever (42%), decreased appetite (38%), viral infectious disorders (38%), headache (35%), febrile neutropenia (34%), hemorrhage (32%), musculoskeletal pain (32%), vomiting (32%), encephalopathy (30%), bacterial infectious disorders (29%), diarrhea (29%), hypotension (29%), cough (27%), nausea (27%), pain (25%), hypoxia (25%), tachycardia (24%), edema (23%), fatigue (23%), and acute kidney injury (22%).
The adverse reactions with greater or equal to 10% incidence for any Grade are summarized in Table 3.
| aTachycardia includes sinus tachycardia and tachycardia.
bAbdominal pain includes abdominal pain, abdominal pain upper. cPain includes pain and pain in extremity. dFatigue includes fatigue and malaise. eEdema includes face edema, fluid overload, generalized edema, localized edema, edema peripheral. fHypogammaglobulinemia includes hypogammaglobulinemia, immunoglobulins decreased, blood immunoglobulin G decreased, blood immunoglobulin A decreased, blood immunoglobulin M decreased, immunodeficiency, immunodeficiency common variable. gHyperferritinemia includes serum ferritin increased. hMusculoskeletal pain includes back pain, bone pain, musculoskeletal chest pain, musculoskeletal pain, myalgia, neck pain, and non-cardiac chest pain. iHeadache includes headache and migraine. jEncephalopathy includes encephalopathy, cognitive disorder, confusional state, depressed level of consciousness, disturbance in attention, lethargy, mental status changes, somnolence, memory impairment, and automatism. Encephalopathy is a dominant feature of immune effector cell-associated neurotoxicity syndrome (ICANS), along with other symptoms. kDelirium includes delirium, agitation, hallucination, hallucination visual, irritability, restlessness. lSleep disorder includes sleep disorder, insomnia and nightmare. mAcute kidney injury includes acute kidney injury, anuria, azotemia, renal failure, renal tubular dysfunction, renal tubular necrosis, and blood creatinine increased. nCough includes cough and productive cough. oDyspnea includes acute respiratory failure, dyspnea, respiratory distress, and respiratory failure. pRash includes dermatitis, rash, rash maculo-papular, rash papular, and rash pruritic. qHemorrhage includes anal hemorrhage, catheter site hemorrhage, cerebral hemorrhage, conjunctival hemorrhage, contusion, cystitis hemorrhagic, disseminated intravascular coagulation, epistaxis, gastrointestinal hemorrhage, gingival bleeding, hemarthrosis, hematemesis, hematuria, hemoptysis, heavy menstrual bleeding, melena, mouth hemorrhage, peritoneal hematoma, petechiae, pharyngeal hemorrhage, purpura, retinal hemorrhage, vaginal hemorrhage. |
||
| Adverse Reaction | All Grades
(%) | Grades 3 or Higher
(%) |
| Blood and lymphatic system disorders | ||
| Febrile neutropenia | 34 | 34 |
| Cardiac disorders | ||
| Tachycardiaa | 24 | 4 |
| Gastrointestinal disorders | ||
| Vomiting | 32 | 1 |
| Diarrhea | 29 | 1 |
| Nausea | 27 | 3 |
| Abdominal painb | 18 | 3 |
| Constipation | 18 | 0 |
| General disorders and administration site conditions | ||
| Fever | 42 | 13 |
| Painc | 25 | 3 |
| Fatigued | 23 | 0 |
| Edemae | 23 | 8 |
| Immune system disorders | ||
| Cytokine release syndrome | 77 | 48 |
| Hypogammaglobulinemiaf | 53 | 13 |
| Infections and infestations | ||
| Infections-pathogen unspecified | 57 | 27 |
| Viral infectious disorders | 37 | 22 |
| Bacterial infectious disorders | 29 | 16 |
| Fungal infectious disorders | 15 | 9 |
| Metabolism and nutrition disorders | ||
| Decreased appetite | 38 | 15 |
| Hypocalcemia | 20 | 6 |
| Hyperferritinemiag | 10 | 3 |
| Musculoskeletal and connective tissue disorders | ||
| Musculoskeletal painh | 32 | 4 |
| Arthralgia | 14 | 1 |
| Nervous system disorders | ||
| Headachei | 35 | 3 |
| Encephalopathyj | 30 | 9 |
| Psychiatric disorders | ||
| Deliriumk | 19 | 4 |
| Anxiety | 17 | 3 |
| Sleep disorderl | 11 | 0 |
| Renal and urinary disorders | ||
| Acute kidney injurym | 22 | 14 |
| Respiratory, thoracic and mediastinal disorders | ||
| Coughn | 27 | 0 |
| Hypoxia | 25 | 20 |
| Dyspneao | 19 | 14 |
| Pulmonary edema | 15 | 9 |
| Nasal congestion | 11 | 0 |
| Oropharyngeal pain | 10 | 0 |
| Pleural effusion | 10 | 4 |
| Tachypnea | 10 | 5 |
| Skin and subcutaneous tissue disorders | ||
| Rashp | 18 | 1 |
| Vascular disorders | ||
| Hemorrhageq | 32 | 10 |
| Hypotension | 29 | 20 |
| Hypertension | 19 | 5 |
| aCardiac failure includes cardiac failure, cardiac failure congestive, left ventricular dysfunction, right ventricular dysfunction. bArrhythmia includes cardiac arrest. cSeizure includes generalized tonic-clonic seizure and seizure. dPeripheral neuropathy includes hyperasthesia, hypoasthesia, paresthesia. eSpeech disorder includes aphasia and dysarthria. fMotor dysfunction includes muscle spasms. |
| Additional important adverse reactions that did not meet the threshold criteria for inclusion in Table 3 were: |
| Blood and lymphatic system disorders: coagulopathy (6%), hemophagocytic lymphohistiocytosis (6%), pancytopenia (3%), |
| Cardiac disorders: cardiac failurea (9%), arrhythmiab (4%) |
| Eye disorders: visual impairment (3%) |
| Gastrointestinal disorders: abdominal distention (4%), ascites (4%), stomatitis (4%), abdominal compartment syndrome (1%), dry mouth (1%) |
| General disorders and administration site conditions: chills (9%), asthenia (4%), influenza-like illness (3%), multiple organ dysfunction syndrome (3%) |
| Immune system disorders: infusion related reaction (6%), graft versus host disease (3%) |
| Investigations: prothrombin time prolonged (4%), fibrin D dimer increased (3%), weight decreased (3%) |
| Metabolism and nutrition disorders: tumor lysis syndrome (6%), hypercalcemia (4%) |
| Nervous system disorders: tremor (8%), seizurec (6%), dizziness (5%), peripheral neuropathyd (4%), speech disordere (3%), motor dysfunctionf (1%), neuralgia (1%) |
| Respiratory, thoracic, and mediastinal disorders: acute respiratory distress syndrome (4%), lung infiltration (1%) |
| Skin and subcutaneous tissue disorders: pruritus (9%), erythema (6%), hyperhidrosis (4%), night sweats (1%) |
| Vascular disorders: capillary leak syndrome (3%), thrombosis (3%), flushing (1%) |
Laboratory Abnormalities
| aCTCAE = Common Terminology Criteria for Adverse Events version 4.03. | |
| Laboratory Abnormality | Grade 3 or 4 (%) |
| Hematology | |
| Blood fibrinogen decreased | 11 |
| Biochemistry | |
| Aspartate aminotransferase increased | 29 |
| Hypokalemia | 28 |
| Alanine aminotransferase increased | 22 |
| Hypophosphatemia | 20 |
| Hyperbilirubinemia | 19 |
| Hyperglycemia | 13 |
All patients experienced neutropenia, anemia and thrombocytopenia. See Table 5 for the incidences of ≥ Grade 3 prolonged thrombocytopenia and prolonged neutropenia in responding patients.
| a≥ Grade 3 observed within 14 days after Day 28 or Day 56 in responding patients. | ||
| Prolonged Cytopenia | N = 52 (%) | N = 52 (%) |
| Day 28 | Day 56 | |
| Prolonged neutropeniaa | 40 | 17 |
| Prolonged thrombocytopeniaa | 27 | 12 |
Adult r/r Diffuse Large B-cell Lymphoma (DLBCL)
In the JULIET study (Study 2) 115 adults with r/r DLBCL received a single intravenous dose of KYMRIAH [see Clinical Studies (14.2)]. The most common adverse reactions (incidence > 20%) were cytokine release syndrome, infections-pathogen unspecified, fever, diarrhea, nausea, fatigue, hypotension, edema, bleeding episodes, dyspnea, and headache.
The study population characteristics were: median age of 56 years (range: 22-76 years), 80% DLBCL; a median of 3 prior lines of therapy (range: 1-6), 49% had a prior autologous hematopoietic stem cell transplantation, and 32% had received prior radiation therapy. One hundred seven patients (93%) received lymphodepleting chemotherapy prior to KYMRIAH, that included fludarabine (n = 85) or bendamustine (n = 22).
The adverse reactions with greater than or equal to 10% incidence for any Grade are summarized in Table 6 below.
| aTachycardia includes sinus tachycardia and tachycardia.
bArrhythmia includes atrial fibrillation, cardiac arrest, supraventricular tachycardia, and ventricular extrasystoles. cAbdominal pain includes abdominal discomfort, abdominal pain, and abdominal pain upper. dFatigue includes fatigue and malaise. eEdema includes face edema, fluid overload, fluid retention, generalized edema, localized edema, edema peripheral, peripheral swelling. fPain includes pain and pain in extremity. gHypogammaglobulinemia includes blood immunoglobulin G decreased, immunodeficiency, immunoglobulins decreased and hypogammaglobulinemia. hMusculoskeletal pain includes back pain, flank pain, musculoskeletal chest pain, neck pain, and non-cardiac chest pain. iHeadache includes headache and migraine. jEncephalopathy includes cognitive disorder, confusional state, disturbance in attention, lethargy, mental status changes, somnolence, memory impairment, metabolic encephalopathy and thinking abnormal. Encephalopathy is a dominant feature of immune effector cell-associated neurotoxicity syndrome (ICANS), along with other symptoms. kPeripheral neuropathy includes paraesthesia, hypoaesthesia, hyperaesthesia, peripheral sensory neuropathy, neuropathy peripheral, cranial nerve paralysis, demyelinating polyneuropathy, Horner’s syndrome, polyneuropathy, and sciatica. lDizziness includes dizziness, presyncope, and syncope. mSleep disorder includes insomnia and sleep disorder. nAcute kidney injury includes acute kidney injury, blood creatinine abnormal, and blood creatinine increased. oDyspnea includes dyspnea, dyspnea exertional, respiratory distress, and respiratory failure. pCough includes cough, productive cough, and upper-airway cough syndrome. qRash includes dermatitis, dermatitis acneiform, dermatitis contact, rash, rash maculo-papular, rash papular, and rash pruritic. rHypotension includes hypotension and orthostatic hypotension. sHemorrhage includes anal hemorrhage, blood urine present, cerebral hemorrhage, contusion, cystitis hemorrhagic, disseminated intravascular coagulation, duodenal ulcer hemorrhage, epistaxis, eye contusion, gastrointestinal hemorrhage, hematemesis, hematochezia, hematuria, large intestinal hemorrhage, melena, mouth hemorrhage, petechiae, pharyngeal hemorrhage, post procedural hemorrhage, pulmonary hemorrhage, purpura, retinal hemorrhage, traumatic hematoma, tumor hemorrhage, upper gastrointestinal hemorrhage. |
||
| Adverse Reaction | All Grades
(%) | Grades 3 or Higher
(%) |
| Blood and lymphatic system disorders | ||
| Febrile neutropenia | 17 | 17 |
| Cardiac disorders | ||
| Tachycardiaa | 13 | 3 |
| Arrhythmiab | 10 | 5 |
| Gastrointestinal disorders | ||
| Diarrhea | 31 | 1 |
| Nausea | 29 | 1 |
| Constipation | 17 | 1 |
| Abdominal painc | 10 | 2 |
| General disorders and administration site conditions | ||
| Fever | 35 | 5 |
| Fatigued | 27 | 6 |
| Edemae | 27 | 3 |
| Painf | 14 | 3 |
| Chills | 12 | 0 |
| Immune system disorders | ||
| Cytokine release syndrome | 74 | 23 |
| Hypogammaglobulinemiag | 17 | 6 |
| Infections and infestations | ||
| Infections-pathogen unspecified | 48 | 26 |
| Bacterial infectious disorders | 17 | 8 |
| Fungal infectious disorders | 11 | 5 |
| Viral infectious disorders | 11 | 2 |
| Investigations | ||
| Weight decreased | 12 | 4 |
| Metabolism and nutrition disorders | ||
| Decreased appetite | 14 | 4 |
| Musculoskeletal and connective tissue disorders | ||
| Arthralgia | 14 | 0 |
| Musculoskeletal painh | 13 | 1 |
| Nervous system disorders | ||
| Headachei | 21 | 1 |
| Encephalopathyj | 16 | 11 |
| Peripheral neuropathyk | 12 | 3 |
| Dizzinessl | 12 | 2 |
| Psychiatric disorders | ||
| Anxiety | 10 | 1 |
| Sleep disorderm | 10 | 0 |
| Renal and urinary disorders | ||
| Acute kidney injuryn | 17 | 6 |
| Respiratory, thoracic and mediastinal disorders | ||
| Dyspneao | 21 | 6 |
| Coughp | 17 | 0 |
| Skin and subcutaneous tissue disorders | ||
| Rashq | 11 | 0 |
| Vascular disorders | ||
| Hypotensionr | 25 | 9 |
| Hemorrhages | 22 | 8 |
| aCardiac failure includes cardiac failure congestive.
bVisual impairment includes vision blurred and visual impairment. cHyperferritinemia includes serum ferritin increased. dMotor dysfunction includes muscle spasms, muscle twitching, myoclonus and myopathy. eTremor includes dyskinesia and tremor. fSpeech disorder includes speech disorder, aphasia, and dysarthria. gNeuralgia includes neuralgia and sciatica. hSeizure includes PTs seizure and status epilepticus. iAtaxia includes ataxia and dysmetria. jDelirium includes delirium, agitation, and irritability. kOropharyngeal pain includes oral pain and oropharyngeal pain. lPulmonary edema includes acute pulmonary edema and pulmonary edema. mThrombosis includes deep vein thrombosis, embolism, pulmonary embolism, thrombosis, vena cava thrombosis, and venous thrombosis. |
| Additional important adverse reactions that did not meet the threshold criteria for inclusion in Table 5 were: |
| Blood and lymphatic system disorders: pancytopenia (3%), hemophagocytic lymphohistiocytosis (2%), B-cell aplasia (1%) |
| Cardiac disorders: cardiac failurea (1%) |
| Eye disorders: visual impairmentb (6%) |
| Gastrointestinal disorders: vomiting (9%), stomatitis (6%), dry mouth (5%), abdominal distension (4%), ascites (3%) |
| General disorders and administration site conditions: influenza-like illness (9%), asthenia (7%), multiple organ dysfunction syndrome (3%) |
| Immune system disorders: infusion related reaction (3%) |
| Investigations: fibrin D dimer increased (4%) |
| Metabolism and nutrition disorders: hypocalcemia (5%), hypercalcemia (4%), hyperferritinemiac (4%), tumor lysis syndrome (2%) |
| Musculoskeletal and connective tissue disorders: myalgia (5%) |
| Nervous system disorders: motor dysfunctiond (6%), tremore (6%), speech disorderf (4%), neuralgiag (3%), seizureh (3%), ataxiai (2%), ischemic cerebral infarction (1%) |
| Psychiatric disorders: deliriumj (5%) |
| Respiratory, thoracic, and mediastinal disorders: hypoxia (8%), oropharyngeal paink (8%), pleural effusion (5%), nasal congestion (4%), pulmonary edemal (3%), tachypnea (3%) |
| Skin and subcutaneous tissue disorders: night sweats (5%), pruritus (4%), hyperhidrosis (4%), erythema (2%) |
| Vascular disorders: thrombosism (6%), hypertension (4%), capillary leak syndrome (1%) |
Laboratory Abnormalities
| aCTCAE = Common Terminology Criteria for Adverse Events version 4.03. | |
| Laboratory Parameter | Grade 3 or 4 (%) |
| Hematology | |
| Lymphopenia | 95 |
| Neutropenia | 82 |
| Leukopenia | 78 |
| Anemia | 59 |
| Thrombocytopenia | 56 |
| Biochemistry | |
| Hypophosphatemia | 24 |
| Hypokalemia | 13 |
Adult r/r Follicular Lymphoma (FL)
The safety of KYMRIAH was evaluated in the ELARA study (Study 3), a trial that included 97 patients with r/r FL who received a single intravenous dose of KYMRIAH [see Clinical Studies (14.3)]. Patients with a history of CNS disorders or autoimmune disease requiring systemic immunosuppression were ineligible. The median age was 57 years (range: 29 to 73 years), 34% were female, 75% were White, 13% were Asian, and 1% were Black or African American.
The most common adverse reactions (incidence > 20%) were cytokine release syndrome, infections-pathogen unspecified, fatigue, musculoskeletal pain, headache, and diarrhea.
The adverse reactions with greater than or equal to 10% incidence for any Grade are summarized in Table 8 below.
| aAbdominal pain includes abdominal pain and abdominal pain upper.
bFatigue includes asthenia, fatigue, and malaise. cHypogammaglobulinemia includes blood immunoglobulin G decreased and hypogammaglobulinemia. dMusculoskeletal pain includes back pain, bone pain, flank pain, muscle discomfort, musculoskeletal chest pain, musculoskeletal pain, myalgia, neck pain, and non-cardiac chest pain. eHeadache includes headache and migraine. fCough includes cough and productive cough. gRash includes rash, rash maculo-papular, and rash papular. |
||
| Adverse Reaction | All Grades
(%) | Grades 3 or Higher
(%) |
| Blood and lymphatic system disorders | ||
| Febrile neutropenia | 13 | 13 |
| Gastrointestinal disorders | ||
| Diarrhea | 24 | 2 |
| Nausea | 16 | 2 |
| Constipation | 16 | 0 |
| Abdominal paina | 10 | 1 |
| General disorders and administration site conditions | ||
| Fatigueb | 27 | 3 |
| Fever | 19 | 1 |
| Immune system disorders | ||
| Cytokine release syndrome | 53 | 0 |
| Hypogammaglobulinemiac | 18 | 1 |
| Infections and infestations | ||
| Infections-pathogen unspecified | 38 | 12 |
| Viral infectious disorders | 18 | 5 |
| Musculoskeletal and connective tissue disorders | ||
| Musculoskeletal paind | 25 | 1 |
| Arthralgia | 10 | 0 |
| Nervous system disorders | ||
| Headachee | 25 | 2 |
| Respiratory, thoracic and mediastinal disorders | ||
| Coughf | 19 | 0 |
| Skin and subcutaneous tissue disorders | ||
| Rashg | 10 | 0 |
| aHemolysis includes hemolysis and hemolytic anemia.
bCoagulopathy includes coagulopathy and international normalized ratio increased. cTachycardia includes sinus tachycardia. dArrhythmia includes atrial fibrillation, atrioventricular block first degree, and electrocardiogram QT prolonged. eVisual impairment includes blindness (preexisting progressive blindness, which initiated prior to start of lymphodepleting chemotherapy, further worsened after KYMRIAH infusion), vision blurred, and visual impairment. fStomatitis includes mouth ulceration and stomatitis. gEdema includes edema peripheral, fluid retention, hypervolemia, localized edema, and peripheral swelling. hPain includes ear pain, pain, and pain in extremity. iGraft versus host disease includes graft versus host disease in gastrointestinal tract and graft versus host disease in skin. jDizziness includes dizziness and syncope. kMotor dysfunction includes dyskinesia, muscle spasms, muscular weakness, musculoskeletal stiffness, and myoclonus. lPeripheral neuropathy includes dysesthesia, hypoesthesia, neuropathy peripheral, paresthesia, and peripheral sensory neuropathy. mSleep disorder includes insomnia. nAcute kidney injury includes acute kidney injury and blood creatinine increased. oDyspnea includes acute respiratory failure, dyspnea, and dyspnea exertional. pHypotension includes hypotension and orthostatic hypotension. qHemorrhage includes blood blister, catheter site hemorrhage, contusion, epistaxis, hematochezia, hematoma, mucosal hemorrhage, oral blood blister, petechiae, and purpura. rThrombosis includes deep vein thrombosis. |
| Additional important adverse reactions that did not meet the threshold criteria for inclusion in Table 8 were: |
| Blood and lymphatic system disorders: pancytopenia (3%), hemolysisa (2%), coagulopathyb (2%) |
| Cardiac disorders: tachycardiac (2%), arrhythmiad (4%) |
| Eye disorders: visual impairmente (4%) |
| Gastrointestinal disorders: vomiting (9%), stomatitisf (4%), abdominal distension (2%), dry mouth (2%) |
| General disorders and administration site conditions: edemag (9%), painh (8%), chills (6%) |
| Immune system disorders: infusion related reaction (3%), graft versus host diseasei (1%), hemophagocytic lymphohistiocytosis (1%) |
| Infections and infestations: bacterial infectious disorders (7%), fungal infectious disorders (2%) |
| Investigations: weight decreased (7%) |
| Metabolism and nutrition disorders: decreased appetite (8%), tumor lysis syndrome (2%) |
| Nervous system disorders: dizzinessj (8%), motor dysfunctionk (9%), peripheral neuropathyl (7%), immune effector cell-associated neurotoxicity syndrome (4%), encephalopathy (3%), tremor (3%) |
| Psychiatric disorders: sleep disorderm (6%), anxiety (2%), delirium (1%) |
| Renal and urinary disorder: acute kidney injuryn (4%) |
| Respiratory, thoracic, and mediastinal disorders: dyspneao (8%), pleural effusion (6%), oropharyngeal pain (5%), nasal congestion (2%), rhinorrhea (2%) |
| Skin and subcutaneous tissue disorders: pruritus (9%), night sweats (3%), erythema (2%), hyperhidrosis (1%) |
| Vascular disorders: hypotensionp (9%), hemorrhageq (6%), hypertension (5%), thrombosisr (1%) |
Laboratory Abnormalities
| aCTCAE = Common Terminology Criteria for Adverse Events version 4.03. *Evaluable population (n = 91 to 97) for each laboratory value included number of patients who had both baseline (before KYMRIAH infusion) and at least one post-KYMRIAH infusion on-study laboratory value available. |
|
| Laboratory Abnormality | Grade 3 or 4 (%) |
| Hematology | |
| Neutropenia | 63 |
| Leukopenia | 40 |
| Thrombocytopenia | 21 |
| Anemia | 20 |
| Lymphopenia | 19 |
| Biochemistry | |
| Hypophosphatemia | 12 |
| KYMRIAH
tisagenlecleucel injection, suspension |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| KYMRIAH
tisagenlecleucel injection, suspension |
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
|
|||||||||||||||
| Labeler - Novartis Pharmaceuticals Corporation (002147023) |