Drug Detail:Mavenclad (Cladribine (oral) [ klad-ri-been ])
Drug Class: Antimetabolites
Highlights of Prescribing Information
MAVENCLAD® (cladribine) tablets, for oral use
Initial U.S. Approval: 1993
WARNING: MALIGNANCIES and RISK OF TERATOGENICITY
See full prescribing information for complete boxed warning.
• Malignancies
MAVENCLAD may increase the risk of malignancy. MAVENCLAD is contraindicated in patients with current malignancy; evaluate the benefits and risks on an individual basis for patients with prior or increased risk of malignancy. (5.1)
• Risk of Teratogenicity
MAVENCLAD is contraindicated for use in pregnant women and in women and men of reproductive potential who do not plan to use effective contraception because of the risk of fetal harm. (5.2)
Recent Major Changes
| Dosage and Administration (2.1) | 9/2022 |
| Warnings and Precautions (5.4) | 9/2022 |
Indications and Usage for Mavenclad
MAVENCLAD is a purine antimetabolite indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include relapsing-remitting disease and active secondary progressive disease, in adults. Because of its safety profile, use of MAVENCLAD is generally recommended for patients who have had an inadequate response to, or are unable to tolerate, an alternate drug indicated for the treatment of MS [see Warnings and Precautions (5)]. (1)
Limitations of Use
MAVENCLAD is not recommended for use in patients with clinically isolated syndrome (CIS) because of its safety profile [see Warnings and Precautions (5)]. (1)
Mavenclad Dosage and Administration
- Assessments are required prior to starting each MAVENCLAD treatment course. (2.1)
- Cumulative dosage of 3.5 mg/kg administered orally and divided into 2 treatment courses (1.75 mg/kg per treatment course). Each treatment course is divided into 2 treatment cycles. (2.2)
- MAVENCLAD is a cytotoxic drug. (2.4)
- Separate administration from any other oral drug by at least 3 hours. (2.4)
Dosage Forms and Strengths
Tablets: 10 mg (3)
Contraindications
- Patients with current malignancy. (4)
- Pregnant women, and women and men of reproductive potential who do not plan to use effective contraception during MAVENCLAD dosing and for 6 months after the last dose in each treatment course. (4, 8.3)
- HIV infection. (4)
- Active chronic infections (e.g., hepatitis or tuberculosis). (4)
- History of hypersensitivity to cladribine. (4, 5.8)
- Women intending to breastfeed on a MAVENCLAD treatment day and for 10 days after the last dose. (4, 8.2)
Warnings and Precautions
- Lymphopenia: Monitor lymphocyte counts before, during and after treatment. (5.3)
- Infections: Screen patients for latent infections; consider delaying treatment until infection is fully controlled. Vaccination of patients seronegative to varicella zoster virus (VZV) is recommended prior to treatment. Vaccination of patients seropositive to VZV with zoster vaccine recombinant, adjuvanted, is recommended prior to or during treatment. Administer anti-herpes prophylaxis in patients with lymphocyte counts less than 200 cells per microliter. Monitor for infections. (5.4)
- Hematologic toxicity: Monitor complete blood count before, during and after treatment. (5.5)
- Graft-versus-host-disease with blood transfusion: Irradiation of cellular blood components is recommended. (5.6)
- Liver injury: Obtain tests prior to treatment. Discontinue if clinically significant injury is suspected. (5.7)
Adverse Reactions/Side Effects
Most common adverse reactions (incidence > 20%) are upper respiratory tract infection, headache, and lymphopenia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact EMD Serono at 1-800-283-8088 ext. 5563 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Immunosuppressive drugs: Consider overlapping effects on immune system, when used sequentially. Concomitant use not recommended. (7.1)
- Hematotoxic drugs: Monitor patients for additive effects on the hematological profile. (7.3)
- Antiviral and antiretroviral drugs: Avoid concomitant use. (7.4)
- BCRP or ENT/CNT inhibitors: May alter bioavailability of cladribine. Avoid concomitant use. (7.5)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 9/2022
Related/similar drugs
Ocrevus, Aubagio, Copaxone, Gilenya, Tecfidera, Tysabri, AvonexFull Prescribing Information
1. Indications and Usage for Mavenclad
MAVENCLAD is indicated for the treatment of relapsing forms of multiple sclerosis (MS), to include relapsing-remitting disease and active secondary progressive disease, in adults. Because of its safety profile, use of MAVENCLAD is generally recommended for patients who have had an inadequate response to, or are unable to tolerate, an alternate drug indicated for the treatment of MS [see Warnings and Precautions (5)].
2. Mavenclad Dosage and Administration
2.2 Recommended Dosage
The recommended cumulative dosage of MAVENCLAD is 3.5 mg per kg body weight administered orally and divided into 2 yearly treatment courses (1.75 mg per kg per treatment course) (see Table 1). Each treatment course is divided into 2 treatment cycles:
Administration of Second Treatment Course
- Second Course/First Cycle: administer at least 43 weeks after the last dose of First Course/Second Cycle.
- Second Course/Second Cycle: administer 23 to 27 days after the last dose of Second Course/First Cycle.
| Weight Range | Dose in mg (Number of 10 mg Tablets) per Cycle | |
|---|---|---|
| kg | First Cycle | Second Cycle |
|
||
| 40* to less than 50 | 40 mg (4 tablets) | 40 mg (4 tablets) |
| 50 to less than 60 | 50 mg (5 tablets) | 50 mg (5 tablets) |
| 60 to less than 70 | 60 mg (6 tablets) | 60 mg (6 tablets) |
| 70 to less than 80 | 70 mg (7 tablets) | 70 mg (7 tablets) |
| 80 to less than 90 | 80 mg (8 tablets) | 70 mg (7 tablets) |
| 90 to less than 100 | 90 mg (9 tablets) | 80 mg (8 tablets) |
| 100 to less than 110 | 100 mg (10 tablets) | 90 mg (9 tablets) |
| 110 and above | 100 mg (10 tablets) | 100 mg (10 tablets) |
Administer the cycle dosage as 1 or 2 tablets once daily over 4 or 5 consecutive days [see How Supplied/Storage and Handling (16.1)]. Do not administer more than 2 tablets daily.
Following the administration of 2 treatment courses, do not administer additional MAVENCLAD treatment during the next 2 years. Treatment during these 2 years may further increase the risk of malignancy [see Warnings and Precautions (5.1)]. The safety and efficacy of reinitiating MAVENCLAD more than 2 years after completing 2 treatment courses has not been studied.
2.3 Missed Dose
If a dose is missed, patients should not take double or extra doses.
If a dose is not taken on the scheduled day, then the patient must take the missed dose on the following day and extend the number of days in that treatment cycle. If two consecutive doses are missed, the treatment cycle is extended by 2 days.
2.4 Administration
MAVENCLAD tablets are taken orally, with water, and swallowed whole without chewing. MAVENCLAD can be taken with or without food.
Separate administration of MAVENCLAD and any other oral drugs by at least 3 hours during the 4 to 5 day MAVENCLAD treatment cycles [see Clinical Pharmacology (12.6)].
MAVENCLAD is a cytotoxic drug. Follow applicable special handling and disposal procedures [see References (15)]. MAVENCLAD is an uncoated tablet and must be swallowed immediately once removed from the blister. If a tablet is left on a surface, or if a broken or fragmented tablet is released from the blister, the area must be thoroughly washed with water.
The patient's hands must be dry when handling the tablets and washed thoroughly afterwards. Avoid prolonged contact with skin.
3. Dosage Forms and Strengths
MAVENCLAD is available as 10 mg tablets. The tablets are uncoated, white, round, biconvex, and engraved with a "C" on one side and "10" on the other side.
4. Contraindications
MAVENCLAD is contraindicated:
- in patients with current malignancy [see Warnings and Precautions (5.1)].
- in pregnant women and in women and men of reproductive potential who do not plan to use effective contraception during MAVENCLAD dosing and for 6 months after the last dose in each treatment course. May cause fetal harm [see Warnings and Precautions (5.2) and Use in Specific Populations (8.1, 8.3)].
- in patients infected with the human immunodeficiency virus (HIV) [see Warnings and Precautions (5.4)].
- in patients with active chronic infections (e.g., hepatitis or tuberculosis) [see Warnings and Precautions (5.4)].
- in patients with a history of hypersensitivity to cladribine [see Warnings and Precautions (5.8)].
- in women intending to breastfeed on a MAVENCLAD treatment day and for 10 days after the last dose [see Use in Specific Populations (8.2)].
5. Warnings and Precautions
5.1 Malignancies
Treatment with MAVENCLAD may increase the risk of malignancy. In controlled and extension clinical studies worldwide, malignancies occurred more frequently in MAVENCLAD-treated patients [10 events in 3,754 patient-years (0.27 events per 100 patient-years)], compared to placebo patients [3 events in 2,275 patient-years (0.13 events per 100 patient-years)]. Malignancy cases in MAVENCLAD patients included metastatic pancreatic carcinoma, malignant melanoma (2 cases), ovarian cancer, compared to malignancy cases in placebo patients, all of which were curable by surgical resection [basal cell carcinoma, cervical carcinoma in situ (2 cases)]. The incidence of malignancies in United States MAVENCLAD clinical study patients was higher than the rest of the world [4 events in 189 patient-years (2.21 events per 100 patient-years) compared to 0 events in United States placebo patients]; however, the United States results were based on a limited amount of patient data.
After the completion of 2 treatment courses, do not administer additional MAVENCLAD treatment during the next 2 years [see Dosage and Administration (2.2)]. In clinical studies, patients who received additional MAVENCLAD treatment within 2 years after the first 2 treatment courses had an increased incidence of malignancy [7 events in 790 patient-years (0.91 events per 100 patient-years) calculated from the start of cladribine treatment in Year 3]. The risk of malignancy with reinitiating MAVENCLAD more than 2 years after the completion of 2 treatment courses has not been studied.
MAVENCLAD is contraindicated in patients with current malignancy. In patients with prior malignancy or with increased risk of malignancy, evaluate the benefits and risks of the use of MAVENCLAD on an individual patient basis. Follow standard cancer screening guidelines in patients treated with MAVENCLAD.
5.2 Risk of Teratogenicity
MAVENCLAD may cause fetal harm when administered to pregnant women. Malformations and embryolethality occurred in animals [see Use in Specific Populations (8.1)]. Advise women of the potential risk to a fetus during MAVENCLAD dosing and for 6 months after the last dose in each treatment course.
In females of reproductive potential, pregnancy should be excluded before initiation of each treatment course of MAVENCLAD and prevented by the use of effective contraception during MAVENCLAD dosing and for at least 6 months after the last dose of each treatment course. Women who become pregnant during treatment with MAVENCLAD should discontinue treatment [see Use in Specific Populations (8.1, 8.3)]. MAVENCLAD is contraindicated for use in pregnant women and in women and men of reproductive potential who do not plan to use effective contraception.
5.3 Lymphopenia
MAVENCLAD causes a dose-dependent reduction in lymphocyte count. In clinical studies, 87% of MAVENCLAD-treated patients experienced lymphopenia. The lowest absolute lymphocyte counts occurred approximately 2 to 3 months after the start of each treatment course and were lower with each additional treatment course. In patients treated with a cumulative dose of MAVENCLAD 3.5 mg per kg over 2 courses as monotherapy, 26% and 1% had nadir absolute lymphocyte counts less than 500 and less than 200 cells per microliter, respectively. At the end of the second treatment course, 2% of clinical study patients had lymphocyte counts less than 500 cells per microliter; median time to recovery to at least 800 cells per microliter was approximately 28 weeks.
Additive hematological adverse reactions may be expected if MAVENCLAD is administered prior to or concomitantly with other drugs that affect the hematological profile [see Drug Interactions (7.3)]. The incidence of lymphopenia less than 500 cells per microliter was higher in patients who had used drugs to treat relapsing forms of MS prior to study entry (32.1%), compared to those with no prior use of these drugs (23.8%).
Obtain complete blood count (CBC) with differential including lymphocyte count prior to, during, and after treatment with MAVENCLAD. See Dosage and Administration (2.1, 2.5) and Warnings and Precautions (5.4) for timing of CBC measurements and additional instructions based on the patient's lymphocyte counts and clinical status (e.g., infections).
5.4 Infections
MAVENCLAD can reduce the body's immune defense and may increase the likelihood of infections. Infections occurred in 49% of MAVENCLAD-treated patients compared to 44% of placebo patients in clinical studies. The most frequent serious infections in MAVENCLAD- treated patients included herpes zoster and pyelonephritis (see Herpes Virus Infections). Fungal infections were observed, including cases of coccidioidomycosis.
HIV infection, active tuberculosis, and active hepatitis must be excluded before initiation of each treatment course of MAVENCLAD [see Contraindications (4)].
Consider a delay in initiation of MAVENCLAD in patients with an acute infection until the infection is fully controlled.
Initiation of MAVENCLAD in patients currently receiving immunosuppressive or myelosuppressive therapy is not recommended [see Drug Interactions (7.1)]. Concomitant use of MAVENCLAD with these therapies could increase the risk of immunosuppression.
Herpes Virus Infections
In controlled clinical studies, 6% of MAVENCLAD-treated patients developed a herpes viral infection compared to 2% of placebo patients. The most frequent types of herpes viral infections were herpes zoster infections (2.0% vs. 0.2%) and oral herpes (2.6% vs. 1.2%). Serious herpes zoster infections occurred in 0.2% of MAVENCLAD-treated patients.
Vaccination of patients who are seronegative for varicella zoster virus is recommended prior to initiation of MAVENCLAD. Administer live-attenuated or live vaccines at least 4 to 6 weeks prior to starting MAVENCLAD. Vaccination with zoster vaccine recombinant, adjuvanted is recommended for patients who are seropositive to VZV, either prior to or during MAVENCLAD treatment, including when their lymphocyte counts are less than or equal to 500 cells per microliter.
The incidence of herpes zoster was higher during the period of absolute lymphocyte count less than 500 cells per microliter, compared to the time when the patients were not experiencing this degree of lymphopenia. Administer anti-herpes prophylaxis in patients with lymphocyte counts less than 200 cells per microliter.
Patients with lymphocyte counts below 500 cells per microliter should be monitored for signs and symptoms suggestive of infections, including herpes infections. If such signs and symptoms occur, initiate treatment as clinically indicated. Consider interruption or delay of MAVENCLAD until resolution of the infection.
5.5 Hematologic Toxicity
In addition to lymphopenia [see Warnings and Precautions (5.3)], decreases in other blood cells and hematological parameters have been reported with MAVENCLAD in clinical studies. Mild to moderate decreases in neutrophil counts (cell count between 1,000 cells per microliter and < lower limit of normal (LLN)) were observed in 27% of MAVENCLAD-treated patients, compared to 13% of placebo patients whereas severe decreases in neutrophil counts (cell count below 1,000 cells per microliter) were observed in 3.6% of MAVENCLAD-treated patients, compared to 2.8% of placebo patients. Decreases in hemoglobin levels, in general mild to moderate (hemoglobin 8.0 g per dL to < LLN), were observed in 26% of MAVENCLAD-treated patients, compared to 19% of placebo patients. Decreases in platelet counts were generally mild (cell count 75,000 cells per microliter to < LLN) and were observed in 11% of MAVENCLAD-treated patients, compared to 4% of placebo patients.
In clinical studies at dosages similar to or higher than the approved MAVENCLAD dosage, serious cases of thrombocytopenia, neutropenia, and pancytopenia (some with documented bone marrow hypoplasia) requiring transfusion and granulocyte-colony stimulating factor treatment have been reported [see Warnings and Precautions (5.6) for information regarding graft-versus- host disease with blood transfusion].
Obtain complete blood count (CBC) with differential prior to, during, and after treatment with MAVENCLAD [see Dosage and Administration (2.1, 2.5)].
5.6 Graft-Versus-Host Disease With Blood Transfusion
Transfusion-associated graft-versus-host disease has been observed rarely after transfusion of nonirradiated blood in patients treated with cladribine for non-MS treatment indications.
In patients who require blood transfusion, irradiation of cellular blood components is recommended prior to administration to decrease the risk of transfusion-related graft-versus-host disease. Consultation with a hematologist is advised.
5.7 Liver Injury
In clinical studies, 0.3% of MAVENCLAD-treated patients had liver injury (serious or causing treatment discontinuation) considered related to treatment, compared to 0 placebo patients. Onset has ranged from a few weeks to several months after initiation of treatment with MAVENCLAD. Signs and symptoms of liver injury, including elevation of serum aminotransferases to greater than 20-fold the upper limit of normal, have been observed. These abnormalities resolved upon treatment discontinuation.
Obtain serum aminotransferase, alkaline phosphatase, and total bilirubin levels prior to the first and second treatment course [see Dosage and Administration (2.1)]. If a patient develops clinical signs, including unexplained liver enzyme elevations or symptoms suggestive of hepatic dysfunction (e.g., unexplained nausea, vomiting, abdominal pain, fatigue, anorexia, or jaundice and/or dark urine), promptly measure serum transaminases and total bilirubin and interrupt or discontinue treatment with MAVENCLAD, as appropriate.
5.8 Hypersensitivity
In clinical studies, 11% of MAVENCLAD-treated patients had hypersensitivity reactions, compared to 7% of placebo patients. Hypersensitivity reactions that were serious and/or led to discontinuation of MAVENCLAD (e.g., dermatitis, pruritis) occurred in 0.5% of MAVENCLAD-treated patients, compared to 0.1% of placebo patients. One patient had a serious hypersensitivity reaction with rash, mucous membrane ulceration, throat swelling, vertigo, diplopia, and headache after the first dose of MAVENCLAD.
If a hypersensitivity reaction is suspected, discontinue MAVENCLAD therapy. Do not use MAVENCLAD in patients with a history of hypersensitivity to cladribine [see Contraindications (4)].
5.9 Cardiac Failure
In clinical studies, one MAVENCLAD-treated patient experienced life-threatening acute cardiac failure with myocarditis, which improved after approximately one week. Cases of cardiac failure have also been reported with parenteral cladribine used for treatment indications other than multiple sclerosis.
Instruct patients to seek medical advice if they experience symptoms of cardiac failure (e.g., shortness of breath, rapid or irregular heartbeat, swelling).
6. Adverse Reactions/Side Effects
The following serious adverse reactions and potential risks are discussed, or discussed in greater detail, in other sections of the labeling:
- Malignancies [see Warnings and Precautions (5.1)]
- Risk of Teratogenicity [see Warnings and Precautions (5.2)]
- Lymphopenia [see Warnings and Precautions (5.3)]
- Infections [see Warnings and Precautions (5.4)]
- Hematologic Toxicity [see Warnings and Precautions (5.5)]
- Graft-Versus-Host Disease With Blood Transfusion [see Warnings and Precautions (5.6)]
- Liver Injury [see Warnings and Precautions (5.7)]
- Hypersensitivity [see Warnings and Precautions (5.8)]
- Cardiac Failure [see Warnings and Precautions (5.9)]
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
In the clinical trial program of cladribine in MS, 1,976 patients received cladribine for a total of 9,509 patient years. The mean time on study including follow-up was approximately 4.8 years, and approximately 24% of cladribine-treated patients had approximately 8 years of time on study including follow-up. Of these, 923 patients aged 18 to 66 years received MAVENCLAD as monotherapy at a cumulative dose of 3.5 mg per kg.
Table 2 shows adverse reactions in Study 1 [see Clinical Studies (14)] with an incidence of at least 5% for MAVENCLAD and higher than placebo. The most common (> 20%) adverse reactions reported in Study 1 are upper respiratory tract infection, headache, and lymphopenia.
| MAVENCLAD (N=440) % | Placebo (N=435) % |
|
|---|---|---|
| Upper respiratory tract infection | 38 | 32 |
| Headache | 25 | 19 |
| Lymphopenia | 24 | 2 |
| Nausea | 10 | 9 |
| Back pain | 8 | 6 |
| Arthralgia and arthritis | 7 | 5 |
| Insomnia | 6 | 4 |
| Bronchitis | 5 | 3 |
| Hypertension | 5 | 3 |
| Fever | 5 | 3 |
| Depression | 5 | 3 |
7. Drug Interactions
|
7.1 Immunomodulatory, Immunosuppressive, or Myelosuppressive Drugs |
|
| Clinical Impact | Concomitant use of MAVENCLAD with immunomodulatory, immunosuppressive, or myelosuppressive drugs may increase the risk of adverse reactions because of the additive effects on the immune system [see Warnings and Precautions (5.4)]. |
| Prevention or Management | Concomitant use with myelosuppressive or other immunosuppressive drugs is not recommended. Acute short-term therapy with corticosteroids can be administered. In patients who have previously been treated with immunomodulatory or immunosuppressive drugs, consider potential additive effect, the mode of action, and duration of effect of the other drugs prior to initiation of MAVENCLAD. |
| Clinical Impact | Concomitant use of MAVENCLAD with interferon-beta did not change the exposure of cladribine to a clinically significant effect; however, lymphopenia risk may be increased [see Warnings and Precautions (5.3)]. |
| Prevention or Management | Concomitant use is not recommended. |
| Clinical Impact | Concomitant use of MAVENCLAD with hematotoxic drugs may increase the risk of adverse reactions because of the additive hematological effects [see Warnings and Precautions (5.5)]. |
| Prevention or Management | Monitor hematological parameters. |
| Clinical Impact | Compounds that require intracellular phosphorylation to become active (e.g., lamivudine, zalcitabine, ribavirin, stavudine, and zidovudine) could interfere with the intracellular phosphorylation and activity of cladribine. |
| Prevention or Management | Avoid concomitant use. |
| Clinical Impact | Cladribine is a substrate of breast cancer resistance protein (BCRP), equilibrative nucleoside (ENT1), and concentrative nucleoside (CNT3) transport proteins. The bioavailability, intracellular distribution, and renal elimination of cladribine may be altered by potent ENT1, CNT3, and BCRP transporter inhibitors. |
| Prevention or Management | Avoid co-administration of potent ENT1, CNT3, or BCRP transporter inhibitors (e.g., ritonavir, eltrombopag, curcumin, cyclosporine, dilazep, nifedipine, nimodipine, cilostazol, sulindac, dipyridamole, or reserpine) during the 4 to 5 day MAVENCLAD treatment cycles. If this is not possible, consider selection of alternative concomitant drugs with no or minimal ENT1, CNT3, or BCRP transporter inhibiting properties. If this is not possible, dose reduction to the minimum mandatory dose of drugs containing these compounds, separation in the timing of administration, and careful patient monitoring is recommended. |
| Clinical Impact | Possible decrease in cladribine exposure if potent BCRP or P-gp transporter inducers are co-administered. |
| Prevention or Management | Consider a possible decrease in cladribine efficacy if potent BCRP (e.g., corticosteroids) or P-gp (e.g., rifampicin, St. John's Wort) transporter inducers are co-administered. |
| Clinical Impact | It is currently unknown whether MAVENCLAD may reduce the effectiveness of systemically acting hormonal contraceptives. |
| Prevention or Management | Women using systemically acting hormonal contraceptives should add a barrier method during MAVENCLAD dosing and for at least 4 weeks after the last dose in each treatment course. |
8. Use In Specific Populations
8.4 Pediatric Use
The safety and effectiveness in pediatric patients (below 18 years of age) have not been established. Use of MAVENCLAD is not recommended in pediatric patients because of the risk of malignancies [see Warnings and Precautions (5.1)].
8.5 Geriatric Use
Clinical studies with MAVENCLAD did not include sufficient numbers of patients aged 65 and over to determine whether they respond differently from younger patients. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. Caution is recommended when MAVENCLAD is used in elderly patients, taking into account the potential greater frequency of decreased hepatic, renal, or cardiac function, concomitant diseases, and other drug therapy.
8.6 Patients with Renal Impairment
The concentration of cladribine is predicted to increase in patients with renal impairment [see Clinical Pharmacology (12.3)]. No dosage adjustment is recommended in patients with mild renal impairment (creatinine clearance 60 to 89 mL per minute). MAVENCLAD is not recommended in patients with moderate to severe renal impairment (creatinine clearance below 60 mL per minute) [see Clinical Pharmacology (12.3)].
8.7 Patients with Hepatic Impairment
The effect of hepatic impairment on the pharmacokinetics of cladribine is unknown [see Clinical Pharmacology (12.3)]. No dosage adjustment is recommended in patients with mild hepatic impairment. MAVENCLAD is not recommended in patients with moderate to severe hepatic impairment (Child-Pugh score greater than 6) [see Clinical Pharmacology (12.3)].
10. Overdosage
There is no experience with overdose of MAVENCLAD. Lymphopenia is known to be dose- dependent. Particularly close monitoring of hematological parameters is recommended in patients who have been exposed to an overdose of MAVENCLAD [see Warnings and Precautions (5.3, 5.5)].
There is no known specific antidote to an overdose of MAVENCLAD. Treatment consists of careful observation and initiation of appropriate supportive measures. Discontinuation of MAVENCLAD may need to be considered. Because of the rapid and extensive intracellular and tissue distribution, hemodialysis is unlikely to eliminate cladribine to a significant extent.
11. Mavenclad Description
MAVENCLAD contains the nucleoside metabolic inhibitor cladribine, which is a white or almost white, non-hydroscopic, crystalline powder with the molecular formula C10H12ClN5O3 and molecular weight 285.69. It differs in structure from the naturally occurring nucleoside, deoxyadenosine, by the substitution of chlorine for hydrogen in the 2-position of the purine ring.
The chemical name of cladribine is 2-chloro-2′-deoxy-adenosine. The structural formula is shown below:
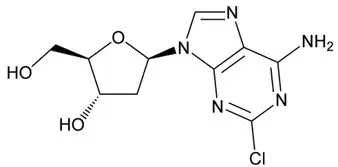
Cladribine is stable at slightly basic and at neutral pH. The main degradation pathway is hydrolysis and at acidic pH significant decomposition occurs with time. The ionization behavior of the molecule over the pH range 0 to 12 is characterized by a single pKa of approximately 1.21.
MAVENCLAD is provided as 10 mg tablets for oral use. Each MAVENCLAD 10 mg tablet contains cladribine as an active ingredient and hydroxypropyl betadex, magnesium stearate, and sorbitol as inactive ingredients.
12. Mavenclad - Clinical Pharmacology
12.1 Mechanism of Action
The mechanism by which cladribine exerts its therapeutic effects in patients with multiple sclerosis has not been fully elucidated but is thought to involve cytotoxic effects on B and T lymphocytes through impairment of DNA synthesis, resulting in depletion of lymphocytes.
12.2 Pharmacodynamics
MAVENCLAD causes a dose-dependent reduction in lymphocyte count. The lowest absolute lymphocyte counts occurred approximately 2 to 3 months after the start of each treatment cycle and were lower with each additional treatment cycle. At the end of Year 2, 2% of patients continued to have absolute lymphocyte counts less than 500 cells per microliter. The median time to recovery from lymphocyte counts less than 500 cells per microliter to at least 800 cells per microliter was approximately 28 weeks [see Warnings and Precautions (5.3)].
12.3 Pharmacokinetics
Cladribine is a prodrug that becomes active upon phosphorylation to its 2-chlorodeoxyadenosine triphosphate (Cd-ATP) metabolite.
The pharmacokinetic parameters presented below were assessed following oral administration of cladribine 10 mg, unless otherwise specified. The cladribine mean maximum concentration (Cmax) was in the range of 22 to 29 ng/ mL and corresponding mean AUC was in the range of 80 to 101 ng∙h/mL.
The Cmax and AUC of cladribine increased proportionally across a dose range from 3 to 20 mg.
No accumulation of cladribine concentration in plasma was observed after repeated dosing.
12.6 Hydroxypropyl Betadex-Related Complex Formation
MAVENCLAD contains hydroxypropyl betadex that may be available for complex formation with the active ingredients of other drugs. Complex formation between free hydroxypropyl betadex, released from the cladribine tablet formulation, and concomitant ibuprofen, furosemide, and gabapentin was observed. Concomitant use with MAVENCLAD may increase the bioavailability of other drugs (especially agents with low solubility), which may increase the risk or severity of adverse reactions [see Dosage and Administration (2.4)].
14. Clinical Studies
The efficacy of MAVENCLAD was demonstrated in a 96-week randomized, double-blind, placebo-controlled clinical study in patients with relapsing forms of MS (Study 1; NCT00213135).
Patients were required to have at least 1 relapse in the previous 12 months. The median age was 39 years (range 18 to 65) and the female-to-male ratio was approximately 2:1. The mean duration of MS prior to study enrollment was 8.7 years, and the median baseline neurological disability based on Kurtzke Expanded Disability Status Scale (EDSS) score across all treatment groups was 3.0. Over two thirds of the study patients were treatment-naive for drugs used to treat relapsing forms of MS.
1,326 patients were randomized to receive either placebo (n = 437), or a cumulative oral dosage of MAVENCLAD 3.5 mg per kg (n = 433) or 5.25 mg per kg body weight (n = 456) over the 96-week study period in 2 treatment courses. Patients randomized to the 3.5 mg per kg cumulative dose received a first treatment course at Weeks 1 and 5 of the first year and a second treatment course at Weeks 1 and 5 of the second year [see Dosage and Administration (2.2)]. Patients randomized to the 5.25 mg per kg cumulative dose received additional treatment at Weeks 9 and 13 of the first year. Higher cumulative doses did not add any clinically meaningful benefit, but were associated with a higher incidence in grade 3 lymphopenia or higher (44.9% in the 5.25 mg per kg group vs. 25.6% in the 3.5 mg per kg group). Ninety-two percent of patients treated with MAVENCLAD 3.5 mg per kg and 87% of patients receiving placebo completed the full 96 weeks of the study.
The primary outcome of Study 1 was the annualized relapse rate (ARR). Additional outcome measures included the proportion of patients with confirmed disability progression, the time to first qualifying relapse, the mean number of MRI T1 Gadolinium-enhancing (Gd+) lesions, and new or enlarging MRI T2 hyperintense lesions. Disability progression was measured in terms of a 3-month sustained change in EDSS score of at least one point, if baseline EDSS score was between 0.5 and 4.5 inclusively, or at least 1.5 points if the baseline EDSS score was 0, or at least 0.5 point if the baseline EDSS score was at least 5, over a period of at least 3 months.
MAVENCLAD 3.5 mg per kg significantly lowered the annualized relapse rate. The results from Study 1 are presented in Table 4.
| Endpoints | MAVENCLAD | Placebo |
|---|---|---|
| Cumulative Dose 3.5 mg per kg (n = 433) | (n = 437) | |
| HR: Hazard Ratio | ||
|
||
| Clinical Endpoints | ||
| Annualized relapse rate (ARR) | 0.14* | 0.33 |
| Relative reduction in ARR | 58% | |
| Proportion of patients without relapse | 81%† | 63% |
| Time to 3-month confirmed EDSS progression, HR | 0.67† | |
| Proportion of patients with 3-month EDSS progression | 13% | 19% |
| MRI Endpoints | ||
| Median Number of Active T1 Gd+ Lesions | 0* | 0.33 |
| Median Number of Active T2 Lesions | 0* | 0.67 |
16. How is Mavenclad supplied
16.1 How Supplied
MAVENCLAD tablets, 10 mg, are uncoated, white, round, biconvex, and engraved with a "C" on one side and "10" on the other side. Each tablet is packaged in a child-resistant day pack containing one or two tablets in a blister card.
Dispense one box for each treatment cycle with a Medication Guide [see Dosage and Administration (2.2)].
16.2 Storage and Handling
Store at controlled room temperature, 20°C to 25°C (68°F to 77°F); excursions permitted to 15°C to 30°C (59°F to 86°F) [see USP Controlled Room Temperature]. Store in original package in order to protect from moisture.
MAVENCLAD is a cytotoxic drug. Follow applicable special handling and disposal procedures [see References (15)].1
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Issued: 3/2019 | |||||
|
MEDICATION GUIDE
|
||||||
|
What is the most important information I should know about MAVENCLAD? MAVENCLAD can cause serious side effects, including:
|
||||||
|
What is MAVENCLAD? MAVENCLAD is a prescription medicine used to treat relapsing forms of multiple sclerosis (MS), to include relapsing-remitting disease and active secondary progressive disease, in adults. Because of its safety profile, MAVENCLAD is generally used in people who have tried another MS medicine that they could not tolerate or that has not worked well enough. MAVENCLAD is not recommended for use in people with clinically isolated syndrome (CIS). It is not known if MAVENCLAD is safe and effective in children under 18 years of age. |
||||||
|
||||||
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. |
||||||
|
How should I take MAVENCLAD?
Your healthcare provider will continue to monitor your health during the 2 yearly treatment courses, and for at least another 2 years during which you do not need to take MAVENCLAD. It is not known if MAVENCLAD is safe and effective in people who restart MAVENCLAD treatment more than 2 years after completing 2 yearly treatment courses. |
||||||
|
What are the possible side effects of MAVENCLAD? MAVENCLAD can cause serious side effects, including:
|
||||||
|
|
|||||
|
||||||
|
|
|||||
|
||||||
|
|
|||||
Your healthcare provider may delay or completely stop treatment with MAVENCLAD if you have severe side effects. The most common side effects of MAVENCLAD include: |
||||||
|
|
|
||||
|
These are not all the possible side effects of MAVENCLAD. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||||||
|
How should I store MAVENCLAD?
Keep MAVENCLAD and all medicines out of the reach of children. |
||||||
|
General information about the safe and effective use of MAVENCLAD Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use MAVENCLAD for a condition for which it was not prescribed. Do not give MAVENCLAD to other people, even if they have the same symptoms that you have. It may harm them. You can ask your healthcare provider for information about MAVENCLAD that is written for health professionals. |
||||||
|
What are the ingredients in MAVENCLAD? Active ingredient: cladribine Inactive ingredients: hydroxypropyl betadex, magnesium stearate, and sorbitol.
Distributed by: EMD Serono, Inc., Rockland, MA 02370 |
||||||
| MAVENCLAD
cladribine tablet |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| Labeler - EMD Serono, Inc. (088514898) |





