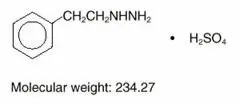
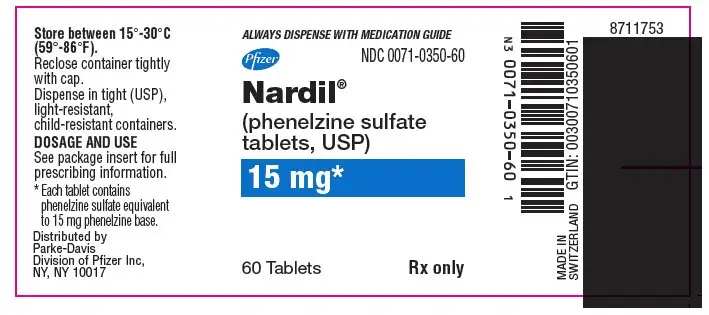
Drug Detail:Nardil (Phenelzine [ fen-el-zeen ])
Drug Class: Monoamine oxidase inhibitors
Suicidality and Antidepressant Drugs
Antidepressants increased the risk compared to placebo of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults in short-term studies of major depressive disorder (MDD) and other psychiatric disorders. Anyone considering the use of Nardil or any other antidepressant in a child, adolescent, or young adult must balance this risk with the clinical need. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction in risk with antidepressants compared to placebo in adults aged 65 and older. Depression and certain other psychiatric disorders are themselves associated with increases in the risk of suicide. Patients of all ages who are started on antidepressant therapy should be monitored appropriately and observed closely for clinical worsening, suicidality, or unusual changes in behavior. Families and caregivers should be advised of the need for close observation and communication with the prescriber. Nardil is not approved for use in pediatric patients. (See Warnings: Clinical Worsening and Suicide Risk, Precautions: Information for Patients, and Precautions: Pediatric Use)
Nardil - Clinical Pharmacology
Monoamine oxidase is a complex enzyme system, widely distributed throughout the body. Drugs that inhibit monoamine oxidase in the laboratory are associated with a number of clinical effects. Thus, it is unknown whether MAO inhibition per se, other pharmacologic actions, or an interaction of both is responsible for the clinical effects observed. Therefore, the physician should become familiar with all the effects produced by drugs of this class.
Contraindications
NARDIL should not be used in patients who are hypersensitive to the drug or its ingredients, with pheochromocytoma, congestive heart failure, severe renal impairment or renal disease, a history of liver disease, or abnormal liver function tests.
The potentiation of sympathomimetic substances and related compounds by MAO inhibitors may result in hypertensive crises (see WARNINGS). Therefore, patients being treated with NARDIL should not take sympathomimetic drugs (including amphetamines, cocaine, methylphenidate, dopamine, epinephrine, and norepinephrine) or related compounds (including methyldopa, L-dopa, L-tryptophan, L-tyrosine, and phenylalanine). Hypertensive crises during NARDIL therapy may also be caused by the ingestion of foods with a high concentration of tyramine or dopamine. Therefore, patients being treated with NARDIL should avoid high protein food that has undergone protein breakdown by aging, fermentation, pickling, smoking, or bacterial contamination. Patients should also avoid cheeses (especially aged varieties), pickled herring, beer, wine, liver, yeast extract (including brewer's yeast in large quantities), dry sausage (including Genoa salami, hard salami, pepperoni, and Lebanon bologna), pods of broad beans (fava beans), and yogurt. Excessive amounts of caffeine and chocolate may also cause hypertensive reactions.
NARDIL should not be used in combination with dextromethorphan or with CNS depressants such as alcohol and certain narcotics. Excitation, seizures, delirium, hyperpyrexia, circulatory collapse, coma, and death have been reported in patients receiving MAOI therapy who have been given a single dose of meperidine. NARDIL should not be administered together with or in rapid succession to other MAO inhibitors because HYPERTENSIVE CRISES and convulsive seizures, fever, marked sweating, excitation, delirium, tremor, coma, and circulatory collapse may occur.
Concomitant use with meperidine is contraindicated (see WARNINGS).
A List of MAO Inhibitors by Generic Name Follows:
pargyline hydrochloride
pargyline hydrochloride and methylclothiazide
furazolidone
isocarboxazid
procarbazine
tranylcypromine
NARDIL should also not be used in combination with buspirone HCl, since several cases of elevated blood pressure have been reported in patients taking MAO inhibitors who were then given buspirone HCl. At least 14 days should elapse between the discontinuation of NARDIL and the institution of another antidepressant or buspirone HCl, or the discontinuation of another MAO inhibitor and the institution of NARDIL.
There have been reports of serious reactions (including hyperthermia, rigidity, myoclonic movements and death) when serotoninergic drugs (e.g., dexfenfluramine, fluoxetine, fluvoxamine, paroxetine, sertraline, citalopram, venlafaxine) have been combined with an MAO inhibitor. Therefore, the concomitant use of NARDIL with serotoninergic agents is contraindicated (see PRECAUTIONS-Drug Interactions). At least 14 days should elapse between the discontinuation of an MAO inhibitor and the start of a serotonin re-uptake inhibitor or vice-versa, with the exception of fluoxetine. Allow at least five weeks between discontinuation of fluoxetine and initiation of NARDIL and at least 14 days between discontinuation of NARDIL and initiation of fluoxetine, or other serotoninergic agents. Before initiating NARDIL after using other serotoninergic agents, a sufficient amount of time must be allowed for clearance of the serotoninergic agent and its active metabolites.
The combination of MAO inhibitors and tryptophan has been reported to cause behavioral and neurologic syndromes including disorientation, confusion, amnesia, delirium, agitation, hypomanic signs, ataxia, myoclonus, hyperreflexia, shivering, ocular oscillations, and Babinski signs.
The concurrent administration of an MAO inhibitor and bupropion hydrochloride (Wellbutrin®) is contraindicated. At least 14 days should elapse between discontinuation of an MAO inhibitor and initiation of treatment with bupropion hydrochloride.
Patients taking NARDIL should not undergo elective surgery requiring general anesthesia. Also, they should not be given cocaine or local anesthesia containing sympathomimetic vasoconstrictors. The possible combined hypotensive effects of NARDIL and spinal anesthesia should be kept in mind. NARDIL should be discontinued at least 10 days prior to elective surgery.
MAO inhibitors, including NARDIL, are contraindicated in patients receiving guanethidine.
Warnings
Clinical Worsening and Suicide Risk
Patients with major depressive disorder (MDD), both adult and pediatric, may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressant medications, and this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders, and these disorders themselves are the strongest predictors of suicide. There has been a long-standing concern, however, that antidepressants may have a role in inducing worsening of depression and the emergence of suicidality in certain patients during the early phases of treatment. Pooled analyses of short-term placebo-controlled trials of antidepressant drugs (SSRIs and others) showed that these drugs increase the risk of suicidal thinking and behavior (suicidality) in children, adolescents, and young adults (ages 18–24) with major depressive disorder (MDD) and other psychiatric disorders. Short-term studies did not show an increase in the risk of suicidality with antidepressants compared to placebo in adults beyond age 24; there was a reduction with antidepressants compared to placebo in adults aged 65 and older.
The pooled analyses of placebo-controlled trials in children and adolescents with MDD, obsessive compulsive disorder (OCD), or other psychiatric disorders included a total of 24 short-term trials of 9 antidepressant drugs in over 4400 patients. The pooled analyses of placebo-controlled trials in adults with MDD or other psychiatric disorders included a total of 295 short-term trials (median duration of 2 months) of 11 antidepressant drugs in over 77,000 patients. There was considerable variation in risk of suicidality among drugs, but a tendency toward an increase in the younger patients for almost all drugs studied. There were differences in absolute risk of suicidality across the different indications, with the highest incidence in MDD. The risk differences (drug vs placebo), however, were relatively stable within age strata and across indications. These risk differences (drug-placebo difference in the number of cases of suicidality per 1000 patients treated) are provided in Table 1.
| Age Range | Drug-Placebo Difference in Number of Cases of Suicidality per 1000 Patients Treated |
|---|---|
| Increases Compared to Placebo | |
| <18 | 14 additional cases |
| 18–24 | 5 additional cases |
| Decreases Compared to Placebo | |
| 25–64 | 1 fewer case |
| ≥65 | 6 fewer cases |
No suicides occurred in any of the pediatric trials. There were suicides in the adult trials, but the number was not sufficient to reach any conclusion about drug effect on suicide.
It is unknown whether the suicidality risk extends to longer-term use, i.e., beyond several months. However, there is substantial evidence from placebo-controlled maintenance trials in adults with depression that the use of antidepressants can delay the recurrence of depression.
All patients being treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the initial few months of a course of drug therapy, or at times of dose changes, either increases or decreases.
The following symptoms, anxiety, agitation, panic attacks, insomnia, irritability, hostility, aggressiveness, impulsivity, akathisia (psychomotor restlessness), hypomania, and mania, have been reported in adult and pediatric patients being treated with antidepressants for major depressive disorder as well as for other indications, both psychiatric and nonpsychiatric. Although a causal link between the emergence of such symptoms and either the worsening of depression and/or the emergence of suicidal impulses has not been established, there is concern that such symptoms may represent precursors to emerging suicidality.
Consideration should be given to changing the therapeutic regimen, including possibly discontinuing the medication, in patients whose depression is persistently worse, or who are experiencing emergent suicidality or symptoms that might be precursors to worsening depression or suicidality, especially if these symptoms are severe, abrupt in onset, or were not part of the patient's presenting symptoms.
Families and caregivers of patients being treated with antidepressants for major depressive disorder or other indications, both psychiatric and nonpsychiatric, should be alerted about the need to monitor patients for the emergence of agitation, irritability, unusual changes in behavior, and the other symptoms described above, as well as the emergence of suicidality, and to report such symptoms immediately to health care providers. Such monitoring should include daily observation by families and caregivers. Prescriptions for Nardil should be written for the smallest quantity of tablets consistent with good patient management, in order to reduce the risk of overdose.
Screening Patients for Bipolar Disorder
A major depressive episode may be the initial presentation of bipolar disorder. It is generally believed (though not established in controlled trials) that treating such an episode with an antidepressant alone may increase the likelihood of precipitation of a mixed/manic episode in patients at risk for bipolar disorder. Whether any of the symptoms described above represent such a conversion is unknown. However, prior to initiating treatment with an antidepressant, patients with depressive symptoms should be adequately screened to determine if they are at risk for bipolar disorder; such screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. It should be noted that Nardil is not approved for use in treating bipolar depression.
It should be noted that NARDIL is not approved for use in treating any indications in the pediatric population.
The most serious reactions to NARDIL involve changes in blood pressure.
Precautions
Information for Patients
Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with Nardil and should counsel them in its appropriate use. A patient Medication Guide about "Antidepressant Medicines, Depression and other Serious Mental Illness, and Suicidal Thoughts or Actions" is available for Nardil. The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents. Patients should be given the opportunity to discuss the contents of the Medication Guide and to obtain answers to any questions they may have. The complete text of the Medication Guide is reprinted at the end of this document.
Patients should be advised of the following issues and asked to alert their prescriber if these occur while taking Nardil.
Pediatric Use
Safety and effectiveness in the pediatric population have not been established (see BOX WARNING and WARNINGS—Clinical Worsening and Suicide Risk).
Anyone considering the use of NARDIL in a child or adolescent must balance the potential risks with the clinical need.
Nardil, as with other hydrazine derivatives, has been reported to induce pulmonary and vascular tumors in an uncontrolled lifetime study in mice.
In depressed patients, the possibility of suicide should always be considered and adequate precautions taken. It is recommended that careful observations of patients undergoing NARDIL treatment be maintained until control of depression is achieved. If necessary, additional measures (ECT, hospitalization, etc) should be instituted.
All patients undergoing treatment with NARDIL should be closely followed for symptoms of postural hypotension. Hypotensive side effects have occurred in hypertensive as well as normotensive and hypotensive patients. Blood pressure usually returns to pretreatment levels rapidly when the drug is discontinued or the dosage is reduced.
Because the effect of NARDIL on the convulsive threshold may be variable, adequate precautions should be taken when treating epileptic patients.
Of the more severe side effects that have been reported with any consistency, hypomania has been the most common. This reaction has been largely limited to patients in whom disorders characterized by hyperkinetic symptoms coexist with, but are obscured by, depressive affect; hypomania usually appeared as depression improved. If agitation is present, it may be increased with NARDIL. Hypomania and agitation have also been reported at higher than recommended doses or following long-term therapy.
NARDIL may cause excessive stimulation in schizophrenic patients; in manic-depressive states it may result in a swing from a depressive to a manic phase.
NARDIL should be used with caution in diabetes mellitus; increased insulin sensitivity may occur. Requirements for insulin or oral hypoglycemics may be decreased.
MAO inhibitors, including NARDIL, potentiate hexobarbital hypnosis in animals. Therefore, barbiturates should be given at a reduced dose with NARDIL.
MAO inhibitors inhibit the destruction of serotonin and norepinephrine, which are believed to be released from tissue stores by rauwolfia alkaloids. Accordingly, caution should be exercised when rauwolfia is used concomitantly with an MAO inhibitor, including NARDIL.
There is conflicting evidence as to whether or not MAO inhibitors affect glucose metabolism or potentiate hypoglycemic agents. This should be kept in mind if NARDIL is administered to diabetics.
Drug Interactions
In patients receiving nonselective monoamine oxidase (MAO) inhibitors in combination with serotoninergic agents (e.g., dexfenfluramine, fluoxetine, fluvoxamine, paroxetine, sertraline, citalopram, venlafaxine) there have been reports of serious, sometimes fatal, reactions. Because NARDIL is a monoamine oxidase (MAO) inhibitor, NARDIL should not be used concomitantly with a serotoninergic agent (See CONTRAINDICATIONS).
Administration of guanethidine to patients receiving an MAO inhibitor can produce moderate to severe hypertension due to release of catecholamines. At least two weeks should elapse between withdrawal of the MAO inhibitor and the initiation of guanethidine. (see CONTRAINDICATIONS)
| NARDIL
phenelzine sulfate tablet, film coated |
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
|
||||||||||||||||||
| Labeler - Parke-Davis Div of Pfizer Inc (829076962) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Farmea | 286080408 | MANUFACTURE(0071-0350) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Siegfried Evionnaz SA | 480093164 | API MANUFACTURE(0071-0350) | |