Drug Detail:Prevacid (Lansoprazole [ lan-soe-pra-zol ])
Drug Class: Proton pump inhibitors
Highlights of Prescribing Information
PREVACID (lansoprazole) delayed-release capsules, for oral use PREVACID SOLUTAB (lansoprazole) delayed-release orally disintegrating tablets
Initial U.S. Approval: 1995
Indications and Usage for Prevacid
PREVACID and PREVACID SoluTab are proton pump inhibitors (PPIs) indicated for the:
- Treatment of active duodenal ulcer in adults. (1.1)
- Eradication of H. pylori to reduce the risk of duodenal ulcer recurrence in adults. (1.2)
- Maintenance of healed duodenal ulcers in adults. (1.3)
- Treatment of active benign gastric ulcer in adults. (1.4)
- Healing of nonsteroidal anti-inflammatory drugs (NSAID)-associated gastric ulcer in adults. (1.5)
- Risk reduction of NSAID-associated gastric ulcer in adults. (1.6)
- Treatment of symptomatic gastroesophageal reflux disease (GERD) in adults and pediatric patients 1 year of age and older. (1.7)
- Treatment of erosive esophagitis (EE) in adults and pediatric patients 1 year of age and older. (1.8)
- Maintenance of healing of EE in adults. (1.9)
- Pathological hypersecretory conditions, including Zollinger-Ellison syndrome (ZES) in adults. (1.10)
Prevacid Dosage and Administration
Recommended Dosage:
- See full prescribing information for complete dosing information for PREVACID and PREVACID SoluTab by indication and age group and dosage adjustment in patients with severe hepatic impairment. (2.1, 2.2, 2.3)
Administration Instructions (2.4)
PREVACID capsules
- Should be swallowed whole.
- See full prescribing information for alternative administration options.
PREVACID SoluTab
- Should not be broken or cut.
- Should not be chewed.
- Place the tablet on the tongue and allow it to disintegrate, with or without water, until the particles can be swallowed.
- See full prescribing information for alternative administration options.
Dosage Forms and Strengths
- Delayed-release capsules: 30 mg. (3)
- Delayed-release orally disintegrating tablets: 15 mg and 30 mg. (3)
Contraindications
- Contraindicated in patients with known hypersensitivity to any component of the PREVACID or PREVACID SoluTab formulations. (4)
- Patients receiving rilpivirine-containing products. (4, 7)
Warnings and Precautions
- Gastric Malignancy: In adults, symptomatic response with PREVACID or PREVACID SoluTab does not preclude the presence of gastric malignancy. Consider additional follow-up and diagnostic testing. (5.1)
- Acute Tubulointerstitial Nephritis: Discontinue treatment and evaluate patients. (5.2)
- Clostridium difficile-Associated Diarrhea: PPI therapy may be associated with increased risk of Clostridium difficile-associated diarrhea. (5.3)
- Bone Fracture: Long-term and multiple daily dose PPI therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist or spine. (5.4)
- Severe Cutaneous Adverse Reactions: Discontinue at the first signs or symptoms of severe cutaneous adverse reactions or other signs of hypersensitivity and consider further evaluation. (5.5)
- Cutaneous and Systemic Lupus Erythematosus: Mostly cutaneous; new onset or exacerbation of existing disease; discontinue PREVACID and PREVACID SoluTab and refer to specialist for evaluation. (5.6)
- Cyanocobalamin (Vitamin B12) Deficiency: Daily long-term use (e.g., longer than 3 years) may lead to malabsorption or a deficiency of cyanocobalamin. (5.7)
- Hypomagnesemia and Mineral Metabolism: Hypomagnesemia has been reported rarely with prolonged treatment with PPIs. (5.8)
- Interactions with Investigations for Neuroendocrine Tumors: Increases in intragastric pH may result in hypergastrinemia and enterochromaffin-like cell hyperplasia and increased chromogranin A levels which may interfere with diagnostic investigations for neuroendocrine tumors. (5.9, 7)
- Interaction with Methotrexate: Concomitant use with PPIs may elevate and/or prolong serum concentrations of methotrexate and/or its metabolite, possibly leading to toxicity. With high-dose methotrexate administration, consider a temporary withdrawal of PREVACID. (5.10, 7)
- Patients with Phenylketonuria: Each 15 mg PREVACID SoluTab contains 2.5 mg and each 30 mg PREVACID SoluTab contains 5.1 mg of phenylalanine. (5.11)
- Fundic Gland Polyps: Risk increases with long-term use, especially beyond 1 year. Use the shortest duration of therapy. (5.12)
- Risk of Heart Valve Thickening in Pediatric Patients Less than One Year of Age: PREVACID is not recommended in pediatric patients less than 1 year of age. (5.13, 8.4)
Adverse Reactions/Side Effects
Most commonly reported adverse reactions (≥1%): diarrhea, abdominal pain, nausea and constipation. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Takeda Pharmaceuticals America, Inc. at 1-877-TAKEDA-7 (1-877-825-3327) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
See full prescribing information for a list of clinically important drug interactions. (7)
Use In Specific Populations
- Pregnancy: Based on animal data, may cause adverse effects on fetal bone growth and development. (8.1)
- Pediatrics: Use is not recommended for the treatment of symptomatic GERD in patients 1 month to less than 1 year of age; efficacy was not demonstrated and nonclinical studies have demonstrated adverse effects in juvenile rats. (5.13, 8.4)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 8/2023
Full Prescribing Information
1. Indications and Usage for Prevacid
1.1 Treatment of Active Duodenal Ulcer
PREVACID and PREVACID SoluTab are indicated in adults for short-term treatment (for four weeks) for healing and symptom relief of active duodenal ulcer [see Clinical Studies (14.1)].
1.3 Maintenance of Healed Duodenal Ulcers
PREVACID and PREVACID SoluTab are indicated in adults to maintain healing of duodenal ulcers. Controlled studies do not extend beyond 12 months [see Clinical Studies (14.3)].
1.4 Treatment of Active Benign Gastric Ulcer
PREVACID and PREVACID SoluTab are indicated in adults for short-term treatment (up to eight weeks) for healing and symptom relief of active benign gastric ulcer [see Clinical Studies (14.4)].
1.5 Healing of NSAID-Associated Gastric Ulcer
PREVACID and PREVACID SoluTab are indicated in adults for the treatment of NSAID-associated gastric ulcer in patients who continue NSAID use. Controlled studies did not extend beyond eight weeks [see Clinical Studies (14.5)].
1.6 Risk Reduction of NSAID-Associated Gastric Ulcer
PREVACID and PREVACID SoluTab are indicated in adults for reducing the risk of NSAID-associated gastric ulcers in patients with a history of a documented gastric ulcer who require the use of an NSAID. Controlled studies did not extend beyond 12 weeks [see Clinical Studies (14.6)].
1.7 Treatment of Symptomatic Gastroesophageal Reflux Disease (GERD)
PREVACID and PREVACID SoluTab are indicated for short-term treatment in adults and pediatric patients 12 to 17 years of age (up to eight weeks) and pediatric patients one to 11 years of age (up to 12 weeks) for the treatment of heartburn and other symptoms associated with GERD [see Clinical Studies (14.7)].
1.8 Treatment of Erosive Esophagitis (EE)
PREVACID and PREVACID SoluTab are indicated for short-term treatment in adults and pediatric patients 12 to 17 years of age (up to eight weeks) and pediatric patients one to 11 years of age (up to 12 weeks) for healing and symptom relief of all grades of EE.
For adults who do not heal with PREVACID or PREVACID SoluTab for eight weeks (5 to 10%), it may be helpful to give an additional eight weeks of treatment. If there is a recurrence of erosive esophagitis an additional eight week course of PREVACID or PREVACID SoluTab may be considered [see Clinical Studies (14.8)].
2. Prevacid Dosage and Administration
2.1 Recommended Adult Dosage by Indication
| Indication | Recommended Dose | Frequency |
|---|---|---|
|
||
| Duodenal Ulcers | ||
| Short-Term Treatment | 15 mg | Once daily for 4 weeks |
| Maintenance of Healed | 15 mg | Once daily |
| Eradication of H. pylori to Reduce the Risk of Duodenal Ulcer Recurrence* | ||
| Triple Therapy: | ||
| PREVACID or PREVACID SoluTab | 30 mg | Twice daily for 10 or 14 days |
| Amoxicillin | 1 gram | Twice daily for 10 or 14 days |
| Clarithromycin | 500 mg | Twice daily for 10 or 14 days |
| Dual Therapy: | ||
| PREVACID or PREVACID SoluTab | 30 mg | Three times daily for 14 days |
| Amoxicillin | 1 gram | Three times daily for 14 days |
| Benign Gastric Ulcer | ||
| Short-Term Treatment | 30 mg | Once daily for up to 8 weeks |
| NSAID-Associated Gastric Ulcer | ||
| Healing | 30 mg | Once daily for 8 weeks† |
| Risk Reduction | 15 mg | Once daily for up to 12 weeks† |
| Gastroesophageal Reflux Disease (GERD) | ||
| Short-Term Treatment of Symptomatic GERD | 15 mg | Once daily for up to 8 weeks |
| Short-Term Treatment of Erosive Esophagitis | 30 mg | Once daily for up to 8 weeks‡ |
| Maintenance of Healing of Erosive Esophagitis | 15 mg | Once daily§ |
| Pathological Hypersecretory Conditions Including Zollinger-Ellison Syndrome | 60 mg | Once daily¶ |
2.3 Hepatic Impairment
The recommended dosage is 15 mg orally daily in patients with severe liver impairment (Child-Pugh C) [see Use in Specific Populations (8.6)].
2.4 Important Administration Information
- Take PREVACID or PREVACID SoluTab before meals.
- Do not crush or chew PREVACID capsule or PREVACID SoluTab.
- Take PREVACID or PREVACID SoluTab at least 30 minutes prior to sucralfate [see Drug Interactions (7)].
- Antacids may be used concomitantly with PREVACID or PREVACID SoluTab.
- Missed doses: If a dose is missed, administer as soon as possible. However, if the next scheduled dose is due, do not take the missed dose, and take the next dose on time. Do not take two doses at one time to make up for a missed dose.
3. Dosage Forms and Strengths
PREVACID delayed-release capsules:
- 15 mg strength is not currently marketed by Takeda Pharmaceuticals America, Inc.
- 30 mg strength is an opaque, pink and black capsule imprinted with "TAP" and "PREVACID 30".
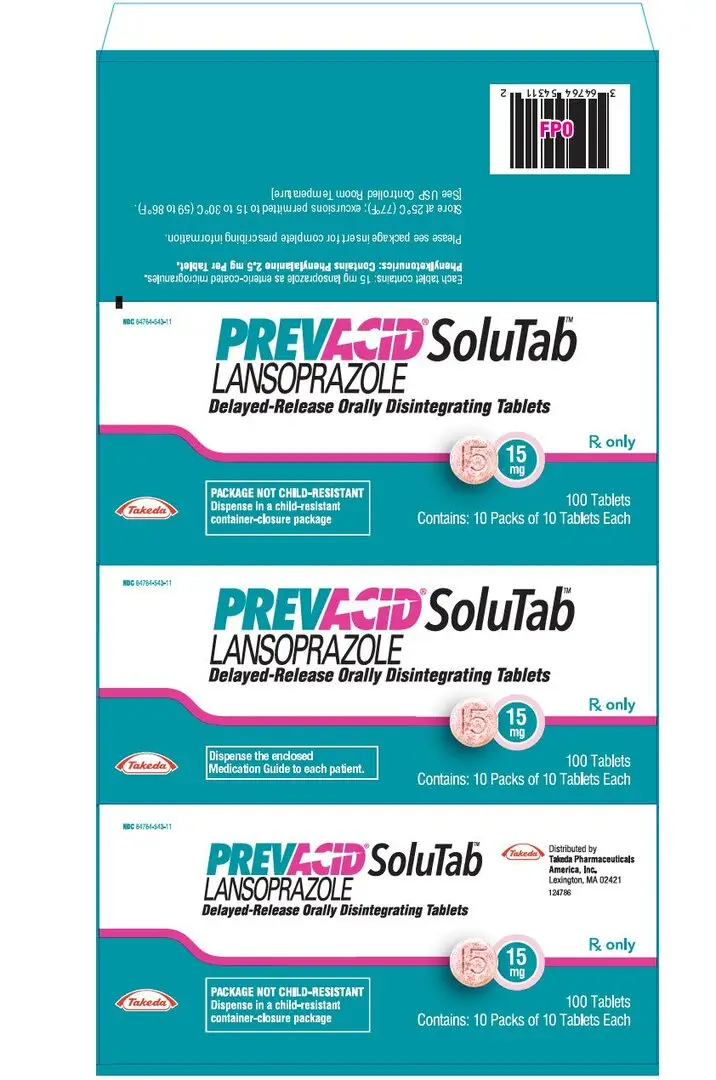
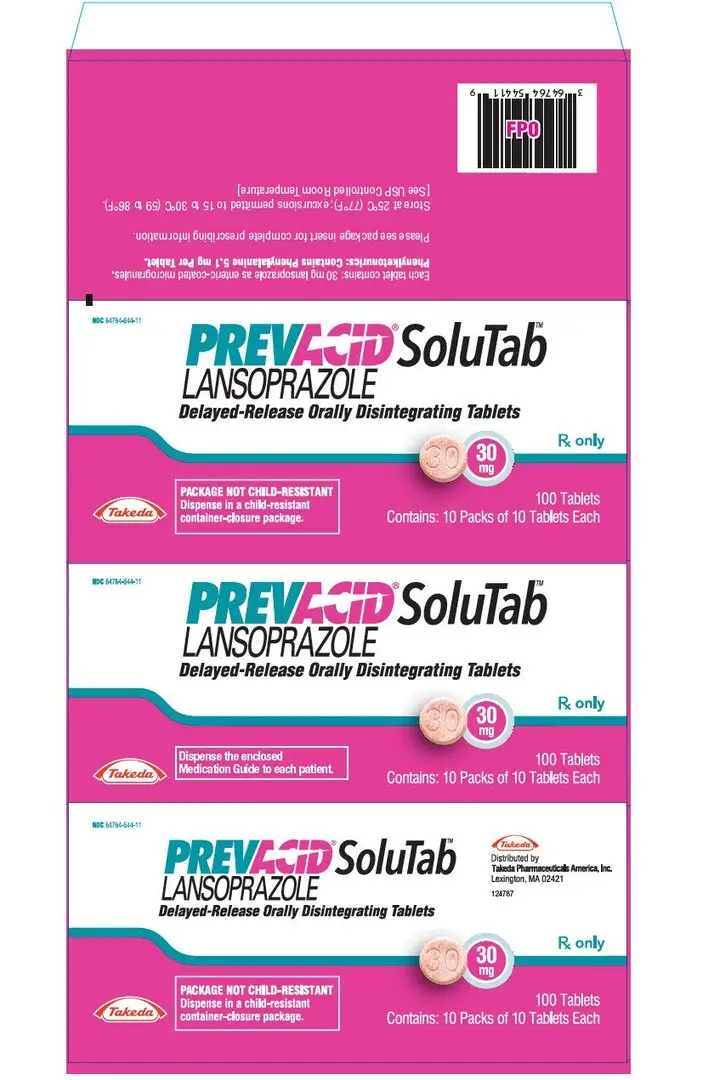
PREVACID SoluTab delayed-release orally disintegrating tablets:
- 15 mg strength is a white to yellowish white, uncoated round tablet containing orange to dark brown speckles with "15" debossed on one side.
- 30 mg strength is a white to yellowish white, uncoated round tablet containing orange to dark brown speckles with "30" debossed on one side.
4. Contraindications
- PREVACID and PREVACID SoluTab are contraindicated in patients with known hypersensitivity to any component of the formulation. Hypersensitivity reactions may include anaphylaxis, anaphylactic shock, angioedema, bronchospasm, acute tubulointerstitial nephritis, and urticaria [see Warnings and Precautions (5.2), Adverse Reactions (6)].
- Proton Pump Inhibitors (PPIs), including PREVACID and PREVACID SoluTab, are contraindicated with rilpivirine-containing products [see Drug Interactions (7)].
- For information about contraindications of antibacterial agents (clarithromycin and amoxicillin) indicated in combination with PREVACID or PREVACID SoluTab, refer to the Contraindications section of their prescribing information.
5. Warnings and Precautions
5.1 Presence of Gastric Malignancy
In adults, symptomatic response to therapy with PREVACID or PREVACID SoluTab does not preclude the presence of gastric malignancy. Consider additional follow-up and diagnostic testing in adult patients who have a suboptimal response or an early symptomatic relapse after completing treatment with a PPI. In older patients, also consider an endoscopy.
5.2 Acute Tubulointerstitial Nephritis
Acute tubulointerstial nephritis (TIN) has been observed in patients taking PPIs and may occur at any point during PPI therapy. Patients may present with varying signs and symptoms from symptomatic hypersensitivity reactions to non-specific symptoms of decreased renal function (e.g., malaise, nausea, anorexia). In reported case series, some patients were diagnosed on biopsy and in the absence of extra-renal manifestations (e.g., fever, rash or arthralgia).
Discontinue PREVACID or PREVACID SoluTab and evaluate patients with suspected acute TIN [see Contraindications (4)].
5.3 Clostridium difficile-Associated Diarrhea
Published observational studies suggest that PPI therapy like PREVACID and PREVACID SoluTab may be associated with an increased risk of Clostridium difficile-associated diarrhea (CDAD), especially in hospitalized patients. This diagnosis should be considered for diarrhea that does not improve [see Adverse Reactions (6.2)].
Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated.
CDAD has been reported with use of nearly all antibacterial agents. For more information specific to antibacterial agents (clarithromycin and amoxicillin) indicated for use in combination with PREVACID or PREVACID SoluTab, refer to Warnings and Precautions section of their prescribing information.
5.4 Bone Fracture
Several published observational studies suggest that PPI therapy may be associated with an increased risk for osteoporosis-related fractures of the hip, wrist or spine. The risk of fracture was increased in patients who received high-dose, defined as multiple daily doses, and long-term PPI therapy (a year or longer). Patients should use the lowest dose and shortest duration of PPI therapy appropriate to the condition being treated. Patients at risk for osteoporosis-related fractures should be managed according to established treatment guidelines [see Dosage and Administration (2), Adverse Reactions (6.2)].
5.5 Severe Cutaneous Adverse Reactions
Severe cutaneous adverse reactions, including Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN), drug reaction with eosinophilia and systemic symptoms (DRESS), and acute generalized exanthematous pustulosis (AGEP) have been reported in association with the use of PPIs [see Adverse Reactions (6.2)]. Discontinue PREVACID or PREVACID SoluTab at the first signs or symptoms of severe cutaneous adverse reactions or other signs of hypersensitivity and consider further evaluation.
5.6 Cutaneous and Systemic Lupus Erythematosus
Cutaneous lupus erythematosus (CLE) and systemic lupus erythematosus (SLE) have been reported in patients taking PPIs, including lansoprazole. These events have occurred as both new onset and an exacerbation of existing autoimmune disease. The majority of PPI-induced lupus erythematosus cases were CLE.
The most common form of CLE reported in patients treated with PPIs was subacute CLE (SCLE) and occurred within weeks to years after continuous drug therapy in patients ranging from infants to the elderly. Generally, histological findings were observed without organ involvement.
Systemic lupus erythematosus (SLE) is less commonly reported than CLE in patients receiving PPIs. PPI-associated SLE is usually milder than nondrug induced SLE. Onset of SLE typically occurred within days to years after initiating treatment primarily in patients ranging from young adults to the elderly. The majority of patients presented with rash; however, arthralgia and cytopenia were also reported.
Avoid administration of PPIs for longer than medically indicated. If signs or symptoms consistent with CLE or SLE are noted in patients receiving PREVACID or PREVACID SoluTab, discontinue the drug and refer the patient to the appropriate specialist for evaluation. Most patients improve with discontinuation of the PPI alone in four to 12 weeks. Serological testing (e.g., ANA) may be positive and elevated serological test results may take longer to resolve than clinical manifestations.
5.7 Cyanocobalamin (Vitamin B12) Deficiency
Daily treatment with any acid-suppressing medications over a long period of time (e.g., longer than three years) may lead to malabsorption of cyanocobalamin (Vitamin B12) caused by hypo- or achlorhydria. Rare reports of cyanocobalamin deficiency occurring with acid-suppressing therapy have been reported in the literature. This diagnosis should be considered if clinical symptoms consistent with cyanocobalamin deficiency are observed in patients treated with PREVACID or PREVACID SoluTab.
5.8 Hypomagnesemia and Mineral Metabolism
Hypomagnesemia, symptomatic and asymptomatic, has been reported rarely in patients treated with PPIs for at least three months, in most cases after a year of therapy. Serious adverse events include tetany, arrhythmias, and seizures. Hypomagnesemia may lead to hypocalcemia and/or hypokalemia and may exacerbate underlying hypocalcemia in at-risk patients. In most patients, treatment of hypomagnesemia required magnesium replacement and discontinuation of the PPI.
For patients expected to be on prolonged treatment or who take PPIs with medications such as digoxin or drugs that may cause hypomagnesemia (e.g., diuretics), health care professionals may consider monitoring magnesium levels prior to initiation of PPI treatment and periodically [see Adverse Reactions (6.2)].
Consider monitoring magnesium and calcium levels prior to initiation of PREVACID or PREVACID SoluTab and periodically while on treatment in patients with a preexisting risk of hypocalcemia (e.g., hypoparathyroidism). Supplement with magnesium and/or calcium, as necessary. If hypocalcemia is refractory to treatment, consider discontinuing the PPI.
5.9 Interactions with Investigations for Neuroendocrine Tumors
Serum chromogranin A (CgA) levels increase secondary to drug-induced decreases in gastric acidity. The increased CgA level may cause false positive results in diagnostic investigations for neuroendocrine tumors. Healthcare providers should temporarily stop lansoprazole treatment at least 14 days before assessing CgA levels and consider repeating the test if initial CgA levels are high. If serial tests are performed (e.g., for monitoring), the same commercial laboratory should be used for testing, as reference ranges between tests may vary [see Drug Interactions (7), Clinical Pharmacology (12.2)].
5.10 Interaction with Methotrexate
Literature suggests that concomitant use of PPIs with methotrexate (primarily at high dose) may elevate and prolong serum levels of methotrexate and/or its metabolite, possibly leading to methotrexate toxicities. In high-dose methotrexate administration, a temporary withdrawal of the PPI may be considered in some patients [see Drug Interactions (7), Clinical Pharmacology (12.3)].
5.11 Patients with Phenylketonuria
Phenylalanine can be harmful to patients with phenylketonuria (PKU). PREVACID SoluTab contains phenylalanine, a component of aspartame. Each 15 mg tablet contains 2.5 mg and each 30 mg tablet contains 5.1 mg of phenylalanine. Before prescribing PREVACID SoluTab to a patient with PKU, consider the combined daily amount of phenylalanine from all sources, including PREVACID SoluTab.
5.12 Fundic Gland Polyps
PPI use is associated with an increased risk of fundic gland polyps that increases with long-term use, especially beyond one year. Most PPI users who developed fundic gland polyps were asymptomatic and fundic gland polyps were identified incidentally on endoscopy. Use the shortest duration of PPI therapy appropriate to the condition being treated.
5.13 Risk of Heart Valve Thickening in Pediatric Patients Less Than One Year of Age
PREVACID and PREVACID SoluTab are not approved in pediatric patients less than one year of age. Nonclinical studies in juvenile rats with lansoprazole have demonstrated an adverse effect of heart valve thickening. The risk of heart valve injury does not appear to be relevant to patients one year of age and older [see Use in Specific Populations (8.4)].
6. Adverse Reactions/Side Effects
The following serious adverse reactions are described below and elsewhere in labeling:
- Acute Tubulointerstitial Nephritis [see Warnings and Precautions (5.2)]
- Clostridium difficile-Associated Diarrhea [see Warnings and Precautions (5.3)]
- Bone Fracture [see Warnings and Precautions (5.4)]
- Severe Cutaneous Adverse Reactions [see Warnings and Precautions (5.5)]
- Cutaneous and Systemic Lupus Erythematosus [see Warnings and Precautions (5.6)]
- Cyanocobalamin (Vitamin B12) Deficiency [see Warnings and Precautions (5.7)]
- Hypomagnesemia and Mineral Metabolism [see Warnings and Precautions (5.8)]
- Fundic Gland Polyps [see Warnings and Precautions (5.12)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in clinical practice.
Worldwide, over 10,000 patients have been treated with PREVACID in Phase 2 or Phase 3 clinical trials involving various dosages and durations of treatment. In general, PREVACID treatment has been well-tolerated in both short-term and long-term trials.
The following adverse reactions were reported by the treating physician to have a possible or probable relationship to drug in 1% or more of PREVACID-treated patients and occurred at a greater rate in PREVACID-treated patients than placebo-treated patients in Table 1.
| Body System/Adverse Reaction | PREVACID (N=2768) % | Placebo (N=1023) % |
|---|---|---|
| Body as a Whole | ||
| Abdominal Pain | 2.1 | 1.2 |
| Digestive System | ||
| Constipation | 1.0 | 0.4 |
| Diarrhea | 3.8 | 2.3 |
| Nausea | 1.3 | 1.2 |
Headache was also seen at greater than 1% incidence but was more common on placebo. The incidence of diarrhea was similar between patients who received placebo and patients who received 15 and 30 mg of PREVACID, but higher in the patients who received 60 mg of PREVACID (2.9, 1.4, 4.2, and 7.4%, respectively).
The most commonly reported possibly or probably treatment-related adverse event during maintenance therapy was diarrhea.
In the risk reduction study of PREVACID for NSAID-associated gastric ulcers, the incidence of diarrhea for patients treated with PREVACID, misoprostol, and placebo was 5, 22, and 3%, respectively.
Another study for the same indication, where patients took either a COX-2 inhibitor or lansoprazole and naproxen, demonstrated that the safety profile was similar to the prior study. Additional reactions from this study not previously observed in other clinical trials with PREVACID included contusion, duodenitis, epigastric discomfort, esophageal disorder, fatigue, hunger, hiatal hernia, hoarseness, impaired gastric emptying, metaplasia, and renal impairment.
Additional adverse experiences occurring in less than 1% of patients or subjects who received PREVACID in domestic trials are shown below:
Body as a Whole – abdomen enlarged, allergic reaction, asthenia, back pain, candidiasis, carcinoma, chest pain (not otherwise specified), chills, edema, fever, flu syndrome, halitosis, infection (not otherwise specified), malaise, neck pain, neck rigidity, pain, pelvic pain
Cardiovascular System – angina, arrhythmia, bradycardia, cerebrovascular accident/cerebral infarction, hypertension/hypotension, migraine, myocardial infarction, palpitations, shock (circulatory failure), syncope, tachycardia, vasodilation
Digestive System – abnormal stools, anorexia, bezoar, cardiospasm, cholelithiasis, colitis, dry mouth, dyspepsia, dysphagia, enteritis, eructation, esophageal stenosis, esophageal ulcer, esophagitis, fecal discoloration, flatulence, gastric nodules/fundic gland polyps, gastritis, gastroenteritis, gastrointestinal anomaly, gastrointestinal disorder, gastrointestinal hemorrhage, glossitis, gum hemorrhage, hematemesis, increased appetite, increased salivation, melena, mouth ulceration, nausea and vomiting, nausea and vomiting and diarrhea, gastrointestinal moniliasis, rectal disorder, rectal hemorrhage, stomatitis, tenesmus, thirst, tongue disorder, ulcerative colitis, ulcerative stomatitis
Endocrine System – diabetes mellitus, goiter, hypothyroidism
Hemic and Lymphatic System – anemia, hemolysis, lymphadenopathy
Metabolism and Nutritional Disorders – avitaminosis, gout, dehydration, hyperglycemia/hypoglycemia, peripheral edema, weight gain/loss
Musculoskeletal System – arthralgia, arthritis, bone disorder, joint disorder, leg cramps, musculoskeletal pain, myalgia, myasthenia, ptosis, synovitis
Nervous System – abnormal dreams, agitation, amnesia, anxiety, apathy, confusion, convulsion, dementia, depersonalization, depression, diplopia, dizziness, emotional lability, hallucinations, hemiplegia, hostility aggravated, hyperkinesia, hypertonia, hypesthesia, insomnia, libido decreased/increased, nervousness, neurosis, paresthesia, sleep disorder, somnolence, thinking abnormality, tremor, vertigo
Respiratory System – asthma, bronchitis, cough increased, dyspnea, epistaxis, hemoptysis, hiccup, laryngeal neoplasia, lung fibrosis, pharyngitis, pleural disorder, pneumonia, respiratory disorder, upper respiratory inflammation/infection, rhinitis, sinusitis, stridor
Skin and Appendages – acne, alopecia, contact dermatitis, dry skin, fixed eruption, hair disorder, maculopapular rash, nail disorder, pruritus, rash, skin carcinoma, skin disorder, sweating, urticaria
Special Senses – abnormal vision, amblyopia, blepharitis, blurred vision, cataract, conjunctivitis, deafness, dry eyes, ear/eye disorder, eye pain, glaucoma, otitis media, parosmia, photophobia, retinal degeneration/disorder, taste loss, taste perversion, tinnitus, visual field defect
Urogenital System – abnormal menses, breast enlargement, breast pain, breast tenderness, dysmenorrhea, dysuria, gynecomastia, impotence, kidney calculus, kidney pain, leukorrhea, menorrhagia, menstrual disorder, penis disorder, polyuria, testis disorder, urethral pain, urinary frequency, urinary retention, urinary tract infection, urinary urgency, urination impaired, vaginitis
6.2 Postmarketing Experience
Additional adverse experiences have been reported since PREVACID and PREVACID SoluTab have been marketed. The majority of these cases are foreign-sourced and a relationship to PREVACID or PREVACID SoluTab has not been established. Because these reactions were reported voluntarily from a population of unknown size, estimates of frequency cannot be made. These events are listed below by COSTART body system.
Body as a Whole – anaphylactic/anaphylactoid reactions, systemic lupus erythematosus; Digestive System – hepatotoxicity, pancreatitis, vomiting; Hemic and Lymphatic System – agranulocytosis, aplastic anemia, hemolytic anemia, leukopenia, neutropenia, pancytopenia, thrombocytopenia, and thrombotic thrombocytopenic purpura; Infections and Infestations – Clostridium difficile-associated diarrhea; Metabolism and Nutritional Disorders – hypomagnesemia, hypocalcemia, hypokalemia, hyponatremia; Musculoskeletal System – bone fracture, myositis; Skin and Appendages – severe dermatologic reactions including erythema multiforme, SJS/TEN (some fatal), DRESS, AGEP, cutaneous lupus erythematosus; Special Senses – speech disorder; Urogenital System – interstitial nephritis, urinary retention.
6.3 Combination Therapy with Amoxicillin and Clarithromycin
In clinical trials using combination therapy with PREVACID plus amoxicillin and clarithromycin, and PREVACID plus amoxicillin, no adverse reactions peculiar to these drug combinations were observed. Adverse reactions that have occurred have been limited to those that had been previously reported with PREVACID, amoxicillin, or clarithromycin.
6.4 Laboratory Values
The following changes in laboratory parameters in patients who received PREVACID were reported as adverse reactions:
Abnormal liver function tests, increased SGOT (AST), increased SGPT (ALT), increased creatinine, increased alkaline phosphatase, increased globulins, increased GGTP, increased/decreased/abnormal WBC, abnormal AG ratio, abnormal RBC, bilirubinemia, blood potassium increased, blood urea increased, crystal urine present, eosinophilia, hemoglobin decreased, hyperlipemia, increased/decreased electrolytes, increased/decreased cholesterol, increased glucocorticoids, increased LDH, increased/decreased/abnormal platelets, increased gastrin levels and positive fecal occult blood. Urine abnormalities such as albuminuria, glycosuria, and hematuria were also reported. Additional isolated laboratory abnormalities were reported.
In the placebo-controlled studies, when SGOT (AST) and SGPT (ALT) were evaluated, 0.4% (4/978) and 0.4% (11/2677) patients, who received placebo and PREVACID, respectively, had enzyme elevations greater than three times the upper limit of normal range at the final treatment visit. None of these patients who received PREVACID reported jaundice at any time during the study.
In clinical trials using combination therapy with PREVACID plus amoxicillin and clarithromycin, and PREVACID plus amoxicillin, no increased laboratory abnormalities particular to these drug combinations were observed.
For information about laboratory value changes with antibacterial agents (amoxicillin and clarithromycin) indicated in combination with PREVACID or PREVACID SoluTab, refer to the Adverse Reactions section of their prescribing information.
7. Drug Interactions
Tables 2 and 3 include drugs with clinically important drug interactions and interaction with diagnostics when administered concomitantly with PREVACID or PREVACID SoluTab and instructions for preventing or managing them.
Consult the labeling of concomitantly used drugs to obtain further information about interactions with PPIs.
| Antiretrovirals | |
| Clinical Impact: | The effect of PPIs on antiretroviral drugs is variable. The clinical importance and the mechanisms behind these interactions are not always known.
|
| Intervention: | Rilpivirine-containing products: Concomitant use with PREVACID or PREVACID SoluTab is contraindicated [see Contraindications (4)]. See prescribing information. Atazanavir: See prescribing information for atazanavir for dosing information. Nelfinavir: Avoid concomitant use with PREVACID or PREVACID SoluTab. See prescribing information for nelfinavir. Saquinavir: See the prescribing information for saquinavir and monitor for potential saquinavir toxicities. Other antiretrovirals: See prescribing information. |
| Warfarin | |
| Clinical Impact: | Increased INR and prothrombin time in patients receiving PPIs and warfarin concomitantly. Increases in INR and prothrombin time may lead to abnormal bleeding and even death. |
| Intervention: | Monitor INR and prothrombin time. Dose adjustment of warfarin may be needed to maintain target INR range. See prescribing information for warfarin. |
| Methotrexate | |
| Clinical Impact: | Concomitant use of PPIs with methotrexate (primarily at high dose) may elevate and prolong serum concentrations of methotrexate and/or its metabolite hydroxymethotrexate, possibly leading to methotrexate toxicities. No formal drug interaction studies of high-dose methotrexate with PPIs have been conducted [see Warnings and Precautions (5.10)]. |
| Intervention: | A temporary withdrawal of PREVACID or PREVACID SoluTab may be considered in some patients receiving high-dose methotrexate. |
| Digoxin | |
| Clinical Impact: | Potential for increased exposure of digoxin. |
| Intervention: | Monitor digoxin concentrations. Dose adjustment of digoxin may be needed to maintain therapeutic drug concentrations. See prescribing information for digoxin. |
| Theophylline | |
| Clinical Impact: | Increased clearance of theophylline [see Clinical Pharmacology (12.3)]. |
| Intervention: | Individual patients may require additional titration of their theophylline dosage when PREVACID or PREVACID SoluTab is started or stopped to ensure clinically effective blood concentrations. |
| Drugs Dependent on Gastric pH for Absorption (e.g., iron salts, erlotinib, dasatinib, nilotinib, mycophenolate mofetil, ketoconazole/itraconazole) | |
| Clinical Impact: | Lansoprazole can reduce the absorption of other drugs due to its effect on reducing intragastric acidity. |
| Intervention: | Mycophenolate mofetil (MMF): Coadministration of PPIs in healthy subjects and in transplant patients receiving MMF has been reported to reduce the exposure to the active metabolite, mycophenolic acid (MPA), possibly due to a decrease in MMF solubility at an increased gastric pH. The clinical relevance of reduced MPA exposure on organ rejection has not been established in transplant patients receiving PREVACID and MMF. Use PREVACID and PREVACID SoluTab with caution in transplant patients receiving MMF. See the prescribing information for other drugs dependent on gastric pH for absorption. |
| Combination Therapy with Clarithromycin and Amoxicillin | |
| Clinical Impact: | Concomitant administration of clarithromycin with other drugs can lead to serious adverse reactions, including potentially fatal arrhythmias, and are contraindicated. Amoxicillin also has drug interactions. |
| Intervention: |
|
| Tacrolimus | |
| Clinical Impact: | Potentially increased exposure of tacrolimus, especially in transplant patients who are intermediate or poor metabolizers of CYP2C19. |
| Intervention: | Monitor tacrolimus whole blood trough concentrations. Dose adjustment of tacrolimus may be needed to maintain therapeutic drug concentrations. See prescribing information for tacrolimus. |
| Interactions with Investigations of Neuroendocrine Tumors | |
| Clinical Impact: | CgA levels increase secondary to PPI-induced decreases in gastric acidity. The increased CgA level may cause false positive results in diagnostic investigations for neuroendocrine tumors [see Warnings and Precautions (5.9), Clinical Pharmacology (12.2)]. |
| Intervention: | Temporarily stop PREVACID or PREVACID SoluTab treatment at least 14 days before assessing CgA levels and consider repeating the test if initial CgA levels are high. If serial tests are performed (e.g., for monitoring), the same commercial laboratory should be used for testing, as reference ranges between tests may vary. |
| Interaction with Secretin Stimulation Test | |
| Clinical Impact: | Hyper-response in gastrin secretion in response to secretin stimulation test, falsely suggesting gastrinoma. |
| Intervention: | Temporarily stop PREVACID or PREVACID SoluTab treatment at least 28 days before assessing to allow gastrin levels to return to baseline [see Clinical Pharmacology (12.2)]. |
| False Positive Urine Tests for THC | |
| Clinical Impact: | There have been reports of false positive urine screening tests for tetrahydrocannabinol (THC) in patients receiving PPIs. |
| Intervention: | An alternative confirmatory method should be considered to verify positive results. |
| CYP2C19 OR CYP3A4 Inducers | |
| Clinical Impact: | Decreased exposure of lansoprazole when used concomitantly with strong inducers [see Clinical Pharmacology (12.3)]. |
| Intervention: | St John's Wort, rifampin: Avoid concomitant use with PREVACID or PREVACID SoluTab. Ritonavir-containing products: See prescribing information. |
| CYP2C19 or CYP3A4 Inhibitors | |
| Clinical Impact: | Increased exposure of lansoprazole is expected when used concomitantly with strong inhibitors [see Clinical Pharmacology (12.3)]. |
| Intervention: | Voriconazole: See prescribing information. |
| Sucralfate | |
| Clinical Impact: | Decreased and delayed absorption of lansoprazole [see Clinical Pharmacology (12.3)]. |
| Intervention: | Take PREVACID or PREVACID SoluTab at least 30 minutes prior to sucralfate [see Dosage and Administration (2.4)]. |
8. Use In Specific Populations
8.4 Pediatric Use
The safety and effectiveness of PREVACID and PREVACID SoluTab have been established in pediatric patients one year to 17 years of age for short-term treatment of symptomatic GERD and erosive esophagitis.
In clinical studies of symptomatic GERD and erosive esophagitis, PREVACID was not administered beyond 12 weeks in patients one year to 11 years of age. It is not known if PREVACID and PREVACID SoluTab are safe and effective if used longer than the recommended duration. Do not exceed the recommended dose and duration of use in pediatric patients (see Juvenile Animal Toxicity Data).
PREVACID was not effective in pediatric patients with symptomatic GERD one month to less than one year of age in a multicenter, double-blind, placebo - controlled study. Therefore, safety and effectiveness have not been established in patients less than one year of age. Nonclinical studies in juvenile rats have demonstrated an adverse effect of heart valve thickening and bone changes at lansoprazole doses higher than the maximum recommended equivalent human dose.
8.5 Geriatric Use
Of the total number of patients (n=21,486) in clinical studies of PREVACID, 16% of patients were aged 65 years and over, while 4% were 75 years and over. No overall differences in safety or effectiveness were observed between these patients and younger patients and other reported clinical experience has not identified significant differences in responses between geriatric and younger patients, but greater sensitivity of some older individuals cannot be ruled out [see Clinical Pharmacology (12.3)].
8.6 Hepatic Impairment
In patients with various degrees of chronic hepatic impairment the exposure to lansoprazole was increased compared to healthy subjects with normal hepatic function [see Clinical Pharmacology (12.3)]. No dosage adjustment for PREVACID or PREVACID SoluTab is necessary for patients with mild (Child-Pugh Class A) or moderate (Child-Pugh Class B) hepatic impairment. The recommended dosage is 15 mg orally daily in patients with severe hepatic impairment (Child-Pugh Class C) [see Dosage and Administration (2.3)].
10. Overdosage
Lansoprazole is not removed from the circulation by hemodialysis. In one reported overdose, a patient consumed 600 mg of PREVACID with no adverse reaction. Oral lansoprazole doses up to 5000 mg/kg in rats [approximately 1300 times the 30 mg human dose based on body surface area (BSA)] and in mice (about 675.7 times the 30 mg human dose based on BSA) did not produce deaths or any clinical signs.
In the event of over-exposure, treatment should be symptomatic and supportive.
If over-exposure occurs, call your poison control center at 1-800-222-1222 for current information on the management of poisoning or over-exposure.
11. Prevacid Description
The active ingredient in PREVACID Delayed-Release Capsules and PREVACID SoluTab Delayed-Release Orally Disintegrating Tablets is lansoprazole, a substituted benzimidazole, 2-[[[3-methyl-4-(2,2,2-trifluoroethoxy)-2-pyridyl] methyl] sulfinyl] benzimidazole, a compound that inhibits gastric acid secretion. Its empirical formula is C16H14F3N3O2S with a molecular weight of 369.37. Lansoprazole has the following structure:
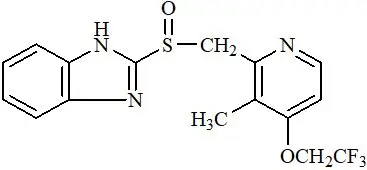
Lansoprazole is a white to brownish-white odorless crystalline powder which melts with decomposition at approximately 166°C. Lansoprazole is freely soluble in dimethylformamide; soluble in methanol; sparingly soluble in ethanol; slightly soluble in ethyl acetate, dichloromethane and acetonitrile; very slightly soluble in ether; and practically insoluble in hexane and water.
Lansoprazole is stable when exposed to light for up to two months. The rate of degradation of the compound in aqueous solution increases with decreasing pH. The degradation half-life of the drug substance in aqueous solution at 25°C is approximately 0.5 hour at pH 5.0 and approximately 18 hours at pH 7.0.
PREVACID is supplied in delayed-release capsules and PREVACID SoluTab is supplied in delayed-release orally disintegrating tablets (SoluTab) for oral administration.
PREVACID is available in one dosage strength: 30 mg of lansoprazole per capsule. Each delayed-release capsule contains enteric-coated granules consisting of 30 mg of lansoprazole (active ingredient) and the following inactive ingredients: sugar sphere, sucrose, methacrylic acid copolymer, low substituted hydroxypropyl cellulose, starch, magnesium carbonate, talc, polyethylene glycol, titanium dioxide, polysorbate 80, hydroxypropyl cellulose, colloidal silicon dioxide, D&C Red No. 28, FD&C Blue No. 1, and FD&C Red No. 40. The 15 mg strength of PREVACID is not currently marketed by Takeda Pharmaceuticals America, Inc.
PREVACID SoluTab is available in two dosage strengths: 15 and 30 mg of lansoprazole per tablet. Each delayed-release orally disintegrating tablet contains enteric-coated microgranules consisting of 15 or 30 mg of lansoprazole (active ingredient) and the following inactive ingredients: mannitol, methacrylic acid, hydroxypropyl cellulose, lactose monohydrate-microcrystalline cellulose sphere, triethyl citrate, crospovidone, polyacrylate, magnesium carbonate, aspartame1, glyceryl monostearate, hypromellose, magnesium stearate, citric acid, titanium dioxide, talc, artificial strawberry flavor, polyethylene glycol, polysorbate 80 and ferric oxide.
- 1
- Phenylketonurics: PREVACID SoluTab Contains Phenylalanine 2.5 mg per 15 mg Tablet and 5.1 mg per 30 mg Tablet.
12. Prevacid - Clinical Pharmacology
12.1 Mechanism of Action
Lansoprazole belongs to a class of antisecretory compounds, the substituted benzimidazoles, that suppress gastric acid secretion by specific inhibition of the (H+, K+)-ATPase enzyme system at the secretory surface of the gastric parietal cell. Because this enzyme system is regarded as the acid (proton) pump within the parietal cell, lansoprazole has been characterized as a gastric acid-pump inhibitor, in that it blocks the final step of acid production. This effect is dose-related and leads to inhibition of both basal and stimulated gastric acid secretion irrespective of the stimulus. Lansoprazole does not exhibit anticholinergic or histamine type-2 antagonist activity.
12.3 Pharmacokinetics
12.4 Microbiology
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In two, 24 month carcinogenicity studies, Sprague-Dawley rats were treated with oral lansoprazole doses of 5 to 150 mg/kg/day, about one to 40 times the exposure on a body surface (mg/m2) basis of a 50 kg person of average height [1.46 m2 body surface area (BSA)] given the recommended human dose of 30 mg/day. Lansoprazole produced dose-related gastric enterochromaffin-like (ECL) cell hyperplasia and ECL cell carcinoids in both male and female rats. It also increased the incidence of intestinal metaplasia of the gastric epithelium in both sexes. In male rats, lansoprazole produced a dose-related increase of testicular interstitial cell adenomas. The incidence of these adenomas in rats receiving doses of 15 to 150 mg/kg/day (four to 40 times the recommended human dose based on BSA) exceeded the low background incidence (range = 1.4 to 10%) for this strain of rat.
In a 24 month carcinogenicity study, CD-1 mice were treated with oral lansoprazole doses of 15 to 600 mg/kg/day, two to 80 times the recommended human dose based on BSA. Lansoprazole produced a dose-related increased incidence of gastric ECL cell hyperplasia. It also produced an increased incidence of liver tumors (hepatocellular adenoma plus carcinoma). The tumor incidences in male mice treated with 300 and 600 mg/kg/day (40 to 80 times the recommended human dose based on BSA) and female mice treated with 150 to 600 mg/kg/day (20 to 80 times the recommended human dose based on BSA) exceeded the ranges of background incidences in historical controls for this strain of mice. Lansoprazole treatment produced adenoma of rete testis in male mice receiving 75 to 600 mg/kg/day (10 to 80 times the recommended human dose based on BSA).
A 26 week p53 (+/-) transgenic mouse carcinogenicity study was not positive.
Lansoprazole was positive in the Ames test and the in vitro human lymphocyte chromosomal aberration assay. Lansoprazole was not genotoxic in the ex vivo rat hepatocyte unscheduled DNA synthesis (UDS) test, the in vivo mouse micronucleus test, or the rat bone marrow cell chromosomal aberration test.
Lansoprazole at oral doses up to 150 mg/kg/day (40 times the recommended human dose based on BSA) was found to have no effect on fertility and reproductive performance of male and female rats.
14. Clinical Studies
14.1 Duodenal Ulcer
In a US multicenter, double-blind, placebo-controlled, dose-response (15, 30, and 60 mg of PREVACID once daily) study of 284 patients with endoscopically documented duodenal ulcer, the percentage of patients healed after two and four weeks was significantly higher with all doses of PREVACID than with placebo. There was no evidence of a greater or earlier response with the two higher doses compared with PREVACID 15 mg. Based on this study and the second study described below, the recommended dose of PREVACID in duodenal ulcer is 15 mg per day (Table 9).
| Week | PREVACID | Placebo (N=72) |
||
|---|---|---|---|---|
| 15 mg daily (N=68) | 30 mg daily (N=74) | 60 mg daily (N=70) |
||
|
||||
| 2 | 42.4%* | 35.6%* | 39.1%* | 11.3% |
| 4 | 89.4%* | 91.7%* | 89.9%* | 46.1% |
PREVACID 15 mg was significantly more effective than placebo in relieving day and nighttime abdominal pain and in decreasing the amount of antacid taken per day.
In a second US multicenter study, also double-blind, placebo-controlled, dose-comparison (15 and 30 mg of PREVACID once daily), and including a comparison with ranitidine, in 280 patients with endoscopically documented duodenal ulcer, the percentage of patients healed after four weeks was significantly higher with both doses of PREVACID than with placebo. There was no evidence of a greater or earlier response with the higher dose of PREVACID. Although the 15 mg dose of PREVACID was superior to ranitidine at four weeks, the lack of significant difference at two weeks and the absence of a difference between 30 mg of PREVACID and ranitidine leaves the comparative effectiveness of the two agents undetermined (Table 10) [see Indications and Usage (1.1)].
| Week | PREVACID | Ranitidine | Placebo (N=41) |
|
|---|---|---|---|---|
| 15 mg daily (N=80) | 30 mg daily (N=77) | 300 mg h.s. (N=82) |
||
|
||||
| 2 | 35.0% | 44.2% | 30.5% | 34.2% |
| 4 | 92.3%* | 80.3%† | 70.5%† | 47.5% |
14.2 Eradication of H. pylori to Reduce the Risk of Duodenal Ulcer Recurrence
Randomized, double-blind clinical studies performed in the US in patients with H. pylori and duodenal ulcer disease (defined as an active ulcer or history of an ulcer within one year) evaluated the efficacy of PREVACID in combination with amoxicillin and clarithromycin as triple 14 day therapy or in combination with amoxicillin as dual 14 day therapy for the eradication of H. pylori. Based on the results of these studies, the safety and efficacy of two different eradication regimens were established:
Triple therapy: PREVACID 30 mg twice daily/amoxicillin 1 g twice daily/clarithromycin 500 mg twice daily
Dual therapy: PREVACID 30 mg three times daily/amoxicillin 1 g three times daily
All treatments were for 14 days. H. pylori eradication was defined as two negative tests (culture and histology) at four to six weeks following the end of treatment.
Triple therapy was shown to be more effective than all possible dual therapy combinations. Dual therapy was shown to be more effective than both monotherapies. Eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence.
A randomized, double-blind clinical study performed in the US in patients with H. pylori and duodenal ulcer disease (defined as an active ulcer or history of an ulcer within one year) compared the efficacy of PREVACID triple therapy for 10 and 14 days. This study established that the 10 day triple therapy was equivalent to the 14 day triple therapy in eradicating H. pylori (Tables 11 and 12) [see Indications and Usage (1.2)].
| Study | Duration | Triple Therapy Evaluable Analysis* | Triple Therapy Intent-to-Treat Analysis† |
|---|---|---|---|
|
|||
| M93-131 | 14 days | 92‡
[80.0-97.7] (N=48) | 86‡
[73.3-93.5] (N=55) |
| M95-392 | 14 days | 86§
[75.7-93.6] (N=66) | 83§
[72.0-90.8] (N=70) |
| M95-399¶ | 14 days | 85 [77.0-91.0] (N=113) | 82 [73.9-88.1] (N=126) |
| 10 days | 84 [76.0-89.8] (N=123) | 81 [73.9-87.6] (N=135) |
|
| Study | Dual Therapy Evaluable Analysis* | Dual Therapy Intent-to-Treat Analysis† |
|---|---|---|
|
||
| M93-131 | 77‡
[62.5-87.2] (N=51) | 70‡
[56.8-81.2] (N=60) |
| M93-125 | 66§
[51.9-77.5] (N=58) | 61§
[48.5-72.9] (N=67) |
14.3 Maintenance of Healed Duodenal Ulcers
PREVACID has been shown to prevent the recurrence of duodenal ulcers. Two independent, double-blind, multicenter, controlled trials were conducted in patients with endoscopically confirmed healed duodenal ulcers. Patients remained healed significantly longer and the number of recurrences of duodenal ulcers was significantly less in patients treated with PREVACID than in patients treated with placebo over a 12 month period (Table 13) [see Indications and Usage (1.3)].
| Trial | Drug | No. of Pts. | Percent in Endoscopic Remission | ||
|---|---|---|---|---|---|
| 0-3 mo. | 0-6 mo. | 0-12 mo. | |||
| %=Life Table Estimate | |||||
|
|||||
| #1 | PREVACID 15 mg daily | 86 | 90%* | 87%* | 84%* |
| Placebo | 83 | 49% | 41% | 39% | |
| #2 | PREVACID 30 mg daily | 18 | 94%* | 94%* | 85%* |
| PREVACID 15 mg daily | 15 | 87%* | 79%* | 70%* | |
| Placebo | 15 | 33% | 0% | 0% | |
In trial #2, no significant difference was noted between PREVACID 15 and 30 mg in maintaining remission.
14.4 Gastric Ulcer
In a US multicenter, double-blind, placebo-controlled study of 253 patients with endoscopically documented gastric ulcer, the percentage of patients healed at four and eight weeks was significantly higher with PREVACID 15 and 30 mg once a day than with placebo (Table 14) [see Indications and Usage (1.4)].
| Week | PREVACID | Placebo (N=64) |
||
|---|---|---|---|---|
| 15 mg daily (N=65) | 30 mg daily (N=63) | 60 mg daily (N=61) |
||
|
||||
| 4 | 64.6%* | 58.1%* | 53.3%* | 37.5% |
| 8 | 92.2%* | 96.8%* | 93.2%* | 76.7% |
Patients treated with any PREVACID dose reported significantly less day and night abdominal pain along with fewer days of antacid use and fewer antacid tablets used per day than the placebo group.
Independent substantiation of the effectiveness of PREVACID 30 mg was provided by a meta-analysis of published and unpublished data.
14.5 Healing of NSAID-Associated Gastric Ulcer
In two US and Canadian multicenter, double-blind, active-controlled studies in patients with endoscopically confirmed NSAID-associated gastric ulcer who continued their NSAID use, the percentage of patients healed after eight weeks was statistically significantly higher with 30 mg of PREVACID than with the active control. A total of 711 patients were enrolled in the study, and 701 patients were treated. Patients ranged in age from 18 to 88 years (median age 59 years), with 67% female patients and 33% male patients. Race was distributed as follows: 87% Caucasian, 8% Black, 5% Other. There was no statistically significant difference between PREVACID 30 mg daily and the active control on symptom relief (i.e., abdominal pain) (Table 15) [see Indications and Usage (1.5)].
|
||
| Study #1 | ||
| PREVACID 30 mg daily | Active Control† | |
| Week 4 | 60% (53/88)‡ | 28% (23/83) |
| Week 8 | 79% (62/79)‡ | 55% (41/74) |
| Study #2 | ||
| PREVACID 30 mg daily | Active Control† | |
| Week 4 | 53% (40/75) | 38% (31/82) |
| Week 8 | 77% (47/61)‡ | 50% (33/66) |
14.6 Risk Reduction of NSAID-Associated Gastric Ulcer
In one large US, multicenter, double-blind, placebo- and misoprostol-controlled (misoprostol blinded only to the endoscopist) study in patients who required chronic use of an NSAID and who had a history of an endoscopically documented gastric ulcer, the proportion of patients remaining free from gastric ulcer at four, eight, and 12 weeks was significantly higher with 15 or 30 mg of PREVACID than placebo. A total of 537 patients were enrolled in the study, and 535 patients were treated. Patients ranged in age from 23 to 89 years (median age 60 years), with 65% female patients and 35% male patients. Race was distributed as follows: 90% Caucasian, 6% Black, 4% Other. The 30 mg dose of PREVACID demonstrated no additional benefit in risk reduction of the NSAID-associated gastric ulcer than the 15 mg dose (Table 16) [see Indications and Usage (1.6)].
| Week | PREVACID 15 mg daily (N=121) | PREVACID 30 mg daily (N=116) | Misoprostol 200 mcg four times daily (N=106) | Placebo (N=112) |
|---|---|---|---|---|
| (p<0.001) PREVACID 15 mg daily vs placebo; PREVACID 30 mg daily vs placebo; and misoprostol 200 mcg four times daily vs placebo. | ||||
| (p<0.05) Misoprostol 200 mcg four times daily vs PREVACID 15 mg daily; and misoprostol 200 mcg four times daily vs PREVACID 30 mg daily. | ||||
|
||||
| 4 | 90% | 92% | 96% | 66% |
| 8 | 86% | 88% | 95% | 60% |
| 12 | 80% | 82% | 93% | 51% |
14.8 Erosive Esophagitis
In a US, multicenter, double-blind, placebo-controlled study of 269 patients entering with an endoscopic diagnosis of esophagitis with mucosal grading of two or more and grades three and four signifying erosive disease, the percentages of patients with healing are presented in Table 18:
| Week | PREVACID | Placebo (N=63) |
||
|---|---|---|---|---|
| 15 mg daily (N=69) | 30 mg daily (N=65) | 60 mg daily (N=72) |
||
|
||||
| 4 | 67.6%* | 81.3%*† | 80.6%*† | 32.8% |
| 6 | 87.7%* | 95.4%* | 94.3%* | 52.5% |
| 8 | 90.9%* | 95.4%* | 94.4%* | 52.5% |
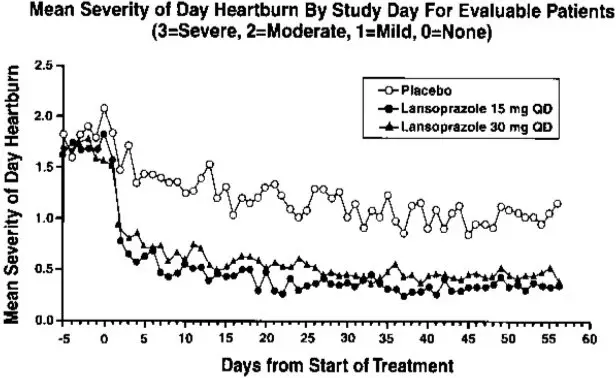
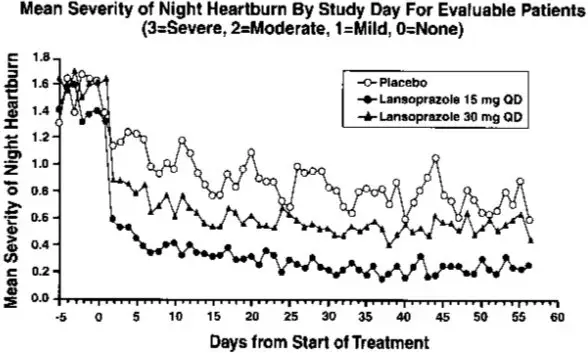
In this study, all PREVACID groups reported significantly greater relief of heartburn and less day and night abdominal pain along with fewer days of antacid use and fewer antacid tablets taken per day than the placebo group. Although all doses were effective, the earlier healing in the higher two doses suggests 30 mg daily as the recommended dose.
PREVACID was also compared in a US, multicenter, double-blind study to a low dose of ranitidine in 242 patients with erosive reflux esophagitis. PREVACID at a dose of 30 mg was significantly more effective than ranitidine 150 mg twice daily as shown below (Table 19).
| Week | PREVACID 30 mg daily (N=115) | Ranitidine 150 mg twice daily (N=127) |
|---|---|---|
|
||
| 2 | 66.7%* | 38.7% |
| 4 | 82.5%* | 52.0% |
| 6 | 93.0%* | 67.8% |
| 8 | 92.1%* | 69.9% |
In addition, patients treated with PREVACID reported less day and nighttime heartburn and took less antacid tablets for fewer days than patients taking ranitidine 150 mg twice daily.
Although this study demonstrates effectiveness of PREVACID in healing erosive esophagitis, it does not represent an adequate comparison with ranitidine because the recommended ranitidine dose for esophagitis is 150 mg four times daily, twice the dose used in this study.
In the two trials described and in several smaller studies involving patients with moderate to severe erosive esophagitis, PREVACID produced healing rates similar to those shown above.
In a US, multicenter, double-blind, active-controlled study, 30 mg of PREVACID was compared with ranitidine 150 mg twice daily in 151 patients with erosive reflux esophagitis that was poorly responsive to a minimum of 12 weeks of treatment with at least one H2-receptor antagonist given at the dose indicated for symptom relief or greater, namely, cimetidine 800 mg/day, ranitidine 300 mg/day, famotidine 40 mg/day or nizatidine 300 mg/day. PREVACID 30 mg was more effective than ranitidine 150 mg twice daily in healing reflux esophagitis, and the percentage of patients with healing were as follows. This study does not constitute a comparison of the effectiveness of histamine H2-receptor antagonists with PREVACID, as all patients had demonstrated unresponsiveness to the histamine H2-receptor antagonist mode of treatment. It does indicate, however, that PREVACID may be useful in patients failing on a histamine H2-receptor antagonist (Table 20) [see Indications and Usage (1.7)].
| Week | PREVACID 30 mg daily (N=100) | Ranitidine 150 mg twice daily (N=51) |
|---|---|---|
|
||
| 4 | 74.7%* | 42.6% |
| 8 | 83.7%* | 32.0% |
14.9 Maintenance of Healing of Erosive Esophagitis
Two independent, double-blind, multicenter, controlled trials were conducted in patients with endoscopically confirmed healed esophagitis. Patients remained in remission significantly longer and the number of recurrences of erosive esophagitis was significantly less in patients treated with PREVACID than in patients treated with placebo over a 12 month period (Table 21).
| Percent in Endoscopic Remission | |||||
|---|---|---|---|---|---|
| Trial | Drug | No. of Pts. | 0-3 mo. | 0-6 mo. | 0-12 mo. |
| %=Life Table Estimate | |||||
|
|||||
| #1 | PREVACID 15 mg daily | 59 | 83%* | 81%* | 79%* |
| PREVACID 30 mg daily | 56 | 93%* | 93%* | 90%* | |
| Placebo | 55 | 31% | 27% | 24% | |
| #2 | PREVACID 15 mg daily | 50 | 74%* | 72%* | 67%* |
| PREVACID 30 mg daily | 49 | 75%* | 72%* | 55%* | |
| Placebo | 47 | 16% | 13% | 13% | |
Regardless of initial grade of erosive esophagitis, PREVACID 15 and 30 mg were similar in maintaining remission.
In a US, randomized, double-blind study, PREVACID 15 mg daily (n=100) was compared with ranitidine 150 mg twice daily (n=106), at the recommended dosage, in patients with endoscopically-proven healed erosive esophagitis over a 12 month period. Treatment with PREVACID resulted in patients remaining healed (Grade 0 lesions) of erosive esophagitis for significantly longer periods of time than those treated with ranitidine (p<0.001). In addition, PREVACID was significantly more effective than ranitidine in providing complete relief of both daytime and nighttime heartburn. Patients treated with PREVACID remained asymptomatic for a significantly longer period of time than patients treated with ranitidine [see Indications and Usage (1.9)].
14.10 Pathological Hypersecretory Conditions Including Zollinger-Ellison Syndrome
In open studies of 57 patients with pathological hypersecretory conditions, such as Zollinger-Ellison syndrome (ZES) with or without multiple endocrine adenomas, PREVACID significantly inhibited gastric acid secretion and controlled associated symptoms of diarrhea, anorexia and pain. Doses ranging from 15 mg every other day to 180 mg per day maintained basal acid secretion below 10 mEq/hr in patients without prior gastric surgery and below 5 mEq/hr in patients with prior gastric surgery.
Initial doses were titrated to the individual patient need, and adjustments were necessary with time in some patients [see Dosage and Administration (2.1)]. PREVACID was well-tolerated at these high-dose levels for prolonged periods (greater than four years in some patients). In most ZES patients, serum gastrin levels were not modified by PREVACID. However, in some patients, serum gastrin increased to levels greater than those present prior to initiation of lansoprazole therapy [see Indications and Usage (1.10)].
16. How is Prevacid supplied
PREVACID 15 mg strength is not currently marketed by Takeda Pharmaceuticals America, Inc.
PREVACID 30 mg delayed-release capsules are opaque, pink and black with "TAP" and "PREVACID 30" imprinted on the capsules. They are available as follows:
| NDC Number | Size |
|---|---|
| 64764-046-13 | Bottles of 100: 30 mg capsules |
PREVACID SoluTab delayed-release orally disintegrating tablets, 15 mg, are white to yellowish white, round uncoated tablets containing orange to dark brown speckles, with "15" debossed on one side of the tablet. The 30 mg are white to yellowish white, round uncoated tablets containing orange to dark brown speckles, with "30" debossed on one side of the tablet. The tablets are available as follows:
| NDC Number | Size |
|---|---|
| 64764-543-11 | Unit dose packages of 100: 15 mg tablets |
| 64764-544-11 | Unit dose packages of 100: 30 mg tablets |
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Medication Guide and Instructions for Use).
Advise patients to:
| MEDICATION GUIDE PREVACID (prev-a-sid) (lansoprazole) delayed-release capsules, for oral use and PREVACID SoluTab (prev-a-sid sol-u-tab) (lansoprazole) delayed-release orally disintegrating tablets |
|
|---|---|
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised: 8/2023 |
| What is the most important information that I should know about PREVACID and PREVACID SoluTab? | |
| You should take PREVACID and PREVACID SoluTab exactly as prescribed, at the lowest dose possible and for the shortest time needed. | |
| PREVACID and PREVACID SoluTab may help your acid-related symptoms, but you could still have serious stomach problems. Talk with your doctor. | |
| PREVACID and PREVACID SoluTab can cause serious side effects, including: | |
|
|
| Talk to your doctor about your risk of these serious side effects. | |
| PREVACID and PREVACID SoluTab can have other serious side effects. See "What are the possible side effects of PREVACID and PREVACID SoluTab?" . | |
| What are PREVACID and PREVACID SoluTab? | |
| A prescription medicine called a proton pump inhibitor (PPI) used to reduce the amount of acid in your stomach. | |
| In adults, PREVACID and PREVACID SoluTab are used for: | |
|
|
| Children: | |
| Give PREVACID and PREVACID SoluTab exactly as prescribed by your child's doctor. Do not increase the dose of PREVACID and PREVACID SoluTab or give your child PREVACID and PREVACID SoluTab longer than the amount of time your doctor tells you to. | |
| In children 1 to 11 years of age, PREVACID and PREVACID SoluTab are used for: | |
|
|
| In children 12 to 17 years of age, PREVACID and PREVACID SoluTab are used for: | |
|
|
| PREVACID and PREVACID SoluTab are not recommended for treating the symptoms of GERD in children less than 1 year of age and may harm them. | |
| Do not take PREVACID or PREVACID SoluTab if you are: | |
|
|
| Before you take PREVACID or PREVACID SoluTab, tell your doctor about all of your medical conditions, including if you: | |
|
|
| Tell your doctor about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Especially tell your doctor if you take methotrexate (OTREXUP, RASUVO, TREXALL, REDITREX, XATMEP). | |
| How should I take PREVACID and PREVACID SoluTab? | |
|
|
|
|
| What are the possible side effects of PREVACID and PREVACID SoluTab? | |
| PREVACID and PREVACID SoluTab can cause serious side effects, including: | |
|
|
| The most common side effects of PREVACID and PREVACID SoluTab include: diarrhea, stomach-area (abdomen) pain, nausea and constipation. | |
| These are not all the possible side effects of PREVACID and PREVACID SoluTab. | |
| Call your doctor for medical advice about side effects. | |
| You may report side effects to FDA at 1-800-FDA-1088. | |
| How should I store PREVACID and PREVACID SoluTab? | |
| Store PREVACID at room temperature between 68°F to 77°F (20°C to 25°C). | |
| Keep PREVACID and PREVACID SoluTab and all medicines out of the reach of children. | |
| General information about the safe and effective use of PREVACID and PREVACID SoluTab. | |
| Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use PREVACID or PREVACID SoluTab for conditions for which it was not prescribed. Do not give PREVACID or PREVACID SoluTab to other people, even if they have the same symptoms that you have. It may harm them. You can ask your doctor or pharmacist for information about PREVACID and PREVACID SoluTab that is written for health professionals. | |
| What are the ingredients in PREVACID and PREVACID SoluTab? | |
| Active ingredient: lansoprazole. | |
| Inactive ingredients in PREVACID capsules: sugar sphere, sucrose, methacrylic acid copolymer, low substituted hydroxypropyl cellulose, starch, magnesium carbonate, talc, polyethylene glycol, titanium dioxide, polysorbate 80, hydroxypropyl cellulose, colloidal silicon dioxide, D&C Red No. 28, FD&C Blue No. 1, and FD&C Red No. 40. | |
| Inactive ingredients in PREVACID SoluTab: mannitol, methacrylic acid, hydroxypropyl cellulose, lactose monohydrate-microcrystalline cellulose sphere, triethyl citrate, crospovidone, polyacrylate, magnesium carbonate, aspartame, glyceryl monostearate, hypromellose, magnesium stearate, citric acid, titanium dioxide, talc, artificial strawberry flavor, polyethylene glycol, polysorbate 80 and ferric oxide. | |
| PREVACID SoluTab contains 2.5 mg of phenylalanine in each 15 mg tablet and 5.1 mg of phenylalanine in each 30 mg tablet. | |
| Distributed by: Takeda Pharmaceuticals America, Inc., Lexington, MA 02421 | |
| PREVACID is a trademark registered in the U.S. Patent and Trademark Office and SoluTab is a trademark of Takeda Pharmaceuticals U.S.A., Inc. and used under license by Takeda Pharmaceuticals America, Inc. All other trademark names are the property of their respective owners. ©1995 – 2023 Takeda Pharmaceuticals America, Inc. |
|
| For more information go to www.PREVACID.com or call 1-877- TAKEDA-7 (1-877- 825- 3327). | |
INSTRUCTIONS FOR USE PREVACID (prev-a-sid) (lansoprazole) delayed-release capsules, for oral use and PREVACID SoluTab (prev-a-sid sol-u-tab) (lansoprazole) delayed-release orally disintegrating tablets
Important:
- Take PREVACID or PREVACID SoluTab before meals.
- Do not crush or chew PREVACID capsules or PREVACID SoluTab.
- PREVACID or PREVACID SoluTab should only be used with the foods and juices listed below.
PREVACID delayed-release capsules (PREVACID capsules)
Taking PREVACID capsules with certain foods:
You can only use applesauce, ENSURE pudding, cottage cheese, yogurt or strained pears.
- Open the capsule.
- Sprinkle the granules on 1 tablespoon of applesauce, ENSURE pudding, cottage cheese, yogurt or strained pears.
- Swallow right away.
Taking PREVACID capsules with certain juices:
You can only use apple juice, orange juice or tomato juice.
- Open the capsule.
- Sprinkle the granules into 60 mL (about ¼ cup) of apple juice, orange juice or tomato juice.
- Stir.
- Swallow right away.
- To make sure that the entire dose is taken, add 1/2 cup or more of juice to the glass, stir and swallow right away.
Giving PREVACID capsules through a nasogastric tube (NG tube) size 16 French or larger:
You can only use apple juice.
- Place 40 mL of apple juice into a clean container.
- Open the capsule and empty the granules into the container of apple juice.
- Use a catheter-tip syringe to draw up the apple juice and granule mixture.
- Gently mix the catheter-tip syringe to keep the granules from settling.
- Attach the catheter-tip syringe to the NG tube.
- Give the mixture right away through the NG tube that goes into the stomach. Do not save the apple juice and granule mixture for later use.
- Refill the catheter-tip syringe with 40 mL of apple juice and mix gently. Flush the NG tube with apple juice.
PREVACID SoluTab Delayed-Release Orally Disintegrating Tablets (PREVACID SoluTab)
- Do not chew, crush, cut or break the tablets.
- Put the tablet on the tongue and let it dissolve, with or without water.
- Swallow after the tablet dissolves.
- The tablet usually dissolves in less than 1 minute.
For patients who have trouble swallowing tablets, PREVACID SoluTab can be given as follows:
Giving PREVACID SoluTab with water using an oral syringe:
- Put a 15 mg tablet in an oral syringe and draw up 4 mL of water into the oral syringe, or put a 30 mg tablet in an oral syringe and draw up 10 mL of water into the oral syringe.
- Gently shake the oral syringe to mix the tablet and the water.
- After the tablet is mixed in the water, place the tip of the oral syringe in the mouth. Give the medicine within 15 minutes of mixing. Do not save the tablet and water mixture for later use.
- Refill the oral syringe with about 2 mL of water for the 15 mg tablet or 5 mL of water for the 30 mg tablet, and shake gently. Place the tip of the oral syringe in the mouth and give the medicine that is left in the syringe.
Giving PREVACID SoluTab with water through a nasogastric tube (NG tube) size 8 French or larger:
- Put a 15 mg tablet in a catheter-tip syringe and draw up 4 mL of water, or put a 30 mg tablet in a catheter-tip syringe and draw up 10 mL of water.
- Gently shake the catheter-tip syringe to mix the tablet and the water.
- Connect the catheter-tip syringe to the NG tube.
- Give the mixture right away through the NG tube that goes into the stomach. Give the medicine within 15 minutes of mixing. Do not save the granule and water mixture for later use.
- Refill the catheter-tip syringe with about 5 mL of water and shake gently. Flush the NG tube with the water.
How should I store PREVACID and PREVACID SoluTab?
- Store PREVACID capsules and PREVACID SoluTab at room temperature between 68°F to 77°F (20°C to 25°C).
Keep PREVACID and PREVACID SoluTab and all medicines out of the reach of children.
This Instruction for Use has been approved by the U.S. Food and Drug Administration.
Distributed by:
Takeda Pharmaceuticals America, Inc.
Lexington, MA 02421
Revised: October 2017
PREVACID is a trademark registered in the U.S. Patent and Trademark Office and SoluTab is a trademark of Takeda Pharmaceuticals U.S.A., Inc. and used under license by Takeda Pharmaceuticals America, Inc.
All other trademark names are the property of their respective owners.
©1995 – 2023 Takeda Pharmaceuticals America, Inc.
PRV012 R56
PRINCIPAL DISPLAY PANEL - 15 mg Capsule Bottle Label
NDC 64764-541-30
30 Capsules
PREVACID®
LANSOPRAZOLE
DELAYED-RELEASE
CAPSULES
15 mg
Dispense the accompanying
Medication Guide to each patient.

PRINCIPAL DISPLAY PANEL - 30 mg Capsule Bottle Label
NDC 64764-046-13
100 Capsules
PREVACID®
LANSOPRAZOLE
DELAYED-RELEASE CAPSULES
30 mg
Dispense the accompanying
Medication Guide to each patient.
Takeda
Rx only

| PREVACID
lansoprazole capsule, delayed release |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| PREVACID
lansoprazole capsule, delayed release |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| PREVACID SOLUTAB
lansoprazole tablet, orally disintegrating, delayed release |
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
| PREVACID SOLUTAB
lansoprazole tablet, orally disintegrating, delayed release |
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||||||
| Labeler - Takeda Pharmaceuticals America, Inc. (039997266) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Bushu Pharmaceuticals, Ltd. | 693460169 | ANALYSIS(64764-046) , MANUFACTURE(64764-046) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Sharp Packaging Services, LLC | 002346625 | LABEL(64764-543, 64764-544) , PACK(64764-543, 64764-544) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Catalent Pharma Solutions, LLC | 014167995 | LABEL(64764-541, 64764-046) , PACK(64764-541, 64764-046) | |