Drug Detail:Prevnar 13 (Pneumococcal 13-valent conjugate vaccine [ noo-moe-kok-al-13-vay-lent-kon-joo-gate-vax-een ])
Drug Class: Bacterial vaccines
Related/similar drugs
Pneumovax 23, Prevnar 13, Prevnar 20, pneumococcal 13-valent vaccine, VaxneuvancePrevnar - Clinical Pharmacology
Results of Clinical Evaluations
Efficacy Against Invasive Disease
| Prevnar®
Number of Cases | Control* Number of Cases | Efficacy | 95% CI | |
|---|---|---|---|---|
| Vaccine serotypes | ||||
| Per protocol | 0 | 17 | 100% | 75.4, 100 |
| Intent-to-treat | 0 | 22 | 100% | 81.7, 100 |
| All pneumococcal serotypes | ||||
| Per protocol | 2 | 20 | 90.0% | 58.3, 98.9 |
| Intent-to-treat | 3 | 27† | 88.9% | 63.8, 97.9 |
| * Investigational meningococcal group C conjugate vaccine (MnCC). † Includes one case in an immunocompromised subject. |
||||
Efficacy Against Otitis Media
| Per Protocol | Intent-to-Treat | |||
|---|---|---|---|---|
| Vaccine Efficacy Estimate* | 95% Confidence Interval | Vaccine Efficacy Estimate* | 95% Confidence Interval |
|
| Finnish Trial | N=1632 | N=1662 | ||
| AOM due to Vaccine Serotypes | 57% | 44, 67 | 54% | 41, 64 |
| All culture-confirmed pneumococcal AOM regardless of serotype | 34% | 21, 45 | 32% | 19, 42 |
| NCKP Trial | N=23,746 | N=34,146 | ||
| All Otitis Media Episodes regardless of etiology† | 7% | 4, 10 | 6% | 4, 9 |
| * All vaccine efficacy estimates in the table are statistically significant. † The vaccine efficacy against all AOM episodes in the Finnish trial, while not reaching statistical significance, was 6% (95% CI: -4, 16) in the per protocol population and 4% (95% CI: -7, 14) in the intent-to-treat population. |
||||
Immunogenicity
Routine Schedule
| Serotype | Post dose 3 GMC†
(95% CI for Prevnar®) | Post dose 4 GMC‡
(95% CI for Prevnar®) |
||
|---|---|---|---|---|
| Prevnar®§ | Control* | Prevnar®§ | Control* | |
| N=88 | N=92 | N=68 | N=61 | |
| 4 | 1.46 (1.19, 1.78) | 0.03 | 2.38 (1.88, 3.03) | 0.04 |
| 6B | 4.70 (3.59, 6.14) | 0.08 | 14.45 (11.17, 18.69) | 0.17 |
| 9V | 1.99 (1.64, 2.42) | 0.05 | 3.51 (2.75, 4.48) | 0.06 |
| 14 | 4.60 (3.70, 5.74) | 0.05 | 6.52 (5.18, 8.21) | 0.06 |
| 18C | 2.16 (1.73, 2.69) | 0.04 | 3.43 (2.70, 4.37) | 0.07 |
| 19F | 1.39 (1.16, 1.68) | 0.09 | 2.07 (1.66, 2.57) | 0.18 |
| 23F | 1.85 (1.46, 2.34) | 0.05 | 3.82 (2.85, 5.11) | 0.09 |
| * Control was investigational meningococcal group C conjugate vaccine (MnCC). † Mean age of Prevnar® group was 7.8 months and of control group was 7.7 months. N is slightly less for some serotypes in each group. ‡ Mean age of Prevnar® group was 14.2 months and of control group was 14.4 months. N is slightly less for some serotypes in each group. § p<0.001 when Prevnar® compared to control for each serotype using a Wilcoxon's test. |
||||
| Efficacy Study | Manufacturing Bridging Study | |||
|---|---|---|---|---|
| Serotype | Post dose 3 GMC‡
(95% CI for Prevnar®) | Post dose 3 GMC§
(95% CI for Prevnar®) |
||
| Prevnar® ll | Control* | Prevnar® ll | Control* | |
| N=32 | N=32 | N=159 | N=83 | |
| 4 | 1.47 (1.08, 2.02) | 0.02 | 2.03 (1.75, 2.37) | 0.02 |
| 6B | 2.18 (1.20, 3.96) | 0.06 | 2.97 (2.43, 3.65) | 0.07 |
| 9V | 1.52 (1.04, 2.22) | 0.04 | 1.18 (1.01, 1.39) | 0.04 |
| 14 | 5.05 (3.32, 7.70) | 0.04 | 4.64 (3.80, 5.66) | 0.04 |
| 18C | 2.24 (1.65, 3.02) | 0.04 | 1.96 (1.66, 2.30) | 0.04 |
| 19F | 1.54 (1.09, 2.17) | 0.10 | 1.91 (1.63, 2.25) | 0.08 |
| 23F | 1.48 (0.97, 2.25) | 0.05 | 1.71 (1.44, 2.05) | 0.05 |
| * Control in efficacy study was investigational meningococcal group C conjugate vaccine (MnCC) and in Manufacturing Bridging Study was concomitant vaccines only. † Sufficient data are not available to reliably assess GMCs following 4 doses of Prevnar® when administered with DTaP in the NCKP efficacy study. ‡ Mean age of the Prevnar® group was 7.4 months and of the control group was 7.6 months. N is slightly less for some serotypes in each group. § Mean age of the Prevnar® group and the control group was 7.2 months. ll p<0.001 when Prevnar® compared to control for each serotype using a Wilcoxon's test in the efficacy study and two-sample t-test in the Manufacturing Bridging Study. |
||||
Previously Unvaccinated Older Infants and Children
| Age group, Vaccinations | Study | Sample Size(s) | 4 | 6B | 9V | 14 | 18C | 19F | 23F |
|---|---|---|---|---|---|---|---|---|---|
| 7-11 mo. 3 doses | 118-12 | 22 | 2.34 | 3.66 | 2.11 | 9.33 | 2.31 | 1.60 | 2.50 |
| 118-16 | 39 | 3.60 | 4.63 | 2.04 | 5.48 | 1.98 | 2.15 | 1.93 | |
| 12-17 mo. 2 doses | 118-15* | 82-84† | 3.91 | 4.67 | 1.94 | 6.92 | 2.25 | 3.78 | 3.29 |
| 118-18 | 33 | 7.02 | 4.25 | 3.26 | 6.31 | 3.60 | 3.29 | 2.92 | |
| 18-23 mo. 2 doses | 118-15* | 52-54† | 3.36 | 4.92 | 1.80 | 6.69 | 2.65 | 3.17 | 2.71 |
| 118-18 | 45 | 6.85 | 3.71 | 3.86 | 6.48 | 3.42 | 3.86 | 2.75 | |
| 24-35 mo. 1 dose | 118-18 | 53 | 5.34 | 2.90 | 3.43 | 1.88 | 3.03 | 4.07 | 1.56 |
| 36-59 mo. 1 dose | 118-18 | 52 | 6.27 | 6.40 | 4.62 | 5.95 | 4.08 | 6.37 | 2.95 |
| 5-9 yrs. 1 dose | 118-18 | 101 | 6.92 | 20.84 | 7.49 | 19.32 | 6.72 | 12.51 | 11.57 |
| 118-8, DTaP | Post dose 3 | 31-32† | 1.47 | 2.18 | 1.52 | 5.05 | 2.24 | 1.54 | 1.48 |
| Bold = GMC not inferior to 118-8, DTaP post dose 3 (one-sided lower limit of the 95% CI of GMC ratio ≥0.50). * Study in Navajo and Apache populations. † Numbers vary with serotype. |
|||||||||
Indications and Usage for Prevnar
(See CLINICAL PHARMACOLOGY for estimates of efficacy against invasive disease and otitis media).
For additional information on usage, see DOSAGE AND ADMINISTRATION.
This vaccine is not intended to be used for treatment of active infection.
Contraindications
Hypersensitivity to any component of the vaccine, including diphtheria toxoid, is a contraindication to use of this vaccine.
Precautions
Prevnar® is for intramuscular use only. Prevnar® SHOULD UNDER NO CIRCUMSTANCES BE ADMINISTERED INTRAVENOUSLY. The safety and immunogenicity for other routes of administration (eg, subcutaneous) have not been evaluated.
Fever, and rarely febrile seizure, have been reported in children receiving Prevnar®. For children at higher risk of seizures than the general population, appropriate antipyretics (dosed according to respective prescribing information) may be administered around the time of vaccination, to reduce the possibility of post-vaccination fever.
Minor illnesses, such as a mild respiratory infection with or without low-grade fever, are not generally contraindications to vaccination. The decision to administer or delay vaccination because of a current or recent febrile illness depends largely on the severity of the symptoms and their etiology. The administration of Prevnar should be postponed in subjects suffering from acute severe febrile illness.32,33
General
CARE IS TO BE TAKEN BY THE HEALTHCARE PROFESSIONAL FOR THE SAFE AND EFFECTIVE USE OF THIS PRODUCT.
- PRIOR TO ADMINISTRATION OF ANY DOSE OF THIS VACCINE, THE PARENT OR GUARDIAN SHOULD BE ASKED ABOUT THE PERSONAL HISTORY, FAMILY HISTORY, AND RECENT HEALTH STATUS OF THE VACCINE RECIPIENT. THE HEALTHCARE PROFESSIONAL SHOULD ASCERTAIN PREVIOUS IMMUNIZATION HISTORY, CURRENT HEALTH STATUS, AND OCCURRENCE OF ANY SYMPTOMS AND/OR SIGNS OF AN ADVERSE EVENT AFTER PREVIOUS IMMUNIZATIONS IN THE CHILD TO BE IMMUNIZED, IN ORDER TO DETERMINE THE EXISTENCE OF ANY CONTRAINDICATION TO IMMUNIZATION WITH THIS VACCINE AND TO ALLOW AN ASSESSMENT OF RISKS AND BENEFITS.
- BEFORE THE ADMINISTRATION OF ANY BIOLOGICAL, THE HEALTHCARE PROFESSIONAL SHOULD TAKE ALL PRECAUTIONS KNOWN FOR THE PREVENTION OF ALLERGIC OR ANY OTHER ADVERSE REACTIONS. This should include a review of the patient's history regarding possible sensitivity; the ready availability of epinephrine 1:1000 and other appropriate agents used for control of immediate allergic reactions; and a knowledge of the recent literature pertaining to use of the biological concerned, including the nature of side effects and adverse reactions that may follow its use.
- Children with impaired immune responsiveness, whether due to the use of immunosuppressive therapy (including irradiation, corticosteroids, antimetabolites, alkylating agents, and cytotoxic agents), a genetic defect, HIV infection, or other causes, may have reduced antibody response to active immunization.32,33,34 (See DRUG INTERACTIONS.)
- The use of pneumococcal conjugate vaccine does not replace the use of 23-valent pneumococcal polysaccharide vaccine in children ≥ 24 months of age with sickle cell disease, asplenia, HIV infection, chronic illness or who are immunocompromised. Data on sequential vaccination with Prevnar® followed by 23-valent pneumococcal polysaccharide vaccine are limited. (See PRECAUTIONS, Special Populations)
- Since this product is a suspension containing an aluminum adjuvant, shake vigorously immediately prior to use to obtain a uniform suspension.
- A separate sterile syringe and needle or a sterile disposable unit should be used for each individual to prevent transmission of hepatitis or other infectious agents from one person to another. Needles should be disposed of properly and should not be recapped.
- Special care should be taken to prevent injection into or near a blood vessel or nerve.
DRUG INTERACTIONS
Simultaneous Administration with Other Vaccines
During clinical studies, Prevnar® was administered simultaneously with DTaP and HbOC, IPV, Hep B vaccines, MMR, and Varicella vaccine. Thus, the safety experience with Prevnar® reflects the use of this product as part of the routine immunization schedule.20,21,25,27,28,30
The immune response to routine vaccines when administered with Prevnar® (at separate sites) was assessed in 3 clinical studies in which there was a control group for comparison. Higher antibody levels (GMC) to Hib were observed after 3 doses of HbOC given with Prevnar in the infant series, compared to HbOC without Prevnar. After the 4th dose, Hib GMCs were lower when HbOC was given with Prevnar compared to control; however, over 97% of children receiving HbOC with Prevnar achieved a serum antibody concentration of ≥1 μg/mL. Although some inconsistent differences in response to pertussis antigens were observed, the clinical relevance is unknown. The response to 2 doses of IPV given concomitantly with Prevnar®, assessed 3 months after the second dose, was equivalent to controls for poliovirus Types 2 and 3, but lower for Type 1. In another study, over 98% of subjects achieved neutralizing antibody titers ≥1:8 for all polio types, following a third dose of IPV given concomitantly with Prevnar at 12 months of age.35 Seroresponse rates to measles, mumps and rubella were similar after MMR was given concomitantly with Prevnar at 12 months of age compared to seroresponse rates after MMR was given without Prevnar at 12 months of age.36 A clinical study demonstrated no interference with the immune response to varicella vaccine when administered concurrently with a 4th dose of Prevnar®.37
CARCINOGENESIS, MUTAGENESIS, IMPAIRMENT OF FERTILITY
Prevnar® has not been evaluated for any carcinogenic or mutagenic potential, or impairment of fertility.
Nursing Mothers
It is not known whether vaccine antigens or antibodies are excreted in human milk. This vaccine is not recommended for use in a nursing mother.
GERIATRIC USE
This vaccine is NOT recommended for use in adult populations. It is not to be used as a substitute for the pneumococcal polysaccharide vaccine in geriatric populations.
Adverse Reactions/Side Effects
Pre-Licensure Clinical Trial Experience
| Reaction | Dose 1 | Dose 2 | Dose 3 | Dose 4 | ||||
| Prevnar® Site | DTaP Site | Prevnar® Site | DTaP Site | Prevnar® Site | DTaP Site | Prevnar® Site | DTaP Site‡ | |
| N=693 | N=693 | N=526 | N=526 | N=422 | N=422 | N=165 | N=165 | |
| Erythema | ||||||||
| Any | 10.0 | 6.7§ | 11.6 | 10.5 | 13.8 | 11.4 | 10.9 | 3.6§ |
| >2.4 cm | 1.3 | 0.4§ | 0.6 | 0.6 | 1.4 | 1.0 | 3.6 | 0.6 |
| Induration | ||||||||
| Any | 9.8 | 6.6§ | 12.0 | 10.5 | 10.4 | 10.4 | 12.1 | 5.5§ |
| >2.4 cm | 1.6 | 0.9 | 1.3 | 1.7 | 2.4 | 1.9 | 5.5 | 1.8 |
| Tenderness | ||||||||
| Any | 17.9 | 16.0 | 19.4 | 17.3 | 14.7 | 13.1 | 23.3 | 18.4 |
| Interfered with limb movement | 3.1 | 1.8§ | 4.1 | 3.3 | 2.9 | 1.9 | 9.2 | 8.0 |
| * HbOC was administered in the same limb as Pneumococcal 7-valent Conjugate Vaccine (Diphtheria CRM197 Protein), Prevnar®. If reactions occurred at either or both sites on that limb, the more severe reaction was recorded. † If Hep B vaccine was administered simultaneously, it was administered into the same limb as DTaP. If reactions occurred at either or both sites on that limb, the more severe reaction was recorded. ‡ Subjects may have received DTP or a mixed DTP/DTaP regimen for the primary series. Thus, this is the 4th dose of a pertussis vaccine, but not a 4th dose of DTaP. § p<0.05 when Prevnar® site compared to DTaP site using the sign test. |
||||||||
Table 7 presents the rates of local reactions in previously unvaccinated older infants and children.
| Age at 1st Vaccination | 7 - 11 Mos. | 12 - 23 Mos. | 24 - 35 Mos. | 36 - 59 Mos. | 5 - 9 Yrs. | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study No. | 118-12 | 118-16 | 118-9* | 118-18 | 118-18 | 118-18 | 118-18 | |||||
| Dose Number | 1 | 2 | 3† | 1 | 2 | 3† | 1 | 1 | 2 | 1 | 1 | 1 |
| Number of Subjects | 54 | 51 | 24 | 81 | 76 | 50 | 60 | 114 | 117 | 46 | 48 | 49 |
| Reaction | ||||||||||||
| Erythema | ||||||||||||
| Any | 16.7 | 11.8 | 20.8 | 7.4 | 7.9 | 14.0 | 48.3 | 10.5 | 9.4 | 6.5 | 29.2 | 24.2 |
| >2.4 cm‡ | 1.9 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 6.7 | 1.8 | 1.7 | 0.0 | 8.3 | 7.1 |
| Induration | ||||||||||||
| Any | 16.7 | 11.8 | 8.3 | 7.4 | 3.9 | 10.0 | 48.3 | 8.8 | 6.0 | 10.9 | 22.9 | 25.5 |
| >2.4 cm‡ | 3.7 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 3.3 | 0.9 | 0.9 | 2.2 | 6.3 | 9.3 |
| Tenderness | ||||||||||||
| Any | 13.0 | 11.8 | 12.5 | 8.6 | 10.5 | 12.0 | 46.7 | 25.7 | 26.5 | 41.3 | 58.3 | 82.8 |
| Interfered with limb movement§ | 1.9 | 2.0 | 4.2 | 1.2 | 1.3 | 0.0 | 3.3 | 6.2 | 8.5 | 13.0 | 20.8 | 39.4 |
| * For 118-9, 2 of 60 subjects were ≥24 months of age. † For 118-12, dose 3 was administered at 15 - 18 mos. of age. For 118-16, dose 3 was administered at 12 - 15 mos. of age. ‡ For 118-16 and 118-18, ≥2 cm. § Tenderness interfering with limb movement. |
||||||||||||
| Reaction | Dose 1 | Dose 2 | Dose 3 | Dose 4‡ | ||||
| Prevnar® | Control† | Prevnar® | Control† | Prevnar® | Control† | Prevnar® | Control† | |
| N=710 | N=711 | N=559 | N=508 | N=461 | N=414 | N=224 | N=230 | |
| Fever | ||||||||
| ≥38.0°C | 15.1 | 9.4§ | 23.9 | 10.8§ | 19.1 | 11.8§ | 21.0 | 17.0 |
| >39.0°C | 0.9 | 0.3 | 2.5 | 0.8§ | 1.7 | 0.7 | 1.3 | 1.7 |
| Irritability | 48.0 | 48.2 | 58.7 | 45.3§ | 51.2 | 44.8 | 44.2 | 42.6 |
| Drowsiness | 40.7 | 42.0 | 25.6 | 22.8 | 19.5 | 21.9 | 17.0 | 16.5 |
| Restless Sleep | 15.3 | 15.1 | 20.2 | 19.3 | 25.2 | 19.0§ | 20.2 | 19.1 |
| Decreased Appetite | 17.0 | 13.5 | 17.4 | 13.4 | 20.7 | 13.8§ | 20.5 | 23.1 |
| Vomiting | 14.6 | 14.5 | 16.8 | 14.4 | 10.4 | 11.6 | 4.9 | 4.8 |
| Diarrhea | 11.9 | 8.4§ | 10.2 | 9.3 | 8.3 | 9.4 | 11.6 | 9.2 |
| Urticaria-like Rash | 1.4 | 0.3§ | 1.3 | 1.4 | 0.4 | 0.5 | 0.5 | 1.7 |
| * Approximately 75% of subjects received prophylactic or therapeutic antipyretics within 48 hours of each dose. † Investigational meningococcal group C conjugate vaccine (MnCC). ‡ Most of these children had received DTP for the primary series. Thus, this is a 4th dose of a pertussis vaccine, but not of DTaP. § p<0.05 when Prevnar® compared to control group using a Chi-Square test. |
||||||||
| Reaction | Dose 1 | Dose 2 | Dose 3 | |||
| Prevnar® | Control† | Prevnar® | Control† | Prevnar® | Control† | |
| N=498 | N=108 | N=452 | N=99 | N=445 | N=89 | |
| Fever | ||||||
| ≥38.0°C | 21.9 | 10.2‡ | 33.6 | 17.2‡ | 28.1 | 23.6 |
| >39.0°C | 0.8 | 0.9 | 3.8 | 0.0 | 2.2 | 0.0 |
| Irritability | 59.7 | 60.2 | 65.3 | 52.5‡ | 54.2 | 50.6 |
| Drowsiness | 50.8 | 38.9‡ | 30.3 | 31.3 | 21.2 | 20.2 |
| Decreased Appetite | 19.1 | 15.7 | 20.6 | 11.1‡ | 20.4 | 9.0‡ |
| * Approximately 72% of subjects received prophylactic or therapeutic antipyretics within 48 hours of each dose. † Control group received concomitant vaccines only in the same schedule as the Prevnar® group (DTaP, HbOC at dose 1, 2, 3; IPV at doses 1 and 2; Hep B at doses 1 and 3). ‡ p<0.05 when Prevnar® compared to control group using Fisher's Exact test. |
||||||
| Age at 1st Vaccination | 7 - 11 Mos. | 12 - 23 Mos. | 24 - 35 Mos. | 36 - 59 Mos. | 5 - 9 Yrs. | |||||||
| Study No. | 118-12 | 118-16 | 118-9* | 118-18 | 118-18 | 118-18 | 118-18 | |||||
| Dose Number | 1 | 2 | 3† | 1 | 2 | 3† | 1 | 1 | 2 | 1 | 1 | 1 |
| Number of Subjects | 54 | 51 | 24 | 85 | 80 | 50 | 60 | 120 | 117 | 47 | 52 | 100 |
| Reaction | ||||||||||||
| Fever ≥38.0°C | 20.8 | 21.6 | 25.0 | 17.6 | 18.8 | 22.0 | 36.7 | 11.7 | 6.8 | 14.9 | 11.5 | 7.0 |
| >39.0°C | 1.9 | 5.9 | 0.0 | 1.6 | 3.9 | 2.6 | 0.0 | 4.4 | 0.0 | 4.2 | 2.3 | 1.2 |
| Fussiness | 29.6 | 39.2 | 16.7 | 54.1 | 41.3 | 38.0 | 40.0 | 37.5 | 36.8 | 46.8 | 34.6 | 29.3 |
| Drowsiness | 11.1 | 17.6 | 16.7 | 24.7 | 16.3 | 14.0 | 13.3 | 18.3 | 11.1 | 12.8 | 17.3 | 11.0 |
| Decreased Appetite | 9.3 | 15.7 | 0.0 | 15.3 | 15.0 | 30.0 | 25.0 | 20.8 | 16.2 | 23.4 | 11.5 | 9.0 |
| * For 118-9, 2 of 60 subjects were ≥24 months of age. † For 118-12, dose 3 was administered at 15 - 18 mos. of age. For 118-16, dose 3 was administered at 12 - 15 mos. of age. |
||||||||||||
| Vaccine | <One Week After Immunization | ≤Two Weeks After Immunization | ≤One Month After Immunization | ≤One Year After Immunization | ||||
| Exp | Obs | Exp | Obs | Exp | Obs | Exp | Obs | |
| Prevnar® | 1.06 | 1 | 2.09 | 2 | 4.28 | 2 | 8.08 | 4 |
| Control* | 1.06 | 2 | 2.09 | 3† | 4.28 | 3† | 8.08 | 8† |
| * Investigational meningococcal group C conjugate vaccine (MnCC). † Does not include one additional case of SIDS-like death in a child older than the usual SIDS age (448 days). |
||||||||
| Systemic Event | Prevnar®
Concurrently With DTaP and HbOC (3,848 Doses)† | DTaP and HbOC Control (538 Doses)‡ |
| Fever | ||
| ≥38.0°C | 21.1 | 14.2 |
| >39.0°C | 1.8 | 0.4 |
| Irritability | 52.5 | 45.2 |
| Drowsiness | 32.9 | 27.7 |
| Restless Sleep | 20.6 | 22.3 |
| Decreased Appetite | 18.1 | 13.6 |
| Vomiting | 13.4 | 9.8 |
| Diarrhea | 9.8 | 4.4 |
| Urticaria-like Rash | 0.6 | 0.3 |
| † Total from which reaction data are available varies between reactions from 3,121‑3,848 doses. Data from studies 118-8, 118-12, 118-16. ‡ Total from which reaction data are available varies between reactions from 295-538 doses. Data from studies 118-12 and 118-16. |
||
| Systemic Event | Prevnar®
Concurrently With DTaP and HbOC (270 Doses)† | Prevnar® Only No Concurrent Vaccines (727 Doses) ‡ |
| Fever | ||
| ≥38.0°C | 19.6 | 13.4 |
| >39.0°C | 1.5 | 1.2 |
| Irritability | 45.9 | 45.8 |
| Drowsiness | 17.5 | 15.9 |
| Restless Sleep | 21.2 | 21.2 |
| Decreased Appetite | 21.1 | 18.3 |
| Vomiting | 5.6 | 6.3 |
| Diarrhea | 13.7 | 12.8 |
| Urticaria-like Rash | 0.7 | 1.2 |
| † Total from which reaction data are available varies between reactions from 269-270 doses. Data from studies 118-7 and 118-8. ‡ Total from which reaction data are available varies between reactions from 725-727 doses. Data from studies 118-7 and 118-8. |
||
Postmarketing Experience
Blood and lymphatic system disorders: lymphadenopathy localized to the region of the injection site
Skin and subcutaneous tissue disorders: angioneurotic edema, erythema multiforme
Postmarketing Observational Safety Surveillance Study
Safety outcomes were evaluated in an observational study that included 65,927 infants. Primary safety outcomes analyses included an evaluation of pre-defined adverse events occurring in temporal relationship to immunization. Rates of adverse events occurring within various time periods post-vaccination (e.g., 0-2, 0-7, 0-14, 0-30 days) were compared to the rates of those events occurring within a control time window (i.e., 31-60 days). Secondary safety outcomes analyses included comparisons to a historical control population of infants (1995-1996, N=40,223) prior to the introduction of Prevnar®. In addition, the study included extended follow-up of subjects originally enrolled in the NCKP efficacy trial (N=37,866).
The primary safety outcomes analyses did not demonstrate a consistently elevated risk of healthcare utilization for croup, gastroenteritis, allergic reactions, seizures, wheezing diagnoses, or breath-holding across doses, health care settings, or multiple time windows. As in pre-licensure trials, fever was associated with Prevnar® administration. In analyses of secondary safety outcomes, the adjusted relative risk of hospitalization for reactive airways disease was 1.23 (95% CI: 1.11, 1.35). Potential confounders, such as differences in concomitantly administered vaccines, yearly variation in respiratory infections, or secular trends in reactive airways disease incidence, could not be controlled. Extended follow-up of subjects originally enrolled in the NCKP efficacy trial revealed no increased risk of reactive airways disease among Prevnar® recipients. In general, the study results support the previously described safety profile of Prevnar®.41,42
ADVERSE EVENT REPORTING
The VAERS toll-free number for VAERS forms and information is 800-822-7967.43
Overdosage
There have been reports of overdose with Prevnar®, including cases of administration of a higher than recommended dose and cases of subsequent doses administered closer than recommended to the previous dose. Most individuals were asymptomatic. In general, adverse events reported with overdose have also been reported with recommended single doses of Prevnar®.
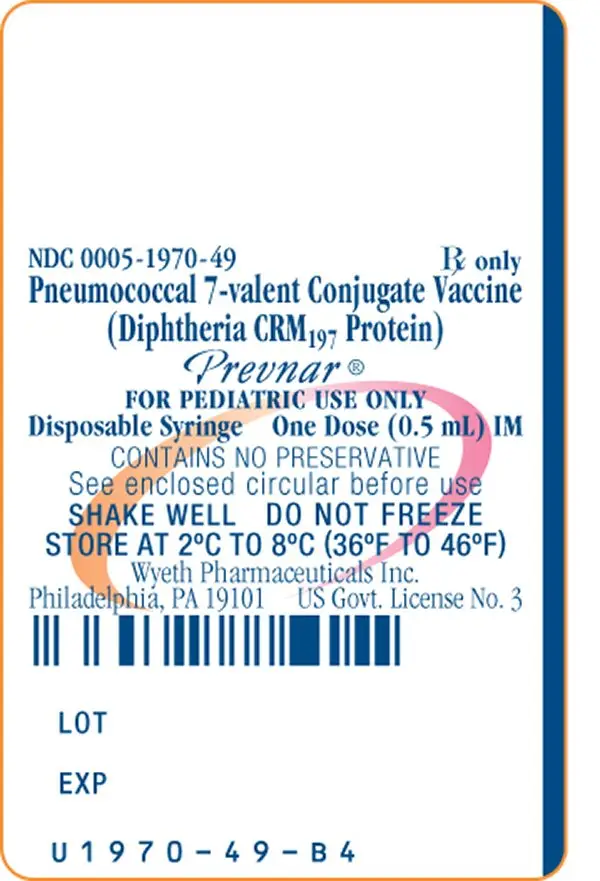
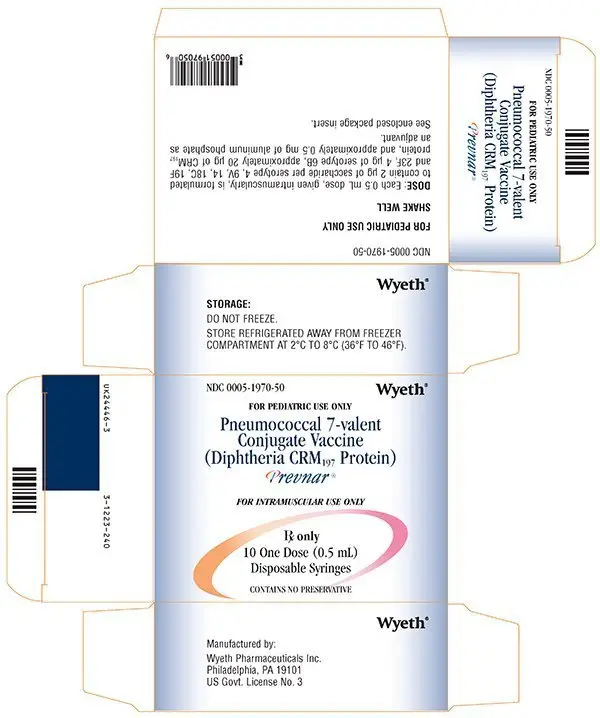
Prevnar Dosage and Administration
For intramuscular injection only. Do not inject intravenously.
The dose is 0.5 mL to be given intramuscularly.
After shaking, the vaccine is a homogeneous, white suspension.
The vaccine is not to be mixed with other vaccines/products in the same syringe.
Vaccine Schedule
| Vaccination schedule for infants and toddlers | ||||
|---|---|---|---|---|
| Dose: | Dose 1*† | Dose 2† | Dose 3† | Dose 4‡ |
| Age at Dose: | 2 months | 4 months | 6 months | 12-15 months |
| * Dose 1 may be given as early as 6 weeks of age. † The recommended dosing interval is 4 to 8 weeks. ‡ The fourth dose should be administered at approximately 12-15 months of age, and at least 2 months after the third dose. |
||||
Previously Unvaccinated Older Infants and Children
| Vaccine schedule for previously unvaccinated children ≥7 months of age | |
|---|---|
| Age at First Dose | Total Number of 0.5 mL Doses |
| 7-11 months of age | 3* |
| 12-23 months of age | 2† |
| ≥24 months through 9 years of age | 1 |
| * 2 doses at least 4 weeks apart; third dose after the one-year birthday, separated from the second dose by at least 2 months. † 2 doses at least 2 months apart. |
|
References
- Schuchat A, Robinson K, Wenger JD, et al. Bacterial meningitis in the United States in 1995. N Engl J Med. 1997; 337:970-6.
- Zangwill KM, Vadheim CM, Vannier AM, et al. Epidemiology of invasive pneumococcal disease in Southern California: implications for the design and conduct of a pneumococcal conjugate vaccine efficacy trial. J Infect Dis. 1996; 174:752-9.
- Breiman R, Spika J, Navarro V, et al. Pneumococcal bacteremia in Charleston County, South Carolina. Arch Intern Med. 1990; 150:1401-5.
- Levine O, Farley M, Harrison LH, et al. Risk factors for invasive pneumococcal disease in children: a population-based case-control study in North America. Pediatrics. 1999; 103:1-5.
- Kaplan SL, Mason EO, Barson WJ, et al. Three-year multicenter surveillance of systemic pneumococcal infections in children. Pediatrics. 1998; 102:538-44.
- Arditi M, Mason E, Bradley J, et al. Three-year multicenter surveillance of pneumococcal meningitis in children: clinical characteristics and outcome related to penicillin susceptibility and dexamethasone use. Pediatrics. 1998; 102:1087-97.
- Shappert SM. Ambulatory care visits to physician offices, hospital outpatient departments, and emergency departments: United States, 1997. National Center for Health Statistics. Vital Health Sat. 1999; 13(143):1-41.
- Hall MJ, Lawrence L. Ambulatory surgery in the United States, 1996. Adv Data Vital Health Stat. 1998; 300:1-16.
- Teele DW, Klein JO, Rosner B, et al. Epidemiology of otitis media during the first seven years of life in children in greater Boston: a prospective, cohort study. J Infect Dis. 1989; 160:83-94.
- Shappert, SM. Office visits for otitis media: United States, 1975-1990. Adv Data Vital Health Stat. 1992; 214:1-20.
- Bluestone CD, Stephenson BS, Martin LM. Ten-year review of otitis media pathogens. Pediatr Infect Dis J. 1992; 11:S7-S11.
- Giebink GS. The microbiology of otitis media. Pediatr Infect Dis J. 1989; 8:S18-S20.
- Rodriguez WJ, Schwartz RH. Streptococcus pneumoniae causes otitis media with higher fever and more redness of tympanic membrane than Haemophilus influenzae or Moraxella catarrhalis. Pediatr Infect Dis J. 1999; 18:942-4.
- Barnett ED, Klein JO. The problem of resistant bacteria for the management of acute otitis media. Ped Clin North Am. 1995; 42:509-17.
- Butler JC, Breiman RF, Lipman HB, et al. Serotype distribution of Streptococcus pneumoniae infections among preschool children in the United States, 1978-1994: implications for development of a conjugate vaccine. J Infect Dis. 1995; 171:885-9.
- Paisley JW, Lauer BA, McIntosh K, et al. Pathogens associated with acute lower respiratory tract infection in young children. Pediatr Infect Dis J. 1984; 3:14-9.
- American Academy of Pediatrics Committee on Infectious Diseases. Therapy for children with invasive pneumococcal infections. Pediatrics. 1997; 99:289-300.
- Hausdorff WP, Bryant J, Paradiso PR, Siber GR. Which pneumococcal serogroups cause the most invasive disease: implications for conjugate vaccine formulation and use, part I. Clin Infect Dis. 2000; 30:100-21.
- Bulter JC, Hoffman J, Cetron MS, et al. The continued emergence of drug-resistant Streptococcus pneumoniae in the United States. An Update from the Centers for Disease Control and Prevention's Pneumococcal Sentinel Surveillance System. J Infect Dis. 1996; 174:986-93.
- Lederle Laboratories, Data on File: D118-P8.
- Black S, Shinefield H, Ray P, et al. Efficacy, safety and immunogenicity of heptavalent pneumococcal conjugate vaccine in children. Pediatr Infect Dis J. 2000; 19:187-195.
- Lederle Laboratories, Data on File: D118-P809.
- Eskola J, Kilpi T, Palma A, et al. Efficacy of a pneumococcal conjugate vaccine against acute otitis media. N Engl J Med. 2001; 344:403-409.
- Fireman B, Black S, Shinefield H, et al. The impact of the pneumococcal conjugate vaccine on otitis media. Pediatr Infect Dis J. 2003;22:10-16.
- Lederle Laboratories, Data on File: D118-P16.
- Lederle Laboratories, Data on File: D118-P8 Addendum DTaP Immunogenicity.
- Shinefield HR, Black S, Ray P. Safety and immunogenicity of heptavalent pneumococcal CRM197 conjugate vaccine in infants and toddlers. Pediatr Infect Dis J. 1999; 18:757-63.
- Lederle Laboratories, Data on File: D118-P12.
- Rennels MD, Edwards KM, Keyserling HL, et al. Safety and immunogenicity of heptavalent pneumococcal vaccine conjugated to CRM197 in United States infants. Pediatrics. 1998; 101(4):604-11.
- Lederle Laboratories, Data on File: D118-P3.
- Lederle Laboratories, Data on File: Integrated Summary on Catch-Up.
- Report of the Committee on Infectious Diseases 24th Edition. Elk Grove Village, IL: American Academy of Pediatrics. 1997; 31-3.
- Update: Vaccine Side Effects, Adverse Reactions, Contraindications, and Precautions. MMWR. 1996; 45 (RR-12):1-35.
- Centers for Disease Control and Prevention. General recommendations on immunization. Recommendations of the Advisory Committee on Immunization Practices (ACIP) and the American Academy of Family Physicians (AAFP). MMWR. 2002; 51(RR-2):1-36.
- Wyeth, Data on file: Final clinical study report D140-P1.
- Wyeth, Data on file: Final clinical study report MMR100495.
- Wyeth, Data on file: Final clinical study report, Addendum MMR100495: Varicella immunogenicity.
- Wyeth, Data on file: Final clinical study report 0887X-100722.
- Vernacchio L, Neufeld EJ, MacDonald K, et al. Combined schedule of 7-valent pneumococcal conjugate vaccine followed by 23-valent pneumococcal vaccine in children and young adults with sickle cell disease. J Pediatr. 1998;103:275-278.
- Fawcett HA, Smith NP. Injection-site granuloma due to aluminum. Archives Dermatology. 1984; 120:1318-22.
- Wyeth, Data on file: Final clinical study report 100494.
- Wyeth, Data on file: Addendum 1: Final clinical study report 100494.
- Vaccines Adverse Event Reporting System – United States. MMWR. 1990; 39:730-3.
 | This product's label may have been updated. For current package insert and further product information, please visit www.wyeth.com or call our medical communications department toll-free at 1-800-934-5556. |  |
| PREVNAR
pneumococcal 7-valent injection, suspension |
|||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||
| Labeler - Wyeth Pharmaceutical Division of Wyeth Holdings Corporation, a subsidiary of Pfizer Inc. (054065909) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Wyeth Pharmaceutical Division of Wyeth Holdings Corporation, a subsidiary of Pfizer Inc. | 054065909 | ANALYSIS, API MANUFACTURE, MANUFACTURE | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Wyeth Pharmaceutical Division of Wyeth Holdings Corporation, a subsidiary of Pfizer Inc. | 883534067 | MANUFACTURE, ANALYSIS, API MANUFACTURE | |