Drug Detail:Rhogam ultra-filtered plus (Rho (d) immune globulin [ roe-d-im-myoon-glob-yoo-lin ])
Drug Class: Immune globulins
Highlights of Prescribing Information
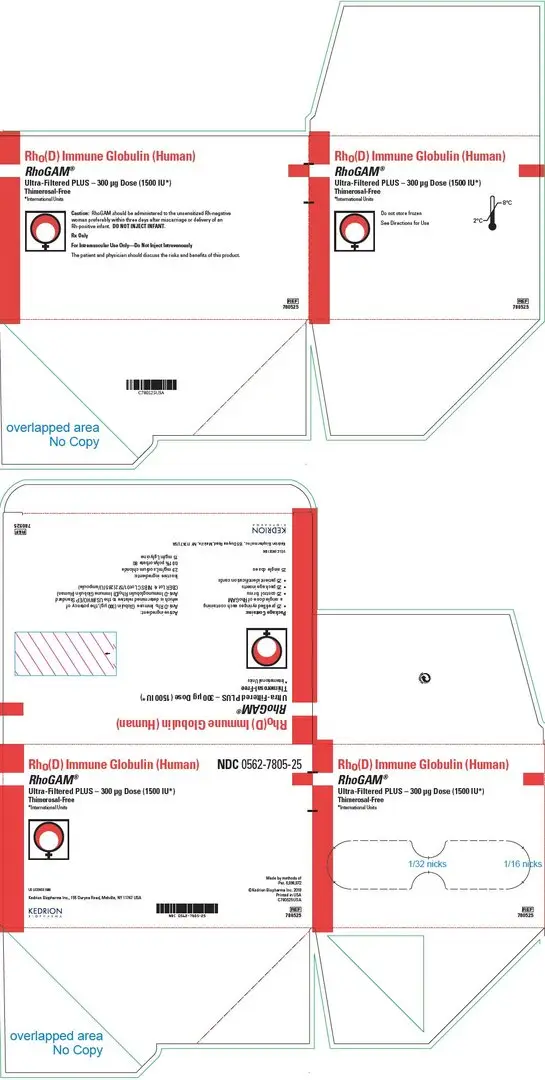
RhoGAM® Ultra-Filtered PLUS [Rho(D) Immune Globulin (Human)] (300 μg) (1500 IU), prefilled syringe, for intramuscular use
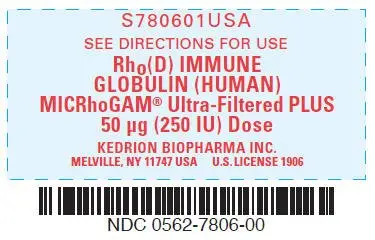
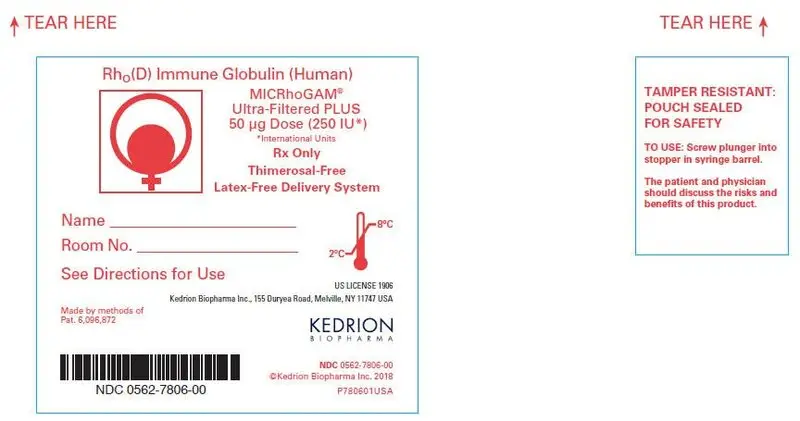
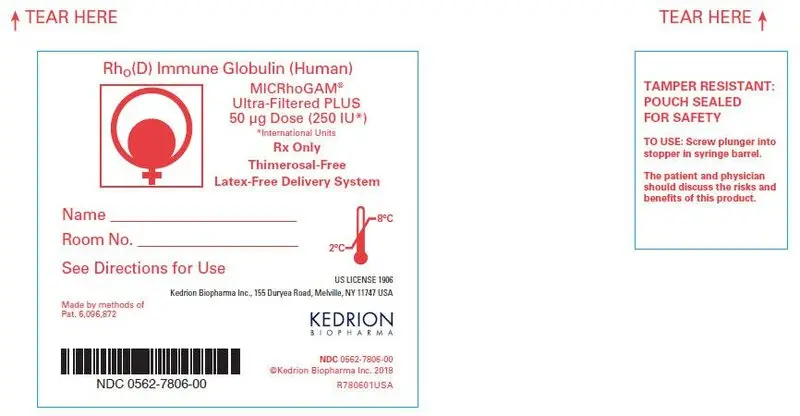
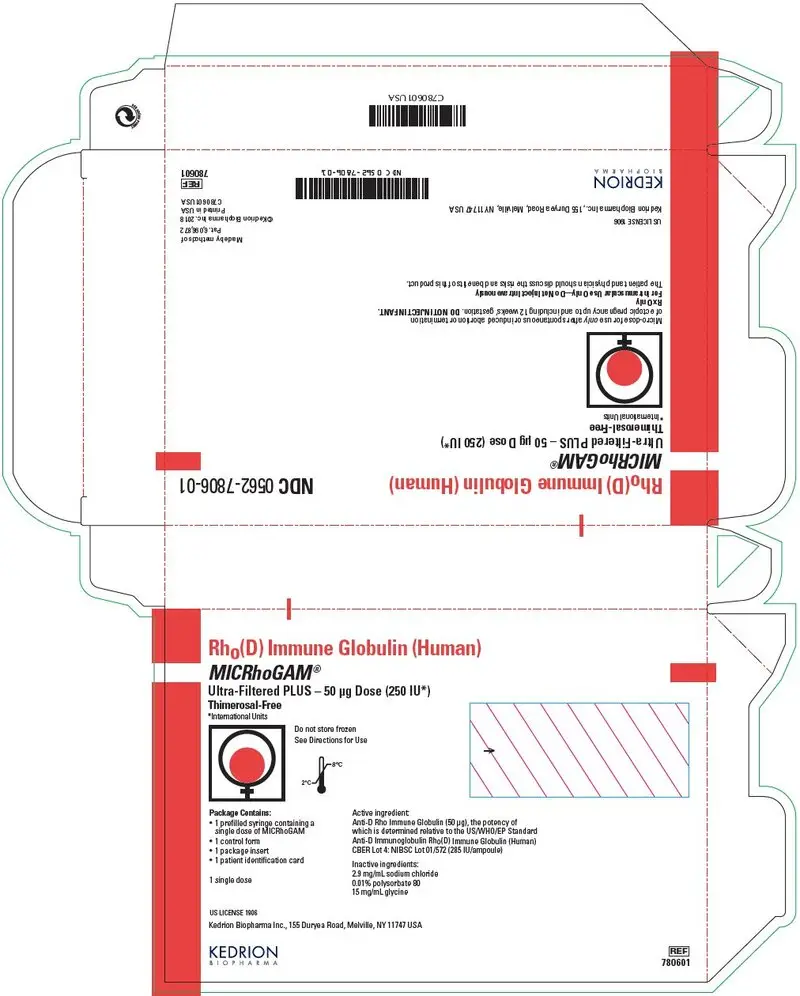
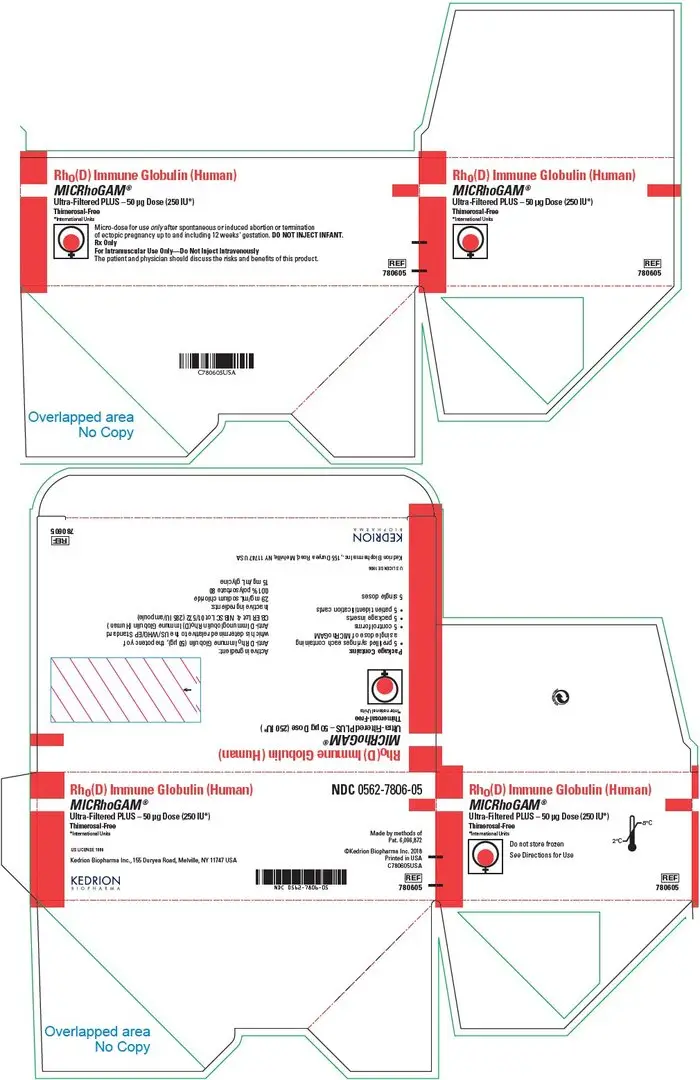
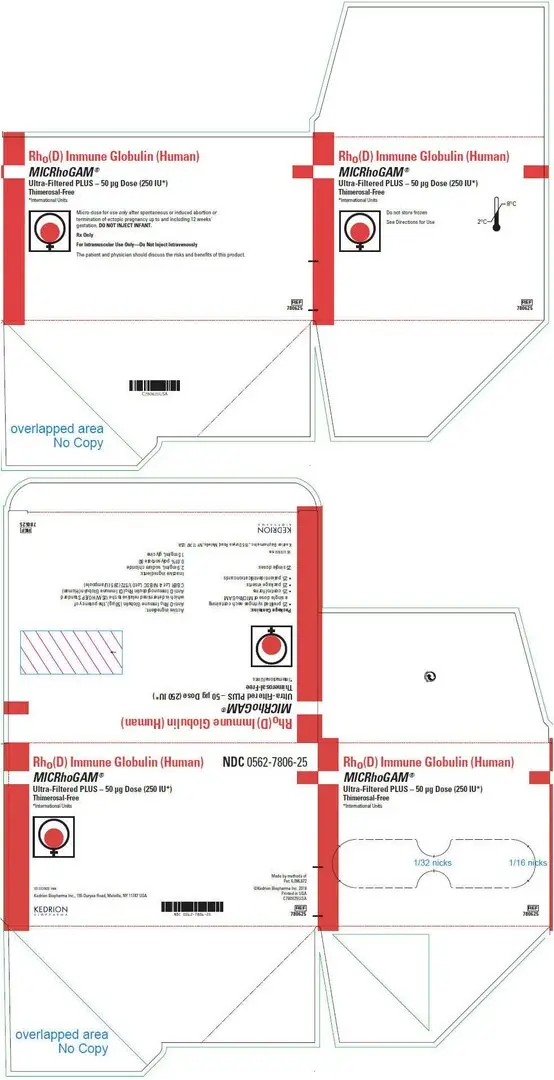
MICRhoGAM® Ultra-Filtered PLUS [Rho(D) Immune Globulin (Human)] (50 μg) (250 IU), prefilled syringe, for intramuscular use
Initial U.S. Approval: 1968
Recent Major Changes
| Description (11) | 12/2022 |
Indications and Usage for RhoGAM Ultra-Filtered PLUS
RhoGAM and MICRhoGAM are immune globulins indicated for use in preventing Rh immunization for:
- Pregnancy and other obstetrical conditions in Rh-negative women unless the father or baby are conclusively Rh-negative, e.g. delivery of an Rh-positive baby irrespective of the ABO groups of the mother and baby, any antepartum fetal-maternal hemorrhage (suspected or proven), actual or threatened pregnancy loss at any stage of gestation and ectopic pregnancy. (1.1)
- Prevention of Rh immunization in any Rh-negative person after incompatible transfusion of Rh-positive blood or blood products. (1.2)
- Limitation of use
Pregnancy and other obstetrical conditions: In the case of postpartum use, RhoGAM and MICRhoGAM are intended for maternal administration. Do not inject the newborn infant. (1.3)
RhoGAM Ultra-Filtered PLUS Dosage and Administration
For intramuscular use only. (2)
Pregnancy and other obstetrical conditions (2.1)
| Dose | Indication | Notes* |
|---|---|---|
|
||
| RhoGAM (300 µg) (1500 IU) | Postpartum (if the newborn is Rh-positive) Administer within 72 hours of delivery | Additional doses of RhoGAM are indicated when the patient has been exposed to > 15 mL of Rh-positive red blood cells. |
Antepartum:
| If antepartum prophylaxis is indicated, it is essential that the mother receive a postpartum dose if the infant is Rh-positive. | |
| MICRhoGAM (50 µg) (250 IU) | Actual or threatened termination of pregnancy (spontaneous or induced) up to and including 12 weeks gestation Administer within 72 hours | RhoGAM may be administered if MICRhoGAM is not available. |
Transfusion of Rh-incompatible blood or blood products (2.1)
Administer within 72 hours of suspected or proven exposure to Rh-positive red blood cells. (2.1)
| Dose | Indication | Notes |
|---|---|---|
| MICRhoGAM (50 µg) (250 IU) | < 2.5 mL Rh-positive red blood cells | RhoGAM may be administered if MICRhoGAM is not available. |
| RhoGAM (300 µg) (1500 IU) | ≥ 2.5 mL Rh-positive red blood cells | Administer 20 µg of RhoGAM per mL of Rh-positive red blood cell exposure, rounding up to the next whole syringe. |
Dosage Forms and Strengths
Rho(D) Immune Globulin (Human)
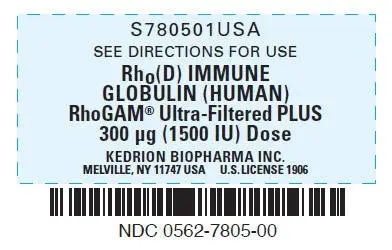
- RhoGAM® Ultra-Filtered PLUS - 300 μg (1500 IU) – Prefilled Syringes (3)
- MICRhoGAM® Ultra-Filtered PLUS - 50 μg (250 IU) – Prefilled Syringes (3)
Contraindications
- Rh-positive individuals. (4)
- Patients with a known history of anaphylactic or severe systemic reactions to the administration of human immune globulin products. (4)
Warnings and Precautions
- Severe hypersensitivity reactions may occur with the use of RhoGAM and MICRhoGAM. (5.1)
- RhoGAM and MICRhoGAM should be administered in a setting where appropriate equipment, medications such as epinephrine, and personnel trained in the management of hypersensitivity, anaphylaxis, and shock are available. (5.1)
- Products made from human blood may carry a risk of transmitting infectious agents e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent. (5.2)
- After administration of Rho(D) immune globulin, a transitory increase of various passively transferred antibodies in the patient's blood may yield positive serological testing results. (5.3)
Incompatible blood transfusion
- Patients treated for Rh-incompatible transfusion should be monitored by clinical and laboratory means for signs and symptoms of a hemolytic reaction. (5.4)
Adverse Reactions/Side Effects
- The most frequently reported adverse reactions in patients receiving Rho(D) Immune Globulin (Human) products are injection site reactions, such as swelling, induration, redness and mild pain or warmth. Possible systemic reactions are skin rash, body aches or a slight elevation in temperature. (6)
- Severe systemic reactions include allergic reactions and hemolytic reactions. (6)
To report SUSPECTED ADVERSE REACTIONS, contact Kedrion Biopharma Inc. at 1-855-3KDRION (1-855-353-7466) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch. Outside of the United States, the company distributing these products should be contacted.
Drug Interactions
- May impair the efficacy of live vaccines such as measles, mumps and varicella. Administration of live vaccines should generally be delayed until 12 weeks after the final dose of immune globulin. If administered within 14 days after administration of a live vaccine, the efficacy of the vaccination may be impaired. (7)
- The postpartum vaccination of rubella-susceptible women with rubella or MMR vaccine should not be delayed because of the receipt of Rho(D) Immune Globulin (Human). (7)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 12/2022
Full Prescribing Information
1. Indications and Usage for RhoGAM Ultra-Filtered PLUS
1.1 Pregnancy and other obstetrical conditions
RhoGAM and MICRhoGAM are indicated for administration to Rh-negative women not previously sensitized to the Rho(D) factor, unless the father or baby are conclusively Rh-negative, in case of:
- Delivery of an Rh-positive baby irrespective of the ABO groups of the mother and baby
- Antepartum prophylaxis at 26 to 28 weeks gestation
- Antepartum fetal-maternal hemorrhage (suspected or proven) as a result of placenta previa, amniocentesis, chorionic villus sampling, percutaneous umbilical blood sampling, other obstetrical manipulative procedure (e.g., version) or abdominal trauma
- Actual or threatened pregnancy loss at any stage of gestation
- Ectopic pregnancy
2. RhoGAM Ultra-Filtered PLUS Dosage and Administration
For intramuscular use only.
2.2 Administration
- Visually inspect RhoGAM and MicRhoGAM for particulate matter, discoloration and syringe damage prior to administration.
- Do not use if particulate matter is observed.
- RhoGAM and MicRhoGAM are clear or slightly opalescent. Do not use if discolored.
- Administer injection per standard protocol.
| Note: When administering RhoGAM intramuscularly, place fingers in contact with glass syringe barrel through windows in shield to prevent possible premature activation of safety guard. | 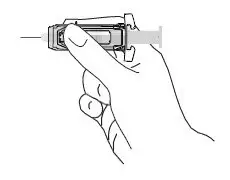 |
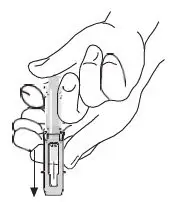 | After injection, to engage the safety guard, use free hand to slide safety guard over needle. An audible "click" indicates proper activation. Keep hands behind needle at all times. Dispose of the syringe in accordance with local regulations. |
As with all blood products, patients should be observed for at least 20 minutes following administration of RhoGAM or MICRhoGAM.
3. Dosage Forms and Strengths
- RhoGAM® Ultra-Filtered PLUS - 300 μg (1500 IU)1 – Prefilled Syringes
- MICRhoGAM® Ultra-Filtered PLUS - 50 μg (250 IU)1 – Prefilled Syringes
- 1
- The anti-D content of RhoGAM / MICRhoGAM is expressed as μg per dose or as International Units (IU) per dose. The conversion factor is 1 μg = 5 IU.2
4. Contraindications
The use of RhoGAM and MICRhoGAM is contraindicated in the following:
- Rh-positive individuals
- Patients with a known history of anaphylactic or severe systemic reactions to the administration of human immune globulin products.
5. Warnings and Precautions
5.1 Hypersensitivity
Severe hypersensitivity reactions may occur with the use of RhoGAM/MICRhoGAM, even in patients who have tolerated previous administrations.
RhoGAM / MICRhoGAM contain a small quantity of IgA3. There is a potential risk of hypersensitivity in IgA deficient individuals. Although high doses of intravenous immune globulin containing IgA at levels of 270-720 μg/mL have been given without incident during treatment of patients with high-titer antibodies to IgA4, the attending physician must weigh the benefit against the potential risks of hypersensitivity reactions.
RhoGAM / MICRhoGAM should be administered in a setting where appropriate equipment, medications such as epinephrine, and personnel trained in the management of hypersensitivity, anaphylaxis, and shock are available.
5.2 Transmissible Infectious Agents
Because RhoGAM and MICRhoGAM are made from human blood, they may carry a risk of transmitting infectious agents, e.g., viruses, the variant Creutzfeldt-Jakob disease (vCJD) and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent.
All infections thought by a physician possibly to have been transmitted by these products should be reported by the physician or other healthcare provider in the United States to Kedrion Biopharma Inc. at 1-855-3KDRION (1-855-353-7466). Outside the United States, the company distributing these products should be contacted. The physician should discuss the risks and benefits of these products with the patient.
5.3 Interference with Laboratory Tests
After administration of Rho(D) immune globulin, a transitory increase of various passively transferred antibodies in the patient's blood may yield positive serological testing results, with the potential for misleading interpretation. Passive transmission of antibodies to erythrocyte antigens (e.g., A, B, C and E) and other blood group antibodies may cause a positive direct or indirect antiglobulin (Coombs') test.
Recovery of anti-D in plasma or serum after injection of RhoGAM or other Rho(D) Immune Globulin (Human) products is highly variable among individuals. Anti-D detection in a patient's plasma is dependent on assay sensitivity and time of sample collection post-injection. Currently there are no requirements or practice standards to test for the presence of anti-D in order to determine adequacy or efficacy of dose following an injection of RhoGAM.
The presence of passively acquired anti-D antibodies in the maternal serum may cause a positive antibody screening test. This does not preclude further antepartum or postpartum prophylaxis.
A large fetomaternal hemorrhage late in pregnancy or following delivery may cause a weak mixed field positive Du test result. Assess such an individual for a large fetomaternal hemorrhage and adjust the dose of Rho(D) immune globulin accordingly. The presence of passively administered anti Rho(D) in maternal or fetal blood can lead to a positive direct antiglobulin (Coombs') test. If there is an uncertainty about the father's Rh group or immune status, administer Rho(D) immune globulin to the mother.
6. Adverse Reactions/Side Effects
The most frequently reported adverse reactions in patients receiving Rho(D) Immune Globulin (Human) products are injection site reactions, such as swelling, induration, redness and mild pain or warmth. Possible systemic reactions are skin rash, body aches or a slight elevation in temperature. Severe systemic reactions include allergic reactions and hemolytic reactions (see Warnings and Precautions [5.2]).
There have been no reported fatalities due to anaphylaxis or any other cause related to RhoGAM or MICRhoGAM administration.
6.1 Clinical Studies Experience
Because clinical studies are conducted under different protocols and widely varying conditions, adverse reaction rates observed cannot be directly compared to rates in other clinical trials and may not reflect the rates observed in practice.
No clinical studies with RhoGAM and MICRhoGAM have been conducted under the current Good Clinical Practices (GCP) Guidelines.
6.2 Postmarketing Experience
Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or to establish a causal relationship to Rho(D) Immune Globulin (Human) products.
The following adverse reactions have been reported during post-approval use of RhoGAM/MICRhoGAM: hypersensitivity reactions, including cases of anaphylactic shock or anaphylactoid reactions, skin rash, erythema, pruritus, chill, pyrexia, malaise, and back pain. Transient injection-site irritation and pain have been reported following intramuscular administration.
7. Drug Interactions
7.1 Live Virus Vaccines
Immune globulin preparations including Rho(D) Immune Globulin (Human) may impair the efficacy of live vaccines such as measles, mumps and varicella. Administration of live vaccines should generally be delayed until 12 weeks after the final dose of immune globulin. If an immune globulin is administered within 14 days after administration of a live vaccine, the immune response to the vaccination may be inhibited.5
Because of the importance of rubella immunity among women of childbearing age, the postpartum vaccination of rubella-susceptible women with rubella or MMR vaccine should not be delayed because of the receipt of Rho(D) Immune Globulin (Human) during the last trimester of pregnancy or at delivery. Vaccination should occur immediately after delivery and if possible, testing should be performed after 3 or more months to ensure immunity to rubella and if necessary, to measles.5
10. Overdosage
There are no reports of known overdoses in patients being treated with RhoGAM or MICRhoGAM.
11. RhoGAM Ultra-Filtered PLUS Description
RhoGAM and MICRhoGAM Rho(D) Immune Globulin (Human) are sterile solutions containing immunoglobulin G (IgG) anti-D (anti-Rh) for use in preventing Rh immunization. They are manufactured from human plasma containing anti-D from Rh-negative donors immunized with Rh-positive red blood cells. A single dose of RhoGAM contains sufficient anti-D (300 μg or 1500 IU) to suppress the immune response to up to 15 mL of Rh-positive red blood cells.7 A single dose of MICRhoGAM contains sufficient anti-D (50 μg or 250 IU) to suppress the immune response to up to 2.5 mL of Rh-positive red blood cells. The anti-D dose is measured by comparison to the RhoGAM in-house reference standard, the potency of which is established relative to the U.S./World Health Organization/European Pharmacopoeia Standard Anti-D Immunoglobulin Rho(D) Immune Globulin (Human).8
Plasma for RhoGAM is typically sourced from a donor center owned and operated by KEDPlasma LLC., US Lic. No. 1876. All donors are carefully screened by history and laboratory testing to reduce the risk of transmitting blood-borne pathogens from infected donors. Each plasma donation is tested and found to be non-reactive for the presence of hepatitis B surface antigen (HBsAg) and antibodies to hepatitis C (HCV) and human immunodeficiency viruses (HIV) 1 and 2. Additionally, plasma is tested by FDA licensed Nucleic Acid Testing (NAT) for hepatitis B virus (HBV), HCV and HIV-1. Each plasma unit must be negative (non-reactive) in all tests. Plasma is tested by in-process NAT procedures for hepatitis A virus (HAV) and parvovirus B19 (B19) in a minipool format. Only plasma that has passed virus screening is used for production. The NAT procedure for B19 detects all three genotypes based upon sequence alignment of known virus isolates. The limit of B19 DNA in the manufacturing pool is set not to exceed 104 IU per mL.
Fractionation of the plasma is performed by a modification of the cold alcohol procedure that has been shown to significantly lower viral titers.3 Following plasma fractionation, a viral clearance filtration step and a viral inactivation step are performed. The viral filtration step removes viruses via a size-exclusion mechanism utilizing a Viresolve 180 nanofiltration membrane (ultrafiltration mode) to remove enveloped and non-enveloped viruses.
Following viral filtration, quality control tests (CorrTest and diffusion test) are performed on the Viresolve 180 nanofiltration membrane to ensure filter integrity.9 The viral inactivation step utilizes Triton X-100 and tri-n-butyl phosphate (TNBP) to inactivate enveloped viruses such as HCV, HIV and West Nile Virus (WNV).3,10
The donor selection process, the fractionation process, the viral filtration step and the viral inactivation process increase product safety by reducing the virus load and thus the risk of transmission of enveloped and non-enveloped viruses. Rho(D) Immune Globulin (Human) intended for intramuscular use and prepared by cold alcohol fractionation has not been shown to transmit hepatitis or other infectious diseases.11 There have been no documented cases of infectious disease transmission by RhoGAM or MICRhoGAM.
Laboratory spiking studies3,12 have shown that the cumulative viral removal and inactivation capability of the RhoGAM / MICRhoGAM manufacturing process is as follows:
| Virus | HIV-1 | BVDV | PRV | PPV | EMC |
|---|---|---|---|---|---|
| Note : Data of viral removal/inactivation capability was generated from Kedrion Biopharma Inc. RhoGAM / MICRhoGAM can be manufactured at both Kedrion Biopharma Inc. and Ortho Clinical Diagnostics Inc. up to drug substance: regardless of which product is administered (manufactured at Kedrion Biopharma Inc. or Ortho Clinical Diagnostics Inc.) data of viral removal/inactivation are applicable to both processes (Ortho and Kedrion Biopharma Inc.). | |||||
| Units = log10 reduction | |||||
| HIV Human Immunodeficiency Virus, Relevant virus for HIV-1 and 2 and model virus for Human T-cell Lymphotropic Virus (HTLV) 1 and 2 BVDV Bovine Viral Diarrhea Virus, Model for Hepatitis C Virus and West Nile Virus (WNV) PRV Pseudorabies Virus, Model for large enveloped DNA viruses such as Herpes Viruses PPV Porcine Parvovirus, Model for Parvovirus B19 EMC Encephalomyocarditis Virus, Model for Hepatitis A Virus N/A Not Applicable |
|||||
|
|||||
| Lipid Enveloped | Yes | Yes | Yes | No | No |
| Size (nm) | 80-120 | 40-70 | 120-200 | 18-24 | 25-30 |
| Genome | ss-RNA | ss-RNA | ds-DNA | ss-DNA | ss-RNA |
| Step | |||||
| Methanol precipitation | 5.16 | 4.46 | 4.95 | 4.02 | 4.57 |
| CUNO Depth filtration | ≥ 4.95 | 2.53 | 2.34 | 3.83 | Not Significant (<1 Log) |
| Viral Grade Filtration (Nanofiltration) | ≥ 3.35 (≥ 4.76)* | ≥ 3.67 (≥ 5.02)* | ≥ 3.09 (≥ 4.19)* | 4.88 | 4.63 |
| Solvent/Detergent treatment | ≥ 5.08 | ≥ 4.47 | ≥ 4.05 | N/A | N/A |
| Total Viral Reduction | ≥ 18.54 | ≥ 15.13 | ≥ 14.43 | 12.73 | 9.20 |
The safety of Rho(D) Immune Globulin (Human) has been further shown in an empirical study of viral marker rates in female blood donors in the United States.13 This study revealed that Rh-negative donors, of whom an estimated 55-60% had received Rho(D) Immune Globulin (Human) for pregnancy-related indications, had prevalence and incidence viral marker rates similar to those of Rh-positive female donors who had not received Rho(D) Immune Globulin (Human).
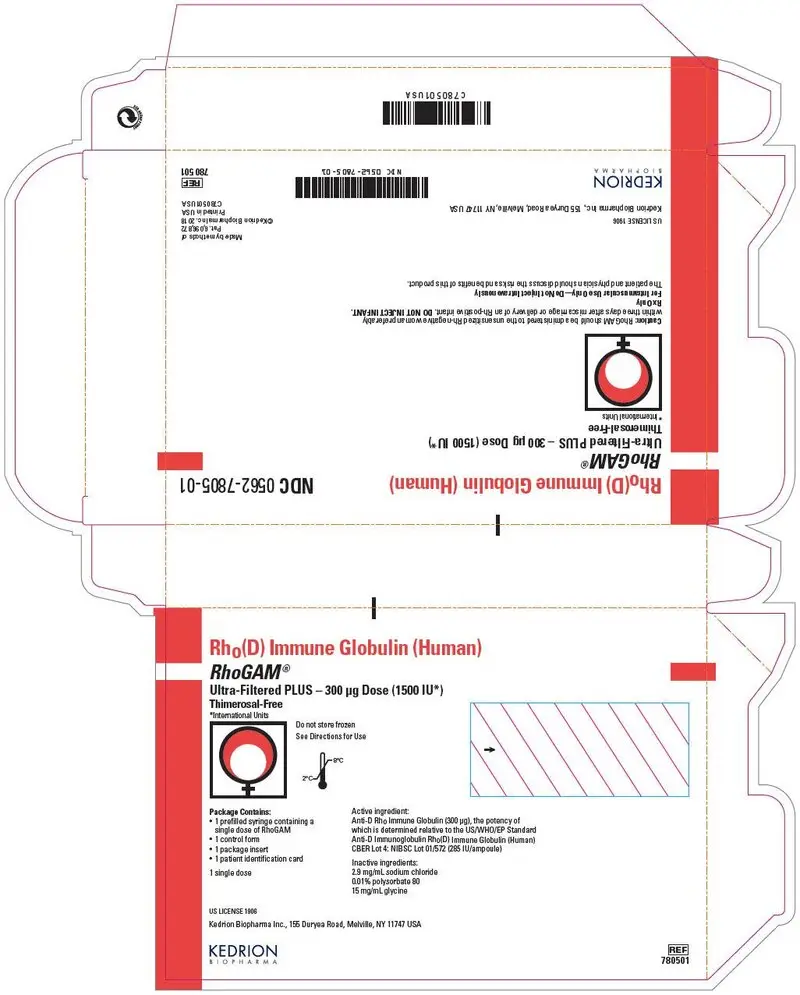
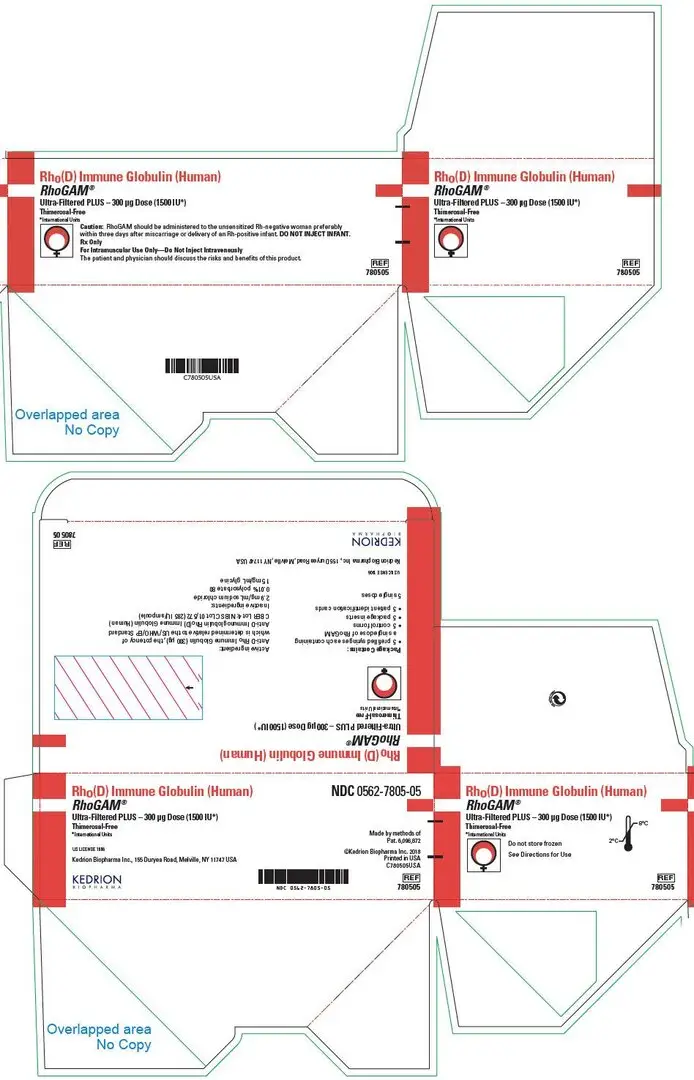
The final product contains 5 ± 1% IgG, 2.9 mg/mL sodium chloride, 0.01% Polysorbate 80 (non-animal derived) and 15 mg/mL glycine. Small amounts of IgA, typically less than 15 μg per dose, are present.3 The pH range is 6.20 - 7.00 and IgG purity is > 98%. The product contains no added human serum albumin (HSA), no thimerosal or other preservatives and utilizes a latex-free delivery system.
RhoGAM Ultra-Filtered PLUS and MICRhoGAM Ultra-Filtered PLUS are manufactured for Kedrion Biopharma Inc. either by Ortho-Clinical Diagnostics, Inc. or by Kedrion Biopharma Inc. up to the bulk products, and all are filled and packaged by Kedrion Biopharma Inc., 155 Duryea Road, Melville, NY 11747 USA.
12. RhoGAM Ultra-Filtered PLUS - Clinical Pharmacology
12.1 Mechanism of Action
RhoGAM and MICRhoGAM act by suppressing the immune response of Rh-negative individuals to Rh-positive red blood cells. The mechanism of action is unknown. RhoGAM, MICRhoGAM and other Rho(D) Immune Globulin (Human) products are not effective in altering the course or consequences of Rh immunization once it has occurred.
12.3 Pharmacokinetics
Pharmacokinetic studies after intramuscular injection were performed on sixteen Rh-negative subjects receiving a single dose of (368 μg or 1840 IU) RhoGAM.3 Plasma anti-D levels were monitored for thirteen weeks using a validated Automated Quantitative Hemagglutination method with sensitivity of approximately 1 ng/mL. The following mean pharmacokinetic parameters were obtained from data collected over the first ten weeks of a thirteen-week study:
| Parameter | Mean | SD | Units |
|---|---|---|---|
| Maximum plasma concentration obtained (Cmax) | 54.0 | 13.0 | ng/mL |
| Time to attain Cmax (Tmax) | 4 | days | |
| Elimination half-life (T1/2) | 30.9 | 13.8 | days |
| Volume of distribution (Vd) | 7.3 | 1.5 | liters |
| Clearance (CL) | 150.4 | 53.3 | mL/day |
14. Clinical Studies
Rho(D) Immune Globulin (Human) administered at 28 weeks, as well as within 72 hours of delivery, has been shown to reduce the Rh immunization rate to about 0.1-0.2%.15,16 Clinical studies demonstrated that administration of MICRhoGAM within three hours following pregnancy termination was 100% effective in preventing Rh immunization.17
Multiple studies have been performed that prove the safety and efficacy of RhoGAM in both the obstetrical and post transfusion settings.
Freda, Gorman and colleagues18 studied the efficacy of RhoGAM in the postpartum setting in a randomized, controlled study completed in 1967. The control group received no immunoglobulin therapy after delivery, while the test group received 300 μg of RhoGAM intramuscularly within 72 hours of delivery of an Rh-positive infant. Six months after delivery, the incidence of Rh immunization in the control group was 6.4% (32/499) versus 0.13% (1/781) in the RhoGAM group (p < 0.001).
Pollack et al. performed two randomized, placebo-controlled studies in the post transfusion setting that were designed to establish the dose response relationship of RhoGAM. In the first study,7 178 (176 males, 2 females) Rh-negative volunteers received varying volumes of Rh- positive red cells; 92 subjects then received RhoGAM. A single dose of RhoGAM (1.1 mL @ 267 μg/mL) was shown to suppress anti-D formation after injection of up to 15.1 mL of Rh-positive red cells. In a companion study, Pollack administered 500 mL of Rh-positive whole blood to 44 Rh-negative male volunteers. Twenty-two (22) subjects received 20 μg RhoGAM per mL of Rh-positive red cells and 22 received no RhoGAM. None of the RhoGAM-treated subjects developed anti-D; 18/22 control arm subjects developed anti-D (p < 0.0001).
Human clinical studies3 were subsequently performed to prove the efficacy of MICRhoGAM and the low protein (5%) formulations. In the MICRhoGAM study, 81 Rh-negative male volunteers received an initial injection of 2.5 mL Rh-positive red cells, followed by a booster injection (0.1 mL) of red cells at 26 weeks; 40 subjects received an injection of MICRhoGAM after the initial red cell injection. None of the subjects who received MICRhoGAM developed anti-D, both before and after the booster red cell injection. A similar study was performed in 1985 using the low protein formulation of RhoGAM. None of the 30 Rh-negative male volunteers who received RhoGAM after injection of 15 mL of Rh-positive red cells developed anti-D.
15. References
- 1
- AABB Technical Manual. 19th ed. Bethesda, Maryland: AABB, October 2017.
- 2
- Gunson HH, Bowell PJ, Kirkwood TBL. Collaborative study to recalibrate the International Reference Preparation of anti-D immunoglobulin. J Clin Pathol 1980;33:249-53.
- 3
- Data on file at Kedrion Biopharma Inc.
- 4
- Cunningham-Rundles C, Zhuo Z, Mankarious S, Courter S. Long-term use of IgA- depleted intravenous immunoglobulin in immunodeficient subjects with anti-IgA antibodies. J Clin Immunol 1993;13:272-78.
- 5
- Centers for Disease Control and Prevention. General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices and the American Academy of Family Physicians. MMWR 2002;51 (No. RR-2):6-7.
- 6
- Thornton JG, Page C, Foote G, Arthur GR, Tovey LAD, Scott JS. Efficacy and long term effects of antenatal propylaxis with anti-D immunoglobulin. Br Med J. 1989;298: 1671-1673
- 7
- Pollack W, Ascari WQ, Kochesky RJ, O'Connor RR, Ho TY, Tripodi D. Studies on Rh prophylaxis. I. Relationship between doses of anti-Rh and size of antigenic stimulus. Transfusion 1971;11:333-39.
- 8
- Thorpe SJ, Sands D, Fox B, Behr-Gross ME, Schaffner G, Yu MW. A global standard for anti-D immunoglobulin: international collaborative study to evaluate a candidate preparation. Vox Sang 2003;85:313-21.
- 9
- Phillips MW, DiLeo AJ. A Validatible Porosimetric Technique for verifying the integrity of virus-retentive membranes. Biologicals 1996;24:243-53.
- 10
- Horowitz B, Wiebe ME, Lippin A, Stryker MH. Inactivation of viruses in labile blood derivatives. I. Disruption of lipid-enveloped viruses by tri (n-butyl) phosphate detergent combinations. Transfusion 1985; 25(6):516-22.
- 11
- Tabor E. The epidemiology of virus transmission by plasma derivatives: clinical studies verifying the lack of transmission of hepatitis B and C viruses and HIV type 1. Transfusion 1999;39:1160-68.
- 12
- Van Holten RW, Ciavarella D, Oulundsen G, Harmon F, Riester S. Incorporation of an additional viral-clearance step into a human immunoglobulin manufacturing process. Vox Sang 2002;83:227-33.
- 13
- Watanabe KK, Busch MP, Schreiber GB, Zuck TF. Evaluation of the safety of Rh Immunoglobulin by monitoring viral markers among Rh-negative female blood donors. Vox Sang 2000;8:1-6.
- 14
- Zipursky A, Israels LG. The pathogenesis and prevention of Rh immunization. Can Med Assoc J 1967;97:1245-56.
- 15
- de Haas M, Finning K, Massey E, Roberts DJ. Anti-D prophylaxis: past, present and future. Transfus Med 2014;24:1–7. (ex 22-24)
- 16
- Bowman J. Thirty-five years of Rh prophylaxis. Transfusion 2003;43:1661–6. (ex 22-24)
- 17
- Stewart FH, Burnhill MS, Bozorgi N. Reduced dose of Rh immunoglobulin following first trimester pregnancy termination. Obstet Gynecol 1978;51:318-22.
- 18
- McBain RD, Crowther CA, Middleton P. Anti-D administration in pregnancy for preventing Rhesus alloimmunisation. Cochrane Database Syst Rev. 2015 Sep
16. How is RhoGAM Ultra-Filtered PLUS supplied
The following presentations of RhoGAM are available:
| Presentation | Product description/ package sizes | Carton NDC number | Primary container NDC number |
|---|---|---|---|
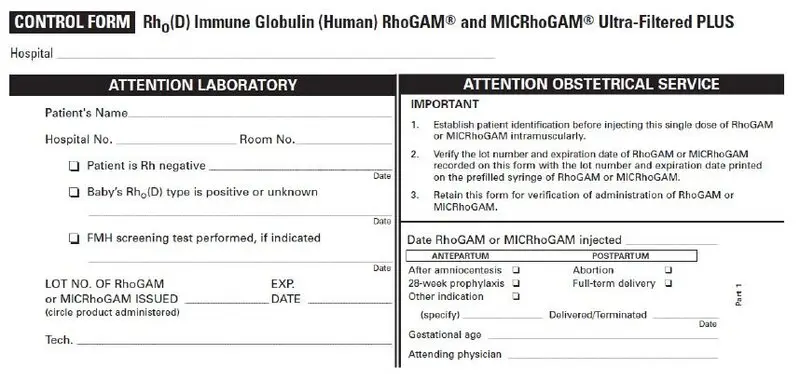
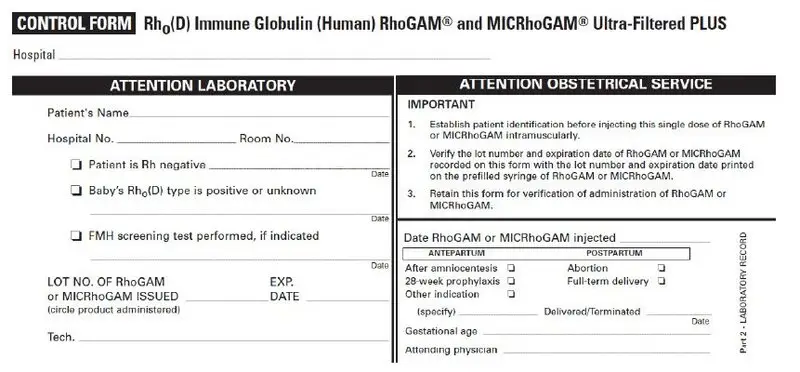
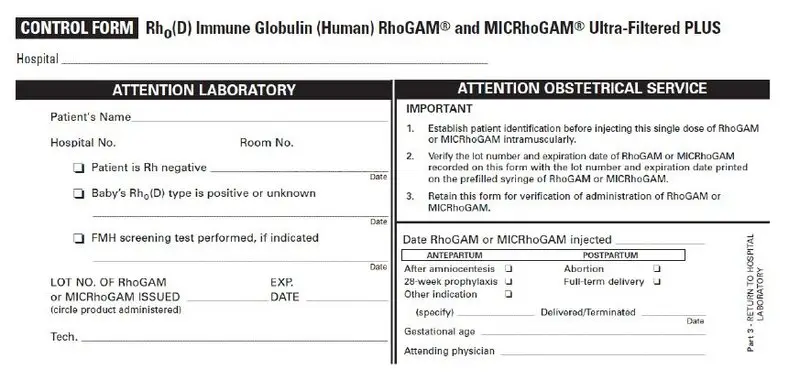
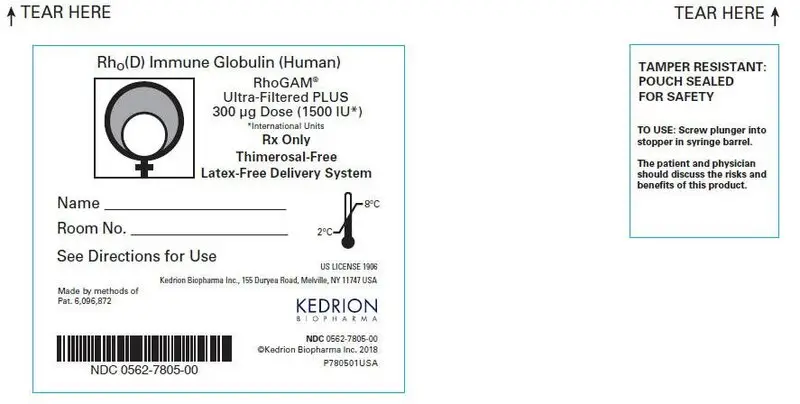
| RhoGAM® Ultra-Filtered PLUS (300 µg) (1500 IU) – Carton of 1 syringe | 1 prefilled single-dose syringe in a pouch, 1 package insert, 1 control form, 1 patient identification card | NDC 0562-7805-01 | prefilled single-dose syringe NDC 0562-7805-00 |
| RhoGAM® Ultra-Filtered PLUS (300 µg) (1500 IU) – Carton of 5 syringes | 5 prefilled single-dose syringe in a pouch, 5 package insert, 5 control form, 5 patient identification card | NDC 0562-7805-05 | |
| RhoGAM® Ultra-Filtered PLUS (300 µg) (1500 IU) – Carton of 25 syringes | 25 prefilled single-dose syringe in a pouch, 25 package insert, 25 control form, 25 patient identification card | NDC 0562-7805-25 |
The following presentations of MICRhoGAM are available:
| Presentation | Product description/ package sizes | Carton NDC number | Primary container NDC number |
|---|---|---|---|
| MICRhoGAM Ultra-Filtered PLUS (50 µg) (250 IU) – Carton of 1 syringe | 1 prefilled single-dose syringe in a pouch, 1 package insert, 1 control form, 1 patient identification card | NDC 0562-7806-01 | prefilled single-dose syringe NDC 0562-7806-00 |
| MICRhoGAM Ultra-Filtered PLUS (50 µg) (250 IU) – Carton of 5 syringes | 5 prefilled single-dose syringe in a pouch, 5 package insert, 5 control form, 5 patient identification card | NDC 0562-7806-05 | |
| MICRhoGAM Ultra-Filtered PLUS (50 µg) (250 IU) – Carton of 25 syringes | 25 prefilled single-dose syringe in a pouch, 25 package insert, 25 control form, 25 patient identification card | NDC 0562-7806-25 |
17. Patient Counseling Information
Please inform patients of the following:
- The risks and benefits of RhoGAM and MicRhoGAM.
- The most common adverse reactions are local reactions including swelling, induration, redness and mild pain at the site of injection, and a small number of patients have noted a slight elevation in temperature.
- Allergic reactions to RhoGAM and MICRhoGAM may occur. Patients should be observed for at least 20 minutes after administration. Signs of hypersensitivity reactions include hives, generalized urticaria, tightness of the chest, wheezing, hypotension and anaphylaxis.
- RhoGAM and MICRhoGAM may interfere with the response to live virus vaccines (e.g., measles, mumps, rubella, and varicella). Instruct patients to notify their healthcare professional of this potential interaction when they are receiving vaccinations.
- RhoGAM and MICRhoGAM are prepared from human plasma and may contain infectious agents that can cause disease. Numerous tests have been applied in the plasma collection process and specific viral inactivation steps have been added to the manufacturing process to minimize the risk of transmission of diseases, but all risk cannot be eliminated.
- Retain the RhoGAM Patient Identification Card and advise the patient to retain the card and present it to other health care providers when appropriate.
| SUMMARY OF REVISIONS
Revised to reflect the current manufacturing arrangement, up to the bulk products by either Ortho-Clinical Diagnostics, Inc. or by Kedrion Biopharma Inc., and then the final drug products by Kedrion Biopharma Inc., in section 11 DESCRIPTION and other relevant places. |
| RHOGAM ULTRA-FILTERED PLUS
human rho(d) immune globulin injection, solution |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| MICRHOGAM ULTRA-FILTERED PLUS
human rho(d) immune globulin injection, solution |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| Labeler - Kedrion Biopharma Inc (080452111) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Ortho Clinical Diagnostics | 068715424 | MANUFACTURE(0562-7805, 0562-7806) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Kedrion Biopharma Inc. | 080452111 | MANUFACTURE(0562-7805, 0562-7806) | |