Drug Detail:Rhophylac (Rho (d) immune globulin [ roe-d-im-myoon-glob-yoo-lin ])
Drug Class: Immune globulins
Highlights of Prescribing Information
RHOPHYLAC
Rh0(D) Immune Globulin Intravenous (Human) 1500 IU (300 mcg)
Solution for Intravenous (IV) or Intramuscular (IM) Injection
Initial U.S. Approval: 2004
WARNING: INTRAVASCULAR HEMOLYSIS IN ITP
See full prescribing information for complete boxed warning. This warning does not apply to Rh(D)-negative patients treated for the suppression of Rh isoimmunization.
- Intravascular hemolysis leading to death has been reported in Rh (D)-positive patients treated for immune thrombocytopenic purpura (ITP) with Rh(D) Immune Globulin Intravenous (Human) products.
- Intravascular hemolysis can lead to clinically compromising anemia and multi-system organ failure including acute respiratory distress syndrome (ARDS), acute renal insufficiency, renal failure, and disseminated intravascular coagulation (DIC).
- Monitor patients for signs and symptoms of intravascular hemolysis in a healthcare setting for at least 8 hours after administration.
Recent Major Changes
| Dosage and Administration (2.2) | 12/2020 |
Indications and Usage for Rhophylac
RHOPHYLAC is a Rh(D) Immune Globulin Intravenous (Human) indicated for:
Suppression of Rhesus (Rh) Isoimmunization (1.1) in:
- Pregnancy and obstetric conditions in non-sensitized, Rh(D)-negative women with an Rh-incompatible pregnancy, including:
- Routine antepartum and postpartum Rh prophylaxis
- Rh prophylaxis in obstetric complications or invasive procedures
- Incompatible transfusions in Rh(D)-negative individuals transfused with blood components containing Rh(D)-positive red blood cells (RBCs)
Immune Thrombocytopenic Purpura (ITP) (1.2)
- Raising platelet counts in Rh(D)-positive, non-splenectomized adults with chronic ITP.
Rhophylac Dosage and Administration
DO NOT confuse micrograms (mcg) with International Units (IU) when calculating the dose. Miscalculations could result in overdose or underdose
Suppression of Rh Isoimmunization (2.2) (IV or IM administration only)
| Indication | Timing | Dose* (1 mcg = 5 IU) | |
|---|---|---|---|
| Rh-incompatible Pregnancy: | mcg | IU | |
|
|||
| Routine antepartum prophylaxis | Week 28-30 of pregnancy | 300 mcg | 1500 IU |
| Postpartum prophylaxis (required only if the newborn is Rh(D)-positive, or of unknown status) | Within 72 hours of birth | 300 mcg† | 1500 IU |
| Obstetric complications/invasive procedures | Within 72 hours of complication / procedure | 300 mcg† | 1500 IU |
| Excessive fetomaternal hemorrhage (>15 mL fetal RBCs) | Within 72 hours of complication | 300 mcg plus:
20 mcg per mL RhD-positive fetal RBCs in excess of 15 mL if excess transplacental bleeding is quantified, or An additional 300 mcg if excess transplacental bleeding cannot be quantified | 1500 IU plus:
100 IU per mL RhD- positive fetal RBCs in excess of 15 mL if excess transplacental bleeding is quantified, or An additional 1500 IU if excess transplacental bleeding cannot be quantified |
| Incompatible transfusions | Within 72 hours of exposure | 20 mcg per 2 mL transfused Rh(D)-positive whole blood or per 1 mL Rh(D)- positive RBCs | 100 IU per 2 mL transfused Rh(D)- positive whole blood or per 1 mL Rh(D)- positive RBCs |
Treatment of ITP (2.2) (IV administration only)
| Dose (mcg) | Rate of administration |
|---|---|
| 50 mcg per kg body weight | 2 mL per 15 to 60 seconds |
Dosage Forms and Strengths
1500 IU (300 mcg) per 2 mL single-dose, prefilled, ready-to-use glass syringe (3)
Contraindications
- History of anaphylactic or severe systemic reaction to human immune globulin products (4)
- IgA deficient patients with antibodies against IgA and a history of hypersensitivity to RHOPHYLAC or any of its components (4)
- Do not administer to the newborn infant of the mother that received RHOPHYLAC postpartum (4).
Warnings and Precautions
- Hypersensitivity: Severe hypersensitivity and anaphylactic reactions may occur (5.1).
- Transmissible Infectious Agents: Potential of viruses and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent (5.3).
- Intravascular Hemolysis in ITP Treatment: Monitor patients for signs and symptoms and perform confirmatory laboratory tests (5.4).
- Pre-existing Anemia in ITP Treatment: RHOPHYLAC may increase the severity of anemia (5.5).
Adverse Reactions/Side Effects
Suppression of Rh Isoimmunization: Most common adverse reactions in ≥0.5% of subjects are nausea, dizziness, headache, injection-site pain, and malaise (6.1).
ITP: Most common adverse reactions reported in >14% of subjects are chills, pyrexia/increased body temperature, headache, and hemolysis (increased bilirubin, decreased hemoglobin, or decreased haptoglobin) (6.1).
To report SUSPECTED ADVERSE REACTIONS, contact CSL Behring Pharmacovigilance at 1-866-915-6958 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
Immunoglobulin administration may transiently interfere with the immune response to live virus vaccines, such as measles, mumps and rubella (7.1).
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 12/2020
Full Prescribing Information
WARNING: INTRAVASCULAR HEMOLYSIS IN ITP
This warning does not apply to Rh(D)-negative patients treated for the suppression of Rh isoimmunization.
- Intravascular hemolysis leading to death has been reported in Rh(D)-positive patients treated for immune thrombocytopenic purpura (ITP) with Rh(D) Immune Globulin Intravenous (Human) products.
- Intravascular hemolysis can lead to clinically compromising anemia and multi-system organ failure including acute respiratory distress syndrome (ARDS), acute renal insufficiency, renal failure, and disseminated intravascular coagulation (DIC).
- Monitor patients treated for signs and symptoms of hemolysis in a healthcare setting for at least 8 hours after administration. Perform a dipstick urinalysis at baseline, 2 hours and 4 hours after administration, and prior to the end of the monitoring period. Alert patients to, and monitor them for back pain, shaking chills, fever, and discolored urine or hematuria. Absence of these signs and/or symptoms within 8 hours does not indicate IVH cannot occur subsequently. If signs and/or symptoms of intravascular hemolysis are present or suspected after RHOPHYLAC administration, perform post-treatment laboratory tests, including plasma hemoglobin, haptoglobin, LDH, and plasma bilirubin (direct and indirect).
1. Indications and Usage for Rhophylac
RHOPHYLAC is a Rh(D) Immune Globulin Intravenous (Human) (anti-D) product that is indicated for the suppression of Rh isoimmunization in non-sensitized Rh(D)-negative patients and for the treatment of immune thrombocytopenic purpura (ITP) in Rh(D)-positive patients.
2. Rhophylac Dosage and Administration
Observe patients for at least 20 minutes following administration of RHOPHYLAC.
2.1 Preparation and Handling
- RHOPHYLAC is a clear or slightly opalescent, colorless to pale yellow solution. Inspect RHOPHYLAC visually for particulate matter and discoloration prior to administration. Do not use if the solution is cloudy or contains particulates.
- Prior to intravenous use, ensure that the needle-free intravenous administration system is compatible with the tip of the RHOPHYLAC glass syringe.
- Do not freeze.
- Bring RHOPHYLAC to room temperature before use.
- RHOPHYLAC is for single dose only. Dispose of any unused product or waste material in accordance with local requirements.
3. Dosage Forms and Strengths
1500 IU (300 mcg) per 2 mL single-dose, prefilled, ready-to-use, glass syringe for IV or IM use
4. Contraindications
RHOPHYLAC is contraindicated in:
- patients who have had an anaphylactic or severe systemic reaction to the administration of human immune globulin,
- IgA-deficient patients with antibodies to IgA and a history of hypersensitivity to RHOPHYLAC or any of its components,
- the newborn infant of a mother that received RHOPHYLAC postpartum.
5. Warnings and Precautions
5.1 Hypersensitivity
Severe hypersensitivity reactions may occur even in patients who have tolerated previous administrations. If symptoms of allergic or early signs of hypersensitivity reactions (including generalized urticaria, tightness of the chest, wheezing, hypotension, and anaphylaxis) occur, discontinue RHOPHYLAC administration immediately and institute appropriate treatment. Medications such as epinephrine should be available for immediate treatment of acute hypersensitivity reactions.
RHOPHYLAC contains trace amounts of IgA (less than 5 mcg/mL) [see Description (11)]. Patients with known antibodies to IgA have a risk of developing potentially severe hypersensitivity and anaphylactic reactions. RHOPHYLAC is contraindicated in patients with antibodies against IgA and a history of hypersensitivity reactions to RHOPHYLAC or any of its components [see Contraindications (4)].
5.2 Interference with Laboratory Tests
The administration of Rh (D) immune globulin may affect the results of blood typing, the antibody screening test, and the direct antiglobulin (Coombs') test. Antepartum administration of Rh(D) immune globulin to the mother can also affect these tests in the newborn infant.
RHOPHYLAC can contain antibodies to other Rh antigens (e.g., anti-C antibodies), which might be detected by sensitive serological tests following administration.
5.3 Transmissible Infectious Agents
Because RHOPHYLAC is made from human blood, it may carry a risk of transmitting infectious agents, e.g., viruses and, theoretically, the Creutzfeldt-Jakob disease (CJD) agent. The risk of infectious agent transmission has been reduced by screening plasma donors for prior exposure to certain viruses, testing for the presence of certain current virus infections, and including virus inactivation/removal steps in the manufacturing process for RHOPHYLAC.
Report any infections thought to be possibly transmitted by RHOPHYLAC to CSL Behring Pharmacovigilance at 1-866-915-6958.
5.4 Intravascular Hemolysis in ITP Treatment
Serious intravascular hemolysis has occurred in a clinical study with RHOPHYLAC. All cases resolved completely. However, as reported in the literature, some Rh(D)-positive patients treated with Rh(D) Immune Globulin Intravenous (Human) for ITP developed clinically compromising anemia, acute renal insufficiency, and, very rarely, disseminated intravascular coagulation (DIC) and death.2 Note: This warning does not apply to Rh(D)-negative patients treated for the suppression of Rh isoimmunization.
Monitor patients in a healthcare setting for at least 8 hours after administration of RHOPHYLAC. Perform a dipstick urinalysis at baseline, 2 hours and 4 hours after administration, and prior to the end of the monitoring period.
Alert patients to, and monitor them for, the signs and symptoms of intravascular hemolysis, including back pain, shaking chills, fever, and discolored urine or hematuria. Absence of these signs and/or symptoms of intravascular hemolysis within 8 hours do not indicate intravascular hemolysis cannot occur subsequently.
If signs and/or symptoms of intravascular hemolysis are present or suspected after RHOPHYLAC administration, perform post-treatment laboratory tests, including plasma hemoglobin, haptoglobin, LDH, and plasma bilirubin (direct and indirect). DIC may be difficult to detect in the ITP population; the diagnosis is dependent mainly on laboratory testing.
If patients who develop hemolysis with clinically compromising anemia after receiving RHOPHYLAC are to be transfused, Rh(D)-negative packed RBCs should be used to avoid exacerbating ongoing hemolysis.
6. Adverse Reactions/Side Effects
The most serious adverse reactions in patients receiving Rh(D) Immune Globulin Intravenous (Human) have been observed in the treatment of ITP and include intravascular hemolysis, clinically compromising anemia, acute renal insufficiency, and, very rarely, DIC and death [see Boxed Warning, and Warnings and Precautions (5.4)].2
The most common adverse reactions observed with the use of RHOPHYLAC for suppression of Rh isoimmunization (≥0.5% of subjects) are nausea, dizziness, headache, injection-site pain, and malaise.
The most common adverse reactions observed in the treatment of ITP (>14% of subjects) are chills, pyrexia/increased body temperature, and headache. Hemolysis (manifested by an increase in bilirubin, a decrease in hemoglobin, or a decrease in haptoglobin) was also observed.
6.1 Clinical Trials Experience
Because clinical studies are conducted under different protocols and widely varying conditions, adverse reaction rates observed cannot be directly compared to rates in other clinical trials and may not reflect the rates observed in practice.
6.2 Postmarketing Experience
Because postmarketing adverse reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to product exposure. The following adverse reactions have been identified during post-approval use of RHOPHYLAC:
7. Drug Interactions
7.1 Live Virus Vaccines
Passive transfer of antibodies may transiently impair the immune response to live attenuated virus vaccines such as measles, mumps, rubella, and varicella [see Patient Counseling Information (17)]. Do not immunize with live vaccines within 3 months after the final dose of RHOPHYLAC. If RHOPHYLAC is administered within 14 days after administration of a live vaccine, the immune response to the vaccination may be inhibited.3
10. Overdosage
During clinical trials, there were no reports of known overdoses in patients being treated for suppression of Rh isoimmunization or ITP. In postmarketing reporting, there have been a limited number of overdose reports including medication error reports related to dosage calculations in which higher doses than that recommended for RHOPHYLAC were administered potentially due to confusion between mcg and international units (IU). In these reports there were no adverse reactions identified due to overdose. Patients with incompatible transfusion or ITP who receive an overdose of Rh(D) immune globulin should be monitored because of the potential risk for hemolysis.
11. Rhophylac Description
RHOPHYLAC is a sterile Rh(D) Immune Globulin Intravenous (Human) (anti-D) solution in a ready-to-use prefilled glass syringe for intravenous or intramuscular injection. One syringe contains at least 1500 IU (300 mcg) of IgG antibodies to Rh(D) in a 2 mL solution, sufficient to suppress the immune response to at least 15 mL of Rh(D)-positive RBCs.1 The product potency is expressed in IUs by comparison to the World Health Organization (WHO) standard, which is also the US and the European Pharmacopoeia standard.
Plasma is obtained from healthy Rh(D)-negative donors who have been immunized with Rh(D)-positive RBCs. The donors are screened carefully to reduce the risk of receiving donations containing blood-borne pathogens. Each plasma donation used in the manufacture of RHOPHYLAC is tested for the presence of HBV surface antigen (HBsAg), HIV-1/2, and HCV antibodies. In addition, plasma used in the manufacture of RHOPHYLAC is tested by FDA-licensed Nucleic Acid Testing (NAT) for HBV, HCV, and HIV-1 and found to be negative. The source plasma is also tested by NAT for hepatitis A virus (HAV) and B19 virus (B19V).
RHOPHYLAC is produced by an ion-exchange chromatography isolation procedure5, using pooled plasma obtained by plasmapheresis of immunized Rh(D)-negative US donors. The manufacturing process includes a solvent/detergent treatment step (using tri-n-butyl phosphate and Triton™ X-100) that is effective in inactivating enveloped viruses such as HIV, HCV, and HBV.6,7 RHOPHYLAC is filtered using a Planova® 15 nanometer (nm) virus filter that has been validated to be effective in removing both enveloped and non-enveloped viruses. Table 5 presents viral clearance and inactivation data from validation studies, expressed as the mean log10 reduction factor (LRF).
| HIV | PRV | BVDV | MVM | |
|---|---|---|---|---|
| HIV, a model for HIV-1 and HIV-2; PRV, pseudorabies virus, a model for large, enveloped DNA viruses (e.g., herpes virus); BVDV, bovine viral diarrhea virus, a model for HCV and West Nile virus; MVM, minute virus of mice, a model for B19V and other small, non-enveloped DNA viruses. | ||||
| Virus property | ||||
| Genome | RNA | DNA | RNA | DNA |
| Envelope | Yes | Yes | Yes | No |
| Size (nm) | 80-100 | 120-200 | 40-70 | 18-24 |
| Manufacturing step | Mean LRF | |||
| Solvent/detergent treatment | ≥6.0 | ≥5.6 | ≥5.4 | Not tested |
| Chromatographic process steps | 4.5 | ≥3.9 | 1.6 | ≥2.6 |
| Virus filtration | ≥6.3 | ≥5.6 | ≥5.5 | 3.4 |
| Overall reduction (log10 units) | ≥16.8 | ≥15.1 | ≥12.5 | ≥6.0 |
RHOPHYLAC contains a maximum of 30 mg/mL of human plasma proteins, 10 mg/mL of which is human albumin added as a stabilizer. Prior to the addition of the stabilizer, RHOPHYLAC has a purity greater than 95% IgG. RHOPHYLAC contains less than 5 mcg/mL of IgA, which is the limit of detection. Additional excipients are approximately 20 mg/mL of glycine and up to 0.25 M of sodium chloride. RHOPHYLAC contains no preservative. Human albumin is manufactured from pooled plasma of US donors by cold ethanol fractionation, followed by pasteurization.
14. Clinical Studies
14.1 Suppression of Rh Isoimmunization
In two clinical studies, 447 Rh(D)-negative pregnant women received a 1500 IU (300 mcg) dose of RHOPHYLAC during Week 28 of gestation. The women who gave birth to an Rh(D)-positive baby received a second 1500 IU (300 mcg) dose within 72 hours of birth.
- Study 1 (Pharmacokinetic Study) – Eight of the women who participated in the pharmacokinetic study [see Clinical Pharmacology (12.3)] gave birth to an Rh(D)-positive baby and received the postpartum dose of 1500 IU (300 mcg) of RHOPHYLAC.9 Antibody tests performed 6 to 8 months later were negative for all women. This suggests that no Rh(D) immunization occurred.
- Study 2 (Pivotal Study) – In an open-label, single-arm clinical study at 22 centers in the US and United Kingdom, 432 pregnant women received the antepartum dose of 1500 IU (300 mcg) of RHOPHYLAC either as an intravenous or intramuscular injection (two randomized groups of 216 women each).11 Subjects received an additional 1500 IU (300 mcg) dose if an obstetric complication occurred between the routine antepartum dose and birth or if extensive fetomaternal hemorrhage was measured after birth. Of the 270 women who gave birth to an Rh(D)-positive baby, 248 women were evaluated for Rh(D) immunization 6 to 11.5 months postpartum. None of these women developed antibodies against the Rh(D) antigen.
14.2 ITP
In an open-label, single-arm, multicenter study, 98 Rh(D)-positive adult subjects with chronic ITP and a platelet count of 30 × 109/L or less were treated with RHOPHYLAC. Subjects received a single intravenous dose of 250 IU (50 mcg) per kg body weight.
The primary efficacy endpoint was the response rate defined as achieving a platelet count of ≥30 × 109/L as well as an increase of >20 × 109/L within 15 days after treatment with RHOPHYLAC. Secondary efficacy endpoints included the response rate defined as an increase in platelet counts to ≥50 × 109/L within 15 days after treatment and, in subjects who had bleeding at baseline, the regression of hemorrhage defined as any decrease from baseline in the severity of overall bleeding status.
Table 6 presents the primary response rates for the intent-to-treat (ITT) and per-protocol (PP) populations.
| Primary Response Rate at Day 15 | ||||
|---|---|---|---|---|
| Analysis Population | No. Subjects | No. Responders | % Responders | 95% Confidence Interval (CI) |
| ITT | 98 | 65 | 66.3% | 56.5%, 74.9% |
| PP | 92 | 62 | 67.4% | 57.3%, 76.1% |
The primary efficacy response rate (ITT population) demonstrated a clinically relevant response to treatment, i.e., the lower bound of the 95% confidence interval (CI) was greater than the predefined response rate of 50%. The median time to platelet response was 3 days, and the median duration of platelet response was 22 days.
Table 7 presents the response rates by baseline platelet count for subjects in the ITT population.
| Response Rates at Day 15 | |||
|---|---|---|---|
| Baseline Platelet count (× 109/L) | Total No. Subjects | No. (%) Subjects Achieving a Platelet Count of ≥30 × 109/L and an Increase of >20 × 109/L | No. (%) Subjects With an Increase in Platelet Counts to ≥50 × 109/L |
|
|||
| ≤10 | 38 | 15 (39.5) | 10 (26.3) |
| >10 to 20 | 28 | 22 (78.6) | 17 (60.7) |
| >20 to 30 | 27 | 24 (88.9) | 22 (81.5) |
| >30* | 5 | 4 (80.0) | 5 (100.0) |
| Overall (all subjects) | 98 | 65 (66.3) | 54 (55.1) |
During the study, an overall regression of hemorrhage was seen in 44 (88%, 95% CI: 76% to 94%) of the 50 subjects with bleeding at baseline. The percentage of subjects showing a regression of hemorrhage increased from 20% at Day 2 to 64% at Day 15. There was no evidence of an association between the overall hemorrhage regression rate and baseline platelet count.
Approximately half of the 98 subjects in the ITT population had evidence of bleeding at baseline. Post-baseline, the percentage of subjects without bleeding increased to a maximum of 70.4% at Day 8.
15. References
- Pollack W, Ascari WQ, Kochesky RJ, O'Connor RR, Ho TY, Tripodi D. Studies on Rh prophylaxis. 1. relationship between doses of anti-Rh and size of antigenic stimulus. Transfusion. 1971;11:333-339.
- Gaines AR. Disseminated intravascular coagulation associated with acute hemoglobinemia or hemoglobinuria following Rh0(D) immune globulin intravenous administration for immune thrombocytopenic purpura. Blood. 2005;106:1532-1537.
- Centers for Disease Control and Prevention. General recommendations on immunization: recommendations of the Advisory Committee on Immunization Practices and the American Academy of Family Physicians. MMWR 2002;51 (No. RR-2):6-7.
- Thornton JG, Page C, Foote G, Arthur GR, Tovey LAD, Scott JS. Efficacy and long term effects of antenatal prophylaxis with anti-D immunoglobulin. Br Med J. 1989;298:1671-1673.
- Stucki M, Moudry R, Kempf C, Omar A, Schlegel A, Lerch PG. Characterisation of a chromatographically produced anti-D immunoglobulin product. J Chromatogr B. 1997;700:241-248.
- Horowitz B, Chin S, Prince AM, Brotman B, Pascual D, Williams B. Preparation and characterization of S/D-FFP, a virus sterilized "fresh frozen plasma". J Thromb Haemost. 1991;65:1163.
- Horowitz B, Bonomo R, Prince AM, Chin S, Brotman B, Shulman RW. Solvent/detergent-treated plasma: a virus-inactivated substitute for fresh frozen plasma. Blood. 1992;79:826-831.
- Lazarus AH, Crow AR. Mechanism of action of IVIG and anti-D in ITP. Transfus Apher Sci. 2003;28:249-255.
- Bichler J, Schöndorfer G, Pabst G, Andresen I. Pharmacokinetics of anti-D IgG in pregnant RhD-negative women. BJOG. 2003;110:39-45.
- Ware RE, Zimmerman SA. Anti-D: mechanisms of action. Semin Hematol. 1998;35:14-22.
- MacKenzie IZ, Bichler J, Mason GC, et al. Efficacy and safety of a new, chromatographically purified rhesus (D) immunoglobulin. Eur J Obstetr Gynecol Reprod Biol. 2004;117:154-161.
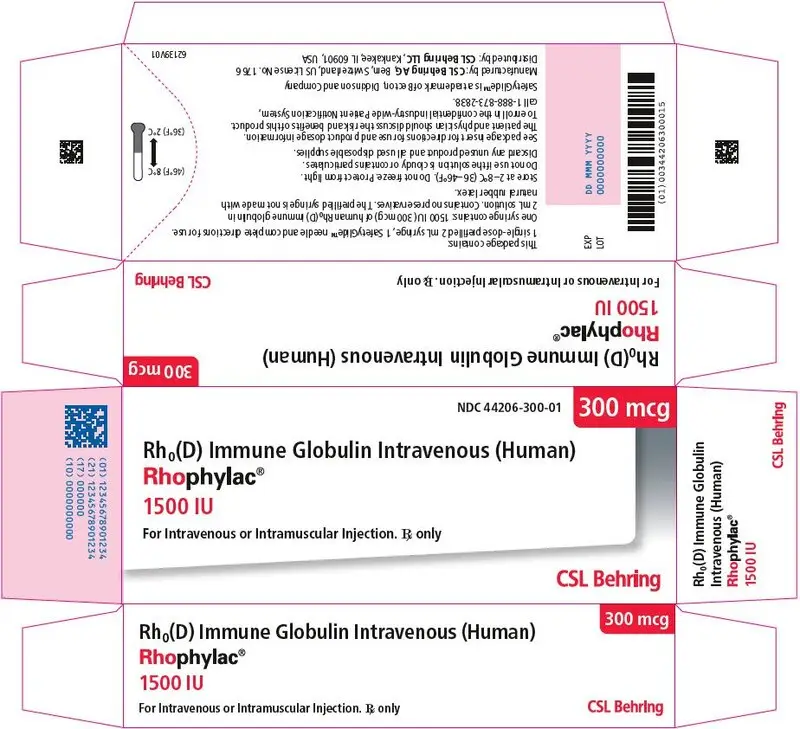
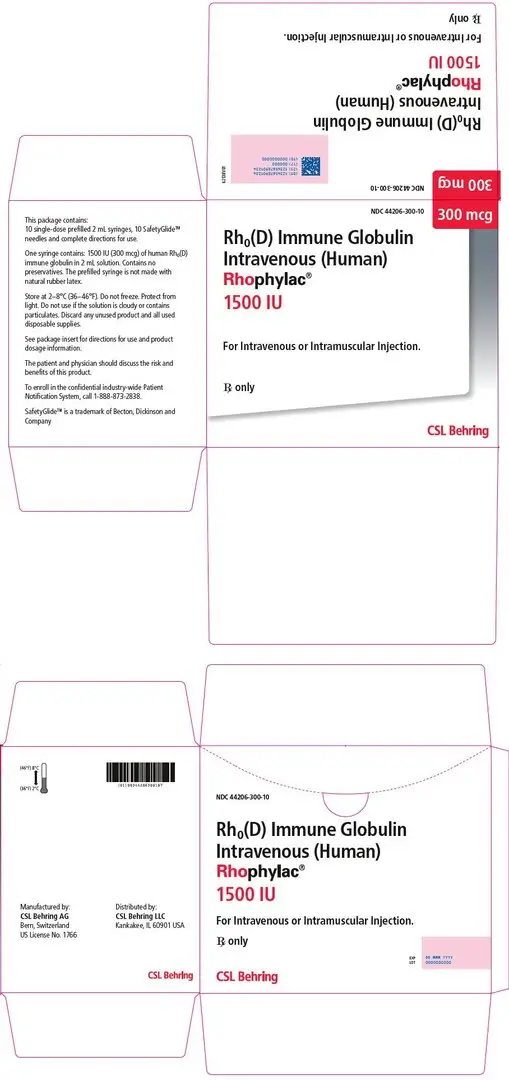
16. How is Rhophylac supplied
- RHOPHYLAC 1500 IU (300 mcg) is supplied in packages of one or ten (10) single-dose, prefilled, ready-to-use, glass syringe(s), each containing 2 mL liquid for injection. Each syringe is accompanied by a SafetyGlide™ needle for intravenous or intramuscular use.
Each product presentation includes a package insert and the following components:
| Presentation | Carton NDC Number | Components |
|---|---|---|
| 1500 IU (300 mcg) | 44206-300-01 |
|
| 1500 IU (300 mcg) Multipack | 44206-300-10 |
|
17. Patient Counseling Information
Please inform patients of the following:
- Immediately report the following signs and symptoms to their physician: hives, chest tightness, wheezing, hypotension, and anaphylaxis [see Warnings and Precautions (5.1)].
- RHOPHYLAC is made from human blood and may contain infectious agents that can cause disease (e.g., viruses and, theoretically, the CJD agent). Explain that the risk RHOPHYLAC may transmit an infectious agent has been reduced by screening all plasma donors, by testing the donated plasma for certain viruses, and by inactivating and/or removing certain viruses during manufacturing. Advise patients to report any symptoms that concern them and that may be related to viral infections [see Warnings and Precautions (5.3)].
- RHOPHYLAC may interfere with the response to live virus vaccines (e.g., measles, mumps, rubella, and varicella), and instruct them to notify their healthcare professional of this potential interaction when they are receiving vaccinations.
- Receiving the antepartum dose of RHOPHYLAC for suppression of Rh isoimmunization will need a second dose within 72 hours of birth if the baby's blood type is Rh-positive.
- Patients being treated with RHOPHYLAC for ITP to immediately report symptoms of intravascular hemolysis, including back pain, shaking chills, fever, discolored urine, decreased urine output, sudden weight gain, edema, and/or shortness of breath [see Warnings and Precautions (5.4)].
| RHOPHYLAC
human rho(d) immune globulin solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - CSL Behring AG (481152762) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| CSL Behring AG | 481152762 | MANUFACTURE(44206-300) | |