Drug Detail:Tarpeyo (Budesonide (oral) [ bue-des-oh-nide ])
Drug Class: Glucocorticoids
Highlights of Prescribing Information
TARPEYO (budesonide) delayed release capsules, for oral use
Initial U.S. Approval: 1997
Indications and Usage for Tarpeyo
TARPEYO is a corticosteroid indicated to reduce proteinuria in adults with primary immunoglobulin A nephropathy (IgAN) at risk of rapid disease progression, generally a urine protein-to-creatinine ratio (UPCR) ≥ 1.5 g/g. (1)
This indication is approved under accelerated approval based on a reduction in proteinuria. It has not been established whether TARPEYO slows kidney function decline in patients with IgAN. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory clinical trial. (1)
Tarpeyo Dosage and Administration
- The recommended dosage is 16 mg administered orally once daily, in the morning at least 1 hour before a meal. (2)
- Swallow whole. Do not open, crush or chew. (2)
When discontinuing, reduce dosage to 8 mg once daily for the last two weeks. (2, 5.1)
Dosage Forms and Strengths
Delayed release capsules: 4 mg (3)
Contraindications
- Hypersensitivity to budesonide or any of the ingredients in TARPEYO. (4)
Warnings and Precautions
- Hypercorticism and Adrenal Axis Suppression: Follow general warnings concerning corticosteroids, patients with hepatic impairment may be at increased risk. Taper upon discontinuation. (2, 5.1, 8.6, 12.3)
- Risks of immunosuppression: Avoid use in patients with active or quiescent tuberculosis infection, untreated fungal, bacterial, systemic viral or parasitic infections, or ocular herpes simplex. May affect vaccine efficacy. (5.2)
- Other Corticosteroid Effects: Monitor patients with concomitant conditions where corticosteroids may have unwanted effects (e.g., hypertension, diabetes mellitus). (5.3)
Adverse Reactions/Side Effects
Most common adverse reactions ( ≥5%) are hypertension, peripheral edema, muscle spasms, acne, dermatitis, weight increase, dyspnea, face edema, dyspepsia, fatigue, hirsutism. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Calliditas Therapeutics at 1-844-IGA-0011 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
Potent CYP3A4 Inhibitors (e.g. ketoconazole, grapefruit juice): Can increase systemic budesonide concentrations: avoid concomitant use. (7.1)
Use In Specific Populations
Lactation: Routine monitoring of linear growth in infants is recommended with chronic use of budesonide in the nursing mother. (8.2).
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 12/2021
Related/similar drugs
budesonide, cyclophosphamide, Cytoxan, sparsentan, FilspariFull Prescribing Information
1. Indications and Usage for Tarpeyo
TARPEYO is indicated to reduce proteinuria in adults with primary immunoglobulin A nephropathy (IgAN) at risk of rapid disease progression, generally a urine protein-to-creatinine ratio (UPCR) ≥1.5 g/g.
This indication is approved under accelerated approval based on a reduction in proteinuria. It has not been established whether TARPEYO slows kidney function decline in patients with IgAN. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory clinical trial.
2. Tarpeyo Dosage and Administration
The recommended duration of therapy is 9 months, with a dosage of 16 mg administered orally once daily [see Clinical Studies (14.1)]. When discontinuing therapy, reduce the dosage to 8 mg once daily for the last 2 weeks of therapy [see Warnings and Precautions (5.1)].
The delayed release capsules should be swallowed whole in the morning, at least 1 hour before a meal. Do not open, crush or chew.
If a dose is missed, take the prescribed dose at the next scheduled time. Do not double the next dose.
Safety and efficacy of treatment with subsequent courses of TARPEYO have not been established.
3. Dosage Forms and Strengths
Delayed release capsule containing 4 mg budesonide. White coated opaque capsules printed with “CAL10 4MG” in black ink.
4. Contraindications
TARPEYO is contraindicated in patients with hypersensitivity to budesonide or any of the ingredients of TARPEYO. Serious hypersensitivity reactions, including anaphylaxis have occurred with other budesonide formulations.
5. Warnings and Precautions
5.1 Hypercorticism and Adrenal Axis Suppression
When corticosteroids are used chronically, systemic effects such as hypercorticism and adrenal suppression may occur. Corticosteroids can reduce the response of the hypothalamus-pituitary-adrenal (HPA) axis to stress. In situations where patients are subject to surgery or other stress situations, supplementation with a systemic corticosteroid is recommended. When discontinuing therapy [see Dosing and Administration (2)] or switching between corticosteroids, monitor for signs of adrenal axis suppression.
Patients with moderate to severe hepatic impairment (Child-Pugh Class B and C respectively) could be at an increased risk of hypercorticism and adrenal axis suppression due to an increased systemic exposure of oral budesonide. Avoid use in patients with severe hepatic impairment (Child-Pugh Class C). Monitor for increased signs and/or symptoms of hypercorticism in patients with moderate hepatic impairment (Child-Pugh Class B) [see Use in Specific Populations (8.6), Clinical Pharmacology (12.3)].
5.2 Risks of Immunosupression
Patients who are on drugs that suppress the immune system are more susceptible to infection than healthy individuals. Chickenpox and measles, for example, can have a more serious or even fatal course in susceptible patients or patients on immunosuppressant doses of corticosteroids. Avoid corticosteroid therapy in patients with active or quiescent tuberculosis infection, untreated fungal, bacterial, systemic viral or parasitic infections, or ocular herpes simplex. Avoid exposure to active, easily-transmitted infections (e.g., chicken pox, measles). Corticosteroid therapy may decrease the immune response to some vaccines.
How the dose, route, and duration of corticosteroid administration affect the risk of developing a disseminated infection is not known. The contribution of the underlying disease and/or prior corticosteroid treatment to the risk is also not known. If exposed to chickenpox, consider therapy with varicella zoster immune globulin (VZIG) or pooled intravenous immunoglobulin (IVIG). If exposed to measles, consider prophylaxis with pooled intramuscular immunoglobulin (IG). If chickenpox develops, consider treatment with antiviral agents.
5.3 Other Corticosteroid Effects
TARPEYO is a systemically available corticosteroid and is expected to cause related adverse reactions. Monitor patients with hypertension, prediabetes, diabetes mellitus, osteoporosis, peptic ulcer, glaucoma or cataracts, or with a family history of diabetes or glaucoma, or with any other condition where corticosteroids may have unwanted effects.
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Hypercorticism and adrenal suppression [see Warnings and Precautions (5.1)]
- Risks of immunosuppression [see Warnings and Precautions (5.2)]
- Other corticosteroid effects [see Warnings and Precautions (5.3)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The safety of TARPEYO has been evaluated in a randomized controlled study in 197 patients.
The most common adverse reactions reported in greater than or equal to 5% of TARPEYO-treated patients are listed in Table 1.
The majority of adverse reactions were mild or moderate in severity.
| Adverse Reaction | TARPEYO 16 mg (N=97) | Placebo (N=100) |
| n (%) | n (%) | |
| Patients with any Adverse Reaction | 84 (87) | 73 (73) |
| Hypertension | 15 (16) | 2 (2) |
| Peripheral edema | 14 (14) | 4 (4) |
| Muscle spasms | 13 (13) | 4 (4) |
| Acne | 11 (11) | 2 (2) |
| Dermatitis | 7 (7) | 1 (1) |
| Weight increased | 7 (7) | 3 (3) |
| Dyspnea | 6 (6) | 0 (0) |
| Face edema | 6 (6) | 1 (1) |
| Dyspepsia | 5 (5) | 2 (2) |
| Fatigue | 5 (5) | 2 (2) |
| Hirsutism | 5 (5) | 0 (0) |
Most adverse reactions that occurred at a greater incidence for TARPEYO compared to placebo were consistent with hypercortisolism.
7. Drug Interactions
7.1 Interaction with CYP3A4 Inhibitors
Budesonide is a substrate for CYP3A4. Avoid use with potent CYP3A4 inhibitors; e.g. ketoconazole, itraconazole, ritonavir, indinavir, saquinavir, erythromycin, and cyclosporine [see Clinical Pharmacology (12.3)].
Avoid ingestion of grapefruit juice with TARPEYO. Intake of grapefruit juice, which inhibits CYP3A4 activity, can increase the systemic exposure to budesonide [see Clinical Pharmacology (12.3)].
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
The available data from published case series, epidemiological studies and reviews with oral budesonide use in pregnant women have not identified a drug-associated risk of major birth defects, miscarriage or other adverse maternal or fetal outcomes. There are risks to the mother and fetus associated with IgA Nephropathy. Infants exposed to in-utero corticosteroids, including budesonide, are at risk for hypoadrenalism (see Clinical Considerations). In animal reproduction studies with pregnant rats and rabbits, administration of subcutaneous budesonide during organogenesis at doses approximately 0.3 times or 0.03 times, respectively, the maximum recommended human dose (MRHD), resulted in increased fetal loss, decreased pup weights, and skeletal abnormalities. Maternal toxicity was observed in both rats and rabbits at these dose levels (see Data).
The estimated background risk of major birth defects and miscarriage of the indicated population is unknown. All pregnancies have a background risk of birth defect, loss, or other adverse outcomes. In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Clinical Considerations
Disease-Associated Maternal and/or Embryo/Fetal Risk
IgA nephropathy in pregnancy is associated with adverse maternal outcomes, including increased rates of cesarean section, pregnancy-induced hypertension, pre-eclampsia and preterm delivery, and adverse fetal/neonatal outcomes, including stillbirth and low birth weight.
Fetal/Neonatal Adverse Reactions
Hypoadrenalism may occur in infants born to mothers receiving corticosteroids during pregnancy. Infants should be carefully observed for signs of hypoadrenalism, such as poor feeding, irritability, weakness, and vomiting, and managed accordingly [see Warnings and Precautions (5.1)].
Data
Animal Data
Budesonide was teratogenic and embryo-lethal in rabbits and rats.
In an embryo-fetal development study in pregnant rats dosed subcutaneously with budesonide during the period of organogenesis on gestation days 6 to 15 there were effects on fetal development and survival at subcutaneous doses up to approximately 500 mcg/kg in rats (approximately 0.3 times the maximum recommended human dose (MRHD) on a body surface area basis).
In an embryo-fetal development study in pregnant rabbits dosed during the period of organogenesis on gestation days 6 to 18, there was an increase in maternal abortion, and effects on fetal development and reduction in litter weights at subcutaneous doses from approximately 25 mcg/kg (approximately 0.03 times the MRHD on a body surface area basis).
Maternal toxicity, including reduction in body weight gain, was observed at subcutaneous doses of 5 mcg/kg in rabbits (approximately 0.006 times the maximum recommended human dose on a body surface area basis) and 500 mcg/kg in rats (approximately 0.3 times the maximum recommended human dose on a body surface area basis).
In a peri- and post-natal development study, subcutaneous treatment of pregnant rats with budesonide during the period from Day 15 post coitum to Day 21 post partum, budesonide had no effects on delivery, but did have an effect on growth and development of offspring. In addition, offspring survival was reduced and surviving offspring had decreased mean body weights at birth and during lactation at exposures ≥ 0.012 times the MRHD (on a mg/m2 basis at maternal subcutaneous doses of 20 mcg/kg/day and higher). These findings occurred in the presence of maternal toxicity.
8.2 Lactation
Risk Summary
Breastfeeding is not expected to result in significant exposure of the infant to TARPEYO. Lactation studies have not been conducted with oral budesonide, including TARPEYO, and no information is available on the effects of the drug on the breastfed infant or the effects on the drug on milk production. One published study reports that budesonide is present in human milk following maternal inhalation of budesonide (see Data). Routine monitoring of linear growth in infants is recommended with chronic use of budesonide in the nursing mother. The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for TARPEYO and any potential adverse effects on the breastfed infant from TARPEYO, or from the underlying maternal condition.
Data
One published study reports that budesonide is present in human milk following maternal inhalation of budesonide, which resulted in infant doses approximately 0.3% to 1% of the maternal weight-adjusted dosage and a milk to plasma ratio was approximately 0.5. Budesonide was not detected in plasma, and no adverse events were noted in the breastfed infants following maternal use of inhaled budesonide.
Assuming a daily average milk intake of about 150 mL/kg/day and a milk to plasma ratio of 0.5, the estimated oral dose of budesonide for a 5 kg infant is expected to be less than 2 mcg/day for a maternal dose of 16 mg TARPEYO. Assuming 100% bio-availability in the infant this is about 0.1% of the maternal dose and about 3% of the highest inhaled dose used clinically for asthma in infants.
8.4 Pediatric Use
The safety and efficacy of TARPEYO in pediatric patients have not been established.
8.5 Geriatric Use
Clinical studies of TARPEYO did not include sufficient numbers of subjects aged 65 and over to determine whether they respond differently from younger subjects. Other reported clinical experience has not identified differences in responses between the elderly and younger patients. In general, dose selection for an elderly patient should be cautious, reflecting the greater frequency of decreased hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
8.6 Hepatic Impairment
Patients with moderate to severe hepatic impairment (Child-Pugh Class B and C, respectively) could be at an increased risk of hypercorticism and adrenal axis suppression due to an increased systemic exposure to budesonide [see Warnings and Precautions (5.1) and Clinical Pharmacology (12.3)]. Avoid use in patients with severe hepatic impairments (Child-Pugh Class C). Monitor for increased signs and/or symptoms of hypercorticism in patients with moderate hepatic impairment (Child-Pugh Class B).
10. Overdosage
Reports of acute toxicity and/or death following overdosage of corticoids are rare.
In the event of acute overdosage, no specific antidote is available. Treatment consists of supportive and symptomatic therapy.
11. Tarpeyo Description
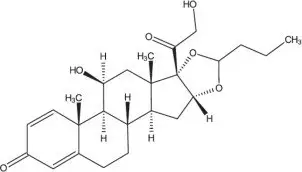
TARPEYO (budesonide) delayed release capsules, for oral administration, contain budesonide, a synthetic corticosteroid, as the active ingredient. Budesonide is designated chemically as 16α, 17α-[(1RS)-Butylidenebis(oxy)]-11β, 21-dihydroxypregna-1,4-diene-3,20-dione.
Budesonide is provided as a mixture of two epimers (22R and 22S). The empirical formula of budesonide is C25H34O6 and its molecular weight is 430.5. Its structural formula is:
Budesonide is a white to off-white, tasteless, odorless powder that is practically insoluble in water, sparingly soluble in alcohol, and freely soluble in chloroform.
The beads in each capsule contain the following inactive ingredients: sugar spheres (sucrose and starch), hypromellose, polyethylene glycol, citric acid monohydrate, ethyl cellulose, medium chain triglycerides and oleic acid. The capsule shells contain hypromellose and titanium oxide (E171); and the printing ink on the capsules contain shellac, propylene glycol and black iron oxide (E172). The enteric coating on the capsules contain: methacrylic acid and methacrylate copolymer, talc and dibutyl sebacate.
12. Tarpeyo - Clinical Pharmacology
12.1 Mechanism of Action
Budesonide is a corticosteroid with potent glucocorticoid activity and weak mineralocorticoid activity that undergoes substantial first pass metabolism. Mucosal B-cells present in the ileum, including the Peyer's patches, express glucocorticoid receptors and are responsible for the production of galactose-deficient IgA1 antibodies (Gd-Ag1) causing IgA nephropathy. Through their anti-inflammatory and immunosuppressive effects at the glucocorticoid receptor, corticosteroids can modulate B-cell numbers and activity. It has not been established to what extent TARPEYO's efficacy is mediated via local effects in the ileum vs systemic effects.
12.2 Pharmacodynamics
Treatment with corticosteroids, including TARPEYO, is associated with a suppression of endogenous cortisol concentrations and an impairment of the hypothalamus-pituitary-adrenal (HPA) axis function.
12.3 Pharmacokinetics
Absorption
Following single oral administration of TARPEYO 16 mg to healthy subjects, the average geometric mean Cmax (CV%) was 4.4 ng/mL (58.3), and AUC0-24 was 24.1 h*ng/mL (49.7). Median Tlag (min, max) was 3.1 h (0, 6) while median Tmax (min, max) was 5.1 h (4.5, 10).
Distribution
Approximately 85 to 90% of budesonide binds to plasma proteins in blood over the concentration range of 0.43 to 99 ng/mL. The volume of distribution at steady state reported in the literature is 3 to 4 L/kg.
Metabolism
Budesonide is metabolized by the liver (and to lesser extent the gut), primarily by oxidative pathways via CYP3A4 to two main metabolites, 16α-hydroxyprednisolone and 6β-hydroxybudesonide, which have less than 1% of the corticosteroid activity of budesonide.
Elimination
Budesonide had a high plasma clearance, 0.9 to 1.8 L/min in healthy adults, which is close to the estimated liver blood flow, and, accordingly, suggests that budesonide is a high hepatic clearance drug.
Following single oral administration of TARPEYO 16 mg to healthy subjects, the elimination half-life (t½) for TARPEYO ranged from 5.0 to 6.8 hours.
Excretion
Budesonide was excreted in urine and feces in the form of metabolites. After oral as well as intravenous administration of micronized [3H]-budesonide, approximately 60% of the recovered radioactivity was found in urine. The major metabolites, including 16α-hydroxyprednisolone and 6β-hydroxybudesonide, are mainly renally excreted, intact or in conjugated forms. No unchanged budesonide was detected in urine.
Specific Populations
Age, race, and body weight
The effect of age, race, and body weight on the pharmacokinetics of TARPEYO has not been established.
Sex
Of the 143 healthy volunteers included in the Phase 1 studies, 29% were female. Pharmacokinetics of budesonide was similar between males and females.
Hepatic Impairment
Subjects with moderate hepatic impairment (Child-Pugh class B) had 3.5 times the budesonide AUC compared with healthy volunteers while subjects with mild hepatic impairment (Child-Pugh class A) had approximately 40% higher budesonide AUC compared with healthy volunteers.
Patients with severe hepatic impairment (Child-Pugh Class C) have not been studied.
Drug Interaction Studies
Budesonide is metabolized via CYP3A4. Potent inhibitors of CYP3A4 can increase plasma levels of budesonide.
Thus, clinically relevant drug interactions with potent CYP3A inhibitors, such as ketoconazole, itraconazole, ritonavir, indinavir, saquinavir, erythromycin, cyclosporine, and grapefruit juice, are to be expected. Conversely, induction of CYP3A4 potentially could result in the lowering of budesonide plasma concentrations.
Effects of Other Drugs on Budesonide
Ketoconazole
In an open, non-randomized, cross-over study, 6 healthy subjects were given budesonide 10 mg as a single dose, either alone or concomitantly with the last ketoconazole dose of 3 days treatment with ketoconazole 100 mg twice daily. Co-administration of ketoconazole resulted in 8-fold the AUC of budesonide, compared to budesonide alone.
In an open, randomized, cross-over study 8 healthy subjects were given Entocort EC 3 mg as a single dose, either alone or concomitantly with the last ketoconazole dose of 4 days treatment with ketoconazole 200 mg once daily. Co-administration of ketoconazole resulted in 6.5-fold the AUC of budesonide, compared to budesonide alone.
Grapefruit Juice
In an open, randomized, cross-over study, 8 healthy subjects were given Entocort EC 3 mg, either alone, or concomitantly with 600 mL concentrated grapefruit juice (which inhibits CYP3A4 activity predominantly in the intestinal mucosa), on the last of 4 daily administrations. Concomitant administration of grapefruit juice resulted in doubling the bioavailability of budesonide compared to budesonide alone.
Proton Pump Inhibitors
The pharmacokinetics of TARPEYO have not been evaluated in combination with proton pump inhibitors (PPIs). Since the disintegration of TARPEYO is pH dependent, the release properties and uptake of budesonide may be altered when TARPEYO is taken after treatment with PPIs. In a study assessing intragastric and intraduodenal pH in healthy volunteers after repeated dosing with the PPI omeprazole 40 mg once daily, intragastric and intraduodenal pH did not exceed that required for disintegration of TARPEYO. Beyond the duodenum, PPIs such as omeprazole are unlikely to affect pH.
Oral Contraceptives (CYP3A4 Substrates)
In a parallel study, the pharmacokinetics of budesonide were not significantly different between healthy female subjects who received oral contraceptives containing desogestrel 0.15 mg and ethinyl estradiol 30 μg and healthy female subjects who did not receive oral contraceptives. Budesonide 4.5 mg once daily for one week did not affect the plasma concentrations of ethinyl estradiol, a CYP3A4 substrate. The effect of budesonide 16 mg once daily on the plasma concentrations of desogestrel and ethinyl estradiol was not studied.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenicity studies with budesonide were conducted in rats and mice. In a two-year study in Sprague-Dawley rats, budesonide caused a statistically significant increase in the incidence of gliomas in male rats at an oral dose of 50 mcg/kg (approximately 0.03 times the maximum recommended human dose (MRHD) on a body surface area basis). In addition, there were increased incidences of primary hepatocellular tumors in male rats at 25 mcg/kg (approximately 0.015 times the MRHD on a body surface area basis) and above. No tumorigenicity was seen in female rats at oral doses up to 50 mcg/kg (approximately 0.03 times the MRHD on a body surface area basis). In an additional two-year study in male Sprague-Dawley rats, budesonide caused no gliomas at an oral dose of 50 mcg/kg (approximately 0.03 times the MRHD on a body surface area basis). However, it caused a statistically significant increase in the incidence of hepatocellular tumors at an oral dose of 50 mcg/kg (approximately 0.03 times the MRHD of a body surface area basis). The concurrent reference corticosteroids (prednisolone and triamcinolone acetonide) showed similar findings. In a 91-week study in mice, budesonide caused no treatment-related carcinogenicity at oral doses up to 200 mcg/kg (approximately 0.06 times the MRHD on a body surface area basis).
Budesonide was not genotoxic in the Ames text, the mouse lymphoma cell forward gene mutation (TK+/-) test, the human lymphocyte chromosome aberration test, the Drosophila melanogaster sex-linked recessive lethal test, the rat hepatocyte UDS test and the mouse micronucleus test.
In rats, budesonide had no effect on fertility at subcutaneous doses up to 80 mcg/kg (approximately 0.05 times the MRHD on a body surface area basis). However, it caused a decrease in prenatal viability and viability in pups at birth and during lactation, along with a decrease in maternal food consumption and body weight gain, at subcutaneous doses of 20 mcg/kg (approximately 0.012 times the MRHD on a body surface area basis) and above. No such effects were noted at 5 mcg/kg (approximately 0.003 times the MRHD on a body surface area basis).
14. Clinical Studies
14.1 Treatment of IgAN
The effect of TARPEYO on proteinuria was assessed in a randomized, double-blind, multicenter study (Nef-301, NCT: 03643965) in patients with biopsy-proven IgAN, eGFR ≥35 mL/min/1.73 m2, and proteinuria (defined as either ≥1 g/day or UPCR ≥0.8 g/g) who were on a stable dose of maximally-tolerated RAS inhibitor therapy. Patients with other glomerulopathies, nephrotic syndrome, or those who had been treated with systemic immunosuppressive medications were excluded. Patients were randomized 1:1 to either TARPEYO 16 mg once daily or placebo and treated for nine months followed by a 2-week taper of either TARPEYO 8 mg once daily or placebo.
Of the 199 patients who completed the Month 9 visit, 68% were male, 86% were Caucasian, 12% were Asian, and 16% were from the US. The median age was 44 years (range 23 to 73 years). At baseline, the mean eGFR was approximately 58 mL/min/1.73 m2, with 62% of patients having an eGFR <60 mL/min/1.73 m2. The mean baseline UPCR was 1.6 g/g and 25% of patients had proteinuria >3.5 g/24 hours. Approximately 73% of patients had a history of hypertension and 5% had a history of type 2 diabetes mellitus. At baseline, 98% were treated with an ACE inhibitor or ARB and <1% of patients were on an SGLT2 inhibitor.
The primary endpoint was the percentage reduction in UPCR at 9 months compared to baseline. The results are shown in Table 2.
|
a All patients with a UPCR reading regardless of use of prohibited medication at 9 months. |
||
|
bAdjusted geometric least squares mean ratio of UPCR relative to baseline were based on a longitudinal repeated measures model. |
||
|
c The estimate of the ratio of geometric mean ratio of UPCR relative to baseline comparing TARPEYO 16 mg with placebo was reported as percentage reduction along with the respective 95% confidence interval from the longitudinal repeated measures model and p-values. |
||
|
CI: confidence interval; UPCR: urine protein creatinine ratio. |
||
| Primary Endpoint: UPCR g/g a | TARPEYO 16 mg
(N=97) | Placebo
(N=102) |
| Percentage reduction from baseline (Adjusted for baseline) b | 34% | 5% |
| TARPEYO 16 mg versus Placebo : Percentage reduction (95% CI) c; 2-sided p-value | 31% (16% to 42%); p=0.0001 |
|
The treatment effect for the UPCR endpoint at 9 months were consistent across key subgroups, including key demographic (such as age, sex, race) and baseline disease (such as baseline proteinuria) characteristics.
16. How is Tarpeyo supplied
TARPEYO (budesonide) delayed release capsules 4 mg, are white opaque- coated capsules marked with “CAL10 4 MG” in black ink on the body of the capsule. They are supplied as follows:
NDC 81749-004-01: Bottles of 120 capsules. Child-resistant cap.
Store at 20-25°C (68 - 77°F); excursions permitted to 15° to 30°C (59° to 86°F). [See USP Controlled Room Temperature].
Keep container tightly closed. Protect from moisture.
17. Patient Counseling Information
Advise the patient to read the FDA-approved patient labeling (Patient Information).
Advise patients that TARPEYO may cause hypercorticism and adrenal axis suppression and to follow a taper schedule, as instructed by their healthcare provider if discontinuing therapy [see Warnings and Precautions (5.1)].
TARPEYO causes immunosuppression. Advise patients to avoid exposure to people with chicken pox or measles and, if exposed, to consult their healthcare provider immediately. There is an increased risk of developing a variety of infections, including worsening of existing tuberculosis, fungal, bacterial, viral or parasitic infections, or ocular herpes simplex, and to contact their healthcare provider if they develop any symptoms of infection [see Warnings and Precautions (5.3)]. Provide advice regarding vaccination schedules for immunocompromised patients.
Advise patients that TARPEYO delayed release capsules should be swallowed whole and not chewed, crushed or broken and to take TARPEYO in the morning, at least 1 hour before a meal [See Dosage and Administration (2)].
Advise patients to avoid the consumption of grapefruit juice for the duration of their TARPEYO therapy [See Drug Interactions (7.1)].
TARPEYO is a trademark of Calliditas Therapeutics AB, or its affiliates.
© 2021 Calliditas Therapeutics AB (publ)
Manufactured for and distributed by:
Calliditas Therapeutics AB
Stockholm, Sweden
Patent: http://www.calliditas.com/patents
|
This Patient Information has been approved by the U.S. Food and Drug Administration. |
Issued: 12/2021 |
|
| Patient Information
TARPEYO (tar-PAY-oh) (budesonide) delayed release capsules |
||
| What is TARPEYO?
TARPEYO is a prescription medicine used to reduce levels of protein in the urine (proteinuria) in adults with a kidney disease called primary immunoglobulin A nephropathy (IgAN), who are at high risk of disease progression. It is not known if TARPEYO is safe and effective in children. |
||
| Do not take TARPEYO if you are allergic to budesonide or any of the ingredients in TARPEYO. See the end of this leaflet for a complete list of ingredients in TARPEYO. | ||
Before taking TARPEYO, tell your healthcare provider about all of your medical conditions, including if you:
|
||
| Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. TARPEYO and other medicines may affect each other causing side effects. | ||
How should I take TARPEYO?
|
||
| What should I avoid while taking TARPEYO?
Do not eat grapefruit or drink grapefruit juice during your treatment with TARPEYO. Eating grapefruit or drinking grapefruit juice can increase the level of TARPEYO in your blood. |
||
| What are the possible side effects of TARPEYO?
TARPEYO may cause serious side effects, including:
|
||
|
|
|
|
||
|
|
|
| Tell your healthcare provider if you are under stress or have any symptoms of adrenal suppression during treatment with TARPEYO. |
||
|
||
|
|
|
| The most common side effects of TARPEYO include: | ||
|
|
|
| These are not all the possible side effects of TARPEYO. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||
How should I store TARPEYO?
|
||
| Keep TARPEYO and all medicines out of the reach of children. | ||
| General information about the safe and effective use of TARPEYO.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use TARPEYO for a condition for which it was not prescribed. Do not give TARPEYO to other people, even if they have the same symptoms you have. It may harm them. You can ask your pharmacist or healthcare provider for information about TARPEYO that is written for health professionals. |
||
| What are the ingredients in TARPEYO?
Active ingredient: budesonide Inactive ingredients: sugar spheres (sucrose and starch), hypromellose, polyethylene glycol, citric acid monohydrate, ethyl cellulose, medium chain triglycerides and oleic acid. The capsules contain: hypromellose and titanium oxide (E171). The printing ink on the capsules contain: shellac, propylene glycol and black iron oxide (E172). The enteric coating on the capsules contain: methacrylic acid and methacrylate copolymer, talc and dibutyl sebacate. |
||
| Manufactured for and distributed by: Calliditas Therapeutics AB, Stockholm, Sweden TARPEYO is a trademark of Calliditas Therapeutics AB, or its affiliates. © 2021 Calliditas Therapeutics AB (publ) Patent: http://www.calliditas.com/patents For more information, go to www.TARPEYOTouchpoints.com or call 1-933-444-8277. |
||
| TARPEYO
budesonide capsule, delayed release |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| Labeler - Calliditas Therapeutics AB (351157735) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Micro-Macinazione S.A. | 480918515 | PARTICLE SIZE REDUCTION(81749-004) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Minakem Dunkerque Production S.A.S | 277412599 | API MANUFACTURE(81749-004) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Patheon Pharmaceuticals Inc. | 005286822 | MANUFACTURE(81749-004) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Sicor Società Italiana Corticosteroidi S.r.l | 338950678 | API MANUFACTURE(81749-004) | |