Drug Detail:Zirabev (Bevacizumab [ bev-a-ciz-oo-mab ])
Drug Class: VEGF/VEGFR inhibitors
Highlights of Prescribing Information
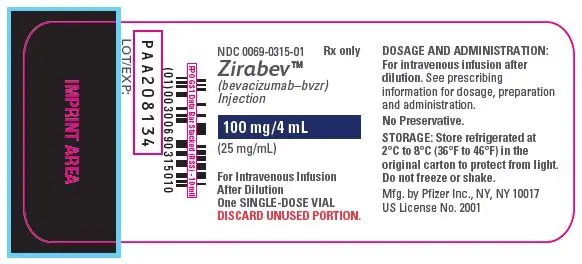
ZIRABEV™ (bevacizumab-bvzr) injection, for intravenous use
Initial U.S. Approval: 2019
ZIRABEV (bevacizumab-bvzr) is biosimilar* to AVASTIN (bevacizumab).
Recent Major Changes
|
Warnings and Precautions, Infusion-Related Reactions (5.9) |
02/2023 |
Indications and Usage for Zirabev
ZIRABEV is a vascular endothelial growth factor inhibitor indicated for the treatment of:
- •
- Metastatic colorectal cancer, in combination with intravenous fluorouracil-based chemotherapy for first- or second-line treatment. (1.1)
- •
- Metastatic colorectal cancer, in combination with fluoropyrimidine-irinotecan- or fluoropyrimidine-oxaliplatin-based chemotherapy for second-line treatment in patients who have progressed on a first-line bevacizumab product-containing regimen. (1.1)
Limitations of Use: ZIRABEV is not indicated for adjuvant treatment of colon cancer. (1.1)
- •
- Unresectable, locally advanced, recurrent or metastatic non-squamous non-small cell lung cancer, in combination with carboplatin and paclitaxel for first-line treatment. (1.2)
- •
- Recurrent glioblastoma in adults. (1.3)
- •
- Metastatic renal cell carcinoma in combination with interferon alfa. (1.4)
- •
- Persistent, recurrent, or metastatic cervical cancer, in combination with paclitaxel and cisplatin or paclitaxel and topotecan. (1.5)
- •
- Epithelial ovarian, fallopian tube, or primary peritoneal cancer:
- o
- in combination with carboplatin and paclitaxel, followed by ZIRABEV as a single agent, for stage III or IV disease following initial surgical resection. (1.6)
- o
- in combination with paclitaxel, pegylated liposomal doxorubicin, or topotecan for platinum-resistant recurrent disease who received no more than 2 prior chemotherapy regimens. (1.6)
- o
- in combination with carboplatin and paclitaxel or carboplatin and gemcitabine, followed by ZIRABEV as a single agent, for platinum-sensitive recurrent disease. (1.6)
Zirabev Dosage and Administration
Withhold for at least 28 days prior to elective surgery. Do not administer ZIRABEV for 28 days following major surgery and until adequate wound healing. (2.1)
Metastatic colorectal cancer. (2.2)
- •
- 5 mg/kg every 2 weeks with bolus-IFL.
- •
- 10 mg/kg every 2 weeks with FOLFOX4.
- •
- 5 mg/ kg every 2 weeks or 7.5 mg/kg every 3 weeks with fluoropyrimidine-irinotecan- or fluoropyrimidine-oxaliplatin based chemotherapy after progression on a first-line bevacizumab product containing regimen.
First-line non−squamous non−small cell lung cancer. (2.3)
- •
- 15 mg/kg every 3 weeks with carboplatin and paclitaxel.
Recurrent glioblastoma. (2.4)
- •
- 10 mg/kg every 2 weeks.
Metastatic renal cell carcinoma. (2.5)
- •
- 10 mg/kg every 2 weeks with interferon alfa.
Persistent, recurrent, or metastatic cervical cancer. (2.6)
- •
- 15 mg/kg every 3 weeks with paclitaxel and cisplatin or paclitaxel and topotecan.
Stage III or IV epithelial ovarian, fallopian tube or primary peritoneal cancer following initial surgical resection. (2.7)
- •
- 15 mg/kg every 3 weeks with carboplatin and paclitaxel for up to 6 cycles, followed by 15 mg/kg every 3 weeks as a single agent, for a total of up to 22 cycles.
Platinum-resistant recurrent epithelial ovarian, fallopian tube or primary peritoneal cancer. (2.7)
- •
- 10 mg/kg every 2 weeks with paclitaxel, pegylated liposomal doxorubicin, or topotecan given every week.
- •
- 15 mg/kg every 3 weeks with topotecan given every 3 weeks
Platinum-sensitive recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer. (2.7)
- •
- 15 mg/kg every 3 weeks with carboplatin and paclitaxel for 6–8 cycles, followed by 15 mg/kg every 3 weeks as a single agent.
- •
- 15 mg/kg every 3 weeks with carboplatin and gemcitabine for 6–10 cycles, followed by 15 mg/kg every 3 weeks as a single agent.
Administer as an intravenous infusion after dilution. See full Prescribing Information for preparation and administration instructions and dosage modifications for adverse reactions. (2.8, 2.9)
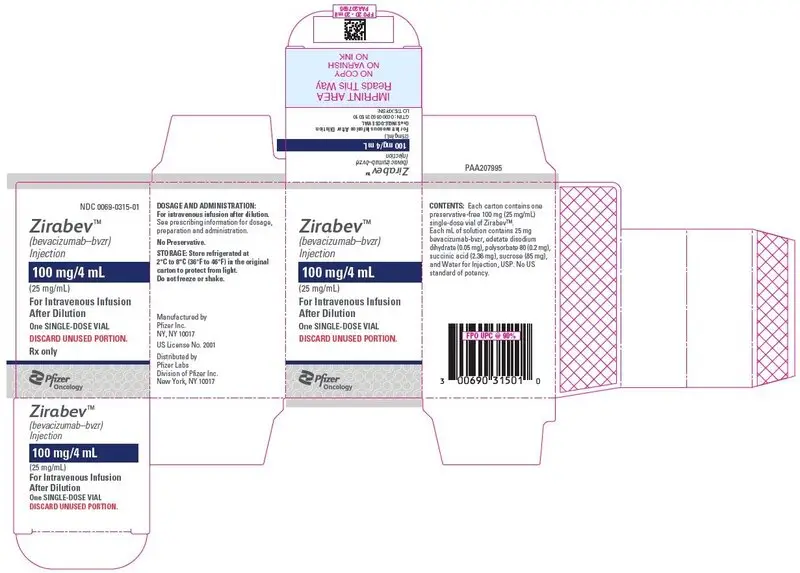
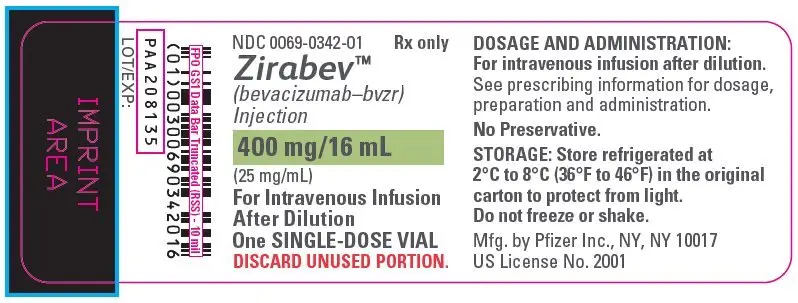
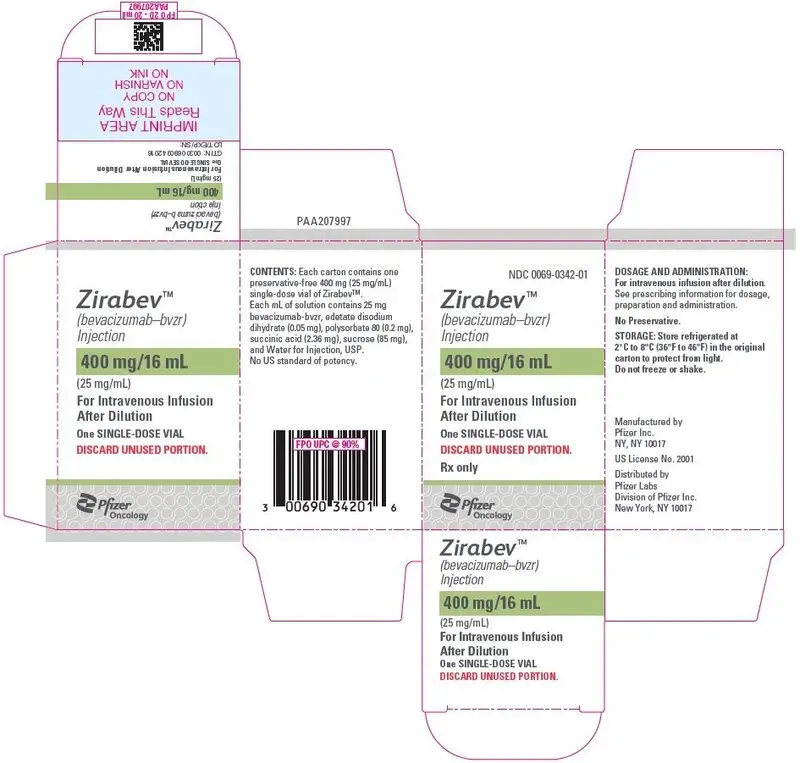
Dosage Forms and Strengths
Injection: 100 mg/4 mL (25 mg/mL) or 400 mg/16 mL (25 mg/mL) in a single-dose vial. (3)
Contraindications
None (4)
Warnings and Precautions
- •
- Gastrointestinal Perforations and Fistula: Discontinue for gastrointestinal perforations, tracheoesophageal fistula, grade 4 fistula, or fistula formation involving any organ. (5.1)
- •
- Surgery and Wound Healing Complications: In patients who experience wound healing complications during ZIRABEV treatment, withhold ZIRABEV until adequate wound healing. Withhold for at least 28 days prior to elective surgery. Do not administer ZIRABEV for at least 28 days following a major surgery, and until adequate wound healing. The safety of resumption of bevacizumab products after resolution of wound healing complication has not been established. Discontinue for wound healing complications of necrotizing fasciitis. (5.2)
- •
- Hemorrhage: Severe or fatal hemorrhages have occurred. Do not administer for recent hemoptysis. Discontinue for Grade 3–4 hemorrhage. (5.3)
- •
- Arterial Thromboembolic Events (ATE): Discontinue for severe ATE. (5.4)
- •
- Venous Thromboembolic Events (VTE): Discontinue for Grade 4 VTE. (5.5)
- •
- Hypertension: Monitor blood pressure and treat hypertension. Withhold if not medically controlled; resume once controlled. Discontinue for hypertensive crisis or hypertensive encephalopathy. (5.6)
- •
- Posterior Reversible Encephalopathy Syndrome (PRES): Discontinue. (5.7)
- •
- Renal Injury and Proteinuria: Monitor urine protein. Discontinue for nephrotic syndrome. Withhold until less than 2 grams of protein in urine. (5.8)
- •
- Infusion–Related Reactions: Decrease rate for infusion-related reactions. Discontinue for severe infusion-related reactions and administer medical therapy. (5.9)
- •
- Embryo-Fetal Toxicity: May cause fetal harm. Advise females of potential risk to fetus and need for use of effective contraception. (5.10, 8.1, 8.3)
- •
- Ovarian Failure: Advise females of the potential risk. (5.11, 8.3)
- •
- Congestive Heart Failure (CHF): Discontinue ZIRABEV in patients who develop CHF. (5.12)
Adverse Reactions/Side Effects
Most common adverse reactions incidence (incidence >10%) are epistaxis, headache, hypertension, rhinitis, proteinuria, taste alteration, dry skin, hemorrhage, lacrimation disorder, back pain and exfoliative dermatitis. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Pfizer Inc. at 1-800-438-1985 and https://www.pfizer.com or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Use In Specific Populations
Lactation: Advise not to breastfeed. (8.2)
See 17 for PATIENT COUNSELING INFORMATION.
- *
- Biosimilar means that the biological product is approved based on data demonstrating that it is highly similar to an FDA-approved biological product, known as a reference product, and that there are no clinically meaningful differences between the biosimilar product and the reference product. Biosimilarity of ZIRABEV has been demonstrated for the condition(s) of use (e.g. indication(s), dosing regimen(s)), strength(s), dosage form(s), and route(s) of administration described in its Full Prescribing Information.
Revised: 2/2023
Full Prescribing Information
1. Indications and Usage for Zirabev
1.1 Metastatic Colorectal Cancer
ZIRABEV, in combination with intravenous fluorouracil-based chemotherapy, is indicated for the first- or second-line treatment of patients with metastatic colorectal cancer (mCRC).
ZIRABEV, in combination with fluoropyrimidine-irinotecan- or fluoropyrimidine-oxaliplatin-based chemotherapy, is indicated for the second-line treatment of patients with mCRC who have progressed on a first-line bevacizumab product-containing regimen.
1.2 First-Line Non-Squamous Non-Small Cell Lung Cancer
ZIRABEV, in combination with carboplatin and paclitaxel, is indicated for the first-line treatment of patients with unresectable, locally advanced, recurrent or metastatic non–squamous non–small cell lung cancer (NSCLC).
1.3 Recurrent Glioblastoma
ZIRABEV is indicated for the treatment of recurrent glioblastoma (GBM) in adults.
1.4 Metastatic Renal Cell Carcinoma
ZIRABEV, in combination with interferon alfa, is indicated for the treatment of metastatic renal cell carcinoma (mRCC).
1.5 Persistent, Recurrent, or Metastatic Cervical Cancer
ZIRABEV, in combination with paclitaxel and cisplatin or paclitaxel and topotecan, is indicated for the treatment of patients with persistent, recurrent, or metastatic cervical cancer.
1.6 Epithelial Ovarian, Fallopian Tube, or Primary Peritoneal Cancer
ZIRABEV, in combination with carboplatin and paclitaxel, followed by ZIRABEV as a single agent, is indicated for the treatment of patients with stage III or IV epithelial ovarian, fallopian tube, or primary peritoneal cancer following initial surgical resection.
ZIRABEV, in combination with paclitaxel, pegylated liposomal doxorubicin, or topotecan, is indicated for the treatment of patients with platinum-resistant recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who received no more than 2 prior chemotherapy regimens.
ZIRABEV, in combination with carboplatin and paclitaxel, or with carboplatin and gemcitabine, followed by ZIRABEV as a single agent, is indicated for the treatment of patients with platinum-sensitive recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer.
2. Zirabev Dosage and Administration
2.1 Important Administration Information
Withhold for at least 28 days prior to elective surgery. Do not administer ZIRABEV until at least 28 days following major surgery and until adequate wound healing.
2.2 Metastatic Colorectal Cancer
The recommended dosage when ZIRABEV is administered in combination with intravenous fluorouracil-based chemotherapy is:
- •
- 5 mg/kg intravenously every 2 weeks in combination with bolus-IFL.
- •
- 10 mg/kg intravenously every 2 weeks in combination with FOLFOX4.
- •
- 5 mg/kg intravenously every 2 weeks or 7.5 mg/kg intravenously every 3 weeks in combination with fluoropyrimidine-irinotecan- or fluoropyrimidine-oxaliplatin-based chemotherapy in patients who have progressed on a first-line bevacizumab product-containing regimen.
2.3 First-Line Non-Squamous Non-Small Cell Lung Cancer
The recommended dosage is 15 mg/kg intravenously every 3 weeks in combination with carboplatin and paclitaxel.
2.5 Metastatic Renal Cell Carcinoma
The recommended dosage is 10 mg/kg intravenously every 2 weeks in combination with interferon alfa.
2.6 Persistent, Recurrent, or Metastatic Cervical Cancer
The recommended dosage is 15 mg/kg intravenously every 3 weeks in combination with paclitaxel and cisplatin or in combination with paclitaxel and topotecan.
2.7 Epithelial Ovarian, Fallopian Tube, or Primary Peritoneal Cancer
Stage III or IV Disease Following Initial Surgical Resection
The recommended dosage is 15 mg/kg intravenously every 3 weeks in combination with carboplatin and paclitaxel for up to 6 cycles, followed by ZIRABEV 15 mg/kg every 3 weeks as a single agent for a total of up to 22 cycles or until disease progression, whichever occurs earlier.
Recurrent Disease
Platinum Resistant
The recommended dosage is 10 mg/kg intravenously every 2 weeks in combination with paclitaxel, pegylated liposomal doxorubicin, or topotecan (every week).
The recommended dosage is 15 mg/kg intravenously every 3 weeks in combination with topotecan (every 3 weeks).
Platinum Sensitive
The recommended dosage is 15 mg/kg intravenously every 3 weeks, in combination with carboplatin and paclitaxel for 6 to 8 cycles, followed by ZIRABEV 15 mg/kg every 3 weeks as a single agent until disease progression.
The recommended dosage is 15 mg/kg intravenously every 3 weeks, in combination with carboplatin and gemcitabine for 6 to 10 cycles, followed by ZIRABEV 15 mg/kg every 3 weeks as a single agent until disease progression.
2.8 Dosage Modifications for Adverse Reactions
Table 1 describes dosage modifications for specific adverse reactions. No dose reductions for ZIRABEV are recommended.
| Adverse Reaction | Severity | Dosage Modification |
|---|---|---|
|
Gastrointestinal Perforations and Fistulae [see Warnings and Precautions (5.1)]. |
|
Discontinue ZIRABEV |
|
Wound Healing Complications [see Warnings and Precautions (5.2)]. |
|
Withhold ZIRABEV until adequate wound healing. The safety of resumption of bevacizumab products after resolution of wound healing complications has not been established. |
|
Discontinue ZIRABEV |
|
|
Hemorrhage [see Warnings and Precautions (5.3)]. |
|
Discontinue ZIRABEV |
|
Withhold ZIRABEV |
|
|
Thromboembolic Events [see Warnings and Precautions (5.4, 5.5)]. |
|
Discontinue ZIRABEV |
|
Discontinue ZIRABEV |
|
|
Hypertension [see Warnings and Precautions (5.6)]. |
|
Discontinue ZIRABEV |
|
Withhold ZIRABEV if not controlled with medical management; resume once controlled |
|
|
Posterior Reversible Encephalopathy Syndrome (PRES) [see Warnings and Precautions (5.7)]. |
|
Discontinue ZIRABEV |
|
Renal Injury and Proteinuria [see Warnings and Precautions (5.8)]. |
|
Discontinue ZIRABEV |
|
Withhold ZIRABEV until proteinuria less than 2 grams per 24 hours |
|
|
Infusion-Related Reactions [see Warnings and Precautions (5.9)]. |
|
Discontinue ZIRABEV |
|
Interrupt infusion; resume at a decreased rate of infusion after symptoms resolve |
|
|
Decrease infusion rate |
|
|
Congestive Heart Failure [see Warnings and Precautions (5.12)]. |
|
Discontinue ZIRABEV |
2.9 Preparation and Administration
Preparation
- •
- Use appropriate aseptic technique.
- •
- Use sterile needle and syringe to prepare ZIRABEV.
- •
- Visually inspect vial for particulate matter and discoloration prior to preparation for administration. Discard vial if solution is cloudy, discolored, or contains particulate matter.
- •
- Withdraw necessary amount of ZIRABEV and dilute in a total volume of 100 mL of 0.9% Sodium Chloride Injection, USP. DO NOT ADMINISTER OR MIX WITH DEXTROSE SOLUTION.
- •
- Discard any unused portion left in a vial, as the product contains no preservatives.
- •
- Diluted ZIRABEV solution may be stored at 2°C to 8°C (36°F to 46°F) for up to 8 hours, if not used immediately.
- •
- No incompatibilities between ZIRABEV and polyvinylchloride or polyolefin bags have been observed.
Administration
- •
- Administer as an intravenous infusion.
- •
- First infusion: Administer infusion over 90 minutes.
- •
- Subsequent infusions: Administer second infusion over 60 minutes if first infusion is tolerated. Administer all subsequent infusions over 30 minutes if second infusion over 60 minutes is tolerated.
3. Dosage Forms and Strengths
Injection: 100 mg/4 mL (25 mg/mL) or 400 mg/16 mL (25 mg/mL) clear to slightly opalescent, colorless to pale brown solution in a single-dose vial
5. Warnings and Precautions
5.1 Gastrointestinal Perforations and Fistulae
Serious and sometimes fatal gastrointestinal perforation occurred at a higher incidence in patients receiving bevacizumab products compared to patients receiving chemotherapy. The incidence ranged from 0.3% to 3% across clinical studies, with the highest incidence in patients with a history of prior pelvic radiation. Perforation can be complicated by intra-abdominal abscess, fistula formation, and the need for diverting ostomies. The majority of perforations occurred within 50 days of the first dose [see Adverse Reactions (6.1)].
Serious fistulae (including, tracheoesophageal, bronchopleural, biliary, vaginal, renal and bladder sites) occurred at a higher incidence in patients receiving bevacizumab products compared to patients receiving chemotherapy. The incidence ranged from <1% to 1.8% across clinical studies, with the highest incidence in patients with cervical cancer. The majority of fistulae occurred within 6 months of the first dose. Patients who develop a gastrointestinal vaginal fistula may also have a bowel obstruction and require surgical intervention, as well as a diverting ostomy.
Avoid ZIRABEV in patients with ovarian cancer who have evidence of recto-sigmoid involvement by pelvic examination or bowel involvement on CT scan or clinical symptoms of bowel obstruction. Discontinue in patients who develop gastrointestinal perforation, tracheoesophageal fistula or any Grade 4 fistula. Discontinue in patients with fistula formation involving any internal organ.
5.2 Surgery and Wound Healing Complications
In a controlled clinical study in which bevacizumab was not administered within 28 days of major surgical procedures, the incidence of wound healing complications, including serious and fatal complications, was 15% in patients with mCRC who underwent surgery while receiving bevacizumab and 4% in patients who did not receive bevacizumab. In a controlled clinical study in patients with relapsed or recurrent GBM, the incidence of wound healing events was 5% in patients who received bevacizumab and 0.7% in patients who did not receive bevacizumab [see Adverse Reactions (6.1)].
In patients who experience wound healing complications during ZIRABEV treatment, withhold ZIRABEV until adequate wound healing. Withhold for at least 28 days prior to elective surgery. Do not administer for at least 28 days following major surgery and until adequate wound healing. The safety of resumption of bevacizumab products after resolution of wound healing complications has not been established [see Dosage and Administration (2.7)].
Necrotizing fasciitis including fatal cases, has been reported in patients receiving bevacizumab usually secondary to wound healing complications, gastrointestinal perforation or fistula formation. Discontinue ZIRABEV in patients who develop necrotizing fasciitis.
5.3 Hemorrhage
Bevacizumab products can result in two distinct patterns of bleeding: minor hemorrhage, which is most commonly Grade 1 epistaxis, and serious hemorrhage, which in some cases has been fatal. Severe or fatal hemorrhage, including hemoptysis, gastrointestinal bleeding, hematemesis, CNS hemorrhage, epistaxis, and vaginal bleeding occurred up to 5-fold more frequently in patients receiving bevacizumab compared to patients receiving chemotherapy alone. Across clinical studies, the incidence of Grades 3–5 hemorrhagic events ranged from 0.4% to 7% in patients receiving bevacizumab [see Adverse Reactions (6.1)].
Serious or fatal pulmonary hemorrhage occurred in 31% of patients with squamous NSCLC and 4% of patients with non-squamous NSCLC receiving bevacizumab with chemotherapy compared to none of the patients receiving chemotherapy alone.
Do not administer ZIRABEV to patients with recent history of hemoptysis of 1/2 teaspoon or more of red blood. Discontinue in patients who develop a Grades 3–4 hemorrhage.
5.4 Arterial Thromboembolic Events
Serious, sometimes fatal, arterial thromboembolic events (ATE) including cerebral infarction, transient ischemic attacks, myocardial infarction, and angina, occurred at a higher incidence in patients receiving bevacizumab compared to patients receiving chemotherapy. Across clinical studies, the incidence of Grades 3–5 ATE was 5% in patients receiving bevacizumab with chemotherapy compared to ≤2% in patients receiving chemotherapy alone; the highest incidence occurred in patients with GBM. The risk of developing ATE was increased in patients with a history of arterial thromboembolism, diabetes, or ≥65 years [see Use in Specific Populations (8.5)].
Discontinue in patients who develop a severe ATE. The safety of reinitiating bevacizumab products after an ATE is resolved is not known.
5.5 Venous Thromboembolic Events
An increased risk of venous thromboembolic events (VTE) was observed across clinical studies [see Adverse Reactions (6.1)]. In Study GOG-0240, Grades 3–4 VTE occurred in 11% of patients receiving bevacizumab with chemotherapy compared with 5% of patients receiving chemotherapy alone. In EORTC 26101, the incidence of Grades 3–4 VTE was 5% in patients receiving bevacizumab with chemotherapy compared to 2% in patients receiving chemotherapy alone.
Discontinue ZIRABEV in patients with a Grade 4 VTE, including pulmonary embolism.
5.6 Hypertension
Severe hypertension occurred at a higher incidence in patients receiving bevacizumab products as compared to patients receiving chemotherapy alone. Across clinical studies, the incidence of Grades 3–4 hypertension ranged from 5% to 18%.
Monitor blood pressure every two to three weeks during treatment with ZIRABEV. Treat with appropriate anti-hypertensive therapy and monitor blood pressure regularly. Continue to monitor blood pressure at regular intervals in patients with ZIRABEV-induced or -exacerbated hypertension after discontinuing ZIRABEV. Withhold ZIRABEV in patients with severe hypertension that is not controlled with medical management; resume once controlled with medical management. Discontinue in patients who develop hypertensive crisis or hypertensive encephalopathy.
5.7 Posterior Reversible Encephalopathy Syndrome
Posterior reversible encephalopathy syndrome (PRES) was reported in <0.5% of patients across clinical studies. The onset of symptoms occurred from 16 hours to 1 year after the first dose. PRES is a neurological disorder which can present with headache, seizure, lethargy, confusion, blindness and other visual and neurologic disturbances. Mild to severe hypertension may be present. Magnetic resonance imaging is necessary to confirm the diagnosis of PRES.
Discontinue ZIRABEV in patients who develop PRES. Symptoms usually resolve or improve within days after discontinuing bevacizumab products, although some patients have experienced ongoing neurologic sequelae. The safety of reinitiating bevacizumab products in patients who developed PRES is not known.
5.8 Renal Injury and Proteinuria
The incidence and severity of proteinuria was higher in patients receiving bevacizumab as compared to patients receiving chemotherapy. Grade 3 (defined as urine dipstick 4+ or >3.5 grams of protein per 24 hours) to Grade 4 (defined as nephrotic syndrome) ranged from 0.7% to 7% in clinical studies.
The overall incidence of proteinuria (all grades) was only adequately assessed in Study BO17705, in which the incidence was 20%. Median onset of proteinuria was 5.6 months (15 days to 37 months) after initiating bevacizumab. Median time to resolution was 6.1 months (95% CI: 2.8, 11.3). Proteinuria did not resolve in 40% of patients after median follow-up of 11.2 months and required discontinuation of bevacizumab in 30% of the patients who developed proteinuria [see Adverse Reactions (6.1)].
In an exploratory, pooled analysis of patients from seven randomized clinical studies, 5% of patients receiving bevacizumab with chemotherapy experienced Grades 2–4 (defined as urine dipstick 2+ or greater or >1 gram of protein per 24 hours or nephrotic syndrome) proteinuria. Grades 2–4 proteinuria resolved in 74% of patients.
Bevacizumab was reinitiated in 42% of patients. Of the 113 patients who reinitiated bevacizumab, 48% experienced a second episode of Grades 2–4 proteinuria.
Nephrotic syndrome occurred in <1% of patients receiving bevacizumab across clinical studies, in some instances with fatal outcome. In a published case series, kidney biopsy of 6 patients with proteinuria showed findings consistent with thrombotic microangiopathy. Results of a retrospective analysis of 5805 patients who received bevacizumab with chemotherapy and 3713 patients who received chemotherapy alone, showed higher rates of elevated serum creatinine levels (between 1.5 to 1.9 times baseline levels) in patients who received bevacizumab. Serum creatinine levels did not return to baseline in approximately one-third of patients who received bevacizumab.
Monitor proteinuria by dipstick urine analysis for the development or worsening of proteinuria with serial urinalyses during ZIRABEV therapy. Patients with a 2+ or greater urine dipstick reading should undergo further assessment with a 24-hour urine collection. Withhold for proteinuria greater than or equal to 2 grams per 24 hours and resume when less than 2 grams per 24 hours. Discontinue in patients who develop nephrotic syndrome.
Data from a postmarketing safety study showed poor correlation between UPCR (Urine Protein/Creatinine Ratio) and 24-hour urine protein [Pearson Correlation 0.39 (95% CI: 0.17, 0.57)].
5.9 Infusion-Related Reactions
Infusion-related reactions reported across clinical studies and postmarketing experience include hypertension, hypertensive crises associated with neurologic signs and symptoms, wheezing, oxygen desaturation, Grade 3 hypersensitivity, anaphylactoid/anaphylactic reactions, chest pain, headaches, rigors, and diaphoresis. In clinical studies, infusion-related reactions with the first dose occurred in <3% of patients and severe reactions occurred in 0.4% of patients.
Decrease the rate of infusion for mild, clinically insignificant infusion-related reactions. Interrupt the infusion in patients with clinically significant infusion-related reactions and consider resuming at a slower rate following resolution. Discontinue in patients who develop a severe infusion-related reaction and administer appropriate medical therapy (e.g., epinephrine, corticosteroids, intravenous antihistamines, bronchodilators and/or oxygen).
5.10 Embryo-Fetal Toxicity
Based on its mechanism of action and findings from animal studies, bevacizumab products may cause fetal harm when administered to pregnant women. Congenital malformations were observed with the administration of bevacizumab to pregnant rabbits during organogenesis every 3 days at a dose as low as a clinical dose of 10 mg/kg.
Furthermore, animal models link angiogenesis and VEGF and VEGFR2 to critical aspects of female reproduction, embryo-fetal development, and postnatal development. Advise pregnant women of the potential risk to a fetus. Advise females of reproductive potential to use effective contraception during treatment with ZIRABEV and for 6 months after the last dose [see Use in Specific Populations (8.1, 8.3)].
5.11 Ovarian Failure
The incidence of ovarian failure was 34% vs. 2% in premenopausal women receiving bevacizumab with chemotherapy as compared to those receiving chemotherapy alone for adjuvant treatment of a solid tumor. After discontinuing bevacizumab, recovery of ovarian function at all time points during the post-treatment period was demonstrated in 22% of women receiving bevacizumab. Recovery of ovarian function is defined as resumption of menses, a positive serum β-HCG pregnancy test, or an FSH level <30 mIU/mL during the post-treatment period. Long-term effects of bevacizumab products on fertility are unknown. Inform females of reproductive potential of the risk of ovarian failure prior to initiating ZIRABEV [see Adverse Reactions (6.1), Use in Specific Populations (8.3)].
5.12 Congestive Heart Failure (CHF)
ZIRABEV is not indicated for use with anthracycline-based chemotherapy. The incidence of Grade ≥3 left ventricular dysfunction was 1% in patients receiving bevacizumab compared to 0.6% of patients receiving chemotherapy alone. Among patients who received prior anthracycline treatment, the rate of CHF was 4% for patients receiving bevacizumab with chemotherapy as compared to 0.6% for patients receiving chemotherapy alone.
In previously untreated patients with a hematological malignancy, the incidence of CHF and decline in left ventricular ejection fraction (LVEF) were increased in patients receiving bevacizumab with anthracycline-based chemotherapy compared to patients receiving placebo with the same chemotherapy regimen. The proportion of patients with a decline in LVEF from baseline of ≥20% or a decline from baseline of 10% to <50%, was 10% in patients receiving bevacizumab with chemotherapy compared to 5% in patients receiving chemotherapy alone. Time to onset of left-ventricular dysfunction or CHF was 1 to 6 months after the first dose in at least 85% of the patients and was resolved in 62% of the patients who developed CHF in the bevacizumab arm compared to 82% in the placebo arm. Discontinue ZIRABEV in patients who develop CHF.
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are described elsewhere in the labeling:
- •
- Gastrointestinal Perforations and Fistulae [see Warnings and Precautions (5.1)].
- •
- Surgery and Wound Healing Complications [see Warnings and Precautions (5.2)].
- •
- Hemorrhage [see Warnings and Precautions (5.3)].
- •
- Arterial Thromboembolic Events [see Warnings and Precautions (5.4)].
- •
- Venous Thromboembolic Events [see Warnings and Precautions (5.5)].
- •
- Hypertension [see Warnings and Precautions (5.6)].
- •
- Posterior Reversible Encephalopathy Syndrome [see Warnings and Precautions (5.7)].
- •
- Renal Injury and Proteinuria [see Warnings and Precautions (5.8)].
- •
- Infusion-Related Reactions [see Warnings and Precautions (5.9)].
- •
- Ovarian Failure [see Warnings and Precautions (5.11)].
- •
- Congestive Heart Failure [see Warnings and Precautions (5.12)].
6.1 Clinical Trials Experience
Because clinical studies are conducted under widely varying conditions, adverse reaction rates observed in the clinical studies of a drug cannot be directly compared to rates in the clinical studies of another drug and may not reflect the rates observed in practice.
The safety data in Warnings and Precautions and described below reflect exposure to bevacizumab in 4463 patients including those with mCRC (AVF2107g, E3200), non-squamous NSCLC (E4599), GBM (EORTC 26101), mRCC (BO17705), cervical cancer (GOG-0240), epithelial ovarian, fallopian tube, or primary peritoneal cancer (MO22224, AVF4095, GOG-0213, and GOG-0218) or another cancer at the recommended dose and schedule for a median of 6 to 23 doses. The most common adverse reactions observed in patients receiving bevacizumab as a single agent or in combination with other anti-cancer therapies at a rate >10% were epistaxis, headache, hypertension, rhinitis, proteinuria, taste alteration, dry skin, hemorrhage, lacrimation disorder, back pain, and exfoliative dermatitis.
Across clinical studies, bevacizumab was discontinued in 8% to 22% of patients because of adverse reactions [see Clinical Studies (14)].
Metastatic Colorectal Cancer
In Combination with bolus IFL
The safety of bevacizumab was evaluated in 392 patients who received at least one dose of bevacizumab in a double-blind, active-controlled study (AVF2107g), which compared bevacizumab (5 mg/kg every 2 weeks) with bolus-IFL to placebo with bolus IFL in patients with mCRC [see Clinical Studies (14.1)]. Patients were randomized (1:1:1) to placebo with bolus IFL, bevacizumab with bolus IFL, or bevacizumab with fluorouracil and leucovorin. The demographics of the safety population were similar to the demographics of the efficacy population. All Grades 3–4 adverse reactions and selected Grades 1–2 adverse reactions (i.e., hypertension, proteinuria, thromboembolic events) were collected in the entire study population. Adverse reactions are presented in Table 2.
| Adverse Reaction* | Bevacizumab with IFL
(N=392) | Placebo with IFL
(N=396) |
|---|---|---|
|
||
|
Hematology |
||
|
Leukopenia |
37% |
31% |
|
Neutropenia |
21% |
14% |
|
Gastrointestinal |
||
|
Diarrhea |
34% |
25% |
|
Abdominal pain |
8% |
5% |
|
Constipation |
4% |
2% |
|
Vascular |
||
|
Hypertension |
12% |
2% |
|
Deep vein thrombosis |
9% |
5% |
|
Intra-abdominal thrombosis |
3% |
1% |
|
Syncope |
3% |
1% |
|
General |
||
|
Asthenia |
10% |
7% |
|
Pain |
8% |
5% |
In Combination with FOLFOX4
The safety of bevacizumab was evaluated in 521 patients in an open-label, active-controlled study (E3200) in patients who were previously treated with irinotecan and fluorouracil for initial therapy for mCRC. Patients were randomized (1:1:1) to FOLFOX4, bevacizumab (10 mg/kg every 2 weeks prior to FOLFOX4 on Day 1) with FOLFOX4, or bevacizumab alone (10 mg/kg every 2 weeks). Bevacizumab was continued until disease progression or unacceptable toxicity. The demographics of the safety population were similar to the demographics of the efficacy population.
Selected Grades 3–5 non-hematologic and Grades 4–5 hematologic occurring at a higher incidence (≥2%) in patients receiving bevacizumab with FOLFOX4 compared to FOLFOX4 alone were fatigue (19% vs. 13%), diarrhea (18% vs. 13%), sensory neuropathy (17% vs. 9%), nausea (12% vs. 5%), vomiting (11% vs. 4%), dehydration (10% vs. 5%), hypertension (9% vs. 2%), abdominal pain (8% vs. 5%), hemorrhage (5% vs. 1%), other neurological (5% vs. 3%), ileus (4% vs. 1%) and headache (3% vs. 0%). These data are likely to under-estimate the true adverse reaction rates due to the reporting mechanisms.
First-Line Non-Squamous Non-Small Cell Lung Cancer
The safety of bevacizumab was evaluated as first-line treatment in 422 patients with unresectable NSCLC who received at least one dose of bevacizumab in an active-controlled, open-label, multicenter trial (E4599) [see Clinical Studies (14.3)]. Chemotherapy-naïve patients with locally advanced, metastatic or recurrent non–squamous NSCLC were randomized (1:1) to receive six 21-day cycles of paclitaxel and carboplatin with or without bevacizumab (15 mg/kg every 3 weeks). After completion or upon discontinuation of chemotherapy, patients randomized to receive bevacizumab continued to receive bevacizumab alone until disease progression or until unacceptable toxicity. The trial excluded patients with predominant squamous histology (mixed cell type tumors only), CNS metastasis, gross hemoptysis (1/2 teaspoon or more of red blood), unstable angina, or receiving therapeutic anticoagulation. The demographics of the safety population were similar to the demographics of the efficacy population.
Only Grades 3–5 non-hematologic and Grades 4–5 hematologic adverse reactions were collected. Grades 3–5 non-hematologic and Grades 4–5 hematologic adverse reactions occurring at a higher incidence (≥2%) in patients receiving bevacizumab with paclitaxel and carboplatin compared with patients receiving chemotherapy alone were neutropenia (27% vs. 17%), fatigue (16% vs. 13%), hypertension (8% vs. 0.7%), infection without neutropenia (7% vs. 3%), venous thromboembolism (5% vs. 3%), febrile neutropenia (5% vs. 2%), pneumonitis/pulmonary infiltrates (5% vs. 3%), infection with Grade 3 or 4 neutropenia (4% vs. 2%), hyponatremia (4% vs. 1%), headache (3% vs. 1%) and proteinuria (3% vs. 0%).
Recurrent Glioblastoma
The safety of bevacizumab was evaluated in a multicenter, randomized, open-label study (EORTC 26101) in patients with recurrent GBM following radiotherapy and temozolomide of whom 278 patients received at least one dose of bevacizumab and are considered safety evaluable [see Clinical Studies (14.4)]. Patients were randomized (2:1) to receive bevacizumab (10 mg/kg every 2 weeks) with lomustine or lomustine alone until disease progression or unacceptable toxicity. The demographics of the safety population were similar to the demographics of the efficacy population. In the bevacizumab with lomustine arm, 22% of patients discontinued treatment due to adverse reactions compared with 10% of patients in the lomustine arm. In patients receiving bevacizumab with lomustine, the adverse reaction profile was similar to that observed in other approved indications.
Metastatic Renal Cell Carcinoma
The safety of bevacizumab was evaluated in 337 patients who received at least one dose of bevacizumab in a multicenter, double-blind study (BO17705) in patients with mRCC. Patients who had undergone a nephrectomy were randomized (1:1) to receive either bevacizumab (10 mg/kg every 2 weeks) or placebo with interferon alfa [see Clinical Studies (14.5)]. Patients were treated until disease progression or unacceptable toxicity. The demographics of the safety population were similar to the demographics of the efficacy population.
Grades 3–5 adverse reactions occurring at a higher incidence (>2%) were fatigue (13% vs. 8%), asthenia (10% vs. 7%), proteinuria (7% vs. 0%), hypertension (6% vs. 1%; including hypertension and hypertensive crisis), and hemorrhage (3% vs. 0.3%; including epistaxis, small intestinal hemorrhage, aneurysm ruptured, gastric ulcer hemorrhage, gingival bleeding, hemoptysis, hemorrhage intracranial, large intestinal hemorrhage, respiratory tract hemorrhage, and traumatic hematoma). Adverse reactions are presented in Table 3.
| Adverse Reaction* | Bevacizumab with Interferon Alfa
(N=337) | Placebo with Interferon Alfa
(N=304) |
|---|---|---|
|
||
|
Metabolism and nutrition |
||
|
Decreased appetite |
36% |
31% |
|
Weight loss |
20% |
15% |
|
General |
||
|
Fatigue |
33% |
27% |
|
Vascular |
||
|
Hypertension |
28% |
9% |
|
Respiratory, thoracic and mediastinal |
||
|
Epistaxis |
27% |
4% |
|
Dysphonia |
5% |
0% |
|
Nervous system |
||
|
Headache |
24% |
16% |
|
Gastrointestinal |
||
|
Diarrhea |
21% |
16% |
|
Renal and urinary |
||
|
Proteinuria |
20% |
3% |
|
Musculoskeletal and connective tissue |
||
|
Myalgia |
19% |
14% |
|
Back pain |
12% |
6% |
The following adverse reactions were reported at a 5-fold greater incidence in patients receiving bevacizumab with interferon-alfa compared to patients receiving placebo with interferon-alfa and not represented in Table 3: gingival bleeding (13 patients vs. 1 patient); rhinitis (9 vs. 0); blurred vision (8 vs. 0); gingivitis (8 vs. 1); gastroesophageal reflux disease (8 vs. 1); tinnitus (7 vs. 1); tooth abscess (7 vs. 0); mouth ulceration (6 vs. 0); acne (5 vs. 0); deafness (5 vs. 0); gastritis (5 vs. 0); gingival pain (5 vs. 0) and pulmonary embolism (5 vs. 1).
Persistent, Recurrent, or Metastatic Cervical Cancer
The safety of bevacizumab was evaluated in 218 patients who received at least one dose of bevacizumab in a multicenter study (GOG-0240) in patients with persistent, recurrent, or metastatic cervical cancer [see Clinical Studies (14.6)]. Patients were randomized (1:1:1:1) to receive paclitaxel and cisplatin with or without bevacizumab (15 mg/kg every 3 weeks), or paclitaxel and topotecan with or without bevacizumab (15 mg/kg every 3 weeks). The demographics of the safety population were similar to the demographics of the efficacy population.
Grades 3–4 adverse reactions occurring at a higher incidence (≥2%) in 218 patients receiving bevacizumab with chemotherapy compared to 222 patients receiving chemotherapy alone were abdominal pain (12% vs. 10%), hypertension (11% vs. 0.5%), thrombosis (8% vs. 3%), diarrhea (6% vs. 3%), anal fistula (4% vs. 0%), proctalgia (3% vs. 0%), urinary tract infection (8% vs. 6%), cellulitis (3% vs. 0.5%), fatigue (14% vs. 10%), hypokalemia (7% vs. 4%), hyponatremia (4% vs. 1%), dehydration (4% vs. 0.5%), neutropenia (8% vs. 4%), lymphopenia (6% vs. 3%), back pain (6% vs. 3%), and pelvic pain (6% vs. 1%). Adverse reactions are presented in Table 4.
| Adverse Reaction* | Bevacizumab with Chemotherapy
(N=218) | Chemotherapy
(N=222) |
|---|---|---|
|
||
|
General |
||
|
Fatigue |
80% |
75% |
|
Peripheral edema |
15% |
22% |
|
Metabolism and nutrition |
||
|
Decreased appetite |
34% |
26% |
|
Hyperglycemia |
26% |
19% |
|
Hypomagnesemia |
24% |
15% |
|
Weight loss |
21% |
7% |
|
Hyponatremia |
19% |
10% |
|
Hypoalbuminemia |
16% |
11% |
|
Vascular |
||
|
Hypertension |
29% |
6% |
|
Thrombosis |
10% |
3% |
|
Infections |
||
|
Urinary tract infection |
22% |
14% |
|
Infection |
10% |
5% |
|
Nervous system |
||
|
Headache |
22% |
13% |
|
Dysarthria |
8% |
1% |
|
Psychiatric |
||
|
Anxiety |
17% |
10% |
|
Respiratory, thoracic and mediastinal |
||
|
Epistaxis |
17% |
1% |
|
Renal and urinary |
||
|
Increased blood creatinine |
16% |
10% |
|
Proteinuria |
10% |
3% |
|
Gastrointestinal |
||
|
Stomatitis |
15% |
10% |
|
Proctalgia |
6% |
1% |
|
Anal fistula |
6% |
0% |
|
Reproductive system and breast |
||
|
Pelvic pain |
14% |
8% |
|
Hematology |
||
|
Neutropenia |
12% |
6% |
|
Lymphopenia |
12% |
5% |
Epithelial Ovarian, Fallopian Tube, or Primary Peritoneal Cancer
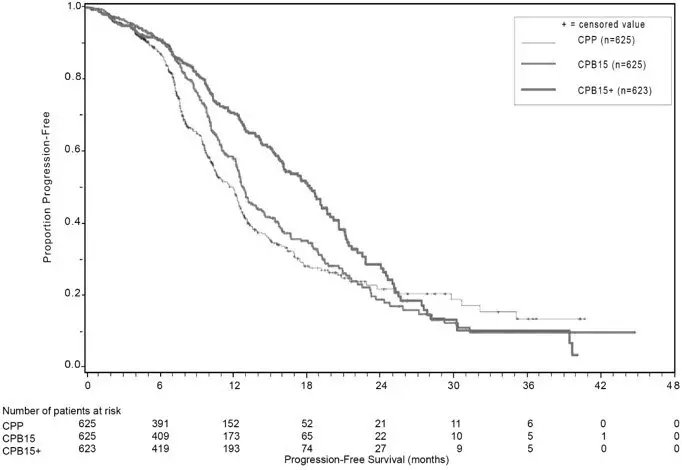
Stage III or IV Following Initial Surgical Resection
The safety of bevacizumab was evaluated in GOG-0218, a multicenter, randomized, double-blind, placebo-controlled, three arm study, which evaluated the addition of bevacizumab to carboplatin and paclitaxel for the treatment of patients with stage III or IV epithelial ovarian, fallopian tube, or primary peritoneal cancer following initial surgical resection [see Clinical Studies (14.7)]. Patients were randomized (1:1:1) to carboplatin and paclitaxel without bevacizumab (CPP), carboplatin and paclitaxel with bevacizumab for up to six cycles (CPB15), or carboplatin and paclitaxel with bevacizumab for six cycles followed by bevacizumab as a single agent for up to 16 additional doses (CPB15+). Bevacizumab was given at 15 mg/kg every three weeks. On this trial, 1215 patients received at least one dose of bevacizumab. The demographics of the safety population were similar to the demographics of the efficacy population.
Grades 3–4 adverse reactions occurring at a higher incidence (≥2%) in either of the bevacizumab arms versus the control arm were fatigue (CPB15+ - 9%, CPB15 - 6%, CPP - 6%), hypertension (CPB15+ - 10%, CPB15 - 6%, CPP - 2%), thrombocytopenia (CPB15+ - 21%, CPB15 - 20%, CPP - 15%) and leukopenia (CPB15+ - 51%, CPB15 - 53%, CPP - 50%). Adverse reactions are presented in Table 5.
| Adverse Reaction* | Bevacizumab with Carboplatin and Paclitaxel followed by Bevacizumab Alone†
(N=608) | Bevacizumab with Carboplatin and Paclitaxel‡
(N=607) | Carboplatin and Paclitaxel§
(N=602) |
|---|---|---|---|
|
|||
|
General |
|||
|
Fatigue |
80% |
72% |
73% |
|
Gastrointestinal |
|||
|
Nausea |
58% |
53% |
51% |
|
Diarrhea |
38% |
40% |
34% |
|
Stomatitis |
25% |
19% |
14% |
|
Musculoskeletal and connective tissue |
|||
|
Arthralgia |
41% |
33% |
35% |
|
Pain in extremity |
25% |
19% |
17% |
|
Muscular weakness |
15% |
13% |
9% |
|
Nervous system |
|||
|
Headache |
34% |
26% |
21% |
|
Dysarthria |
12% |
10% |
2% |
|
Vascular |
|||
|
Hypertension |
32% |
24% |
14% |
|
Respiratory, thoracic and mediastinal |
|||
|
Epistaxis |
31% |
30% |
9% |
|
Dyspnea |
26% |
28% |
20% |
|
Nasal mucosal disorder |
10% |
7% |
4% |
Platinum-Resistant Recurrent Epithelial Ovarian, Fallopian Tube, or Primary Peritoneal Cancer
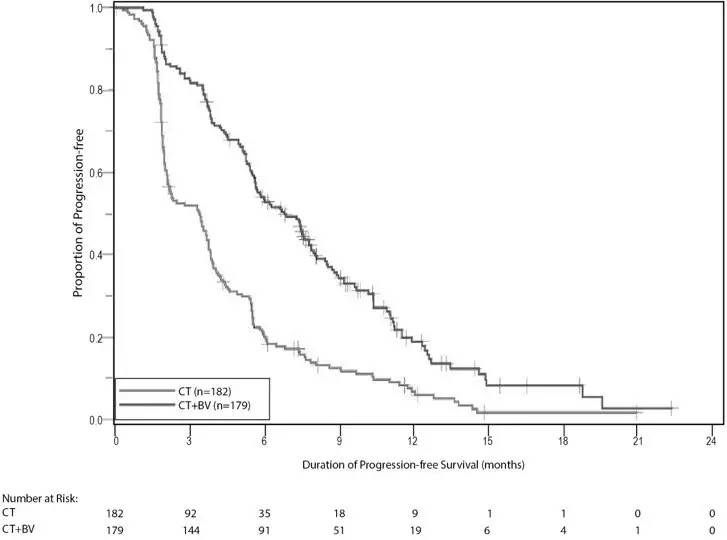
The safety of bevacizumab was evaluated in 179 patients who received at least one dose of bevacizumab in a multicenter, open-label study (MO22224) in which patients were randomized (1:1) to bevacizumab with chemotherapy or chemotherapy alone in patients with platinum-resistant recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer that recurred within <6 months from the most recent platinum based therapy [see Clinical Studies (14.8)]. Patients were randomized to receive bevacizumab 10 mg/kg every 2 weeks or 15 mg/kg every 3 weeks. Patients had received no more than 2 prior chemotherapy regimens. The trial excluded patients with evidence of recto-sigmoid involvement by pelvic examination or bowel involvement on CT scan or clinical symptoms of bowel obstruction. Patients were treated until disease progression or unacceptable toxicity. Forty percent of patients on the chemotherapy alone arm received bevacizumab alone upon progression. The demographics of the safety population were similar to the demographics of the efficacy population.
Grades 3–4 adverse reactions occurring at a higher incidence (≥2%) in 179 patients receiving bevacizumab with chemotherapy compared to 181 patients receiving chemotherapy alone were hypertension (6.7% vs. 1.1%) and palmar-plantar erythrodysaesthesia syndrome (4.5% vs. 1.7%). Adverse reactions are presented in Table 6.
| Adverse Reaction* | Bevacizumab with Chemotherapy
(N=179) | Chemotherapy
(N=181) |
|---|---|---|
|
||
|
Hematology |
||
|
Neutropenia |
31% |
25% |
|
Vascular |
||
|
Hypertension |
19% |
6% |
|
Nervous system |
||
|
Peripheral sensory neuropathy |
18% |
7% |
|
General |
||
|
Mucosal inflammation |
13% |
6% |
|
Renal and urinary |
||
|
Proteinuria |
12% |
0.6% |
|
Skin and subcutaneous tissue |
||
|
Palmar-plantar erythrodysaesthesia |
11% |
5% |
|
Infections |
||
|
Infection |
11% |
4% |
|
Respiratory, thoracic and mediastinal |
||
|
Epistaxis |
5% |
0% |
Platinum-Sensitive Recurrent Epithelial Ovarian, Fallopian Tube, or Primary Peritoneal Cancer
Study AVF4095g
The safety of bevacizumab was evaluated in 247 patients who received at least one dose of bevacizumab in a double-blind study (AVF4095g) in patients with platinum-sensitive recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer [see Clinical Studies (14.9)]. Patients were randomized (1:1) to receive bevacizumab (15 mg/kg) or placebo every 3 weeks with carboplatin and gemcitabine for 6 to 10 cycles followed by bevacizumab or placebo alone until disease progression or unacceptable toxicity. The demographics of the safety population were similar to the demographics of the efficacy population.
Grades 3–4 adverse reactions occurring at a higher incidence (≥2%) in patients receiving bevacizumab with chemotherapy compared to placebo with chemotherapy were: thrombocytopenia (40% vs. 34%), nausea (4% vs. 1.3%), fatigue (6% vs. 4%), headache (4% vs. 0.9%), proteinuria (10% vs. 0.4%), dyspnea (4% vs. 1.7%), epistaxis (5% vs. 0.4%), and hypertension (17% vs. 0.9%). Adverse reactions are presented in Table 7.
| Adverse Reaction* | Bevacizumab with Carboplatin and Gemcitabine
(N=247) | Placebo with Carboplatin and Gemcitabine
(N=233) |
|---|---|---|
|
||
|
General |
||
|
Fatigue |
82% |
75% |
|
Mucosal inflammation |
15% |
10% |
|
Gastrointestinal |
||
|
Nausea |
72% |
66% |
|
Diarrhea |
38% |
29% |
|
Stomatitis |
15% |
7% |
|
Hemorrhoids |
8% |
3% |
|
Gingival bleeding |
7% |
0% |
|
Hematology |
||
|
Thrombocytopenia |
58% |
51% |
|
Respiratory, thoracic and mediastinal |
||
|
Epistaxis |
55% |
14% |
|
Dyspnea |
30% |
24% |
|
Cough |
26% |
18% |
|
Oropharyngeal pain |
16% |
10% |
|
Dysphonia |
13% |
3% |
|
Rhinorrhea |
10% |
4% |
|
Sinus congestion |
8% |
2% |
|
Nervous system |
||
|
Headache |
49% |
30% |
|
Dizziness |
23% |
17% |
|
Vascular |
||
|
Hypertension |
42% |
9% |
|
Musculoskeletal and connective tissue |
||
|
Arthralgia |
28% |
19% |
|
Back pain |
21% |
13% |
|
Psychiatric |
||
|
Insomnia |
21% |
15% |
|
Renal and urinary |
||
|
Proteinuria |
20% |
3% |
|
Injury and procedural |
||
|
Contusion |
17% |
9% |
|
Infections |
||
|
Sinusitis |
15% |
9% |
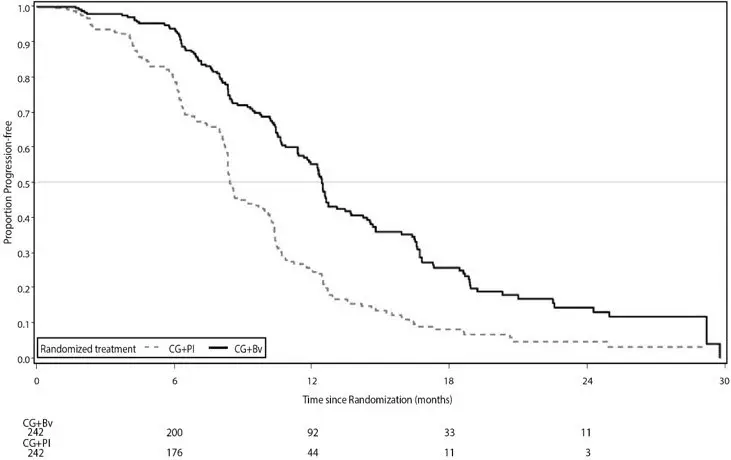
Study GOG-0213
The safety of bevacizumab was evaluated in an open-label, controlled study (GOG-0213) in 325 patients with platinum-sensitive recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer, who have not received more than one previous regimen of chemotherapy [see Clinical Studies (14.9)]. Patients were randomized (1:1) to receive carboplatin and paclitaxel for 6 to 8 cycles or bevacizumab (15 mg/kg every 3 weeks) with carboplatin and paclitaxel for 6 to 8 cycles followed by bevacizumab as a single agent until disease progression or unacceptable toxicity. The demographics of the safety population were similar to the demographics of the efficacy population.
Grades 3–4 adverse reactions occurring at a higher incidence (≥2%) in patients receiving bevacizumab with chemotherapy compared to chemotherapy alone were: hypertension (11% vs. 0.6%), fatigue (8% vs. 3%), febrile neutropenia (6% vs. 3%), proteinuria (8% vs. 0%), abdominal pain (6% vs. 0.9%), hyponatremia (4% vs. 0.9%), headache (3% vs. 0.9%), and pain in extremity (3% vs. 0%). Adverse reactions are presented in Table 8.
| Adverse Reaction* | Bevacizumab with Carboplatin and Paclitaxel
(N=325) | Carboplatin and Paclitaxel
(N=332) |
|---|---|---|
|
||
|
Musculoskeletal and connective tissue |
||
|
Arthralgia |
45% |
30% |
|
Myalgia |
29% |
18% |
|
Pain in extremity |
25% |
14% |
|
Back pain |
17% |
10% |
|
Muscular weakness |
13% |
8% |
|
Neck pain |
9% |
0% |
|
Vascular |
||
|
Hypertension |
42% |
3% |
|
Gastrointestinal |
||
|
Diarrhea |
39% |
32% |
|
Abdominal pain |
33% |
28% |
|
Vomiting |
33% |
25% |
|
Stomatitis |
33% |
16% |
|
Nervous system |
||
|
Headache |
38% |
20% |
|
Dysarthria |
14% |
2% |
|
Dizziness |
13% |
8% |
|
Metabolism and nutrition |
||
|
Decreased appetite |
35% |
25% |
|
Hyperglycemia |
31% |
24% |
|
Hypomagnesemia |
27% |
17% |
|
Hyponatremia |
17% |
6% |
|
Weight loss |
15% |
4% |
|
Hypocalcemia |
12% |
5% |
|
Hypoalbuminemia |
11% |
6% |
|
Hyperkalemia |
9% |
3% |
|
Respiratory, thoracic and mediastinal |
||
|
Epistaxis |
33% |
2% |
|
Dyspnea |
30% |
25% |
|
Cough |
30% |
17% |
|
Rhinitis allergic |
17% |
4% |
|
Nasal mucosal disorder |
14% |
3% |
|
Skin and subcutaneous tissue |
||
|
Exfoliative rash |
23% |
16% |
|
Nail disorder |
10% |
2% |
|
Dry skin |
7% |
2% |
|
Renal and urinary |
||
|
Proteinuria |
17% |
1% |
|
Increased blood creatinine |
13% |
5% |
|
Hepatic |
||
|
Increased aspartate aminotransferase |
15% |
9% |
|
General |
||
|
Chest pain |
8% |
2% |
|
Infections |
||
|
Sinusitis |
7% |
2% |
6.2 Immunogenicity
As with all therapeutic proteins, there is a potential for immunogenicity. The detection of antibody formation is highly dependent on the sensitivity and the specificity of the assay. Additionally, the observed incidence of antibody (including neutralizing antibody) positivity in an assay may be influenced by several factors, including assay methodology, sample handling, timing of sample collection, concomitant medications, and underlying disease. For these reasons, comparison of the incidence of antibodies in the studies described below with the incidence of antibodies in other studies or to other bevacizumab products may be misleading.
In clinical studies for adjuvant treatment of a solid tumor, 0.6% (14/2233) of patients tested positive for treatment-emergent anti-bevacizumab antibodies as detected by an electrochemiluminescent (ECL) based assay. Among these 14 patients, three tested positive for neutralizing antibodies against bevacizumab using an enzyme-linked immunosorbent assay (ELISA). The clinical significance of these anti-bevacizumab antibodies is not known.
6.3 Postmarketing Experience
The following adverse reactions have been identified during postapproval use of bevacizumab products. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure.
General: Polyserositis
Cardiovascular: Pulmonary hypertension, Mesenteric venous occlusion
Gastrointestinal: Gastrointestinal ulcer, Intestinal necrosis, Anastomotic ulceration
Hemic and lymphatic: Pancytopenia
Hepatobiliary disorders: Gallbladder perforation
Musculoskeletal and Connective Tissue Disorders: Osteonecrosis of the jaw
Renal: Renal thrombotic microangiopathy (manifested as severe proteinuria)
Respiratory: Nasal septum perforation
Vascular: Arterial (including aortic) aneurysms, dissections, and rupture
7. Drug Interactions
Effects of ZIRABEV on Other Drugs
No clinically meaningful effect on the pharmacokinetics of irinotecan or its active metabolite SN38, interferon alfa, carboplatin or paclitaxel was observed when bevacizumab was administered in combination with these drugs; however, 3 of the 8 patients receiving bevacizumab with paclitaxel and carboplatin had lower paclitaxel exposure after four cycles of treatment (at Day 63) than those at Day 0, while patients receiving paclitaxel and carboplatin alone had a greater paclitaxel exposure at Day 63 than at Day 0.
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
Based on findings from animal studies and their mechanism of action [see Clinical Pharmacology (12.1)], bevacizumab products may cause fetal harm in pregnant women. Limited postmarketing reports describe cases of fetal malformations with use of bevacizumab products in pregnancy; however, these reports are insufficient to determine drug associated risks. In animal reproduction studies, intravenous administration of bevacizumab to pregnant rabbits every 3 days during organogenesis at doses approximately 1 to 10 times the clinical dose of 10 mg/kg produced fetal resorptions, decreased maternal and fetal weight gain and multiple congenital malformations including corneal opacities and abnormal ossification of the skull and skeleton including limb and phalangeal defects (see Data). Furthermore, animal models link angiogenesis and VEGF and VEGFR2 to critical aspects of female reproduction, embryo-fetal development, and postnatal development. Advise pregnant women of the potential risk to a fetus.
In the U.S. general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal Data
Pregnant rabbits dosed with 10 mg/kg to 100 mg/kg bevacizumab (approximately 1 to 10 times the clinical dose of 10 mg/kg) every three days during the period of organogenesis (gestation day 6–18) exhibited decreases in maternal and fetal body weights and increased number of fetal resorptions. There were dose-related increases in the number of litters containing fetuses with any type of malformation (42% for the 0 mg/kg dose, 76% for the 30 mg/kg dose, and 95% for the 100 mg/kg dose) or fetal alterations (9% for the 0 mg/kg dose, 15% for the 30 mg/kg dose, and 61% for the 100 mg/kg dose). Skeletal deformities were observed at all dose levels, with some abnormalities including meningocele observed only at the 100 mg/kg dose level. Teratogenic effects included: reduced or irregular ossification in the skull, jaw, spine, ribs, tibia and bones of the paws; fontanel, rib and hindlimb deformities; corneal opacity; and absent hindlimb phalanges.
8.2 Lactation
Risk Summary
No data are available regarding the presence of bevacizumab products in human milk, the effects on the breast fed infant, or the effects on milk production. Human IgG is present in human milk, but published data suggest that breast milk antibodies do not enter the neonatal and infant circulation in substantial amounts. Because of the potential for serious adverse reactions in breastfed infants, advise women not to breastfeed during treatment with ZIRABEV and for 6 months after the last dose.
8.3 Females and Males of Reproductive Potential
Infertility
Females
Bevacizumab products increase the risk of ovarian failure and may impair fertility. Inform females of reproductive potential of the risk of ovarian failure prior to the first-dose of ZIRABEV. Long-term effects of bevacizumab products on fertility are not known.
In a clinical study of 179 premenopausal women randomized to receive chemotherapy with or without bevacizumab, the incidence of ovarian failure was higher in patients who received bevacizumab with chemotherapy (34%) compared to patients who received chemotherapy alone (2%). After discontinuing bevacizumab with chemotherapy, recovery of ovarian function occurred in 22% of these patients [see Warnings and Precautions (5.11), Adverse Reactions (6.1)].
8.4 Pediatric Use
The safety and effectiveness of bevacizumab products in pediatric patients have not been established. In published literature reports, cases of non-mandibular osteonecrosis have been observed in patients under the age of 18 years who received bevacizumab. Bevacizumab products are not approved for use in patients under the age of 18 years.
Antitumor activity was not observed among eight pediatric patients with relapsed GBM who received bevacizumab and irinotecan. Addition of bevacizumab to standard of care did not result in improved event-free survival in pediatric patients enrolled in two randomized clinical studies, one in high grade glioma (n=121) and one in metastatic rhabdomyosarcoma or non-rhabdomyosarcoma soft tissue sarcoma (n=154).
Based on the population pharmacokinetics analysis of data from 152 pediatric and young adult patients with cancer (7 months to 21 years of age), bevacizumab clearance normalized by body weight in pediatrics was comparable to that in adults.
Juvenile Animal Toxicity Data
Juvenile cynomolgus monkeys with open growth plates exhibited physeal dysplasia following 4 to 26 weeks exposure at 0.4 to 20 times the recommended human dose (based on mg/kg and exposure). The incidence and severity of physeal dysplasia were dose-related and were partially reversible upon cessation of treatment.
8.5 Geriatric Use
In an exploratory, pooled analysis of 1745 patients from five randomized, controlled studies, 35% of patients were ≥65 years old. The overall incidence of ATE was increased in all patients receiving bevacizumab with chemotherapy as compared to those receiving chemotherapy alone, regardless of age; however, the increase in the incidence of ATE was greater in patients ≥65 years (8% vs. 3%) as compared to patients <65 years (2% vs. 1%) [see Warnings and Precautions (5.4)].
11. Zirabev Description
Bevacizumab-bvzr is a vascular endothelial growth factor inhibitor. Bevacizumab-bvzr is a recombinant humanized monoclonal IgG1 antibody that contains human framework regions and murine complementarity-determining regions. Bevacizumab-bvzr has an approximate molecular weight of 149 kDa. Bevacizumab-bvzr is produced in a mammalian cell (Chinese Hamster Ovary) expression system.
ZIRABEV (bevacizumab-bvzr) injection is a sterile, preservative-free, clear to slightly opalescent, colorless to pale brown solution in a single-dose vial for intravenous use. ZIRABEV contains bevacizumab-bvzr at a concentration of 25 mg/mL in either 100 mg/4 mL or 400 mg/16 mL single-dose vials.
Each mL of solution contains 25 mg bevacizumab-bvzr, edetate disodium dihydrate (0.05 mg), polysorbate 80 (0.2 mg), succinic acid (2.36 mg), sucrose (85 mg), and Water for Injection, USP. Sodium hydroxide is added to adjust the pH. The pH is 5.5.
12. Zirabev - Clinical Pharmacology
12.1 Mechanism of Action
Bevacizumab products bind VEGF and prevent the interaction of VEGF to its receptors (Flt-1 and KDR) on the surface of endothelial cells. The interaction of VEGF with its receptors leads to endothelial cell proliferation and new blood vessel formation in in vitro models of angiogenesis. Administration of bevacizumab to xenotransplant models of colon cancer in nude (athymic) mice caused reduction of microvascular growth and inhibition of metastatic disease progression.
12.3 Pharmacokinetics
The pharmacokinetic profile of bevacizumab was assessed using an assay that measures total serum bevacizumab concentrations (i.e., the assay did not distinguish between free bevacizumab and bevacizumab bound to VEGF ligand). Based on a population pharmacokinetic analysis of 491 patients who received 1 to 20 mg/kg of bevacizumab every week, every 2 weeks, or every 3 weeks, bevacizumab pharmacokinetics are linear and the predicted time to reach more than 90% of steady state concentration is 84 days. The accumulation ratio following a dose of 10 mg/kg of bevacizumab once every 2 weeks is 2.8.
Population simulations of bevacizumab exposures provide a median trough concentration of 80.3 mcg/mL on Day 84 (10th, 90th percentile: 45, 128) following a dose of 5 mg/kg once every two weeks.
Distribution
The mean (% coefficient of variation [CV%]) central volume of distribution is 2.9 (22%) L.
Elimination
The mean (CV%) clearance is 0.23 (33) L/day. The estimated half-life is 20 days (11 to 50 days).
Specific Populations
The clearance of bevacizumab varied by body weight, sex, and tumor burden. After correcting for body weight, males had a higher bevacizumab clearance (0.26 L/day vs. 0.21 L/day) and a larger central volume of distribution (3.2 L vs. 2.7 L) than females. Patients with higher tumor burden (at or above median value of tumor surface area) had a higher bevacizumab clearance (0.25 L/day vs. 0.20 L/day) than patients with tumor burdens below the median. In Study AVF2107g, there was no evidence of lesser efficacy (hazard ratio for overall survival) in males or patients with higher tumor burden treated with bevacizumab as compared to females and patients with low tumor burden.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
No studies have been conducted to assess potential of bevacizumab products for carcinogenicity or mutagenicity.
Bevacizumab products may impair fertility. Female cynomolgus monkeys treated with 0.4 to 20 times the recommended human dose of bevacizumab exhibited arrested follicular development or absent corpora lutea, as well as dose-related decreases in ovarian and uterine weights, endometrial proliferation, and the number of menstrual cycles. Following a 4- or 12-week recovery period, there was a trend suggestive of reversibility. After the 12-week recovery period, follicular maturation arrest was no longer observed, but ovarian weights were still moderately decreased. Reduced endometrial proliferation was no longer observed at the 12-week recovery time point; however, decreased uterine weight, absent corpora lutea, and reduced number of menstrual cycles remained evident.
13.2 Animal Toxicology and/or Pharmacology
Rabbits dosed with bevacizumab exhibited reduced wound healing capacity. Using full-thickness skin incision and partial thickness circular dermal wound models, bevacizumab dosing resulted in reductions in wound tensile strength, decreased granulation and re-epithelialization, and delayed time to wound closure.
14. Clinical Studies
14.1 Metastatic Colorectal Cancer
Study AVF2107g
The safety and efficacy of bevacizumab was evaluated in a double-blind, active-controlled study [AVF2107g (NCT00109070)] in 923 patients with previously untreated mCRC who were randomized (1:1:1) to placebo with bolus-IFL (irinotecan 125 mg/m2, fluorouracil 500 mg/m2, and leucovorin 20 mg/m2 given once weekly for 4 weeks every 6 weeks), bevacizumab (5 mg/kg every 2 weeks) with bolus-IFL, or bevacizumab (5 mg/kg every 2 weeks) with fluorouracil and leucovorin. Enrollment to the bevacizumab with fluorouracil and leucovorin arm was discontinued, after enrollment of 110 patients in accordance with the protocol-specified adaptive design. Bevacizumab was continued until disease progression or unacceptable toxicity or for a maximum of 96 weeks. The main outcome measure was overall survival (OS).
The median age was 60 years; 60% were male, 79% were White, 57% had an ECOG performance status of 0, 21% had a rectal primary and 28% received prior adjuvant chemotherapy. The dominant site of disease was extra-abdominal in 56% of patients and was the liver in 38% of patients.
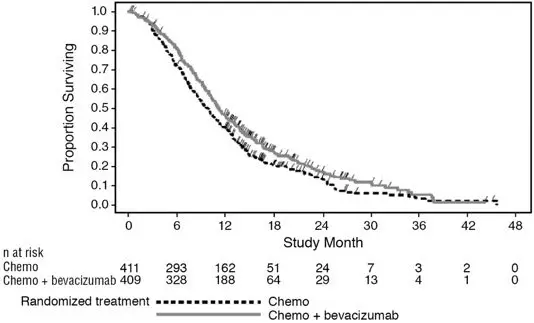
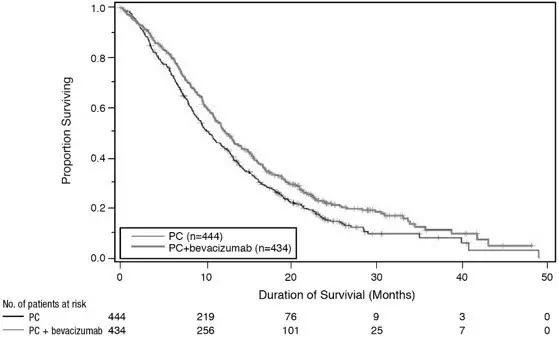
The addition of bevacizumab improved survival across subgroups defined by age (<65 years, ≥65 years) and sex. Results are presented in Table 9 and Figure 1.
| Efficacy Parameter | Bevacizumab with bolus-IFL
(N=402) | Placebo with bolus-IFL
(N=411) |
|---|---|---|
|
||
|
Overall Survival |
||
|
Median, in months |
20.3 |
15.6 |
|
Hazard ratio (95% CI) |
0.66 (0.54, 0.81) |
|
|
p-value* |
< 0.001 |
|
|
Progression-Free Survival |
||
|
Median, in months |
10.6 |
6.2 |
|
Hazard ratio (95% CI) |
0.54 (0.45, 0.66) |
|
|
p-value* |
< 0.001 |
|
|
Overall Response Rate |
||
|
Rate (%) |
45% |
35% |
|
p-value† |
< 0.01 |
|
|
Duration of Response |
||
|
Median, in months |
10.4 |
7.1 |
|
Figure 1: Kaplan-Meier Curves for Duration of Survival in Metastatic Colorectal Cancer in Study AVF2107g |
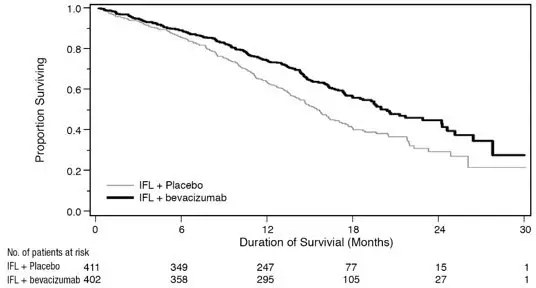 |
Among the 110 patients randomized to bevacizumab with fluorouracil and leucovorin, median OS was 18.3 months, median progression-free survival (PFS) was 8.8 months, overall response rate (ORR) was 39%, and median duration of response was 8.5 months.
Study E3200
The safety and efficacy of bevacizumab were evaluated in a randomized, open-label, active-controlled study [E3200 (NCT00025337)] in 829 patients who were previously treated with irinotecan and fluorouracil for initial therapy for metastatic disease or as adjuvant therapy. Patients were randomized (1:1:1) to FOLFOX4 (Day 1: oxaliplatin 85 mg/m2 and leucovorin 200 mg/m2 concurrently, then fluorouracil 400 mg/m2 bolus followed by 600 mg/m2 continuously; Day 2: leucovorin 200 mg/m2, then fluorouracil 400 mg/m2 bolus followed by 600 mg/m2 continuously; every 2 weeks), bevacizumab (10 mg/kg every 2 weeks prior to FOLFOX4 on Day 1) with FOLFOX4, or bevacizumab alone (10 mg/kg every 2 weeks). Bevacizumab was continued until disease progression or unacceptable toxicity. The main outcome measure was OS.
The bevacizumab alone arm was closed to accrual after enrollment of 244 of the planned 290 patients following a planned interim analysis by the data monitoring committee based on evidence of decreased survival compared to FOLFOX4 alone.
The median age was 61 years; 60% were male, 87% were White, 49% had an ECOG performance status of 0, 26% received prior radiation therapy, and 80% received prior adjuvant chemotherapy, 99% received prior irinotecan with or without fluorouracil for metastatic disease, and 1% received prior irinotecan and fluorouracil as adjuvant therapy.
The addition of bevacizumab to FOLFOX4 resulted in significantly longer survival as compared to FOLFOX4 alone; median OS was 13.0 months vs. 10.8 months [hazard ratio (HR) 0.75 (95% CI: 0.63, 0.89), p-value of 0.001 stratified log-rank test] with clinical benefit seen in subgroups defined by age (<65 years, ≥65 years) and sex. PFS and ORR based on investigator assessment were higher in patients receiving bevacizumab with FOLFOX4.
Study TRC-0301
The activity of bevacizumab with fluorouracil (as bolus or infusion) and leucovorin was evaluated in a single arm study [TRC-0301 (NCT00066846)] enrolling 339 patients with mCRC with disease progression following both irinotecan- and oxaliplatin-based chemotherapy. Seventy-three percent of patients received concurrent bolus fluorouracil and leucovorin. One objective partial response was verified in the first 100 evaluable patients for an ORR of 1% (95% CI: 0%, 5.5%).
Study ML18147
The safety and efficacy of bevacizumab were evaluated in a prospective, randomized, open-label, multinational, controlled study [ML18147 (NCT00700102)] in 820 patients with histologically confirmed mCRC who had progressed on a first-line bevacizumab-containing regimen. Patients were excluded if they progressed within 3 months of initiating first-line chemotherapy and if they received bevacizumab for less than 3 consecutive months in the first-line setting. Patients were randomized (1:1) within 3 months after discontinuing bevacizumab as first-line treatment to receive fluoropyrimidine-irinotecan- or fluoropyrimidine-oxaliplatin-based chemotherapy with or without bevacizumab (5 mg/kg every 2 weeks or 7.5 mg/kg every 3 weeks). The choice of second-line treatment was contingent upon first-line chemotherapy. Second-line treatment was administered until progressive disease or unacceptable toxicity. The main outcome measure was OS. A secondary outcome measure was ORR.
The median age was 63 years (21 to 84 years); 64% were male, 52% had an ECOG performance status of 1, 44% had an ECOG performance status of 0, 58% received irinotecan-based therapy as first-line treatment, 55% progressed on first-line treatment within 9 months, and 77% received their last dose of bevacizumab as first-line treatment within 42 days of being randomized. Second-line chemotherapy regimens were generally balanced between each arm.
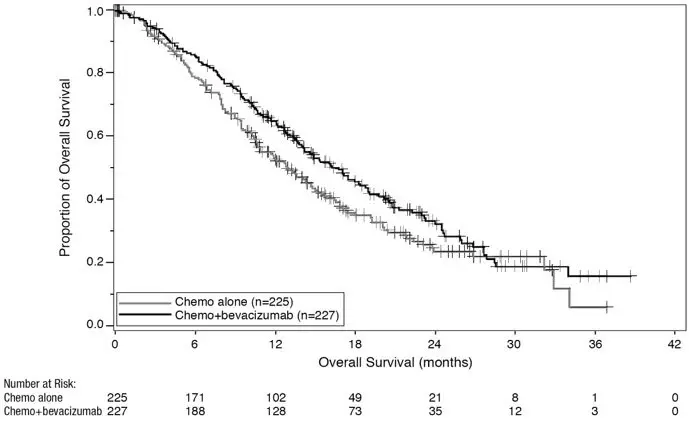
The addition of bevacizumab to fluoropyrimidine-based chemotherapy resulted in a statistically significant prolongation of OS and PFS. There was no significant difference in ORR. Results are presented in Table 10 and Figure 2.
| Efficacy Parameter | Bevacizumab with Chemotherapy
(N=409) | Chemotherapy
(N=411) |
|---|---|---|
|
||
|
Overall Survival* | ||
|
Median, in months |
11.2 |
9.8 |
|
Hazard ratio (95% CI) |
0.81 (0.69, 0.94) |
|
|
Progression-Free Survival† | ||
|
Median, in months |
5.7 |
4.0 |
|
Hazard ratio (95% CI) |
0.68 (0.59, 0.78) |
|
14.2 Lack of Efficacy in Adjuvant Treatment of Colon Cancer
Lack of efficacy of bevacizumab as an adjunct to standard chemotherapy for the adjuvant treatment of colon cancer was determined in two randomized, open-label, multicenter clinical studies.
The first study [BO17920 (NCT00112918)] was conducted in 3451 patients with high-risk stage II and III colon cancer, who had undergone surgery for colon cancer with curative intent. Patients were randomized to receive bevacizumab at a dose equivalent to 2.5 mg/kg/week on either a 2-weekly schedule with FOLFOX4 (N=1155) or on a 3-weekly schedule with XELOX (N=1145) or FOLFOX4 alone (N=1151). The main outcome measure was disease free survival (DFS) in patients with stage III colon cancer.
The median age was 58 years; 54% were male, 84% were White and 29% were ≥65 years. Eighty-three percent had stage III disease.
The addition of bevacizumab to chemotherapy did not improve DFS. As compared to FOLFOX4 alone, the proportion of stage III patients with disease recurrence or with death due to disease progression were numerically higher for patients receiving bevacizumab with FOLFOX4 or with XELOX. The hazard ratios for DFS were 1.17 (95% CI: 0.98, 1.39) for bevacizumab with FOLFOX4 versus FOLFOX4 alone and 1.07 (95% CI: 0.90, 1.28) for bevacizumab with XELOX versus FOLFOX4 alone. The hazard ratios for OS were 1.31 (95% CI: 1.03, 1.67) and 1.27 (95% CI: 1, 1.62) for the comparison of bevacizumab with FOLFOX4 versus FOLFOX4 alone and bevacizumab with XELOX versus FOLFOX4 alone, respectively. Similar lack of efficacy for DFS was observed in the bevacizumab-containing arms compared to FOLFOX4 alone in the high-risk stage II cohort.
In a second study [NSABP-C-08 (NCT00096278)], patients with stage II and III colon cancer who had undergone surgery with curative intent, were randomized to receive either bevacizumab administered at a dose equivalent to 2.5 mg/kg/week with mFOLFOX6 (N=1354) or mFOLFOX6 alone (N=1356). The median age was 57 years, 50% were male and 87% White. Seventy-five percent had stage III disease. The main outcome was DFS among stage III patients. The HR for DFS was 0.92 (95% CI: 0.77, 1.10). OS was not significantly improved with the addition of bevacizumab to mFOLFOX6 [HR 0.96 (95% CI: 0.75, 1.22)].
14.3 First-Line Non–Squamous Non–Small Cell Lung Cancer
Study E4599
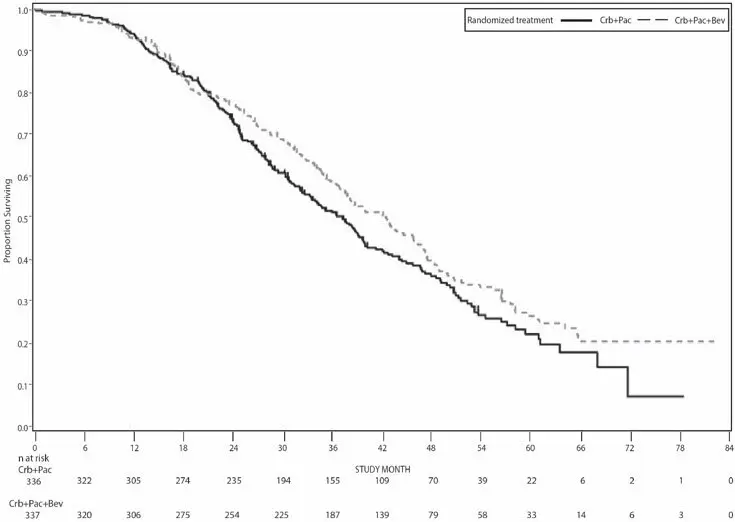
The safety and efficacy of bevacizumab as first-line treatment of patients with locally advanced, metastatic, or recurrent non-squamous NSCLC was studied in a single, large, randomized, active-controlled, open-label, multicenter study [E4599 (NCT00021060)]. A total of 878 chemotherapy-naïve patients with locally advanced, metastatic or recurrent non–squamous NSCLC were randomized (1:1) to receive six 21-day cycles of paclitaxel (200 mg/m2) and carboplatin (AUC 6) with or without bevacizumab 15 mg/kg. After completing or discontinuing chemotherapy, patients randomized to receive bevacizumab continued to receive bevacizumab alone until disease progression or until unacceptable toxicity. The trial excluded patients with predominant squamous histology (mixed cell type tumors only), CNS metastasis, gross hemoptysis (1/2 teaspoon or more of red blood), unstable angina, or receiving therapeutic anticoagulation. The main outcome measure was duration of survival.
The median age was 63 years; 54% were male, 43% were ≥65 years, and 28% had ≥5% weight loss at study entry. Eleven percent had recurrent disease. Of the 89% with newly diagnosed NSCLC, 12% had Stage IIIB with malignant pleural effusion and 76% had Stage IV disease.
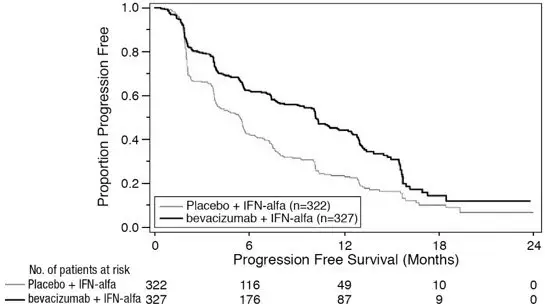
OS was statistically significantly longer for patients receiving bevacizumab with paclitaxel and carboplatin compared with those receiving chemotherapy alone. Median OS was 12.3 months vs. 10.3 months [HR 0.80 (95% CI: 0.68, 0.94), final p-value of 0.013, stratified log-rank test]. Based on investigator assessment which was not independently verified, patients were reported to have longer PFS with bevacizumab with paclitaxel and carboplatin compared to chemotherapy alone. Results are presented in Figure 3.
|
Figure 3: Kaplan-Meier Curves for Duration of Survival in First-Line Non-Squamous Non-Small Cell Lung Cancer in Study E4599 |
 |
In an exploratory analysis across patient subgroups, the impact of bevacizumab on OS was less robust in the following subgroups: women [HR 0.99 (95% CI: 0.79, 1.25)], patients ≥65 years [HR 0.91 (95% CI: 0.72, 1.14)] and patients with ≥5% weight loss at study entry [HR 0.96 (95% CI: 0.73, 1.26)].
Study BO17704
The safety and efficacy of bevacizumab in patients with locally advanced, metastatic or recurrent non-squamous NSCLC, who had not received prior chemotherapy was studied in another randomized, double-blind, placebo-controlled study [BO17704 (NCT00806923)]. A total of 1043 patients were randomized (1:1:1) to receive cisplatin and gemcitabine with placebo, bevacizumab 7.5 mg/kg or bevacizumab 15 mg/kg. The main outcome measure was PFS. Secondary outcome measure was OS.
The median age was 58 years; 36% were female and 29% were ≥65 years. Eight percent had recurrent disease and 77% had Stage IV disease.
PFS was significantly higher in both bevacizumab-containing arms compared to the placebo arm [HR 0.75 (95% CI: 0.62, 0.91), p-value of 0.0026 for bevacizumab 7.5 mg/kg and HR 0.82 (95% CI: 0.68, 0.98), p-value of 0.0301 for bevacizumab 15 mg/kg]. The addition of bevacizumab to cisplatin and gemcitabine failed to demonstrate an improvement in the duration of OS [HR 0.93 (95% CI: 0.78, 1.11), p-value of 0.420 for bevacizumab 7.5 mg/kg and HR 1.03 (95% CI: 0.86, 1.23), p-value of 0.761 for bevacizumab 15 mg/kg].
14.4 Recurrent Glioblastoma
Study EORTC 26101
The safety and efficacy of bevacizumab were evaluated in a multicenter, randomized (2:1), open-label study in patients with recurrent GBM (EORTC 26101, NCT01290939). Patients with first progression following radiotherapy and temozolomide were randomized (2:1) to receive bevacizumab (10 mg/kg every 2 weeks) with lomustine (90 mg/m2 every 6 weeks) or lomustine (110 mg/m2 every 6 weeks) alone until disease progression or unacceptable toxicity. Randomization was stratified by World Health Organization performance status (0 vs. >0), steroid use (yes vs. no), largest tumor diameter (≤40 vs. >40 mm), and institution. The main outcome measure was OS. Secondary outcome measures were investigator-assessed PFS and ORR per the modified Response Assessment in Neuro-oncology (RANO) criteria, health related quality of life (HRQoL), cognitive function, and corticosteroid use.
A total of 432 patients were randomized to receive lomustine alone (N=149) or bevacizumab with lomustine (N=283). The median age was 57 years; 24.8% of patients were ≥65 years. The majority of patients with were male (61%); 66% had a WHO performance status score >0; and in 56% the largest tumor diameter was ≤40 mm. Approximately 33% of patients randomized to receive lomustine received bevacizumab following documented progression.
No difference in OS (HR 0.91, p-value of 0.4578) was observed between arms; therefore, all secondary outcome measures are descriptive only. PFS was longer in the bevacizumab with lomustine arm [HR 0.52 (95% CI: 0.41, 0.64)] with a median PFS of 4.2 months in the bevacizumab with lomustine arm and 1.5 months in the lomustine arm. Among the 50% of patients receiving corticosteroids at the time of randomization, a higher percentage of patients in the bevacizumab with lomustine arm discontinued corticosteroids (23% vs. 12%).
Study AVF3708g and Study NCI 06-C-0064E
The efficacy and safety of bevacizumab 10 mg/kg every 2 weeks in patients with previously treated GBM were evaluated in one single arm single center study (NCI 06-C-0064E) and a randomized noncomparative multicenter study [AVF3708g(NCT00345163)]. Response rates in both studies were evaluated based on modified WHO criteria that considered corticosteroid use. In AVF3708g, the response rate was 25.9% (95% CI: 17%, 36.1%) with a median duration of response of 4.2 months (95% CI: 3, 5.7). In Study NCI 06-C-0064E, the response rate was 19.6% (95% CI: 10.9%, 31.3%) with a median duration of response of 3.9 months (95% CI: 2.4, 17.4).
14.5 Metastatic Renal Cell Carcinoma
Study BO17705
The safety and efficacy of bevacizumab were evaluated in patients with treatment-naïve mRCC in a multicenter, randomized, double-blind, international study [BO17705 (NCT00738530)] comparing interferon alfa and bevacizumab versus interferon alfa and placebo. A total of 649 patients who had undergone a nephrectomy were randomized (1:1) to receive either bevacizumab (10 mg/kg every 2 weeks; N=327) or placebo (every 2 weeks; N=322) with interferon alfa (9 MIU subcutaneously three times weekly for a maximum of 52 weeks). Patients were treated until disease progression or unacceptable toxicity. The main outcome measure was investigator-assessed PFS. Secondary outcome measures were ORR and OS.
The median age was 60 years (18 to 82 years); 70% were male and 96% were White. The study population was characterized by Motzer scores as follows: 28% favorable (0), 56% intermediate (1–2), 8% poor (3–5), and 7% missing.
PFS was statistically significantly prolonged among patients receiving bevacizumab compared to placebo; median PFS was 10.2 months vs. 5.4 months [HR 0.60 (95% CI: 0.49, 0.72), p-value < 0.0001, stratified log-rank test]. Among the 595 patients with measurable disease, ORR was also significantly higher (30% vs. 12%, p-value < 0.0001, stratified CMH test). There was no improvement in OS based on the final analysis conducted after 444 deaths, with a median OS of 23 months in the patients receiving bevacizumab with interferon alfa and 21 months in patients receiving interferon alone [HR 0.86, (95% CI: 0.72, 1.04)]. Results are presented in Figure 4.
14.6 Persistent, Recurrent, or Metastatic Cervical Cancer
Study GOG-0240
The safety and efficacy of bevacizumab were evaluated in patients with persistent, recurrent, or metastatic cervical cancer in a randomized, four-arm, multicenter study comparing bevacizumab with chemotherapy versus chemotherapy alone [GOG-0240 (NCT00803062)]. A total of 452 patients were randomized (1:1:1:1) to receive paclitaxel and cisplatin with or without bevacizumab, or paclitaxel and topotecan with or without bevacizumab.
The dosing regimens for bevacizumab, paclitaxel, cisplatin and topotecan were as follows:
- •
- Day 1: Paclitaxel 135 mg/m2 over 24 hours, Day 2: cisplatin 50 mg/m2 with bevacizumab;
- •
- Day 1: Paclitaxel 175 mg/m2 over 3 hours, Day 2: cisplatin 50 mg/m2 with bevacizumab;
- •
- Day 1: Paclitaxel 175 mg/m2 over 3 hours with cisplatin 50 mg/m2 with bevacizumab;
- •
- Day 1: Paclitaxel 175 mg/m2 over 3 hours with bevacizumab, Days 1–3: topotecan IV 0.75 mg/m2 over 30 minutes.
Patients were treated until disease progression or unacceptable adverse reactions. The main outcome measure was OS. Secondary outcome measures included ORR.
The median age was 48 years (20 to 85 years). Of the 452 patients randomized at baseline, 78% of patients were White, 80% had received prior radiation, 74% had received prior chemotherapy concurrent with radiation, and 32% had a platinum-free interval (PFI) of less than 6 months. Patients had a GOG performance status of 0 (58%) or 1 (42%). Demographic and disease characteristics were balanced across arms.
Results are presented in Figure 5 and Table 11.
| Efficacy Parameter | Bevacizumab with Chemotherapy
(N=227) | Chemotherapy
(N=225) |
|---|---|---|
|
||
|
Overall Survival |
||
|
Median, in months* |
16.8 |
12.9 |
|
Hazard ratio (95% CI) |
0.74 (0.58; 0.94) |
|
|
p-value† |
0.0132 |
|
The ORR was higher in patients who received bevacizumab with chemotherapy [45% (95% CI: 39, 52)] compared to patients who received chemotherapy alone [34% (95% CI: 28, 40)].
| Efficacy Parameter | Topotecan and Paclitaxel with or without Bevacizumab
(N=223) | Cisplatin and Paclitaxel with or without Bevacizumab
(N=229) |
|---|---|---|
|
||
|
Overall Survival |
||
|
Median, in months* |
13.3 |
15.5 |
|
Hazard ratio (95% CI) |
1.15 (0.91, 1.46) |
|
|
p-value |
0.23 |
|
The HR for OS with bevacizumab with cisplatin and paclitaxel as compared to cisplatin and paclitaxel alone was 0.72 (95% CI: 0.51, 1.02). The HR for OS with bevacizumab with topotecan and paclitaxel as compared to topotecan and paclitaxel alone was 0.76 (95% CI: 0.55, 1.06).
14.7 Stage III or IV Epithelial Ovarian, Fallopian Tube, or Primary Peritoneal Cancer Following Initial Surgical Resection
Study GOG-0218
The safety and efficacy of bevacizumab were evaluated in a multicenter, randomized, double-blind, placebo-controlled, three arm study [Study GOG-0218 (NCT00262847)] evaluating the effect of adding bevacizumab to carboplatin and paclitaxel for the treatment of patients with stage III or IV epithelial ovarian, fallopian tube, or primary peritoneal cancer (N=1873) following initial surgical resection. Patients were randomized (1:1:1) to one of the following arms:
- •
- CPP: carboplatin (AUC 6) and paclitaxel (175 mg/m2) for six cycles, with concurrent placebo started at cycle 2, followed by placebo alone every three weeks for a total of up to 22 cycles of therapy (n=625) or
- •
- CPB15: carboplatin (AUC 6) and paclitaxel (175 mg/m2) for six cycles, with concurrent bevacizumab started at cycle 2, followed by placebo alone every three weeks for a total of up to 22 cycles of therapy (n=625) or
- •
- CPB15+: carboplatin (AUC 6) and paclitaxel (175 mg/m2) for six cycles, with concurrent bevacizumab started at cycle 2, followed by bevacizumab as a single agent every three weeks for a total of up to 22 cycles of therapy (n=623).
The main outcome measure was investigator-assessed PFS. OS was a secondary outcome measure.
The median age was 60 years (range 22–89 years) and 28% of patients were >65 years of age. Overall, approximately 50% of patients had a GOG PS of 0 at baseline, and 43% a GOG PS score of 1. Patients had either epithelial ovarian cancer (83%), primary peritoneal cancer (15%), or fallopian tube cancer (2%). Serous adenocarcinoma was the most common histologic type (85% in CPP and CPB15 arms, 86% in CPB15+ arm). Overall, approximately 34% of patients had resected FIGO Stage III with residual disease <1 cm, 40% had resected Stage III with residual disease >1 cm, and 26% had resected Stage IV disease.
The majority of patients in all three treatment arms received subsequent antineoplastic treatment, 78.1% in the CPP arm, 78.6% in the CPB15 arm, and 73.2% in the CPB15+ arm. A higher proportion of patients in the CPP arm (25.3%) and CPB15 arm (26.6%) received at least one anti-angiogenic (including bevacizumab) treatment after discontinuing from study compared with the CPB15+ arm (15.6%).
Study results are presented in Table 13 and Figure 6.
| Efficacy Parameter | Bevacizumab with Carboplatin and Paclitaxel followed by Bevacizumab Alone
(N=623) | Bevacizumab with Carboplatin and Paclitaxel
(N=625) | Carboplatin and Paclitaxel
(N=625) |
|---|---|---|---|
| NS=not significant. | |||
|
|||
|
Progression-Free Survival per Investigator | |||
|
Median, in months |
18.2 |
12.8 |
12.0 |
|
Hazard ratio (95% CI)* |
0.62 (0.52, 0.75) |
0.83 (0.70, 0.98) | |
|
p-value† |
< 0.0001 |
NS | |
|
Overall Survival‡ | |||
|
Median, in months |
43.8 |
38.8 |
40.6 |
|
Hazard ratio (95% CI)* |
0.89 (0.76, 1.05) |
1.06 (0.90, 1.24) | |
14.8 Platinum-Resistant Recurrent Epithelial Ovarian, Fallopian Tube, or Primary Peritoneal Cancer
Study MO22224
The safety and efficacy of bevacizumab were evaluated in a multicenter, open-label, randomized study [MO22224 (NCT00976911)] comparing bevacizumab with chemotherapy versus chemotherapy alone in patients with platinum-resistant recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer that recurred within <6 months from the most recent platinum-based therapy (N=361). Patients had received no more than 2 prior chemotherapy regimens. Patients received one of the following chemotherapy regimens at the discretion of the investigator: paclitaxel (80 mg/m2 on days 1, 8, 15 and 22 every 4 weeks); pegylated liposomal doxorubicin (40 mg/m2 on day 1 every 4 weeks); or topotecan (4 mg/m2 on days 1, 8 and 15 every 4 weeks or 1.25 mg/m2 on days 1–5 every 3 weeks). Patients were treated until disease progression, unacceptable toxicity, or withdrawal. Forty percent of patients on the chemotherapy alone arm received bevacizumab alone upon progression. The main outcome measure was investigator-assessed PFS. Secondary outcome measures were ORR and OS.
The median age was 61 years (25 to 84 years) and 37% of patients were ≥65 years. Seventy-nine percent had measurable disease at baseline, 87% had baseline CA-125 levels ≥2 times ULN and 31% had ascites at baseline. Seventy-three percent had a PFI of 3 months to 6 months and 27% had PFI of <3 months. ECOG performance status was 0 for 59%, 1 for 34%, and 2 for 7% of the patients.
The addition of bevacizumab to chemotherapy demonstrated a statistically significant improvement in investigator-assessed PFS, which was supported by a retrospective independent review analysis. Results for the ITT population are presented in Table 14 and Figure 7. Results for the separate chemotherapy cohorts are presented in Table 15.
| Efficacy Parameter | Bevacizumab with Chemotherapy
(N=179) | Chemotherapy
(N=182) |
|---|---|---|
|
||
|
Progression-Free Survival per Investigator |
||
|
Median (95% CI), in months |
6.8 (5.6, 7.8) |
3.4 (2.1, 3.8) |
|
Hazard ratio (95% CI)* |
0.38 (0.30, 0.49) |
|
|
p-value† |
< 0.0001 |
|
|
Overall Survival |
||
|
Median (95% CI), in months |
16.6 (13.7, 19.0) |
13.3 (11.9, 16.4) |
|
Hazard ratio (95% CI)* |
0.89 (0.69, 1.14) |
|
|
Overall Response Rate |
||
|
Number of patients with measurable disease at baseline |
142 |
144 |
|
Rate, % (95% CI) |
28% (21%, 36%) |
13% (7%, 18%) |
|
Duration of Response |
||
|
Median, in months |
9.4 |
5.4 |
| Efficacy Parameter | Paclitaxel | Topotecan | Pegylated Liposomal Doxorubicin | |||
|---|---|---|---|---|---|---|
| Bevacizumab with Chemotherapy | Chemotherapy | Bevacizumab with Chemotherapy | Chemotherapy | Bevacizumab with Chemotherapy | Chemotherapy | |
| (N=60) | (N=55) | (N=57) | (N=63) | (N=62) | (N=64) | |
| NE=Not Estimable. | ||||||
|
||||||
|
Progression-Free Survival per Investigator |
||||||
|
Median, in months |
9.6 |
3.9 |
6.2 |
2.1 |
5.1 |
3.5 |
|
Hazard ratio*
|
0.47 |
0.24 |
0.47 |
|||
|
Overall Survival |
||||||
|
Median, in months |
22.4 |
13.2 |
13.8 |
13.3 |
13.7 |
14.1 |
|
Hazard ratio*
|
0.64 |
1.12 |
0.94 |
|||
|
Overall Response Rate |
||||||
|
Number of patients with measurable disease at baseline |
45 |
43 |
46 |
50 |
51 |
51 |
|
Rate, % |
53 |
30 |
17 |
2 |
16 |
8 |
|
Duration of Response |
||||||
|
Median, in months |
11.6 |
6.8 |
5.2 |
NE |
8.0 |
4.6 |
14.9 Platinum-Sensitive Recurrent Epithelial Ovarian, Fallopian Tube, or Primary Peritoneal Cancer
Study AVF4095g
The safety and efficacy of bevacizumab were evaluated in a randomized, double-blind, placebo-controlled study [AVF4095g (NCT00434642)] studying bevacizumab with chemotherapy versus chemotherapy alone in the treatment of patients with platinum-sensitive recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who have not received prior chemotherapy in the recurrent setting or prior bevacizumab treatment (N=484). Patients were randomized (1:1) to receive bevacizumab (15 mg/kg day 1) or placebo every 3 weeks with carboplatin (AUC 4, day 1) and gemcitabine (1000 mg/m2 on days 1 and 8) for 6 to 10 cycles followed by bevacizumab or placebo alone until disease progression or unacceptable toxicity. The main outcome measures were investigator-assessed PFS. Secondary outcome measures were ORR and OS.
The median age was 61 years (28 to 87 years) and 37% of patients were ≥65 years. All patients had measurable disease at baseline, 74% had baseline CA-125 levels >ULN (35 U/mL). The PFI was 6 months to 12 months in 42% of patients and >12 months in 58% of patients. The ECOG performance status was 0 or 1 for 99.8% of patients.
A statistically significant prolongation in PFS was demonstrated among patients receiving bevacizumab with chemotherapy compared to those receiving placebo with chemotherapy (Table 16 and Figure 8). Independent radiology review of PFS was consistent with investigator assessment [HR 0.45 (95% CI: 0.35, 0.58)]. OS was not significantly improved with the addition of bevacizumab to chemotherapy [HR 0.95 (95% CI: 0.77, 1.17)].
| Efficacy Parameter | Bevacizumab with Gemcitabine and Carboplatin
(N=242) | Placebo with Gemcitabine and Carboplatin
(N=242) |
|---|---|---|
|
Progression-Free Survival |
||
|
Median, in months |
12.4 |
8.4 |
|
Hazard ratio |
0.46 |
|
|
p-value |
< 0.0001 |
|
|
Overall Response Rate |
||
|
% patients with overall response |
78% |
57% |
|
p-value |
< 0.0001 |
|
Study GOG-0213
The safety and efficacy of bevacizumab were evaluated in a randomized, controlled, open-label study [Study GOG-0213 (NCT00565851)] of bevacizumab with chemotherapy versus chemotherapy alone in the treatment of patients with platinum-sensitive recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer, who have not received more than one previous regimen of chemotherapy (N=673). Patients were randomized (1:1) to receive carboplatin (AUC 5) and paclitaxel (175 mg/m2 IV over 3 hours) every 3 weeks for 6 to 8 cycles (N=336) or bevacizumab (15 mg/kg) every 3 weeks with carboplatin (AUC 5) and paclitaxel (175 mg/m2 IV over 3 hours) for 6 to 8 cycles followed by bevacizumab (15 mg/kg every 3 weeks) as a single agent until disease progression or unacceptable toxicity. The main outcome measure was OS. Other outcome measures were investigator-assessed PFS, and ORR.
The median age was 60 years (23 to 85 years) and 33% of patients were ≥65 years. Eighty-three percent had measurable disease at baseline and 74% had abnormal CA-125 levels at baseline. Ten percent of patients had received prior bevacizumab. Twenty-six percent had a PFI of 6 months to 12 months and 74% had a PFI of >12 months. GOG performance status was 0 or 1 for 99% of patients.
Results are presented in Table 17 and Figure 9.
| Efficacy Parameter | Bevacizumab with Carboplatin and Paclitaxel
(N=337) | Carboplatin and Paclitaxel
(N=336) |
|---|---|---|
|
||
|
Overall Survival |
||
|
Median, in months |
42.6 |
37.3 |
|
Hazard ratio (95% CI) |
0.84 (0.69, 1.01) |
|
|
Hazard ratio (95% CI) |
0.82 (0.68, 0.996) |
|
|
Progression-Free Survival |
||
|
Median, in months |
13.8 |
10.4 |
|
Hazard ratio (95% CI) |
0.61 (0.51, 0.72) |
|
|
Overall Response Rate |
||
|
Number of patients with measurable disease at baseline |
274 |
286 |
|
Rate, % |
213 (78%) |
159 (56%) |
16. How is Zirabev supplied
ZIRABEV (bevacizumab-bvzr) injection is a clear to slightly opalescent, colorless to pale brown, sterile solution for intravenous infusion supplied in a carton containing one single-dose vial in the following strengths:
- •
- 100 mg/4 mL (25 mg/mL) (NDC 0069-0315-01)
- •
- 400 mg/16 mL (25 mg/mL) (NDC 0069-0342-01)
17. Patient Counseling Information
Gastrointestinal Perforations and Fistulae
Bevacizumab products may increase the risk of developing gastrointestinal perforations and fistulae. Advise patients to immediately contact their healthcare provider for high fever, rigors, persistent or severe abdominal pain, severe constipation, or vomiting [see Warnings and Precautions (5.1)].
Surgery and Wound Healing Complications
Bevacizumab products can increase the risk of wound healing complications. Instruct patients not to undergo surgery without first discussing this potential risk with their healthcare provider [see Warnings and Precautions (5.2)].
Hemorrhage
Bevacizumab products can increase the risk of hemorrhage. Advise patients to immediately contact their healthcare provider for signs and symptoms of serious or unusual bleeding including coughing or spitting blood [see Warnings and Precautions (5.3)].
Arterial and Venous Thromboembolic Events
Bevacizumab products increase the risk of arterial and venous thromboembolic events. Advise patients to immediately contact their healthcare provider for signs and symptoms of arterial or venous thromboembolism [see Warnings and Precautions (5.4, 5.5)].
Hypertension
Bevacizumab products can increase blood pressure. Advise patients that they will undergo routine blood pressure monitoring and to contact their healthcare provider if they experience changes in blood pressure [see Warnings and Precautions (5.6)].
Posterior Reversible Leukoencephalopathy Syndrome
Posterior reversible encephalopathy syndrome (PRES) has been associated with bevacizumab products treatment. Advise patients to immediately contact their healthcare provider for new onset or worsening neurological function [see Warnings and Precautions (5.7)].
Renal Injury and Proteinuria
Bevacizumab products increase the risk of proteinuria and renal injury, including nephrotic syndrome. Advise patients that treatment with ZIRABEV requires regular monitoring of renal function and to contact their healthcare provider for proteinuria or signs and symptoms of nephrotic syndrome [see Warnings and Precautions (5.8)].
Infusion-Related Reactions
Bevacizumab products can cause infusion-related reactions. Advise patients to contact their healthcare provider immediately for signs or symptoms of infusion-related reactions [see Warnings and Precautions (5.9)].
Congestive Heart Failure
Bevacizumab products can increase the risk of developing congestive heart failure. Advise patients to contact their healthcare provider immediately for signs and symptoms of CHF [see Warnings and Precautions (5.12)].
Embryo-Fetal Toxicity
Advise female patients that bevacizumab products may cause fetal harm and to inform their healthcare provider with a known or suspected pregnancy [see Warnings and Precautions (5.10), Use in Specific Populations (8.1)]. Advise females of reproductive potential to use effective contraception during treatment with ZIRABEV and for 6 months after the last dose [see Use in Specific Populations (8.3)].
This product's labeling may have been updated. For the most recent prescribing information, please visit www.pfizer.com.
For medical information about ZIRABEV, please visit www.pfizermedinfo.com or call 1-800-438-1985.
Manufactured by
Pfizer Inc.
NY, NY 10017
US License No. 2001
Distributed by
Pfizer Labs
Division of Pfizer Inc.
NY, NY 10017
LAB-1185-5.0
PRINCIPAL DISPLAY PANEL - 4 mL Vial Label
NDC 0069-0315-01
Rx only
Zirabev™
(bevacizumab–bvzr)
Injection
100 mg/4 mL
(25 mg/mL)
For Intravenous Infusion
After Dilution
One SINGLE-DOSE VIAL
DISCARD UNUSED PORTION.
PRINCIPAL DISPLAY PANEL - 4 mL Vial Carton
NDC 0069-0315-01
Zirabev™
(bevacizumab–bvzr)
Injection
100 mg/4 mL
(25 mg/mL)
For Intravenous Infusion
After Dilution
One SINGLE-DOSE VIAL
DISCARD UNUSED PORTION.
Rx only
Pfizer Oncology
| ZIRABEV
bevacizumab-bvzr injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| ZIRABEV
bevacizumab-bvzr injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Pfizer Laboratories Div Pfizer Inc (134489525) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pfizer Ireland Pharmaceuticals | 985586408 | ANALYSIS(0069-0315, 0069-0342) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Pharmacia & Upjohn Company LLC | 618054084 | ANALYSIS(0069-0315, 0069-0342) , MANUFACTURE(0069-0315, 0069-0342) , PACK(0069-0315, 0069-0342) , LABEL(0069-0315, 0069-0342) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Wyeth BioPharma Division of Wyeth Pharmaceuticals LLC | 174350868 | ANALYSIS(0069-0315, 0069-0342) , API MANUFACTURE(0069-0315, 0069-0342) | |