Drug Detail:Roflumilast (topical) (monograph) (Zoryve)
Drug Class:
Highlights of Prescribing Information
ZORYVE™ (roflumilast) cream, for topical use
Initial U.S. Approval: 2011
Indications and Usage for Zoryve Cream
ZORYVE is a phosphodiesterase 4 inhibitor indicated for topical treatment of plaque psoriasis, including intertriginous areas, in patients 12 years of age and older. (1)
Zoryve Cream Dosage and Administration
- Apply once daily to affected areas. (2)
- For topical use only. (2)
- Not for ophthalmic, oral, or intravaginal use. (2)
Dosage Forms and Strengths
Cream, 0.3%: 3 mg of roflumilast per gram in 60-gram tubes. (3)
Contraindications
- Moderate to severe liver impairment (Child-Pugh B or C). (4)
Adverse Reactions/Side Effects
The most common adverse reactions (reported in ≥1% of patients) are diarrhea, headache, insomnia, application site pain, upper respiratory tract infections, and urinary tract infections. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Arcutis Biotherapeutics, Inc. at 1-844-692-6729 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Coadministration of roflumilast with systemic CYP3A4 inhibitors or dual inhibitors that inhibit both CYP3A4 and CYP1A2 simultaneously may increase roflumilast systemic exposure and may result in increased adverse reactions. The risk of such concurrent use should be weighed carefully against benefit. (7.1)
- Coadministration of roflumilast with oral contraceptives containing gestodene and ethinyl estradiol may increase roflumilast systemic exposure and may result in increased side effects. The risk of such concurrent use should be weighed carefully against benefit. (7.2)
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 7/2022
Full Prescribing Information
1. Indications and Usage for Zoryve Cream
ZORYVE™ is indicated for topical treatment of plaque psoriasis, including intertriginous areas, in patients 12 years of age and older.
2. Zoryve Cream Dosage and Administration
Apply ZORYVE to affected areas once daily and rub in completely. Wash hands after application, unless ZORYVE is for treatment of the hands.
ZORYVE is for topical use only and not for ophthalmic, oral, or intravaginal use.
3. Dosage Forms and Strengths
Cream, 0.3%: 3 mg of roflumilast per gram of white to off-white cream in 60-gram tubes.
4. Contraindications
The use of ZORYVE is contraindicated in the following condition:
- Moderate to severe liver impairment (Child-Pugh B or C) [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
6. Adverse Reactions/Side Effects
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
In two multicenter, randomized, double-blind, vehicle-controlled trials (DERMIS-1 and DERMIS-2), 881 subjects 2 years of age or older with plaque psoriasis were treated with ZORYVE or vehicle once daily for 8 weeks.
The median age was 47 years (range 6 to 88). The majority of the subjects were male (64%) and White (82%). The median body surface area (BSA) affected was 5.5% (range 2% to 20%).
The proportion of subjects who discontinued treatment due to adverse reaction was 1.0% for subjects treated with ZORYVE and 1.3% for subjects treated with vehicle. The most common adverse reactions that led to discontinuation of ZORYVE was application site urticaria (0.3%).
Table 1 presents adverse reactions that occurred in at least 1% of subjects treated with ZORYVE, and for which the rate exceeded the rate for vehicle.
| Adverse Reaction | ZORYVE (N=576) n (%) | Vehicle (N=305) n (%) |
|---|---|---|
| Diarrhea | 18 (3.1) | 0 (0.0) |
| Headache | 14 (2.4) | 3 (1.0) |
| Insomnia | 8 (1.4) | 2 (0.7) |
| Nausea | 7 (1.2) | 1 (0.3) |
| Application site pain | 6 (1.0) | 1 (0.3) |
| Upper respiratory tract infection | 6 (1.0) | 1 (0.3) |
| Urinary tract infection | 6 (1.0) | 2 (0.7) |
In 594 subjects who continued treatment with ZORYVE for up to 64 weeks in open-label extension trials, the adverse reaction profile was similar to that observed in vehicle-controlled trials.
7. Drug Interactions
No formal drug-drug interaction studies were conducted with ZORYVE.
7.1 Drugs that Inhibit Cytochrome P450 (CYP) Enzymes
The coadministration of roflumilast with systemic CYP3A4 inhibitors or dual inhibitors that inhibit both CYP3A4 and CYP1A2 simultaneously (e.g., erythromycin, ketoconazole, fluvoxamine, enoxacin, cimetidine) may increase roflumilast systemic exposure and may result in increased adverse reactions. The risk of such concurrent use should be weighed carefully against benefit [see Clinical Pharmacology (12.3)].
7.2 Oral Contraceptives Containing Gestodene and Ethinyl Estradiol
The coadministration of roflumilast with oral contraceptives containing gestodene and ethinyl estradiol may increase roflumilast systemic exposure and may result in increased side effects. The risk of such concurrent use should be weighed carefully against benefit [see Clinical Pharmacology (12.3)].
8. Use In Specific Populations
8.4 Pediatric Use
The safety and effectiveness of ZORYVE have been established in pediatric patients ages 12 years and older for the treatment of plaque psoriasis. Use of ZORYVE in this age group is supported by data from two 8-week vehicle-controlled safety and efficacy trials which included 14 adolescent patients aged 12 to 17 years, of whom 8 received ZORYVE. Eighteen adolescent patients were treated with ZORYVE in open-label trials of 2- and 24-weeks duration. The adverse reaction profile was similar to that observed in adults [see Adverse Reactions (6.1), Clinical Pharmacology (12.3), and Clinical Studies (14)].
The safety and effectiveness of ZORYVE in pediatric patients below the age of 12 years have not been established.
8.5 Geriatric Use
Of the 881 subjects with psoriasis exposed to ZORYVE or vehicle for up to 8 weeks in 2 controlled clinical trials, 106 were 65 years of age or older. No overall differences in safety or effectiveness were observed between these subjects and younger subjects. Other reported clinical experience has not identified differences in responses between the geriatric and younger patients, but greater sensitivity of some older individuals cannot be ruled out. Based on available data for roflumilast, no adjustment of dosage in geriatric patients is warranted [see Clinical Pharmacology (12.3)].
8.6 Hepatic Impairment
Oral roflumilast 250 mcg once daily for 14 days was studied in subjects with hepatic impairment. The AUC and Cmax values of roflumilast and roflumilast N-oxide were increased in subjects with moderate (Child-Pugh B) hepatic impairment. ZORYVE is contraindicated in patients with moderate to severe liver impairment (Child-Pugh B or C) [see Contraindications (4), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
11. Zoryve Cream Description
ZORYVE (roflumilast) cream, 0.3% is a white to off-white cream for topical use. The active ingredient, roflumilast, is a phosphodiesterase 4 (PDE4) inhibitor.
Roflumilast is described chemically as 3-cyclopropylmethoxy-N-(3,5-dichloropyridin-4-yl)-4-(difluoromethoxy)benzamide. The empirical formula is C17H14Cl2F2N2O3, and the molecular weight is 403.21.
The structural formula is represented below:
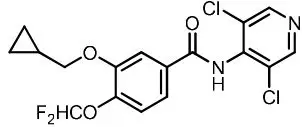
Roflumilast is practically insoluble in water and hexane, sparingly soluble in ethanol, and freely soluble in acetone.
Each gram of ZORYVE contains 3 mg of roflumilast in a cream base containing ceteareth-10 phosphate, cetearyl phosphate, cetostearyl alcohol, diethylene glycol monoethyl ether, hexylene glycol, isopropyl palmitate, methylparaben, propylparaben, purified water, sodium hydroxide, and white petrolatum. Hydrochloric acid may have been added to adjust pH.
12. Zoryve Cream - Clinical Pharmacology
12.1 Mechanism of Action
Roflumilast and its active metabolite (roflumilast N-oxide) are inhibitors of PDE4. Roflumilast and roflumilast N-oxide inhibition of PDE4 (a major cyclic 3',5'-adenosine monophosphate (cyclic AMP) metabolizing enzyme) activity leads to accumulation of intracellular cyclic AMP. The specific mechanism(s) by which roflumilast exerts its therapeutic action is not well defined.
12.3 Pharmacokinetics
Metabolism
Roflumilast is extensively metabolized via Phase I (cytochrome P450) and Phase II (conjugation) reactions. The N-oxide metabolite is the only major metabolite observed in the plasma of humans. Following oral administration, roflumilast and roflumilast N-oxide account for the majority (87.5%) of total dose administered in plasma. Roflumilast was not detectable in urine, while roflumilast N-oxide was only a trace metabolite (less than 1%). Other conjugated metabolites such as roflumilast N-oxide glucuronide and 4-amino-3,5-dichloropyridine N-oxide were detected in urine.
While roflumilast is three times more potent than roflumilast N-oxide at inhibition of the PDE4 enzyme in vitro, the plasma AUC of roflumilast N-oxide on average is approximately 8-fold greater than the plasma AUC of roflumilast following topical administration. A similar ratio was observed following intravenous administration, whereas following oral administration the N-oxide metabolite circulated on average about 10-fold higher than the parent.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Long-term studies were conducted in hamsters and mice with roflumilast to evaluate its carcinogenic potential. In 2-year oral gavage carcinogenicity studies, roflumilast treatment resulted in dose-related, statistically significant increases in the incidence of undifferentiated carcinomas of nasal epithelium in hamsters at doses greater than or equal to 8 mg/kg/day (6 times the MRHD on an AUC basis). The tumorigenicity of roflumilast appears to be attributed to a reactive metabolite of 4-amino-3,5-dichloropyridine N-oxide (ADCP N-oxide). No evidence of tumorigenicity was observed in mice at roflumilast oral doses up to 12 and 18 mg/kg/day in females and males, respectively (6 and 8 times the MRHD, respectively, on an AUC basis).
In a 2-year dermal mouse carcinogenicity study, no evidence of carcinogenicity was observed at topical doses of roflumilast cream up to 1% applied at 2 mL/kg/day (2 times the MRHD on an AUC basis).
Roflumilast tested positive in an in vivo mouse micronucleus test, but negative in the following assays: the Ames test, an in vitro chromosome aberration assay in human lymphocytes, an in vitro HPRT assay with V79 cells, an in vitro micronucleus test with V79 cells, a DNA adduct formation assay in rat nasal mucosa, liver and testes, and an in vivo mouse bone marrow chromosome aberration assay. Roflumilast N-oxide was negative in the Ames test and an in vitro micronucleus test with V79 cells.
In a human spermatogenesis study, oral roflumilast 500 mcg had no effects on semen parameters or reproductive hormones during the 3-month treatment period and the following 3-month off-treatment period. In a fertility study, oral roflumilast decreased fertility rates in male rats at 1.8 mg/kg/day (9 times the MRHD on a mg/m2 basis). The male rats also showed increases in the incidence of tubular atrophy, degeneration in the testis, and spermiogenic granuloma in the epididymides. No effect on rat fertility rate or male reproductive organ morphology was observed at 0.6 mg/kg/day (3 times the MRHD on a mg/m2 basis). In a female fertility study, no effect on fertility was observed up to the highest roflumilast dose of 1.5 mg/kg/day in rats (7 times the MRHD on a mg/m2 basis).
14. Clinical Studies
Two multicenter, randomized, double-blind, vehicle-controlled trials (DERMIS-1 [NCT04211363] and DERMIS-2 [NCT04211389]) enrolled a total of 881 subjects with mild to severe plaque psoriasis and an affected BSA of 2% to 20%. The study population ranged in age from 6 to 88 years with 4 subjects younger than 12 years of age at baseline. At baseline, 16% of subjects had an Investigator's Global Assessment (IGA) score of 2 (mild), 76% had an IGA score of 3 (moderate), and 8% had an IGA score of 4 (severe). One hundred seventy-nine (20%) subjects had an intertriginous IGA (I-IGA) score of 2 or higher (mild) at baseline, and 678 (77%) subjects had a baseline Worst Itch-Numeric Rating Score (WI-NRS) score of 4 or higher on a scale of 0 to 10.
Subjects were randomized 2:1 to receive ZORYVE or vehicle applied once daily for 8 weeks. The primary endpoint was the proportion of subjects who achieved IGA treatment success at Week 8 (Table 2). Success was defined as a score of "Clear" (0) or "Almost Clear" (1), plus a 2-grade improvement from baseline.
Secondary endpoints included the proportion of subjects that achieved I-IGA success at Week 8 and WI-NRS success sequentially at Weeks 8, 4, and 2. WI-NRS success was defined as a reduction of at least 4 points from baseline in subjects with a baseline WI-NRS score of at least 4.
| DERMIS-1 | DERMIS-2 | |||
|---|---|---|---|---|
| ZORYVE | Vehicle | ZORYVE | Vehicle | |
| Number of subjects randomized | N=286 | N=153 | N=290 | N=152 |
| Abbreviations: CI = Confidence Interval | ||||
|
||||
| IGA success* | 41.5% | 5.8% | 36.7% | 7.1% |
| Difference from vehicle (95% CI)† | 39.7% (32.4%, 47.0%) | 29.5% (21.5%, 37.6%) | ||
Among subjects with an I-IGA score of at least 2 (mild) at baseline (approximately 22% of subjects in DERMIS-1 and 19% in DERMIS-2), there was a higher percentage of subjects who achieved I-IGA success at Week 8 in the group who received ZORYVE compared to the group who received vehicle (DERMIS-1: 71.5% vs. 13.8%; DERMIS-2: 67.5% vs. 17.4%).
Figure 1: WI-NRS Success Over Time*
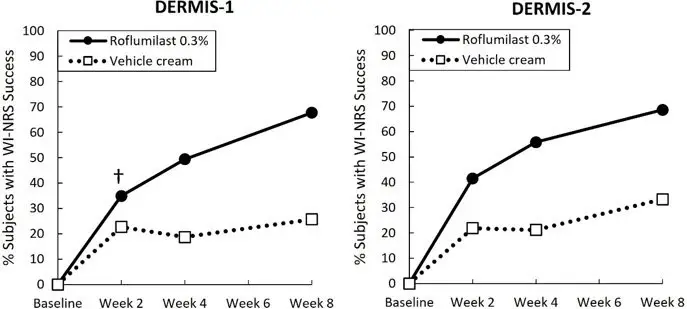
*WI-NRS success is a reduction of at least 4 points in subjects with a WI-NRS score of 4 or higher at baseline.
†The treatment difference at Week 2 in DERMIS-1 was not statistically significant.
16. How is Zoryve Cream supplied
| ZORYVE
roflumilast cream |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Arcutis Biotherapeutics, Inc. (080642948) |