What is angioedema?
Angioedema is sudden swelling caused by fluid that collects in deep layers of the skin. Swelling occurs most often on the face, lips, tongue, or throat, but it can happen anywhere in the body.
What increases my risk for angioedema?
The exact cause of angioedema is often unknown. The following may increase your risk or trigger symptoms:
- Allergic reactions to foods, insect stings, or latex
- Medicines, such as ACE inhibitors, NSAIDs, and aspirin
- Cold, heat, pressure, trauma, or emotional stress
- A medical condition, such as autoimmune thyroid disease, lupus, or cancer
- A family history of angioedema
What are the signs and symptoms of angioedema?
Skin swelling may be the only symptom. Swelling may be on one or both sides of the affected area. You may also have any of the following:
- Pain and burning in the swollen area
- Hives or an itchy rash
- A cough, wheezing, and shortness of breath
- Irritated eyes and nose
- Abdominal pain
How is the cause of angioedema diagnosed?
Your healthcare provider will examine you and ask about your symptoms. Your provider may also ask about your family medical history, medicines you take, and foods you eat. Tell your provider about any recent trauma, stress, or contact with allergens. You may need additional testing if you developed anaphylaxis after you were exposed to a trigger and then exercised. This is called exercise-induced anaphylaxis. You may need any of the following:
- Blood tests may be used to check for an autoimmune disease, infection, or inflammation. The tests may also be used to check your liver function.
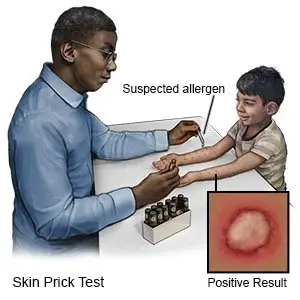
- Skin prick tests are done to check for allergies. Your provider will place drops of solution on your skin. Each drop will contain a small amount of 1 possible allergen. Your provider will then prick or scratch the skin under the drops. This will help the solution get into your skin. If the skin becomes raised, red, and itchy within 20 minutes, you may be allergic to that allergen.
How is angioedema treated?
Angioedema usually goes away within 3 days without treatment, but it may come back. You may need any of the following:
- Antihistamines decrease symptoms such as itching or a rash.
- Epinephrine is medicine used to treat severe allergic reactions such as anaphylaxis.
- Steroids may be given to decrease inflammation.
Treatment options
The following list of medications are in some way related to or used in the treatment of this condition.
- danazol
- Danocrine
What steps do I need to take for signs or symptoms of anaphylaxis?
- Immediately give 1 shot of epinephrine only into the outer thigh muscle.
- Leave the shot in place as directed. Your healthcare provider may recommend you leave it in place for up to 10 seconds before you remove it. This helps make sure all of the epinephrine is delivered.
- Call 911 and go to the emergency department, even if the shot improved symptoms. Do not drive yourself. Bring the used epinephrine shot with you.
What safety precautions do I need to take if I am at risk for anaphylaxis?
- Keep 2 shots of epinephrine with you at all times. You may need a second shot, because epinephrine only works for about 20 minutes and symptoms may return. Your healthcare provider can show you and family members how to give the shot. Check the expiration date every month and replace it before it expires.
- Create an action plan. Your healthcare provider can help you create a written plan that explains the allergy and an emergency plan to treat a reaction. The plan explains when to give a second epinephrine shot if symptoms return or do not improve after the first. Give copies of the action plan and emergency instructions to family members, work and school staff, and daycare providers. Show them how to give a shot of epinephrine.
- Be careful when you exercise. If you have had exercise-induced anaphylaxis, do not exercise right after you eat. Stop exercising right away if you start to develop any signs or symptoms of anaphylaxis. You may first feel tired, warm, or have itchy skin. Hives, swelling, and severe breathing problems may develop if you continue to exercise.
- Carry medical alert identification. Wear medical alert jewelry or carry a card that explains the allergy. Ask your healthcare provider where to get these items.

- Keep a symptom diary. Include information on how often symptoms occur, how long they last, and if they are mild or severe. Also keep information on what you ate, what happened, or which medicines you took before the swelling started.
- Avoid triggers. Triggers include foods, medicines, and other items that you know cause symptoms. You may need to see a specialist, such as an allergist or dietitian, to learn what to avoid.
Call 911 for signs or symptoms of anaphylaxis,
such as trouble breathing, swelling in your mouth or throat, or wheezing. You may also have itching, a rash, hives, or feel like you are going to faint.
When should I seek immediate care?
- You have sudden behavior changes or irritability.
- You are dizzy and your heart is beating faster than usual.
When should I contact my healthcare provider?
- Your swelling does not improve, even after you take your medicines.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2023 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.