What is bronchiectasis?
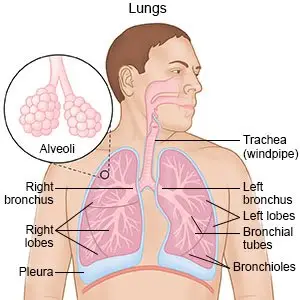
Bronchiectasis is a condition that causes mucus to collect in your airway. Chronic respiratory infections or inflammation cause the bronchi to become thick. Bronchi are larger airways that help carry air in and out of your lungs. Your lungs make mucus to trap and remove germs and irritants that you breathe. Bronchiectasis prevents your lungs from clearing the mucus. This leads to more infections and inflammation, and scarring in your lungs.
 |
What increases my risk for bronchiectasis?
You may have bronchiectasis with or without cystic fibrosis. Any of the following may increase your risk:
- A health condition you were born with that makes mucus difficult to clear, such as primary ciliary dyskinesia
- A respiratory infection when you were a child, such as measles or pertussis (whooping cough)
- Lung infections such as pneumonia, or breathing in harmful fumes
- A condition that causes inflammation, such as allergies, rheumatoid arthritis (RA), or inflammatory bowel disease (IBS)
- An obstruction, such as food that gets stuck in your airway or a tumor in your chest that grows large
- Gastroesophageal reflux (GER)
What are the signs and symptoms of bronchiectasis?
Periods of active signs and symptoms are called exacerbations.
- A chronic cough with mucus that may contain blood
- Wheezing or crackling, shortness of breath, or trouble breathing
- Foul-smelling mucus from your lungs
- Weakness and fatigue
- Clubbing of your fingers or toes
- Chest pain
How is bronchiectasis diagnosed?
Your healthcare provider will listen to your lungs and heart. He or she will ask about your other health conditions and any medicines you take. You may also need any of the following tests:
- A sputum (mucus) sample is collected in a cup when you cough. The sample is sent to a lab to find out if you have an infection.
- Bronchoscopy is done to look inside your airway and lungs. Healthcare providers insert a bronchoscope (a tube with a light on the end) into your mouth and down into your lungs. Healthcare providers may also collect samples of sputum, fluid, or cells from your lungs for testing. This may help find the cause of bronchiectasis or see if you have an infection.
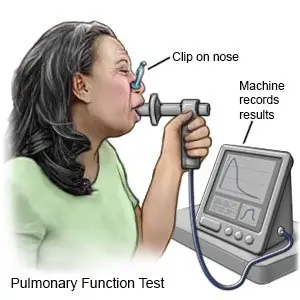
- Pulmonary function tests (PFTs) help healthcare providers learn how well your body uses oxygen. You breathe into a mouthpiece connected to a machine. The machine measures how much air you breathe in and out over a certain amount of time. PFTs help your healthcare providers decide the best treatment for you.
- X-ray or CT scan pictures are used to check your lungs and airway. You may be given contrast liquid to help these show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid.
How is bronchiectasis treated?
- Medicines may help relieve your symptoms. Bronchodilators help open the air passages in your lungs. Antibiotics may be used to treat an infection caused by bacteria. Steroids and some kinds of antibiotics help decrease inflammation in your airway. Medicines may help thin the mucus in your lungs. Thin mucus may be easier to cough up.
- Oxygen may be given to help you breathe easier. Oxygen can also decrease the strain on your heart and can help prevent more breathing problems.
- Surgery may be used to remove a part of your lung causing your symptoms. You may also need a lung transplant if your symptoms become severe. Surgery may also be needed to stop heavy bleeding in your airway if you cough up a lot of blood.
Treatment options
The following list of medications are in some way related to or used in the treatment of this condition.
- albuterol
- ProAir HFA
- Ventolin HFA
- Mucinex
- Ventolin
View more treatment options
How can I manage bronchiectasis?
- Go to pulmonary rehabilitation (rehab) as directed. Pulmonary rehab is a program that can help you learn how to manage bronchiectasis and prevent exacerbations. Your plan will include aerobic exercise, such as walking, swimming, or riding a bicycle. Regular exercise helps your lungs work well and helps keep your airway clear. Rehab can help you increase your ability to exercise for as long as recommended.
- Keep your airway clear and open. Do airway clearance techniques as needed. Healthcare providers will show you how to do these in pulmonary rehab. A saline nasal rinse can help clear irritants from your sinuses. Thin mucus by drinking more liquids or using a cool mist humidifier. Keep your head higher than your body when you sleep. If your bed is not adjustable, you can put extra pillows under your upper body to keep your head up.
- Do not smoke or be around anyone who is smoking. Nicotine and other chemicals in cigarettes and cigars can cause lung damage and make breathing problems worse. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
What can I do to prevent the spread of germs?
 |
- Wash your hands often. Wash your hands several times each day. Wash after you use the bathroom, change a child's diaper, and before you prepare or eat food. Use soap and water every time. Rub your soapy hands together, lacing your fingers. Wash the front and back of your hands, and in between your fingers. Use the fingers of one hand to scrub under the fingernails of the other hand. Wash for at least 20 seconds. Rinse with warm, running water for several seconds. Then dry your hands with a clean towel or paper towel. Use hand sanitizer that contains alcohol if soap and water are not available. Do not touch your eyes, nose, or mouth without washing your hands first.

- Cover a sneeze or cough. Use a tissue that covers your mouth and nose. Throw the tissue away in a trash can right away. Use the bend of your arm if a tissue is not available. Then wash your hands well with soap and water or use a hand sanitizer. Do not stand close to anyone who is sneezing or coughing.
- Stay away from anyone who is sick. Avoid crowds as much as possible. Ask anyone who is sick not to come to your home.
- Ask about vaccines you may need. Vaccines can help prevent some lung infections. Examples include pneumonia, pertussis (whooping cough), diphtheria, and influenza (flu). Get a flu vaccine every year as soon as recommended, usually starting in September or October. Your healthcare provider will tell you if you need other vaccines, and when to get them.
Call your local emergency number (911 in the US) if:
- You have sudden chest pain.
- You have sudden or more severe trouble breathing.
- You are confused or feel faint.
When should I call my doctor?
- Your lips or fingernails turn gray or blue.
- You cough up blood.
- You have a fever.
- You cough more than usual or wheeze.
- Your medicines do not relieve your symptoms.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2023 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.




