What is chronic kidney disease (CKD)?
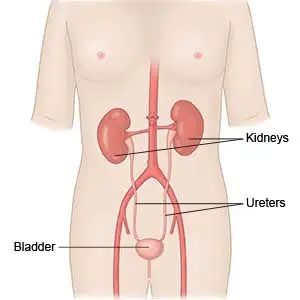
CKD is the gradual and permanent loss of kidney function. It is also called chronic kidney failure, or chronic renal insufficiency. Normally, the kidneys remove fluid, chemicals, and waste from your blood. These wastes are turned into urine by your kidneys. CKD may worsen over time and lead to kidney failure.
 |
What increases my risk for CKD?
- Diabetes or obesity
- High blood pressure or heart disease
- Kidney infections or kidney stones
- Autoimmune diseases, such as lupus
- An enlarged prostate
- NSAIDs, illegal drugs, or smoking
- Family history of kidney disease
What are the signs and symptoms of CKD?
Signs and symptoms depend on how well your kidneys work. You may not have symptoms, or you may have any of the following:
- Changes in how often you need to urinate
- Swelling in your arms, legs, or feet
- Shortness of breath
- Fatigue or weakness
- Bad or bitter taste in your mouth
- Nausea, vomiting, or loss of appetite
How is CKD diagnosed?
CKD has 5 stages. Your healthcare provider will use results from the following tests to find the stage of CKD you have:
- Blood and urine tests show how well your kidneys are working. They may also show the cause of your CKD.
- Ultrasound, CT scan, or MRI pictures may be used to check your kidneys. You may be given contrast liquid to help your kidneys show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
- A biopsy is a procedure to take tissue from your kidney. It is done to find the cause of your CKD.
How is CKD treated?
Treatment can help control signs and symptoms, and prevent a worse stage of CKD. Your care team may include specialists, such as a dietitian or a heart specialist. This depends on the stage of your CKD and if you have other health conditions to manage. Healthcare providers will work with you to create a plan based on your decisions for treatment. Your treatment plan may include any of the following:
- Medicines may be given to decrease your blood pressure and get rid of extra fluid. You may also receive medicine to manage health conditions that may occur with CKD, such as anemia, diabetes, and heart disease.
- Dialysis is a treatment to remove chemicals and waste from your blood when your kidneys can no longer do this.
- Surgery may be needed to create an arteriovenous fistula (AVF) in your arm or insert a catheter into your abdomen. This is done so you can receive dialysis.
- A kidney transplant may be done if your CKD becomes severe.
Treatment options
The following list of medications are in some way related to or used in the treatment of this condition.
- Farxiga
- Kerendia
- dapagliflozin
- finerenone
What can I do to manage CKD?
Management may include making some lifestyle changes. Tell your healthcare provider if you have any concerns about being able to make changes. He or she can help you find solutions, including working with specialists. Ask for help creating a plan to break large goals into smaller steps. Your plan may include any of the following:
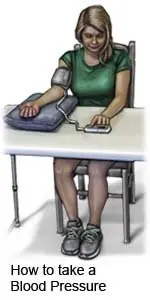
- Manage other health conditions. Your healthcare provider will work with you to make a care plan that meets your needs. You will be checked regularly for heart disease or other conditions that can make CKD worse, such as diabetes. Your blood pressure will be closely monitored. You will also get a target blood pressure and help making a plan to reach your target. This may include taking your blood pressure at home.
- Maintain a healthy weight. Your weight and body mass index (BMI) will be checked regularly. BMI helps find if your weight is healthy for your height. Your healthcare provider will use other tests to check your muscle and protein levels. Extra weight can strain your kidneys. A low weight or low muscle mass can make you feel more tired. You may have trouble doing your daily activities. Ask your provider what a healthy weight is for you. He or she can help you create a plan to lose or gain weight safely, if needed. The plan may include keeping a food diary. This is a list of foods and liquids you have each day. Your provider will use the diary to help you make changes, if needed. Changes are based on your health and any other conditions you have, such as diabetes.
- Create an exercise plan. Regular exercise can help you manage CKD, high blood pressure, and diabetes. Exercise also helps control weight. Your provider can help you create exercise goals and a plan to reach those goals. For example, your goal may be to exercise for 30 minutes in a day. Your plan can include breaking exercise into 10 minute sessions, 3 times during the day.
- Create a healthy eating plan. Your provider may tell you to eat food low in potassium, phosphorus, or protein. Your provider may also recommend vitamin or mineral supplements. Do not take any supplements without talking to your provider. A dietitian can help you plan meals if needed. Ask how much liquid to drink each day and which liquids are best for you.
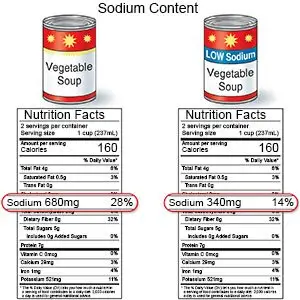
- Limit sodium (salt) as directed. You may need to limit sodium to less than 2,300 milligrams (mg) each day. Ask your dietitian or healthcare provider how much sodium you can have each day. The amount depends on your stage of kidney disease. Table salt, canned foods, soups, salted snacks, and processed meats, like deli meats and sausage, are high in sodium. Your provider or a dietitian can show you how to read food labels for sodium.
- Limit alcohol as directed. Alcohol can cause fluid retention and can affect your kidneys. Ask how much alcohol is safe for you. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause kidney damage. Ask your provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
- Ask about over-the-counter medicines. Medicines such as NSAIDs and laxatives may harm your kidneys. Some cough and cold medicines can raise your blood pressure. Always ask if a medicine is safe before you take it.
- Ask about vaccines you may need. CKD can increase your risk for infections such as pneumonia, influenza, and hepatitis. Vaccines lower your risk for infection. Your healthcare provider will tell you which vaccines you need and when to get them.
Call your local emergency number (911 in the US) if:
- You have a seizure.
- You have shortness of breath.
When should I seek immediate care?
- You are confused and very drowsy.
When should I call my doctor?
- You suddenly gain or lose more weight than your healthcare provider has told you is okay.
- You have itchy skin or a rash.
- You urinate more or less than you normally do.
- You have blood in your urine.
- You have nausea and are vomiting.
- You have fatigue or muscle weakness.
- You have hiccups that will not stop.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2023 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.