What is pleural effusion?
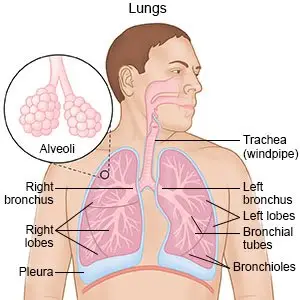
Pleural effusion is fluid buildup in the space between the layers of the pleura. The pleura is a thin piece of tissue with 2 layers. One layer rests directly on the lungs. The other rests on the chest wall. There is normally a small amount of fluid between these layers. This fluid helps your lungs move easily when you breathe.
 |
What causes pleural effusion?
- Heart and lung problems, such as heart failure or a pulmonary embolism (blockage of a blood vessel in the lungs)
- Lung infections such as bacterial pneumonia or tuberculosis (TB)
- Inflammation of the pleura (pleurisy), a trapped lung
- Problems with organs in your chest or abdomen, such as liver cancer, pancreatitis, or an injury
What are the signs and symptoms of pleural effusion?
- Cough, shortness of breath
- Breathing faster than usual
- Chest pain when you breathe in or cough
- Fever
How is pleural effusion diagnosed?
Your healthcare provider will examine you and listen to your heart and lungs through a stethoscope. You may need any of the following:
- Blood tests may show signs of an infection.
- An x-ray, ultrasound, or CT may show fluid around your lungs, an enlarged heart, or signs of infection. You may be given contrast liquid to help your lungs show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid.
- A thoracentesis is a procedure to take fluid out of your chest through a needle put between your ribs. The fluid may be sent to a lab for tests.
How is pleural effusion treated?
Treatment depends on the cause of your pleural effusion and your symptoms. You may need any of the following:
- Cardiac medicines may be needed if your pleural effusion is caused by heart failure.
- Antibiotics help treat an infection caused by bacteria.
- NSAIDs help decrease swelling and pain or fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Chemotherapy may be needed if your pleural effusion is caused by cancer.
- Steroids ,or other types of medicines, may be given to decrease swelling.
- Drainage of extra pleural fluid may be done using thoracentesis or a chest tube. A chest tube may stay in your chest for days or weeks. This allows the extra fluid around your lungs to drain over time. You may need medicines put directly into your chest if the fluid does not drain out easily.
- Surgery may be needed if your pleural effusion keeps coming back or if it increases your risk for other problems.
Treatment options
The following list of medications are in some way related to or used in the treatment of this condition.
- doxycycline
- Vibramycin
- Doryx
- Monodox
- Doxy 100
View more treatment options
How can I prevent another pleural effusion?
Maintain a healthy lifestyle:
- Eat a variety of healthy foods. Healthy foods help with overall health. Healthy foods include fruit, vegetables, whole-grain breads, low-fat dairy products, beans, lean meat, and fish. Limit sugar, alcohol, and fat.
- Do not smoke and do not allow others to smoke around you. Nicotine and other chemicals in cigarettes and cigars increase your risk for lung infections such as pneumonia. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Drink liquids as directed and rest as needed. Liquids help keep your air passages moist. This can help your body get rid of germs and other irritants. Ask your healthcare provider how much liquid to drink each day and which liquids are best for you. You may feel like resting more. Slowly start to do more each day. Rest when you feel it is needed.
- Exercise regularly. Ask about the best exercise plan for you. Exercise will lower your blood pressure and decrease stress. This helps decrease your risk for another pleural effusion, or a lung infection.
Call your local emergency number (911 in the US) if:
- You find it very hard to breathe.
- You feel faint, or you cannot think clearly.
When should I seek immediate care?
- Your breathing problems do not go away, or they get worse.
When should I call my doctor?
- Your lips or fingernails turn blue.
- You have a fever.
- Your pain does not go away or gets worse.
- You cough up yellow, green, gray, or bloody mucus.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2023 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.




