What is pulmonary edema?
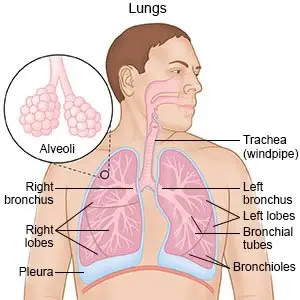
Pulmonary edema is a buildup of fluid in the alveoli (air sacs) of your lungs. The fluid may make it hard for you to breathe. Pulmonary edema may be life-threatening if your body is not able to get the oxygen it needs.
 |
What increases my risk for pulmonary edema?
- A heart condition, such as an abnormal heartbeat, damaged heart valve, heart attack, or heart failure
- Hypertension
- Diabetes, obesity, or a lack of physical activity
- Heavy alcohol use or smoking cigarettes
- Lung infection, injury, or a blocked airway
- Thoracentesis (a procedure to remove fluid from around your lung)
- Travelling to high altitudes, such as in the mountains
- A reaction to a blood transfusion
- Certain medicines, such as those used to treat inflammation, or use of illegal drugs
What are the signs and symptoms of pulmonary edema?
- A fever
- Wheezing, trouble breathing, or faster breathing than usual
- Chest discomfort or heaviness
- Coughing up pink, foamy sputum (spit)
- Fatigue or feeling the need to rest often
- Pale or blue nail beds and lips
- Fast heart rate or sweating for no known reason
- Anxiety
How is pulmonary edema diagnosed?
Your healthcare provider will ask about your signs and symptoms. Your provider will examine you, listen to your heart and lungs, and check your blood pressure. Tell your provider if you have any health conditions or take any medicines. You may also need the following tests:
- Blood tests may help find the cause of your symptoms. They may also be used to make sure organs, such as your kidneys, are working correctly.
- Blood gases may be checked if you are having trouble breathing. Blood is taken from an artery, usually in the wrist. Your blood is tested for the amount of oxygen and carbon dioxide in it. The results can tell healthcare providers how well your lungs are working.
- A chest x-ray may show signs of a lung infection or lung damage.
- An EKG records the electrical activity of your heart. It is used to see if a heart condition is the cause of your pulmonary edema.
- An echocardiogram shows the size and shape of your heart. Healthcare providers may check for problems with your heart valves and signs of heart failure. This may be done to find the cause of your pulmonary edema.
How is pulmonary edema treated?
Treatment will depend on what caused your pulmonary edema. If high altitude caused your pulmonary edema, your symptoms may go away when you go to a lower altitude. You may also need any of the following:
- Medicines may be given to remove extra fluid from around your lungs or decrease your blood pressure. Heart medicines may also be given to make your heartbeat stronger or more regular.
- Breathing support may help you breathe better and decrease the pressure in your lungs. You may need extra oxygen. You may also need to use a machine, such as a noninvasive positive-pressure ventilation (NPPV) or a ventilator. An NPPV is a machine that helps your lungs fill with air. A ventilator is a machine that can breathe for you if you cannot breathe well on your own.
Treatment options
The following list of medications are in some way related to or used in the treatment of this condition.
- furosemide
- Lasix
- Bumex
- Edecrin
- Sodium Edecrin
View more treatment options
How can I manage or prevent pulmonary edema?
- Limit liquids as directed. Follow your healthcare provider's directions about how much liquid you should drink each day. Too much liquid can increase your risk for fluid buildup.
- Weigh yourself daily. Weigh yourself at the same time every morning after you urinate, but before you eat. Weight gain can be a sign of extra fluid in your body.
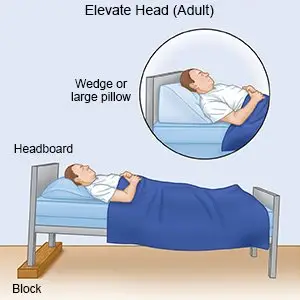
- Rest as needed. Return to activities slowly, and do more each day. You may have trouble breathing when you are lying down. Use foam wedges or elevate the head of your bed. This may help you breathe easier while you are resting or sleeping. Use a device that will tilt your whole body, or bend your body at the waist. The device should not bend your body at the upper back or neck.
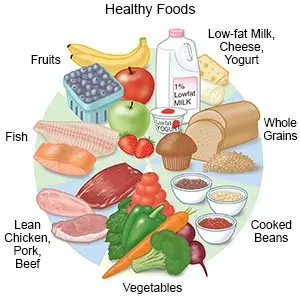
- Eat a variety of healthy foods. Healthy foods include fruits, vegetables, whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Healthy foods may decrease your symptoms and help you have more energy. Ask if you need to eat low-salt or low-fat foods.
- Limit or do not drink alcohol. You will need to limit the alcohol you drink, or avoid alcohol completely. Alcohol can worsen your symptoms and increase your blood pressure. If you have heart failure, alcohol can make it worse.
- Do not smoke cigarettes or use drugs. These can cause blood vessel and brain damage. Ask your provider for information if you currently use cigarettes or drugs and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
- Climb to high altitudes slowly. Go slowly to allow your body to get used to a higher altitude. Ask your healthcare provider about the symptoms of high altitude pulmonary edema (HAPE). Ask what to do if you have these symptoms.
Call your local emergency number (911 in the US) if:
- You are breathing very fast, sweating, and feel confused.
- You have chest pain or trouble breathing that gets worse.
When should I seek immediate care?
- Your heart feels like it skips a beat or flutters.
- You urinate very little or not at all.
- Your lips and nail beds are pale or blue.
When should I call my doctor?
- You have a fever.
- You gain weight for no known reason.
- You urinate more than usual.
- You have new or increased swelling in your legs or feet.
- You hear new or increased wheezing when you breathe.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2023 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.




