What are uterine fibroids?
Uterine fibroids are growths found inside your uterus. Uterine fibroids are benign (not cancer) and may also be called myomas or leiomyomas. Uterine fibroids often appear in groups, or you may have only one. They can be small or large, and they can grow. Fibroids likely will not spread to other parts of your body. They may grow when you are pregnant and shrink after you no longer have a monthly period.
 |
What increases my risk for uterine fibroids?
The cause of uterine fibroids is not clear. Ask your healthcare provider about these and other risk factors for uterine fibroids:
- A family history of uterine fibroids
- Increased hormone levels
- Menstrual periods starting before age 13
- Too much body weight
- Not having children
- Drinking alcohol
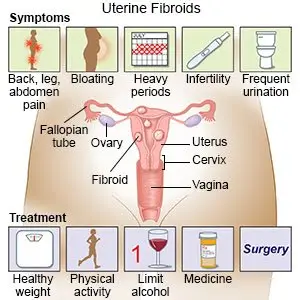
What are the signs and symptoms of uterine fibroids?
Symptoms depend on the size, type, and number of fibroids you have. Symptoms also depend on where the fibroids are inside your uterus:
- Heavy or painful menstrual bleeding that lasts more than 1 week
- Pelvic pressure and pain
- Urge to urinate often
- Constipation or pain when you have a bowel movement
- Increased pelvic pain during sex
How are uterine fibroids diagnosed?
Your healthcare provider will examine you and ask about your symptoms. Tell the provider if any women if your family have had uterine fibroids. You may also need any of the following:
- A pelvic exam is also called an internal or vaginal exam. During a pelvic exam, a speculum is gently placed into your vagina. A speculum is a tool that opens your vagina. This lets your provider see your cervix (bottom part of your uterus). With gloved hands, your provider will check the size and shape of your uterus and ovaries.
- An ultrasound uses sound waves to show pictures on a monitor. An ultrasound may be done to show your uterus and fibroids. The ultrasound device may be moved over your abdomen. Instead, the device may be placed in your vagina.
- A biopsy is a tissue sample of a fibroid that your healthcare provider takes from your uterus for testing.
How are uterine fibroids treated?
Watchful waiting may be recommended if your signs and symptoms are mild. The following treatments may shrink your fibroids and decrease your symptoms:
- Medicines:
- Medicines that decrease hormones may help shrink your fibroids and decrease menstrual bleeding.
- Oral contraceptives can help control menstrual bleeding.
- NSAIDs help decrease swelling and pain or fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- A procedure may be done to stop blood flow to the fibroids to help shrink them. This will help decrease your symptoms.
- Surgery may be used to remove your fibroids and leave your uterus in place. Surgery may instead be used to remove your fibroids and uterus.
Treatment options
The following list of medications are in some way related to or used in the treatment of this condition.
- Oriahnn
- Lupron Depot
- leuprolide
- Myfembree
- ulipristal
View more treatment options
How can I help prevent uterine fibroids?
- Maintain a healthy weight. Extra weight can increase your risk for fibroids. Talk to your healthcare provider about a healthy weight for you. Your provider can help you create a healthy weight loss plan, if needed.
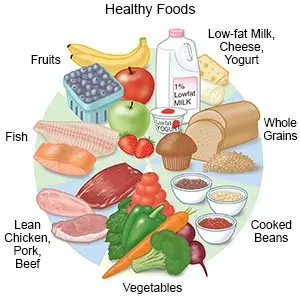
- Eat a variety of healthy foods. Fruits and vegetables are especially important to help lower the risk for fibroid. Other healthy foods include whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Your healthcare provider or a dietitian can help you create a healthy meal plan.
- Limit or do not drink alcohol, as directed. Alcohol can increase your risk for fibroids. A drink of alcohol is 12 ounces of beer, 1½ ounces of liquor, or 5 ounces of wine. Ask your healthcare provider for information if you need help to quit drinking alcohol.
When should I seek immediate care?
- Your heart begins to race, and you feel faint.
- You begin to pass large blood clots from your vagina.
When should I call my doctor or gynecologist?
- Your symptoms do not go away, or they get worse.
- You feel weak and are more tired than usual.
- You do not feel like your bladder is empty after you urinate. You also may urinate small amounts more often.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2023 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.




