Generic name: tezepelumab-ekko
Drug class: Selective immunosuppressants
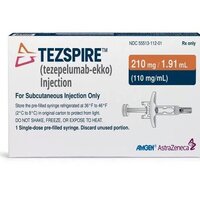
Dosage form: injection, solution
Availability: Prescription only
Pregnancy & Lactation: Risk data available
Brand names: Tezepelumab, Tezspire pre-filled pen, Tezspire pre-filled syringe
What is Tezspire?
Tezspire (Tezepelumab-ekko) is an add-on, injectable treatment that can be self-administered under the skin every 4 weeks for the maintenance treatment of severe asthma in people 12 years of age and older, whose asthma is not controlled with their current asthma medicine. It can help prevent severe asthma attacks and improve breathing but is not a rescue medication and will not relieve acute bronchospasm or status asthmaticus.
Airway inflammation is a significant component of Asthma. When you encounter a trigger, your lungs release multiple substances, including thymic stromal lymphopoietin (TSLP), a cytokine expressed mainly by epithelial cells, that is one of the first substances to be released. Tezspire blocks the action of TSLP, which reduces inflammation and prevents asthma attacks, although the exact way Tezspire works in asthma is not known.
Tezspire is a thymic stromal lymphopoietin (TSLP) blocker, human monoclonal antibody IgG2λ. It is the only biologic approved for severe asthma with no phenotype (ie, eosinophilic or allergic) or biomarker limitation within its approved label.
Tezspire was FDA approved on December 17, 2021.
Warnings
Tezspire may cause hypersensitivity reactions, such as a rash and allergic conjunctivitis) and severe reactions including anaphylaxis have also been reported. Appropriate treatment should be initiated if a reaction occurs.
Abrupt reductions in corticosteroid dosage may be associated with systemic withdrawal symptoms and/or unmask conditions previously suppressed by systemic corticosteroid therapy. Decrease corticosteroids gradually, if appropriate.
TSLP may be involved in the immunological response to some helminth (worm and parasitic) infections. Treat patients' pre-existing helminth infections before starting treatment with Tezspire. If a patient develops a helminth infection during treatment that does not respond, discontinue Tezspire until the infection resolves.
Avoid using live attenuated vaccines in patients receiving Tezspire.
Tell your healthcare provider if your asthma does not get better or if it gets worse after you start treatment with Tezspire.
It is not known if this medicine is safe and effective in children under 12 years of age.
How should I take Tezspire
- Your healthcare provider will give you Tezspire in a healthcare setting.
- Tezspire is injected under your skin (subcutaneously) 1 time every 4 weeks.
- If you miss an appointment, ask your healthcare provider when to schedule your next treatment.
Dosing information
Tezspire is available as a vial, a pre-filled syringe, and a prefilled pen. Each contains a single dose of Tezspire.
- The vial and pre-filled syringe are intended for administration by a healthcare provider. This will take place in their clinic or other suitable location.
- Tezspire pre-filled pens can be administered by patients, their caregivers, or by a healthcare provider. Proper training in the subcutaneous (under the skin) administration technique will be given to you by your healthcare provider if you wish to self-administer Tezspire or have your caregiver give it to you.
The usual dosage of Tezspire is 210mg (one vial/syringe/pen) administered under your skin (subcutaneously) once every 4 weeks.
Each Tezspire pre-filled pen contains 1 dose that can only be used 1 time. It can only be given as an injection under the skin (subcutaneous).
To use the Tezspire pen:
- Take it out of the refrigerator, and leave it in the carton and allow it to come to room temperature between 68°F to 77˚F (20°C to 25°C) for about 60 minutes before giving the injection. Do not remove the cap just yet.
- Do not warm the pre-filled pen in any other way. For example, do not warm it in a microwave or hot water, in direct sunlight, or near other heat sources.
- Do not put the injection back in the refrigerator after it has reached room temperature. Throw away (dispose of) Tezspire that has been stored at room temperature for more than 30 days.
- Check the pen for damage and check the expiry date. Do not use it if there is damage, the expiry date has passed, or if the solution looks cloudy, discolored, or contains large particles. The liquid should be clear and colorless to light yellow. Small air bubbles in the liquid are normal.
- Choose an injection site. If you are giving yourself the injection, the recommended site is the front of your thigh or the lower part of your stomach (abdomen). Do not inject yourself in the arm.
- A caregiver may inject you in the upper arm, thigh, or abdomen.
- For each injection, choose a different site that is at least 1 inch (3 cm) away from where you last injected.
- Do not inject:
- into the 2-inch (5 cm) area around your belly button
- where the skin is tender, bruised, scaly or hard
- into scars or damaged skin
- through clothing.
- Wash your hands well with soap and water and clean the injection site with an alcohol wipe. Let it air dry.
- Pull off the cap. You should see an orange needle guard. This is there to prevent you from touching the needle. Do not touch the needle or push on the orange needle guard with your finger.
- Follow your healthcare provider’s instructions on how to inject. You can either gently pinch the skin at the injection site or give the injection without pinching the skin.
- Inject Tezspire by holding it straight up and down (at a 90-degree angle) to your skin. Press down firmly so you cannot see the needle guard. You will hear the first click that tells you the injection has started. Press and hold the pre-filled pen for 15 seconds until you hear the second click.
- Do not change the position of the pre-filled pen after the injection has started.
- Once you have completed the injection, lift the pen straight up. The orange plunger should fill the viewing window. If it does not, contact your healthcare provider because you may not have received a full dose.
- Cover the injection site with a small bandage if needed. Do not rub the injection site. Dispose of the used pen in an FDA-approved sharps container.
Before Taking
You should not receive Tezspire if you are allergic to tezepelumab or any of the other ingredients. See the end of this page for a complete list of ingredients.
There is no available data on the use of Tezspire during pregnancy but it is known placental transfer of monoclonal antibodies such as tezepelumab-ekko is greater during the third trimester of pregnancy. Consider risks versus benefits including disease-associated maternal and/or embryo/fetal risk in women with poorly or moderately controlled asthma (such as increased risk of preeclampsia, and prematurity, low birth weight, and small for gestational age in the neonate.
There is no information regarding the presence of tezepelumab-ekko in human milk, its effects on the breastfed infant, or its effects on milk production.
Before receiving Tezspire
Before you receive Tezspire, tell your healthcare provider about all of your medical conditions, including if you:
- have ever had a severe allergic reaction (hypersensitivity) to tezepelumab-ekko or any of the ingredients in Tezspire
- have a parasitic (helminth) infection
- have recently received or are scheduled to receive any live attenuated vaccinations. People who receive Tezspire should not receive live attenuated vaccines
- are pregnant, think you may be pregnant, or plan to become pregnant. It is not known if Tezspire may harm your unborn baby
- are breastfeeding or plan to breastfeed. It is not known if Tezspire passes into your breast milk. Talk to your healthcare provider about the best way to feed your baby if you receive Tezspire.
What happens if I miss a dose?
If you miss an appointment, ask your healthcare provider when to schedule your next treatment.
If you are self-administering Tezspire and you miss a dose, inject the dose as soon as you can. Ring your healthcare provider for more information.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
Tezspire side effects
Tezspire may cause serious side effects, including:
- severe allergic reactions. Call your healthcare provider or get emergency medical care if you get any of the following symptoms of an allergic reaction:
- rash
- hives
- breathing problems
- red, itchy, swollen, or inflamed eyes.
The most common side effects occurring in more than 3% of people include:
- sore throat (pharyngitis)
- joint pain (arthralgia)
- back pain.
These are not all of the possible side effects. Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
See more: Tezspire Side EffectsWhat other drugs will affect Tezspire?
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Do not change or stop your corticosteroid medicines or other asthma medicines unless your healthcare provider tells you to.
No formal drug interaction studies have been performed with Tezspire. Refer to the product information for any updates.