What is chronic pancreatitis?

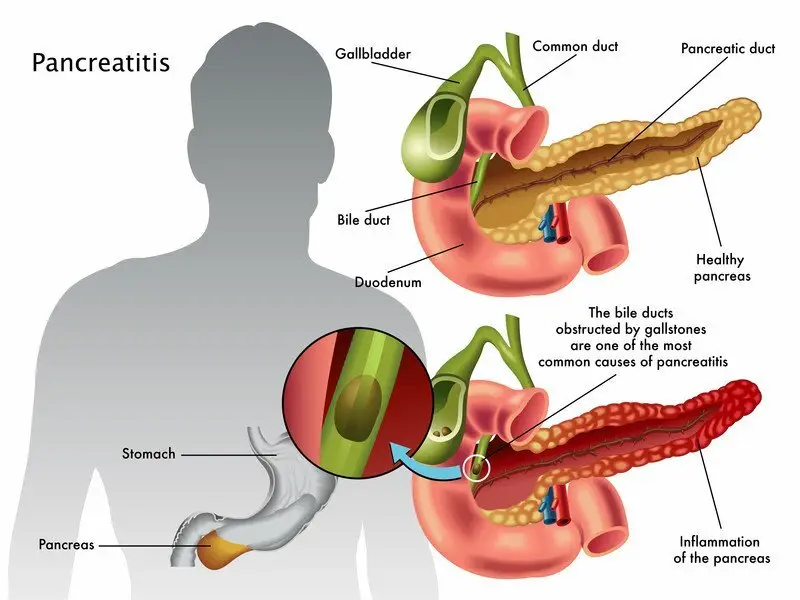
Pancreatitis is inflammation of the pancreas, a gland located behind the stomach. People with chronic pancreatitis have persistent inflammation of the pancreas that leads to permanent damage.
|
|
The main function of the pancreas is to produce digestive enzymes and hormones, such as insulin, that regulate blood sugar levels. Damage to the pancreas can cause problems with digestion, absorption of nutrients, and production of insulin. As a result, people with chronic pancreatitis can lose weight, experience diarrhea, become malnourished with vitamin deficiencies and develop diabetes.
It usually takes several years for permanent changes and symptoms to occur. Most cases of chronic pancreatitis are caused by long-standing over use of alcohol. Since only a small percent of people who over use alcohol develop chronic pancreatitis, there probably are other factors that influence whether someone develops chronic pancreatitis. It is generally thought that people who continue to drink after one or more bouts of alcohol-related acute pancreatitis are more likely to develop chronic pancreatitis.
In some uncommon cases, a single severe episode of acute pancreatitis can cause enough damage that the disease becomes chronic.
Besides over us of alcohol, other causes of chronic pancreatitis include:
- Heredity -- Hereditary chronic pancreatitis is a rare genetic disorder that predisposes a person to develop the disease, usually before age 20.
- Genetic causes -- Mutations of the cystic fibrosis gene is the most widely recognized genetic cause.
- Blockage of the duct that drains digestive enzymes from the pancreas --If the enzymes don't drain properly, they can back up and damage the pancreas. Blockage can be caused by gallstones, scarring from prior surgery, tumors, or abnormalities of the pancreas or of the shape or location of the pancreatic duct. If the blockage is found early, surgery or a procedure called endoscopic retrograde cholangiopancreatography (ERCP) to relieve the blockage may help to prevent damage to the pancreas.
- Autoimmune pancreatitis -- For unexplained reasons, some people develop antibodies that attack their own pancreas.
- Very high blood triglyceride levels
Sometimes the underlying cause of chronic pancreatitis cannot be identified.
Symptoms of chronic pancreatitis
The most common symptom is upper abdominal pain, which often radiates to the back and may be accompanied by nausea, vomiting and loss of appetite. The pain can occur daily or off and on, and can be mild or intense. As the disease gets worse and more of the pancreas is destroyed, pain may actually become less severe. During an attack, the pain often is made worse by drinking alcohol or eating a large meal high in fats.
Because a damaged pancreas can't produce important digestive enzymes, people with chronic pancreatitis may develop problems with digesting and absorbing food and nutrients. This can lead to weight loss, vitamin deficiencies, diarrhea and greasy, foul-smelling stools. Over time, a damaged pancreas also can fail to produce enough insulin, which results in diabetes.
Diagnosing chronic pancreatitis
There is no single test that can be used to diagnose chronic pancreatitis. If you have long-lasting abdominal pain or signs that your food is not being properly absorbed, such as weight loss or greasy stools, your doctor will ask you about alcohol use, and other factors that increase your risk of chronic pancreatitis and other digestive problems.
The diagnosis of chronic pancreatitis can be made based upon:
- Typical symptoms
- Imaging studies that show damage and scarring of the pancreas
- The absence of another medical problem, such as cancer, to explain your symptoms and test results
Tests that may be done include:
- Blood tests to check for high levels of two pancreatic enzymes, amylase and lipase. These enzymes typically are elevated in people with acute pancreatitis, but are often normal in people with chronic pancreatitis.
- A computed tomography (CT) scan, magnetic resonance imaging (MRI), or ultrasound to detect inflammation, scarring, and possible tumors of the pancreas.
- A test called endoscopic retrograde cholangiopancreatography (ERCP), in which the patient swallows a small tube with a camera at the end, which passes through the stomach and into the small intestine. At the site where the bile and pancreatic ducts empty into the small intestine, dye is injected through a small tube into the ducts, which then light up on an X-ray. This technique allows your physician to look for blockages or damage to the ducts. In chronic pancreatitis, the pancreatic duct can appear a certain way during ERCP.
- A noninvasive imaging test called magnetic resonance cholangiopancreatography (MRCP), which evaluates the ducts without requiring an endoscope or contrast material.
Treatment options
The following list of medications are in some way related to or used in the treatment of this condition.
- Creon
- Zenpep
- Pancreaze
- Viokace
- Pertzye
View more treatment options
Expected duration of chronic pancreatitis
Once the cells of the pancreas have been destroyed, they do not regenerate easily. For this reason, diabetes and other problems that are associated with chronic pancreatitis require long-term treatment. It is unclear why pain develops with chronic pancreatitis, but once chronic pain develops, it tends to be long-lasting or even lifelong. Many patients require long-term medications for pain.
Preventing chronic pancreatitis
Since most cases of chronic pancreatitis are associated with alcohol use, the best way to prevent the problem is to avoid or limit alcohol use. Anyone who has had an episode of alcohol-related acute pancreatitis should stop drinking entirely to lower the possibility of developing chronic pancreatitis. People who have been diagnosed with chronic pancreatitis can prevent further damage by eliminating alcohol use.
If blocked bile or pancreatic ducts can be opened by surgery or ERCP, it may prevent further damage to the pancreas. If caught early, scarring can be minimized. However, only a minority of people with chronic pancreatitis actually benefit from this procedure.
Treating chronic pancreatitis
Because chronic pancreatitis cannot be cured, treatment is directed toward relieving pain, improving food absorption, and treating diabetes.
For milder pain, medications such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin and others) may help. Pain management can be very challenging and often requires the help of a pain specialist.
In rare cases, surgery to open blocked ducts or remove part of the pancreas may be done to relieve pain.
Problems absorbing food, and the resulting vitamin deficiencies, can be helped by taking supplemental digestive enzymes in pill or capsule form. Your doctor also may recommend that you follow a low-carbohydrate, high-protein diet that also restricts some types of fats. Once digestive problems are treated, people often gain back weight and diarrhea improves.
Diabetes caused by chronic pancreatitis almost always requires treatment with insulin.
When to call a professional
See a health care provider if you have:
- Repeated episodes of abdominal pain or severe pain
- Unexplained weight loss or diarrhea
- Difficulty cutting back or stopping your alcohol use, especially if you have had a previous attack of acute pancreatitis
Prognosis
Although chronic pancreatitis is an incurable condition, the severity, frequency and type of symptoms can vary. Some people — especially those who quit drinking alcohol entirely — have very mild or occasional symptoms that are easily managed with medications. Other people — especially those who continue to drink alcohol — can have disabling, daily pain and may require frequent hospitalizations.
Additional Info
National Institute of Diabetes and Digestive and Kidney Disorders
https://www.niddk.nih.gov/
American College of Gastroenterology (ACG)
https://gi.org/
American Gastroenterological Association
https://www.gastro.org/