What is Multiple Sclerosis?
Multiple sclerosis (MS) is a neurological illness that affects the brain and spinal cord. Symptoms of the disease be intermittent (they come and go). Or MS can be progressive. This means it worsens over time.
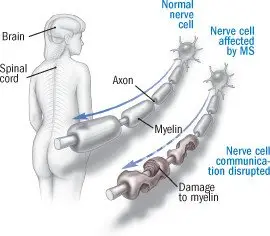
Nerve cells called neurons send out long "fingers" called axons. The axons from one neuron send signals to another neuron that may be a long ways away. A substance called myelin normally is wrapped around the axons. Myelin helps the axon transmit signals from one neuron to another.
In MS, inflammation damages both the neurons and the myelin. This disrupts or slows nerve signals. The inflammation also leaves areas of scarring called sclerosis.
|
|
The disruption of nerve signals causes a variety of symptoms. MS can affect a person's vision, ability to move parts of the body, and ability to feel sensations (such as pain and touch).
In a common type of MS, symptoms usually come and go. Periods when symptoms suddenly get worse are called relapses. They alternate with periods when symptoms improve, called remissions.
Many people have a long history of MS attacks over several decades. In these cases, the disease may worsen in "steps," when the attacks occur. For others, the disease worsens steadily. In a minority of patients, MS causes relatively few problems.
Scientists believe MS is an autoimmune disease. This means the immune system mistakenly attacks its own body. In this case, the body attacks the myelin sheaths of the nerves.
Several viruses have been linked to MS. But they are not proven causes of the disease. Fever, other physical or emotional stress may contribute to a flare-up of symptoms. The timing, duration and damage of MS attacks are unpredictable.
The symptoms of MS usually begin before age 40, but can first appear at an older age. Women are more likely than men to get MS. Having a close relative with MS increases your chances of developing the disease.
Symptoms
Symptoms of MS vary depending on which areas of the brain and spinal cord are affected.
MS can cause:
- Sudden loss of vision
- Blurred or double vision
- Slurred speech
- Clumsiness, especially on one side
- Unsteady gait
- Loss of coordination
- Hand trembling
- Extreme tiredness
- Facial symptoms including numbness, weakness or pain
- Loss of bladder control or inability to empty the bladder
- Tingling, numbness or a feeling of constriction in the arms, legs or elsewhere
- Weakness or a heavy feeling in the arms or legs
- Seizures (in about 2% of patients with MS)
Diagnosis
Your doctor will look for signs of neurological problems. These include:
- Decrease in the sharpness (acuity) of your vision
- Your eyes not working in a coordinated way
- Difficulty walking
- Difficulty coordinating body movements
- Muscle weakness on one side or in one part of your body
- Trembling hands
- Loss of sensation
To confirm the diagnosis, your doctor probably will order a magnetic resonance imaging (MRI) scan. The MRI can detect inflammation and myelin sheath destruction in your brain and spinal cord.
Other possible diagnostic tests include:
- A detailed eye examination by an ophthalmologist.
- Special tests called evoked potentials. These tests record electrical activity in the brain in response to stimuli, such as flashes of light.
- Lumbar puncture (spinal tap) to obtain spinal fluid. Spinal fluid may show abnormal types of immune system proteins called "oligoclonal bands". This is a characteristic finding in MS.
Expected Duration
MS is a lifelong illness. It can follow one of several different patterns.
The three most common patterns seen in MS patients are:
Relapsing remitting MS. There are relapses (episodes when symptoms suddenly get worse), followed by remissions (periods of recovery). Between relapses, the patient's condition usually is stable, without deterioration.
This type accounts for the vast majority of cases at disease onset. About half of people with relapsing remitting MS enter a secondary progressive phase (described below) over time.
Primary progressive MS. Symptoms worsen gradually and continuously. There are no episodes of relapses and remissions.
Secondary progressive MS. Someone who originally had relapsing remitting MS begins to have gradual deterioration in nerve function. This may occur with or without relapses. If relapses occur, it is called "progressive relapsing" MS.
Prevention
There is no way to prevent MS.
Treatment
There is no cure for MS.
There are two types of treatments. One type modifies the immune system to suppress the disease. The other type improves the symptoms of MS.
Symptoms of MS that can be improved with medication include:
- Fatigue – Feelings of overwhelming exhaustion are common in people with MS.
- Spasticity – Muscle tightness and spasms can be disabling for MS patients with spinal cord damage.
- Bladder dysfunction – Bladder dysfunction is common in patients with spinal cord damage from MS.
- Depression – This is a common problem for MS patients.
- Neurological symptoms – Anti-seizure medications decrease the risk of repeat seizures. They may also reduce other uncomfortable neurological symptoms that occur during MS attacks.
Treatments that suppress the disease include:
- Corticosteroid drugs – These are the primary treatment for MS relapses. They are often given directly into a vein. Corticosteroids appear to shorten the length of MS relapses and they may accelerate recovery in an attack. But their long-term effect on the course of the illness is not known.
- Plasma exchange (or plasmapheresis) – This is a procedure in which the liquid portion of the blood (plasma) is removed and replaced with plasma from blood donors or other plasma substitute. This may be recommended for flares of symptoms that do not improve rapidly with corticosteroid treatment.
- Interferon beta – This is used primarily to treat relapsing remitting MS. Different formulations of interferon beta are available, given as an injection either into the muscle or under the skin. Studies have shown that interferon beta may lower the rate of MS relapses. It may also reduce the risk of disease progression and disability.
- Glatiramer acetate (Copaxone) – This drug is an alternative treatment for relapsing remitting MS. Some physicians recommend this drug when interferon beta:
- Cannot be used
- Has been used but is no longer effective
- Is not tolerated well
Other experts prescribe it as initial therapy. It may be used in other patterns of MS. But its overall effectiveness for them is less clear.
- Natalizumab (Tysabri) – This treatment may be prescribed when other treatments fail or are not tolerated. The drug blocks immune cells coming from the blood to attack neurons from entering nervous system tissue. Rarely, natalizumab can cause a very serious complication: a degenerative and potentially fatal brain disease.
- Other immune-modifying medications – Other medications that may quiet the aggressive immune system attack on the neurons in MS include: fingolimod, teriflunomide, alemtuzumab, dimethyl fumarate, , laquinimod, and ocrelizumab.
The choice of treatment is a shared decision between you and your doctor and will depend on the type and severity of symptoms.
Treatment options
The following list of medications are in some way related to or used in the treatment of this condition.
- Copaxone
- Tecfidera
- Gilenya
- Aubagio
- Ocrevus
View more treatment options
When To Call a Professional
Call your doctor immediately if you have symptoms of MS.
Prognosis
A minority of people with MS have a relatively harmless form of the illness. But the majority of patients suffer from neurological disability over time.
MS is a progressive illness that can last for decades. The degree of progression and eventual disability varies from patient to patient.
Additional Info
National Multiple Sclerosis Society
http://www.nationalmssociety.org/
Multiple Sclerosis Foundation
http://msfocus.org/