What is it?

Testicular cancer is the uncontrolled growth of abnormal cells in one or both testicles (testes). The testicles are the male sex glands. They are located in the scrotum, behind the penis. They produce testosterone and other male hormones. The testicles also produce and store sperm, the male cells needed for reproduction.
nce testicular cancer develops, it can remain within the testicle, or it can spread to lymph nodes in the abdomen or pelvis. If it is not detected and treated, testicular cancer eventually can spread to the lungs, brain, liver, and other parts of the body. Certain types of testicular cancer are more likely to spread than others. Sometimes the cancer will have already spread at the initial time of diagnosis.
Most testicular cancer patients are between the ages of 20 and 40. Though testicular cancer accounts for a very small percentage of all cancer cases in men, it is the most common cancer in younger men.
Testicular cancer is more common in white men than in black men. Men who had an undescended testicle as infants have an increased risk for testicular cancer. (An undescended testicle is one that remains in the abdomen or groin instead of moving normally into the scrotum before or soon after birth.) Men who have cancer in one testicle have a small lifetime risk of developing it in the other one, whether or not they had an undescended testicle.
Other men also are at increased risk for testicular cancer, including men who have
-
close relatives who have had testicular cancer
-
an undeveloped testicle
-
been diagnosed as HIV positive
-
certain genetic conditions, such as Down syndrome or Klinefelter syndrome.
Some experts think that these conditions also increase risk:
-
mumps infection of the testicle
-
maternal exposure to diethylstilbestrol (DES), a drug previously prescribed to help treat nausea and vomiting during pregnancy
-
exposure to Agent Orange.
Sometimes, testicular cancer is found when a man is being evaluated for infertility.
The two main types of testicular tumors are germ cell tumors and tumors of supportive tissues, or stromal tumors. Nearly all testicular cancers start in germ cells. These are the cells that make sperm.
There are two types of germ cell tumors: seminomas and non-seminomas. Seminomas tend to grow slowly. These cancers usually stay within the testicles for a long time without spreading.
Non-seminomas form in more mature germ cells. They are more likely to spread, especially to lymph nodes. Lymph nodes are bean-shaped structures throughout the body that produce and store infection-fighting cells. The non-seminomas also can spread through the bloodstream to other organs, such as the lungs, liver or brain.
A small percentage of testicular cancers are tumors of supportive tissues. They begin in the tissues that support the testicles. These stromal cancers are called Sertoli cell tumors and Leydig cell tumors.
Symptoms
Most often, men notice a painless swelling or hardening of a testicle. It may be hard on one side, but not the other. Sometimes, men notice a painful lump in the scrotum.
Men also may notice breast enlargement (called gynecomastia). Rarely, a milky fluid may come out of the nipple. These two symptoms can occur with certain types of testicular cancers. The tumor can secrete hormones that stimulate growth of breast tissue and alter normal male hormone production.
Less common symptoms include
-
a lump in the neck
-
back pain that doesn’t go away
-
shortness of breath
-
coughing up blood
-
a breast lump
-
swollen glands at the base of the neck.
These less common symptoms tend to appear after the cancer has spread to other parts of the body.
Diagnosis
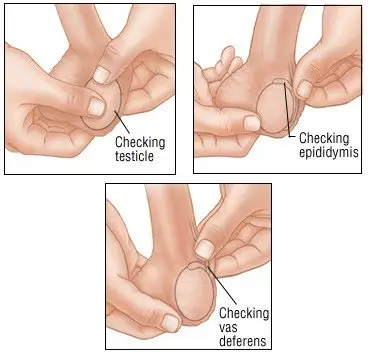
Your doctor will ask when you first noticed symptoms and whether they have worsened over time. He or she will examine the testicle and feel for swollen lymph nodes. Tell your doctor if you had an undescended testicle when you were born.
Your doctor may suspect that you have testicular cancer based on your symptoms or findings during the physical exam, such as a hard lump or area of tenderness. To determine whether a soft lump is solid or fluid filled, your doctor may shine a small flashlight on the lump to see if light travels through it.
|
|
The physical exam may be followed by
-
an ultrasound, which can be used to check for a mass or excess fluid inside the testicle.
-
magnetic resonance imaging (MRI) or computed tomography (CT) scans, which use magnetic fields or x-rays to create images of the abdomen. Your doctor will check the images for abnormal masses and enlarged lymph nodes.
-
a chest x-ray, to see whether the cancer has spread to the lungs.
If your doctor suspects that the testicle has turned and twisted off its blood supply (a testicular torsion), a special type of imaging scan may be done emergently.
The best way to confirm the diagnosis of testicular cancer is to remove the testicle. This procedure is called an orchiectomy. The testicle will then be examined in a laboratory to determine whether cancer is present, and if so, what type. Blood tests also will be done to measure levels of tumor-marker proteins. These include
-
alpha-fetoprotein (AFP)
-
beta-human chorionic gonadotropin (beta-hCG)
-
lactic dehydrogenase (LDH).
-
placental alkaline phosphatase
Expected Duration
In many men, testicular cancer develops slowly and may remain undetected for years. More often, testicular cancer grows rapidly and needs treatment right away.
Like all cancers, testicular cancer will continue to grow and possibly spread until it is treated.
Prevention
There is no way to prevent most cases of testicular cancer.
Men who had an undescended testicle at birth should be monitored regularly for early signs of cancer. Most pediatricians recommend surgery to lower an undescended testicle into the scrotum at a very early age. If the testicle did not even begin its descent into the scrotum, some pediatricians recommend removing it. These "abdominal testes" are more likely to become cancerous over time.
Treatment
Treatment depends on the patient’s overall health, the type of testicular cancer, and its stage, a measure of how far the cancer has spread. The stages of testicular cancer are
-
Stage I. Cancer is found only in the testicle.
-
Stage II. Cancer has spread to nearby lymph nodes in the abdomen or pelvis.
-
Stage III. Cancer has spread to the lungs, brain, liver, or other parts of the body. Or, cancer has spread to nearby lymph nodes and levels of tumor-marker proteins in the blood are quite high.
-
Recurrent. Cancer has returned after treatment.
The treatment for all types and stages of testicular cancer is to remove the testicle. During this procedure, the surgeon removes the testicle through an incision in the groin. Both before the surgery and a few weeks afterward, blood tests will be done to measure levels of tumor markers. Some men will need additional surgery to see whether the cancer has spread to lymph nodes in the abdomen or pelvis.
After surgery, the treatment of testicular cancer depends on the cancer’s stage. Some men will need only regular monitoring. This is called active surveillance. It’s mandatory that the patient return on a very regular basis if this approach is used.
However, most men will need additional treatment, such as radiation or chemotherapy. Radiation can be directed at the lymph nodes to destroy any bits of cancer that can’t be seen. Radiation therapy is often used in the treatment of seminomas.
Chemotherapy is used when cancer has spread beyond the testicle. It can also help keep the cancer from coming back. Typically seminomas don’t require chemotherapy. But it may be used in special circumstances.
In general, patients with seminomas often receive radiation therapy. Radiation therapy doesn’t work as well in patients with non-seminomas. Instead, they tend to undergo surgery to remove cancerous masses after the removal of the testicle and chemotherapy.
After treatment, regular follow-up exams are critical to make certain that the cancer is gone. For the first two years, a man is examined every one to two months. Blood tests, x-rays and CT scans are also done. After that, physical exams and blood tests are done a little less often, with x-rays happening only once or twice a year.
Review your treatment options with an expert in the treatment of testicular cancer. Make sure you understand all of the choices before making a treatment decision.
When To Call a Professional
Contact your doctor if you discover a lump on one or both testicles or in the scrotum. You should also call your doctor if you develop persistent pain or swelling of either testicle. You should also notify a professional if you develop any breast enlargement or have any discharge from the nipple.
Because testicular cancer is so rare, many doctors may never treat a patient with the disease. That’s why patients who have been diagnosed with testicular cancer should be treated at a large cancer center where the staff is expert in evaluating and caring for men with this condition. Doctors who use chemotherapy and/or radiation to treat testicular cancer need special skills and knowledge to treat the disease safely and effectively. Experience counts.
Prognosis
Testicular cancer usually can be cured if it is detected and treated early. However, this cancer can spread silently and quickly. This means that some men will not be diagnosed until the disease is in an advanced stage.
At one time, testicular cancer could not be cured if it had spread beyond the testicles. Now, testicular cancer is one of the most curable cancers. Today’s chemotherapies can shrink and eliminate the cancer cells that have spread to other areas of the body.
Most men with testicular cancer have an excellent prognosis. Men with Stage I disease are very likely to be cured with surgery and radiation therapy. Men with Stage II disease have a very good prognosis following surgery and radiation or chemotherapy. Even men with the most advanced cases have a fair prognosis: More than half of them will be alive five years later.
People who have been cured of testicular cancer involving one testicle have a small risk of developing cancer in the other testicle at some point in their lives. There can also be some long term complications of the chemotherapy and radiation. They can occur many years after the cancer has been treated. These include damage to nerves, kidneys, and the heart. Abnormalities of the blood, including leukemia can also occur years following treatment. Hearing loss is also possible.
If patients have been treated with either radiation or chemotherapy, they will need life-long followup for the potential development of these complications.
Additional Information
National Cancer Institute (NCI)
https://www.cancer.gov/
American Cancer Society (ACS)
https://www.cancer.org/