What is Thyroid Cancer?

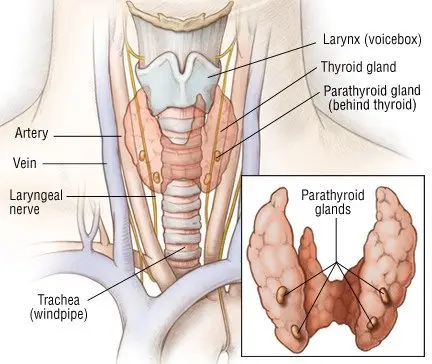
Thyroid cancer is the uncontrolled growth of abnormal cells in the thyroid gland. The thyroid gland is shaped like a butterfly. It is located under the Adam's apple in the front of the neck. Most cases of thyroid cancer can be cured.
One of the functions of the thyroid gland is to make thyroid hormone, which requires iodine. The gland collects iodine from foods, concentrates it, and produces thyroid hormone. Doctors often exploit this important function when treating thyroid cancer.
Thyroid hormone helps regulate the body's metabolism and energy level. An overactive thyroid can lead to hyperactivity, the "jitters," and an irregular heart rhythm; an underactive thyroid, fatigue and sluggishness. Cancer can affect the thyroid and cause these changes.
Nestled against the thyroid gland are four very small glands called parathyroid glands. They play a role in regulating the body's use of calcium. The nerve that controls the voice box is also very close to the thyroid. If you need a thyroid operation, your surgeon needs to identify and avoid damaging these structures. If the voice box nerve is damaged, for example, your voice may sound hoarse permanently.
|
|
The thyroid has two types of cells. They produce hormones that help regulate body functions:
- Follicular cells produce a thyroid hormone called thyroxine, or T-4. It controls the body's metabolism and may affect the function of various organs.
- C-cells, also called parafollicular cells, produce calcitonin. This hormone helps regulate the level of calcium in the blood.
There are five types of thyroid cancers:
- Papillary carcinoma (papillary adenocarcinoma) — This is the most common type of thyroid cancer, accounting for 75 percent of thyroid cancers. It develops from follicular cells and usually grows slowly. In most cases, the cancer only affects one of the thyroid gland's two lobes, but it can affect both. Papillary carcinoma often spreads to nearby lymph nodes in the neck. It can also spread to other parts of the body.
- Follicular carcinoma — The second-most-common type of thyroid cancer, follicular carcinoma starts in follicular cells. It often affects just the thyroid gland, but it can spread to other parts of the body, especially the lungs and bone. Only about one-third of tumors beginning in follicular cells are cancerous. Some thyroid cancers are mixtures of papillary and follicular cells.
- Hürthle cell neoplasm (follicular adenocarcinoma) — This poorly understood cancer seems similar to follicular carcinoma.
- Anaplastic carcinoma (undifferentiated thyroid cancer) — This is the rarest form of thyroid cancer, and it has the worst prognosis. Scientists believe that it develops from existing papillary or follicular carcinoma. Anaplastic carcinoma is aggressive, spreading quickly to other parts of the body. Because the thyroid is so close to the wind pipe (trachea), patients with this type of cancer may experience sudden shortness of breath. They may need to have a tube inserted into the windpipe to help them breathe.
- Medullary thyroid carcinoma (MTC) — This is the only type of thyroid cancer that develops from the C-cells. It can spread to the lymph nodes, the lungs, and the liver before an abnormal lump in the thyroid has even been detected. MTC produces the hormone calcitonin, as well as a protein called carcinoembryonic antigen (CEA). Both of these chemicals are released into the blood. There are two main types of MTC: Sporadic MTC (80 percent of all MTC cases) is not inherited. It usually develops in only one thyroid lobe. Familial MTC (20 percent of cases) can affect several generations of the same family.
Rarely, tumors arising from connective tissue (sarcomas) and lymph nodes (lymphomas) can start in the thyroid gland. They are treated differently than other thyroid cancers.
Although scientists have not identified the exact cause of thyroid cancer, some studies have shown that people exposed to nuclear fallout or nuclear power plant accidents have a higher risk of developing thyroid cancer. In part, this is due to the presence of radioactive iodine. Because the thyroid has an attraction for iodine, the thyroid tissue accumulates this radioactive substance. Over time, it may cause cancer.
Others who have a higher risk of thyroid cancer include people who
- received high-dose radiation for acne or swollen adenoids as a child
- have a diet that's very low in iodine
- have certain medical conditions, such as Cowden's disease and familial polyposis.
Individuals who have received radiation therapy to the chest (to treat Hodgkin's disease, for example) have an increased incidence of thyroid abnormalities, including cancer. This is even more likely if the thyroid was included in the radiation field. Such people will need life-long follow up to assess thyroid function and check for cancer.
Some forms of thyroid cancer are inherited. These occur alone (inherited MTC) or as part of a familial cancer syndrome known as multiple endocrine neoplasia (MEN) type 2. Patients with MEN-2 develop tumors in other parts of the body, such as the adrenal gland and peripheral nervous system.
Some forms of thyroid cancer may be caused by genetic changes (mutations) that occur after birth.
Thyroid cancer is rare, accounting for only a small percentage of all cancers. However, it does strike more women than men.
Symptoms
Usually, a lump in the neck is the only symptom of thyroid cancer. When other symptoms occur, they may include
- pain in the neck that may shoot up into the ears
- difficulty swallowing
- hoarseness
- difficulty breathing
- a persistent cough.
Often, a patient has no symptoms; the disease is diagnosed based on a test performed for another reason.
Having some of these symptoms does not mean you have thyroid cancer. Symptoms can be caused by other conditions. If you have symptoms, see your doctor so that the problem can be diagnosed and treated.
Diagnosis
Your doctor will examine you, feeling your neck to evaluate the size and firmness of the thyroid and to check for lumps and enlarged lymph nodes. Your doctor also may order the following tests and procedures:
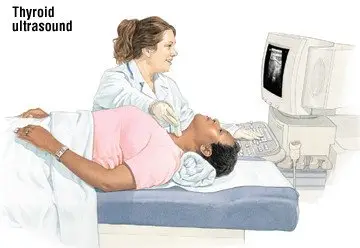
- Thyroid ultrasound — In this test, sound waves, not x-rays, create images of the thyroid. The pictures can help your doctor determine whether a lump is a cyst or a tumor.
|
|
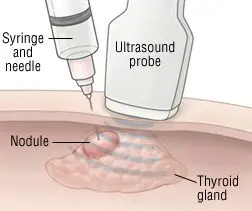
- Fine-needle aspiration (FNA) of a thyroid nodule — If your doctor finds a thyroid nodule in your neck, he or she can determine if it is cancerous by doing an FNA. During this procedure, he or she injects a local anesthetic to numb the skin over the nodule. Next, he or she inserts a thin needle into the nodule to withdraw cells and fluid. These samples are sent to a laboratory and examined under a microscope. In most cases, FNA shows that the nodule is not cancerous (benign). Only a small percentage FNA samples are cancerous. In some cases, the findings are suspicious, meaning that cancer may be present.
|
|
- Blood calcitonin test — Your doctor will order this test if he or she suspects MTC.
- Thyroid scan — For this test, you swallow a small amount of a radioactive substance or have it injected into a vein. Your thyroid gland soaks up the chemical. A special camera positioned next to your neck measures the amount of radioactive chemicals in the thyroid. These scans can help doctors to determine whether a nodule in the gland is actively producing thyroid hormone. If it is producing the hormone, cancer is less likely. If you have thyroid cancer, this test may determine whether it has spread to other parts of your body, especially after the thyroid gland has been removed surgically.
- Computed tomography (CT) or magnetic resonance imaging (MRI) — CT uses a modified x-ray beam to make cross-sectional images of the thyroid gland and nearby structures. MRI also creates cross-sectional, computer-generated images of the thyroid gland and nearby structures, but it uses large magnets and radio waves, not x-rays.
CT scans have become a common way to assess many medical conditions. Because the neck is imaged as part of an abdominal scan, thyroid cancer may be detected even though the test was done for another reason.
Expected Duration
Thyroid cancer can develop slowly, remaining undetected for years. Like other cancers, it will continue to grow until treated.
Prevention
Many people have no risk factors for thyroid cancer but develop it anyway. That's why this cancer usually can't be prevented.
However, genetic blood tests can be used to identify people who have a high risk of developing the familial types of MTC. When inherited MTC strikes one family member, all family members can be tested. Those who test positive but have no symptoms of thyroid cancer may decide to have their thyroid removed to prevent the disease. After surgery, these patients need to take thyroid hormones for the rest of their lives.
Treatment
Surgery is the most common treatment for thyroid cancer. Your surgeon will remove all of the cancer, as well as all or part of the remaining thyroid and nearby lymph nodes.
The treatment of thyroid cancer also is determined by the type of cells that make up the cancer.
Your treatment plan may also include:
- Thyroid hormone therapy — If your entire thyroid gland is removed, taking thyroid hormone medication will help restore your normal metabolism. It also helps suppress a hormone from the pituitary gland that can speed the growth of any remaining cancer cells. You will need to take this medication for the rest of your life.
- Radioactive iodine treatment — Radioactive iodine can be used after thyroid surgery to destroy any remaining normal thyroid tissue. It can also be used to kill any remaining cancer cells or to treat cancer that has returned. When used to destroy normal tissue, you can be treated as an outpatient with relatively low levels of radiation. To kill cancer cells, doctors use much larger doses; treatment often takes place in a hospital.
- Chemotherapy — In this treatment, anticancer drugs are taken by mouth or injected into a vein. Side effects can include hair loss, nausea, and vomiting. Chemotherapy is used to treat more aggressive thyroid cancers, as well as those that are advanced.
- External beam radiation therapy — In this treatment, high-energy beams of radiation are directed at the cancer to kill cancer cells.
A serum thyroglobulin blood test is done routinely after treatment to determine if any active thyroid tissues, including cancerous thyroid cells, are still present.
Your treatment plan will depend on the type of thyroid cancer you have and how far it has spread. Each treatment causes side effects that can linger for a few months. Follow-up care can continue for decades.
Treatment options
The following list of medications are in some way related to or used in the treatment of this condition.
- Armour Thyroid
- Retevmo
- Nexavar
- Caprelsa
- Thyrogen
View more treatment options
When To Call a Professional
Contact your doctor if you discover a lump in your neck. Also seek medical help if you have
- neck pain that doesn't go away
- a persistent cough
- trouble breathing or swallowing.
Prognosis
Thyroid cancer usually can be cured if it is found early. The outlook depends on your age, the type of cancer, the tumor's characteristics, whether the cancer has spread, and whether it was completely removed. The prognosis for MTC depends on whether the cancer occurs with no known cause, is inherited alone, or is inherited as part of a cancer syndrome (MEN-2). Regular follow-up exams are critical because the cancer can come back.
Anaplastic carcinoma is nearly always fatal. Only a small percentage of patients survive five years or longer.
Additional Information
American Cancer Society (ACS)
http://www.cancer.org/
National Cancer Institute (NCI)
http://www.cancer.gov/
American Thyroid Association
http://www.thyroid.org/