Drug Detail:Pradaxa (Dabigatran [ da-big-a-tran ])
Drug Class: Thrombin inhibitors
Highlights of Prescribing Information
PRADAXA® (dabigatran etexilate) capsules, for oral use
Initial U.S. Approval: 2010
WARNING: (A) PREMATURE DISCONTINUATION OF PRADAXA INCREASES THE RISK OF THROMBOTIC EVENTS, and (B) SPINAL/EPIDURAL HEMATOMA
See full prescribing information for complete boxed warning
(A) PREMATURE DISCONTINUATION OF PRADAXA INCREASES THE RISK OF THROMBOTIC EVENTS: Premature discontinuation of any oral anticoagulant, including PRADAXA, increases the risk of thrombotic events. To reduce this risk, consider coverage with another anticoagulant if PRADAXA is discontinued for a reason other than pathological bleeding or completion of a course of therapy (2.6, 2.7, 2.8, 5.1).
(B) SPINAL/EPIDURAL HEMATOMA: Epidural or spinal hematomas may occur in patients treated with PRADAXA who are receiving neuraxial anesthesia or undergoing spinal puncture. These hematomas may result in long-term or permanent paralysis (5.3). Monitor patients frequently for signs and symptoms of neurological impairment and if observed, treat urgently. Consider the benefits and risks before neuraxial intervention in patients who are or who need to be anticoagulated (5.3).
Recent Major Changes
| Indications and Usage (1) | 06/2021 |
| Dosage and Administration (2) | 06/2021 |
Indications and Usage for Pradaxa
PRADAXA Capsules is a direct thrombin inhibitor indicated:
- To reduce the risk of stroke and systemic embolism in adult patients with non-valvular atrial fibrillation (1.1)
- For the treatment of deep venous thrombosis (DVT) and pulmonary embolism (PE) in adult patients who have been treated with a parenteral anticoagulant for 5-10 days (1.2)
- To reduce the risk of recurrence of DVT and PE in adult patients who have been previously treated (1.3)
- For the prophylaxis of DVT and PE in adult patients who have undergone hip replacement surgery (1.4)
- For the treatment of venous thromboembolic events (VTE) in pediatric patients 8 to less than 18 years of age who have been treated with a parenteral anticoagulant for at least 5 days (1.5)
- To reduce the risk of recurrence of VTE in pediatric patients 8 to less than 18 years of age who have been previously treated (1.6)
Pradaxa Dosage and Administration
-
Non-valvular Atrial Fibrillation in Adult Patients:
- For patients with CrCl >30 mL/min: 150 mg orally, twice daily (2.2)
- For patients with CrCl 15-30 mL/min: 75 mg orally, twice daily (2.2)
-
Treatment of DVT and PE in Adult Patients:
- For patients with CrCl >30 mL/min: 150 mg orally, twice daily after 5-10 days of parenteral anticoagulation (2.2)
-
Reduction in the Risk of Recurrence of DVT and PE in Adult Patients:
- For patients with CrCl >30 mL/min: 150 mg orally, twice daily after previous treatment (2.2)
-
Prophylaxis of DVT and PE Following Hip Replacement Surgery in Adult Patients:
- For patients with CrCl >30 mL/min: 110 mg orally first day, then 220 mg once daily (2.2)
-
Treatment of Pediatric VTE:
- For pediatric patients: weight-based dosage, twice daily after at least 5 days of parenteral anticoagulant (2.3)
-
Reduction in the Risk of Recurrence of Pediatric VTE:
- For pediatric patients: weight-based dosage, twice daily after previous treatment (2.3)
- Pradaxa Capsules are NOT substitutable on a milligram-to-milligram basis with other dabigatran etexilate dosage forms
- Review recommendations for converting to or from other oral or parenteral anticoagulants (2.6, 2.7)
- Temporarily discontinue PRADAXA before invasive or surgical procedures when possible, then restart promptly (2.8)
Dosage Forms and Strengths
Capsules: 75 mg, 110 mg and 150 mg (3)
Contraindications
- Active pathological bleeding (4)
- History of serious hypersensitivity reaction to PRADAXA (4)
- Mechanical prosthetic heart valve (4)
Warnings and Precautions
- Bleeding: PRADAXA can cause serious and fatal bleeding (5.2)
- Bioprosthetic heart valves: PRADAXA use not recommended (5.4)
- Increased Risk of Thrombosis in Patients with Triple-Positive Antiphospholipid Syndrome: PRADAXA use not recommended (5.6)
Adverse Reactions/Side Effects
Most common adverse reactions (>15%) are gastrointestinal adverse reactions and bleeding (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Boehringer Ingelheim Pharmaceuticals, Inc. at (800) 542-6257 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
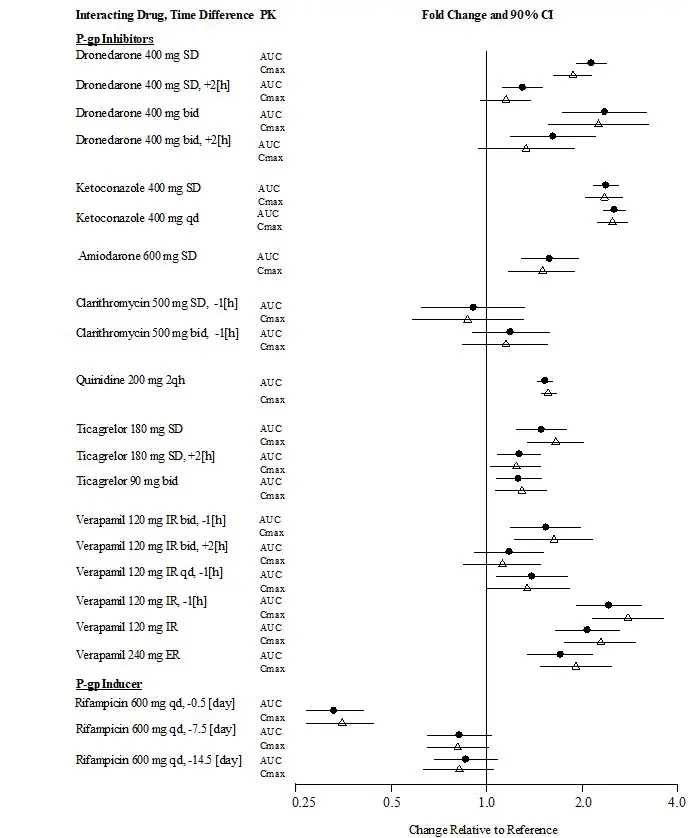
- P-gp inducers: Avoid coadministration with PRADAXA (5.5)
- P-gp inhibitors in adult patients with CrCl 30-50 mL/min: Reduce dose or avoid (7)
- P-gp inhibitors in adult patients with CrCl <30 mL/min: Not recommended (7)
Use In Specific Populations
- Lactation: Breastfeeding not recommended (8.2)
- Geriatric Use: Risk of bleeding increases with age (8.5)
See 17 for PATIENT COUNSELING INFORMATION and Medication Guide.
Revised: 6/2021
Related/similar drugs
aspirin, Eliquis, warfarin, apixaban, Xarelto, enoxaparin, rivaroxabanFull Prescribing Information
WARNING: (A) PREMATURE DISCONTINUATION OF PRADAXA INCREASES THE RISK OF THROMBOTIC EVENTS, and (B) SPINAL/EPIDURAL HEMATOMA
1. Indications and Usage for Pradaxa
1.1 Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult Patients
PRADAXA Capsules is indicated to reduce the risk of stroke and systemic embolism in adult patients with non-valvular atrial fibrillation.
1.2 Treatment of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
PRADAXA Capsules is indicated for the treatment of deep venous thrombosis and pulmonary embolism in adult patients who have been treated with a parenteral anticoagulant for 5-10 days.
1.3 Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
PRADAXA Capsules is indicated to reduce the risk of recurrence of deep venous thrombosis and pulmonary embolism in adult patients who have been previously treated.
1.4 Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism in Adult Patients Following Hip Replacement Surgery
PRADAXA Capsules is indicated for the prophylaxis of deep vein thrombosis and pulmonary embolism, in adult patients who have undergone hip replacement surgery.
1.5 Treatment of Venous Thromboembolic Events in Pediatric Patients
PRADAXA Capsules is indicated for the treatment of venous thromboembolic events (VTE) in pediatric patients 8 to less than 18 years of age who have been treated with a parenteral anticoagulant for at least 5 days (see Dosage and Administration [2.3]).
2. Pradaxa Dosage and Administration
2.1 Important Dosage Information
Dabigatran etexilate is available in different dosage forms and not all dosage forms are approved for the same indications and age groups. In addition, there are differences between the dosage forms with respect to dosing due to differences in bioavailability. Do not substitute different dosage forms on a milligram-to-milligram basis and do not combine more than one dosage form to achieve the total dose [see Clinical Pharmacology (12.3)].
2.2 Recommended PRADAXA Capsules Dose for Adults
| Indication | Dosage | |
|---|---|---|
| Reduction in Risk of Stroke and Systemic Embolism in Non-valvular AF | CrCl >30 mL/min: | 150 mg twice daily |
| CrCl 15 to 30 mL/min: | 75 mg twice daily | |
| CrCl <15 mL/min or on dialysis: | Dosing recommendations cannot be provided | |
| CrCl 30 to 50 mL/min with concomitant use of P-gp inhibitors: | Reduce dose to 75 mg twice daily if given with P-gp inhibitors dronedarone or systemic ketoconazole. | |
| CrCl <30 mL/min with concomitant use of P-gp inhibitors: | Avoid coadministration | |
| Treatment of DVT and PE | CrCl >30 mL/min: | 150 mg twice daily |
| Reduction in the Risk of Recurrence of DVT and PE | CrCl ≤30 mL/min or on dialysis: | Dosing recommendations cannot be provided |
| CrCl <50 mL/min with concomitant use of P-gp inhibitors: | Avoid coadministration | |
| Prophylaxis of DVT and PE Following Hip Replacement Surgery | CrCl >30 mL/min: | 110 mg for first day, then 220 mg once daily |
| CrCl ≤30 mL/min or on dialysis: | Dosing recommendations cannot be provided | |
| CrCl <50 mL/min with concomitant use of P-gp inhibitors: | Avoid coadministration | |
2.3 Recommended PRADAXA Capsules Dose for Pediatrics
PRADAXA Capsules can be used in pediatric patients aged 8 to less than 18 years of age who are able to swallow the capsules whole. Other age-appropriate pediatric dosage forms of dabigatran etexilate are available for pediatric patients less than 8 years of age. For the treatment of VTE in pediatric patients, initiate treatment following treatment with a parenteral anticoagulant for at least 5 days. For reduction in risk of recurrence of VTE, initiate treatment following previous treatment.
PRADAXA Capsules is dosed orally twice daily, one dose in the morning and one dose in the evening, at approximately the same time every day. The dosing interval should be as close to 12 hours as possible.
The recommended dose of PRADAXA Capsules for the treatment of or reducing the risk of VTE in pediatric patients 8 to less than 18 years of age is based on the patient's actual weight as shown in Table 1 below. Administer PRADAXA twice daily. Adjust the dose according to actual weight as treatment progresses [see Dosage and Administration (2.5)].
| Actual Weight (kg) | Dose (mg) | Number of Capsules Needed |
|---|---|---|
| 11 kg to less than 16 kg | 75 mg twice daily | one 75 mg capsule twice daily |
| 16 kg to less than 26 kg | 110 mg twice daily | one 110 mg capsule twice daily |
| 26 kg to less than 41 kg | 150 mg twice daily | one 150 mg capsule twice daily or two 75 mg capsules twice daily |
| 41 kg to less than 61 kg | 185 mg twice daily | one 110 mg capsule plus one 75 mg capsule twice daily |
| 61 kg to less than 81 kg | 220 mg twice daily | two 110 mg capsule twice daily |
| 81 kg or greater | 260 mg twice daily | one 150 mg capsule plus one 110 mg capsule twice daily or one 110 mg capsule plus two 75 mg capsules twice daily |
2.5 Administration
PRADAXA Capsules should be swallowed whole. PRADAXA Capsules should be taken with a full glass of water. Breaking, chewing, or emptying the contents of the capsule can result in increased exposure [see Clinical Pharmacology (12.3)].
If a dose of PRADAXA Capsules is not taken at the scheduled time, the dose should be taken as soon as possible on the same day; the missed dose should be skipped if it cannot be taken at least 6 hours before the next scheduled dose. The dose of PRADAXA Capsules should not be doubled to make up for a missed dose.
Consider administration with food if gastrointestinal distress occurs with PRADAXA Capsules.
2.6 Converting from or to Warfarin
When converting patients from warfarin therapy to PRADAXA Capsules, discontinue warfarin and start PRADAXA Capsules when the INR is below 2.0.
When converting from PRADAXA Capsules to warfarin, adjust the starting time of warfarin as follows:
2.7 Converting from or to Parenteral Anticoagulants
For adult and pediatric patients currently receiving a parenteral anticoagulant, start PRADAXA Capsules 0 to 2 hours before the time that the next dose of the parenteral drug was to have been administered or at the time of discontinuation of a continuously administered parenteral drug (e.g., intravenous unfractionated heparin).
For adult patients currently taking PRADAXA Capsules wait 12 hours (CrCl ≥30 mL/min) or 24 hours (CrCl <30 mL/min) after the last dose of PRADAXA Capsules before initiating treatment with a parenteral anticoagulant [see Clinical Pharmacology (12.3)].
For pediatric patients currently taking PRADAXA, wait 12 hours after the last dose before switching to a parenteral anticoagulant.
2.8 Discontinuation for Surgery and Other Interventions
If possible, discontinue PRADAXA Capsules in adults 1 to 2 days (CrCl ≥50 mL/min) or 3 to 5 days (CrCl <50 mL/min) before invasive or surgical procedures because of the increased risk of bleeding. Consider longer times for patients undergoing major surgery, spinal puncture, or placement of a spinal or epidural catheter or port, in whom complete hemostasis may be required [see Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
For pediatric patients, discontinue PRADAXA Capsules 24 hours before an elective surgery (eGFR > 80 mL/min/1.73m2) or 2 days before an elective surgery (eGFR 50-80 mL/min/1.73m2). Pediatric patients with an eGFR <50 mL/min/1.73m2 have not been studied, avoid use of PRADAXA Capsules in these patients.
If surgery cannot be delayed, there is an increased risk of bleeding [see Warnings and Precautions (5.2)]. This risk of bleeding should be weighed against the urgency of intervention [see Warnings and Precautions (5.1, 5.3)]. Use a specific reversal agent (idarucizumab) in case of emergency surgery or urgent procedures when reversal of the anticoagulant effect of dabigatran is needed in adults. Efficacy and safety of idarucizumab have not been established in pediatric patients [see Warnings and Precautions (5.2)]. Refer to the idarucizumab prescribing information for additional information. Restart PRADAXA Capsules as soon as medically appropriate.
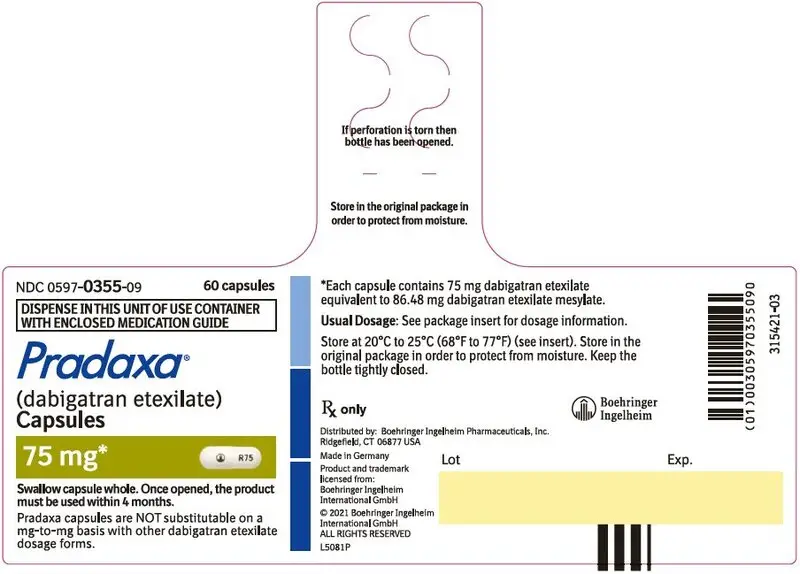
3. Dosage Forms and Strengths
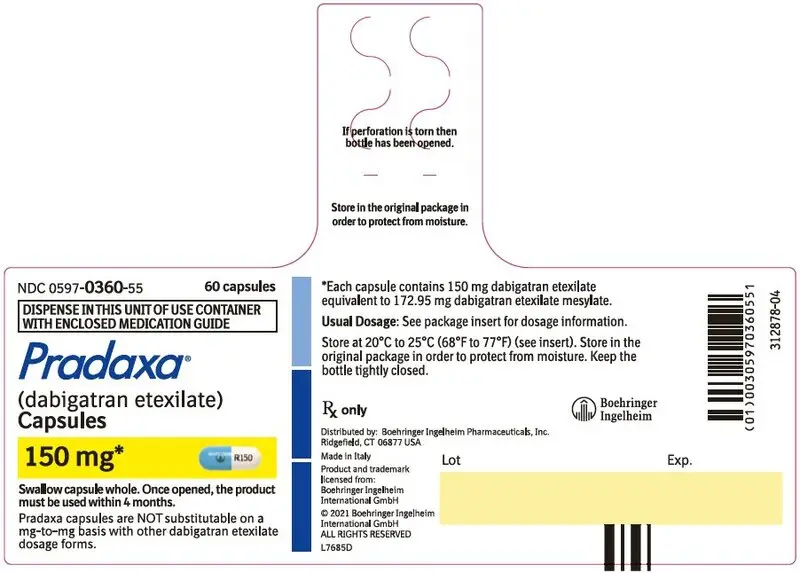
150 mg capsules with a light blue opaque cap imprinted in black with the Boehringer Ingelheim company symbol and a white opaque body imprinted in black with "R150".
110 mg capsules with a light blue opaque cap imprinted in black with the Boehringer Ingelheim company symbol and a light blue opaque body imprinted in black with "R110".
75 mg capsules with a white opaque cap imprinted in black with the Boehringer Ingelheim company symbol and a white opaque body imprinted in black with "R75".
4. Contraindications
PRADAXA is contraindicated in patients with:
- Active pathological bleeding [see Warnings and Precautions (5.2) and Adverse Reactions (6.1)]
- History of a serious hypersensitivity reaction to dabigatran, dabigatran etexilate, or to one of the excipients of the product (e.g., anaphylactic reaction or anaphylactic shock) [see Adverse Reactions (6.1)]
- Mechanical prosthetic heart valve [see Warnings and Precautions (5.4)]
5. Warnings and Precautions
5.1 Increased Risk of Thrombotic Events after Premature Discontinuation
Premature discontinuation of any oral anticoagulant, including PRADAXA, in the absence of adequate alternative anticoagulation increases the risk of thrombotic events. If PRADAXA Capsules is discontinued for a reason other than pathological bleeding or completion of a course of therapy, consider coverage with another anticoagulant and restart PRADAXA Capsules as soon as medically appropriate [see Dosage and Administration (2.6, 2.7, 2.8)].
5.2 Risk of Bleeding
PRADAXA increases the risk of bleeding and can cause significant and, sometimes, fatal bleeding. Promptly evaluate any signs or symptoms of blood loss (e.g., a drop in hemoglobin and/or hematocrit or hypotension). Discontinue PRADAXA Capsules in patients with active pathological bleeding [see Dosage and Administration (2.4)].
Risk factors for bleeding include the concomitant use of other drugs that increase the risk of bleeding (e.g., anti-platelet agents, heparin, fibrinolytic therapy, and chronic use of NSAIDs). PRADAXA's anticoagulant activity and half-life are increased in patients with renal impairment [see Clinical Pharmacology (12.2)].
5.3 Spinal/Epidural Anesthesia or Puncture
When neuraxial anesthesia (spinal/epidural anesthesia) or spinal puncture is employed, patients treated with anticoagulant agents are at risk of developing an epidural or spinal hematoma which can result in long-term or permanent paralysis [see Boxed Warning].
To reduce the potential risk of bleeding associated with the concurrent use of PRADAXA and epidural or spinal anesthesia/analgesia or spinal puncture, consider the pharmacokinetic profile of dabigatran [see Clinical Pharmacology (12.3)]. Placement or removal of an epidural catheter or lumbar puncture is best performed when the anticoagulant effect of dabigatran is low; however, the exact timing to reach a sufficiently low anticoagulant effect in each patient is not known.
Should the physician decide to administer anticoagulation in the context of epidural or spinal anesthesia/analgesia or lumbar puncture, monitor frequently to detect any signs or symptoms of neurological impairment, such as midline back pain, sensory and motor deficits (numbness, tingling, or weakness in lower limbs), bowel and/or bladder dysfunction. Instruct patients to immediately report if they experience any of the above signs or symptoms. If signs or symptoms of spinal hematoma are suspected, initiate urgent diagnosis and treatment including consideration for spinal cord decompression even though such treatment may not prevent or reverse neurological sequelae.
5.4 Thromboembolic and Bleeding Events in Patients with Prosthetic Heart Valves
The safety and efficacy of PRADAXA Capsules in adult patients with bileaflet mechanical prosthetic heart valves was evaluated in the RE-ALIGN trial, in which patients with bileaflet mechanical prosthetic heart valves (recently implanted or implanted more than three months prior to enrollment) were randomized to dose-adjusted warfarin or 150 mg, 220 mg, or 300 mg of PRADAXA Capsules twice a day. RE-ALIGN was terminated early due to the occurrence of significantly more thromboembolic events (valve thrombosis, stroke, transient ischemic attack, and myocardial infarction) and an excess of major bleeding (predominantly post-operative pericardial effusions requiring intervention for hemodynamic compromise) in the PRADAXA Capsules treatment arm as compared to the warfarin treatment arm. These bleeding and thromboembolic events were seen both in patients who were initiated on PRADAXA Capsules postoperatively within three days of mechanical bileaflet valve implantation, as well as in patients whose valves had been implanted more than three months prior to enrollment. Therefore, the use of PRADAXA is contraindicated in all patients with mechanical prosthetic valves [see Contraindications (4)].
The use of PRADAXA for the prophylaxis of thromboembolic events in patients with atrial fibrillation in the setting of other forms of valvular heart disease, including the presence of a bioprosthetic heart valve, has not been studied and is not recommended.
5.5 Effect of P-gp Inducers and Inhibitors on Dabigatran Exposure
The concomitant use of PRADAXA with P-gp inducers (e.g., rifampin) reduces exposure to dabigatran and should generally be avoided [see Clinical Pharmacology (12.3)].
P-gp inhibition and impaired renal function are the major independent factors that result in increased exposure to dabigatran [see Clinical Pharmacology (12.3)]. Concomitant use of P-gp inhibitors in patients with renal impairment is expected to produce increased exposure of dabigatran compared to that seen with either factor alone.
5.6 Increased Risk of Thrombosis in Patients with Triple-Positive Antiphospholipid Syndrome
Direct-acting oral anticoagulants (DOACs), including PRADAXA, are not recommended for use in patients with triple-positive antiphospholipid syndrome (APS). For patients with APS (especially those who are triple-positive [positive for lupus anticoagulant, anticardiolipin, and anti-beta 2-glycoprotein I antibodies]), treatment with DOACs has been associated with increased rates of recurrent thrombotic events compared with vitamin K antagonist therapy.
6. Adverse Reactions/Side Effects
The following clinically significant adverse reactions are described elsewhere in the labeling:
- Increased Risk of Thrombotic Events after Premature Discontinuation [see Warnings and Precautions (5.1)]
- Risk of Bleeding [see Warnings and Precautions (5.2)]
- Spinal/Epidural Anesthesia or Puncture [see Warnings and Precautions (5.3)]
- Thromboembolic and Bleeding Events in Patients with Prosthetic Heart Valves [see Warnings and Precautions (5.4)]
- Increased Risk of Thrombosis in Patients with Triple-Positive Antiphospholipid Syndrome [see Warnings and Precautions (5.6)]
The most serious adverse reactions reported with PRADAXA were related to bleeding [see Warnings and Precautions (5.2)].
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reactions rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Adult Trials
Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation
The RE-LY (Randomized Evaluation of Long-term Anticoagulant Therapy) study provided safety information on the use of two doses of PRADAXA Capsules and warfarin [see Clinical Studies (14.1)]. The numbers of patients and their exposures are described in Table 2. Limited information is presented on the 110 mg dosing arm because this dose is not approved.
| PRADAXA Capsules 110 mg twice daily | PRADAXA Capsules 150 mg twice daily | Warfarin | |
|---|---|---|---|
| Total number treated | 5983 | 6059 | 5998 |
| Exposure | |||
| > 12 months | 4936 | 4939 | 5193 |
| > 24 months | 2387 | 2405 | 2470 |
| Mean exposure (months) | 20.5 | 20.3 | 21.3 |
| Total patient-years | 10,242 | 10,261 | 10,659 |
Bleeding [see Warnings and Precautions (5.2)]
Table 3 shows the number of adjudicated major bleeding events during the treatment period in the RE-LY study, with the bleeding rate per 100 subject-years (%). Major bleeding is defined as bleeding accompanied by one or more of the following: a decrease in hemoglobin of ≥2 g/dL, a transfusion of ≥2 units of packed red blood cells, bleeding at a critical site or with a fatal outcome. Intracranial hemorrhage included intracerebral (hemorrhagic stroke), subarachnoid, and subdural bleeds.
| Event | PRADAXA Capsules 150 mg N = 6059 n (%/yearb) | Warfarin N = 5998 n (%/yearb) | PRADAXA Capsules 150 mg vs Warfarin HR (95% CI) |
|---|---|---|---|
| aPatients during treatment or within 2 days of stopping study treatment. Major bleeding events within each subcategory were counted once per patient, but patients may have contributed events to multiple subcategories. bAnnual event rate per 100 pt-years = 100 * number of subjects with event/subject-years. Subject-years is defined as cumulative number of days from first drug intake to event date, date of last drug intake + 2, death date (whatever occurred first) across all treated subjects divided by 365.25. In case of recurrent events of the same category, the first event was considered. cDefined as bleeding accompanied by one or more of the following: a decrease in hemoglobin of ≥2 g/dL, a transfusion of 2 or more units of packed red blood cells, bleeding at a critical site or with fatal outcome. dIntracranial bleed included intracerebral (hemorrhagic stroke), subarachnoid, and subdural bleeds. eOn-treatment analysis based on the safety population, compared to ITT analysis presented in Section 14 Clinical Studies. fFatal bleed: Adjudicated major bleed as defined above with investigator reported fatal outcome and adjudicated death with primary cause from bleeding. gNon-intracranial fatal bleed: Adjudicated major bleed as defined above and adjudicated death with primary cause from bleeding but without symptomatic intracranial bleed based on investigator's clinical assessment. |
|||
| Major Bleedingc | 350 (3.47) | 374 (3.58) | 0.97 (0.84, 1.12) |
| Intracranial Hemorrhage (ICH)d | 23 (0.22) | 82 (0.77) | 0.29 (0.18, 0.46) |
| Hemorrhagic Strokee | 6 (0.06) | 40 (0.37) | 0.16 (0.07, 0.37) |
| Other ICH | 17 (0.17) | 46 (0.43) | 0.38 (0.22, 0.67) |
| Gastrointestinal | 162 (1.59) | 111 (1.05) | 1.51 (1.19, 1.92) |
| Fatal Bleedingf | 7 (0.07) | 16 (0.15) | 0.45 (0.19, 1.10) |
| ICH | 3 (0.03) | 9 (0.08) | 0.35 (0.09, 1.28) |
| Non-intracranialg | 4 (0.04) | 7 (0.07) | 0.59 (0.17, 2.02) |
There was a higher rate of any gastrointestinal bleeds in patients receiving PRADAXA Capsules 150 mg than in patients receiving warfarin (6.6% vs 4.2%, respectively).
The risk of major bleeds was similar with PRADAXA Capsules 150 mg and warfarin across major subgroups defined by baseline characteristics (see Figure 1), with the exception of age, where there was a trend toward a higher incidence of major bleeding on PRADAXA Capsules (hazard ratio 1.2, 95% CI: 1.0 to 1.5) for patients ≥75 years of age.
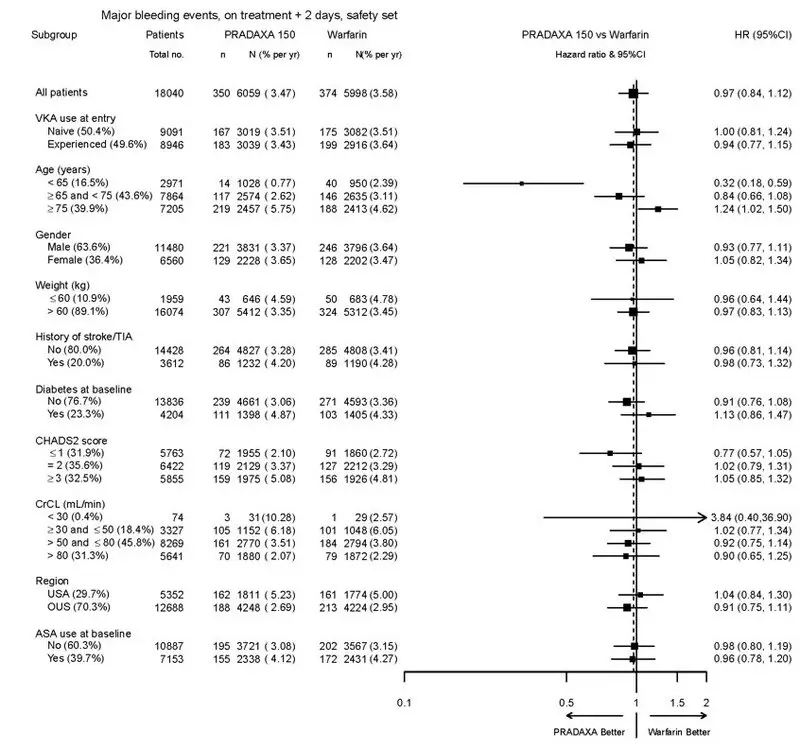
Note: The figure above presents effects in various subgroups all of which are baseline characteristics and all of which were pre-specified. The 95% confidence limits that are shown do not take into account how many comparisons were made, nor do they reflect the effect of a particular factor after adjustment for all other factors. Apparent homogeneity or heterogeneity among groups should not be over-interpreted.
Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism
PRADAXA Capsules was studied in 4387 patients in 4 pivotal, parallel, randomized, double-blind trials. Three of these trials were active-controlled (warfarin) (RE-COVER, RE-COVER II, and RE-MEDY), and one study (RE-SONATE) was placebo-controlled. The demographic characteristics were similar among the 4 pivotal studies and between the treatment groups within these studies. Approximately 60% of the treated patients were male, with a mean age of 55.1 years. The majority of the patients were white (87.7%), 10.3% were Asian, and 1.9% were black with a mean CrCl of 105.6 mL/min.
Bleeding events for the 4 pivotal studies were classified as major bleeding events if at least one of the following criteria applied: fatal bleeding, symptomatic bleeding in a critical area or organ (intraocular, intracranial, intraspinal or intramuscular with compartment syndrome, retroperitoneal bleeding, intra-articular bleeding, or pericardial bleeding), bleeding causing a fall in hemoglobin level of 2.0 g/dL (1.24 mmol/L or more, or leading to transfusion of 2 or more units of whole blood or red cells).
RE-COVER and RE-COVER II studies compared PRADAXA Capsules 150 mg twice daily and warfarin for the treatment of deep vein thrombosis and pulmonary embolism. Patients received 5-10 days of an approved parenteral anticoagulant therapy followed by 6 months, with mean exposure of 164 days, of oral only treatment; warfarin was overlapped with parenteral therapy. Table 4 shows the number of patients experiencing bleeding events in the pooled analysis of RE-COVER and RE-COVER II studies during the full treatment including parenteral and oral only treatment periods after randomization.
| Bleeding Events—Full Treatment Period Including Parenteral Treatment | |||
|---|---|---|---|
| Note: MBE can belong to more than one criterion. aPatients with at least one MBE. bBleeding site based on investigator assessment. Patients can have more than one site of bleeding. cConfidence interval |
|||
| PRADAXA Capsules 150 mg twice daily N (%) | Warfarin N (%) | Hazard Ratio (95% CI)c |
|
| Patients | N=2553 | N=2554 | |
| Major bleeding eventa | 37 (1.4) | 51 (2.0) | 0.73 (0.48, 1.11) |
| Fatal bleeding | 1 (0.04) | 2 (0.1) | |
| Bleeding in a critical area or organ | 7 (0.3) | 15 (0.6) | |
| Fall in hemoglobin ≥2 g/dL or transfusion ≥2 units of whole blood or packed red blood cells | 32 (1.3) | 38 (1.5) | |
| Bleeding sites for MBEb | |||
| Intracranial | 2 (0.1) | 5 (0.2) | |
| Retroperitoneal | 2 (0.1) | 1 (0.04) | |
| Intraarticular | 2 (0.1) | 4 (0.2) | |
| Intramuscular | 2 (0.1) | 6 (0.2) | |
| Gastrointestinal | 15 (0.6) | 14 (0.5) | |
| Urogenital | 7 (0.3) | 14 (0.5) | |
| Other | 8 (0.3) | 8 (0.3) | |
| Clinically relevant non-major bleeding | 101 (4.0) | 170 (6.7) | 0.58 (0.46, 0.75) |
| Any bleeding | 411 (16.1) | 567 (22.7) | 0.70 (0.61, 0.79) |
The rate of any gastrointestinal bleeds in patients receiving PRADAXA Capsules 150 mg in the full treatment period was 3.1% (2.4% on warfarin).
The RE-MEDY and RE-SONATE studies provided safety information on the use of PRADAXA Capsules for the reduction in the risk of recurrence of deep vein thrombosis and pulmonary embolism.
RE-MEDY was an active-controlled study (warfarin) in which 1430 patients received PRADAXA Capsules 150 mg twice daily following 3 to 12 months of oral anticoagulant regimen. Patients in the treatment studies who rolled over into the RE-MEDY study had a combined treatment duration of up to more than 3 years, with mean exposure of 473 days. Table 5 shows the number of patients experiencing bleeding events in the study.
| PRADAXA Capsules 150 mg twice daily N (%) | Warfarin N (%) | Hazard Ratio (95% CI)c |
|
|---|---|---|---|
| Note: MBE can belong to more than one criterion. aPatients with at least one MBE. bBleeding site based on investigator assessment. Patients can have more than one site of bleeding. cConfidence interval |
|||
| Patients | N=1430 | N=1426 | |
| Major bleeding eventa | 13 (0.9) | 25 (1.8) | 0.54 (0.25, 1.16) |
| Fatal bleeding | 0 | 1 (0.1) | |
| Bleeding in a critical area or organ | 7 (0.5) | 11 (0.8) | |
| Fall in hemoglobin ≥2 g/dL or transfusion ≥2 units of whole blood or packed red blood cells | 7 (0.5) | 16 (1.1) | |
| Bleeding sites for MBEb | |||
| Intracranial | 2 (0.1) | 4 (0.3) | |
| Intraocular | 4 (0.3) | 2 (0.1) | |
| Retroperitoneal | 0 | 1 (0.1) | |
| Intraarticular | 0 | 2 (0.1) | |
| Intramuscular | 0 | 4 (0.3) | |
| Gastrointestinal | 4 (0.3) | 8 (0.6) | |
| Urogenital | 1 (0.1) | 1 (0.1) | |
| Other | 2 (0.1) | 4 (0.3) | |
| Clinically relevant non-major bleeding | 71 (5.0) | 125 (8.8) | 0.56 (0.42, 0.75) |
| Any bleeding | 278 (19.4) | 373 (26.2) | 0.71 (0.61, 0.83) |
In the RE-MEDY study, the rate of any gastrointestinal bleeds in patients receiving PRADAXA Capsules 150 mg was 3.1% (2.2% on warfarin).
RE-SONATE was a placebo-controlled study in which 684 patients received PRADAXA Capsules 150 mg twice daily following 6 to 18 months of oral anticoagulant regimen. Patients in the treatment studies who rolled over into the RE-SONATE study had combined treatment duration up to 9 months, with mean exposure of 165 days. Table 6 shows the number of patients experiencing bleeding events in the study.
| PRADAXA Capsules 150 mg twice daily N (%) | Placebo N (%) | Hazard Ratio (95% CI)c |
|
|---|---|---|---|
| Note: MBE can belong to more than one criterion. aPatients with at least one MBE. bBleeding site based on investigator assessment. Patients can have more than one site of bleeding. cConfidence interval |
|||
| Patients | N=684 | N=659 | |
| Major bleeding eventa | 2 (0.3) | 0 | |
| Bleeding in a critical area or organ | 0 | 0 | |
| Gastrointestinalb | 2 (0.3) | 0 | |
| Clinically relevant non-major bleeding | 34 (5.0) | 13 (2.0) | 2.54 (1.34, 4.82) |
| Any bleeding | 72 (10.5) | 40 (6.1) | 1.77 (1.20, 2.61) |
In the RE-SONATE study, the rate of any gastrointestinal bleeds in patients receiving PRADAXA Capsules 150 mg was 0.7% (0.3% on placebo).
Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism Following Hip Replacement Surgery
PRADAXA Capsules was studied in 5476 patients, randomized and treated in two double-blind, active-controlled non-inferiority trials (RE-NOVATE and RE-NOVATE II). The demographic characteristics were similar across the two studies and between the treatment groups within these studies. Approximately 45.3% of the treated patients were male, with a mean age of 63.2 years. The majority of the patients were white (96.1%), 3.6% were Asian, and 0.3% were black with a mean CrCl of 92 mL/min.
Bleeding events for the RE-NOVATE and RE-NOVATE II studies were classified as major bleeding events if at least one of the following criteria applied: fatal bleeding, symptomatic bleeding in a critical area or organ (intraocular, intracranial, intraspinal or retroperitoneal bleeding), bleeding causing a fall in hemoglobin level of 2.0 g/dL (1.24 mmol/L) or more, or leading to transfusion of 2 or more units of whole blood or red cells, requiring treatment cessation or leading to re-operation.
The RE-NOVATE study compared PRADAXA Capsules 75 mg taken orally 1-4 hours after surgery followed by 150 mg once daily, PRADAXA Capsules 110 mg taken orally 1-4 hours after surgery followed by 220 mg once daily and subcutaneous enoxaparin 40 mg once daily initiated the evening before surgery for the prophylaxis of deep vein thrombosis and pulmonary embolism in patients who had undergone hip replacement surgery. The RE-NOVATE II study compared PRADAXA Capsules 110 mg taken orally 1-4 hours after surgery followed by 220 mg once daily and subcutaneous enoxaparin 40 mg once daily initiated the evening before surgery for the prophylaxis of deep vein thrombosis and pulmonary embolism in patients who had undergone hip replacement surgery. In the RE-NOVATE and RE-NOVATE II studies, patients received 28-35 days of PRADAXA Capsules or enoxaparin with median exposure of 33 days. Tables 7 and 8 show the number of patients experiencing bleeding events in the analysis of RE-NOVATE and RE-NOVATE II.
| PRADAXA Capsules 220 mg N (%) | Enoxaparin N (%) |
|
|---|---|---|
| Patients | N=1146 | N=1154 |
| Major bleeding event | 23 (2.0) | 18 (1.6) |
| Clinically relevant non-major bleeding | 48 (4.2) | 40 (3.5) |
| Any bleeding | 141 (12.3) | 132 (11.4) |
| PRADAXA Capsules 220 mg N (%) | Enoxaparin N (%) |
|
|---|---|---|
| Patients | N=1010 | N=1003 |
| Major bleeding event | 14 (1.4) | 9 (0.9) |
| Clinically relevant non-major bleeding | 26 (2.6) | 20 (2.0) |
| Any bleeding | 98 (9.7) | 83 (8.3) |
In the two studies, the rate of major gastrointestinal bleeds in patients receiving PRADAXA Capsules and enoxaparin was the same (0.1%) and for any gastrointestinal bleeds was 1.4% for PRADAXA Capsules 220 mg and 0.9% for enoxaparin.
Pediatric Trials
Treatment of VTE in Pediatric Patients
The safety of PRADAXA in the treatment of VTE in pediatric patients was studied in one phase III trial (DIVERSITY). The DIVERSITY study was a randomized, open-label, active-controlled, parallel-group trial comparing PRADAXA with standard of care – SOC (vitamin K antagonists, low molecular weight heparin, or fondaparinux). There were 266 pediatric patients who received study treatment, 176 patients treated with PRADAXA and 90 patients treated with SOC. Patients on PRADAXA received age- and weight-adjusted doses of an age-appropriate formulation of PRADAXA (capsules, pellets, or oral solution) twice daily.
Patients had a median age of 14 years (range: 0-17 years), 92% were white, and half the patients were male (50%). Following at least 5 days of parenteral anticoagulant therapy, the median duration of treatment with PRADAXA was 85 days (range: 1-105). Patients with estimated glomerular filtration rate (eGFR) < 50 mL/min/1.73m2 were excluded from the trial.
Bleeding
Data on adjudicated major bleeding, clinically relevant non-major (CRNM) bleeding and minor bleeding events, for the PRADAXA group and the SOC group in the DIVERSITY study, are reported in Table 9. There was no statistically significant difference in the time to first major bleeding event.
| PRADAXA N (%) | Standard of Care (SOC) N (%) |
|
|---|---|---|
| 1 Major bleeding event if at least one of the following criteria applied: fatal bleeding, symptomatic bleeding in a critical area or organ (intraocular, intracranial, intraspinal or intramuscular with compartment syndrome, retroperitoneal bleeding, intra-articular bleeding, or pericardial bleeding), bleeding causing a fall in hemoglobin level of 2.0 g/dL (1.24 mmol/L) or more, or leading to transfusion of 2 or more units of whole blood or red cells. | ||
| Patients | N=176 | N=90 |
| Major bleeding event1 | 4 (2.3) | 2 (2.2) |
| Fatal bleeding | 0 | 1 (1.1) |
| Clinically relevant non-major bleeding | 2 (1.1) | 1 (1.1) |
| Minor bleeding | 33 (19) | 21 (23) |
| Major and clinically relevant non-major bleeding | 6 (3.4) | 3 (3.3) |
| Any bleeding | 38 (22) | 22 (24) |
Site-specific bleeding rates were comparable between the two arms, with the exception of the rate of any gastrointestinal bleeds (5.7% in PRADAXA arm vs 1.8% in SOC arm).
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of PRADAXA. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure. The following adverse reactions have been identified during post approval use of PRADAXA: angioedema, thrombocytopenia, esophageal ulcer, alopecia, neutropenia, agranulocytosis.
7. Drug Interactions
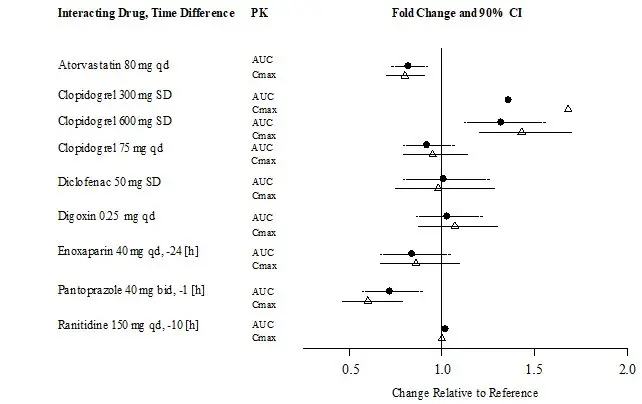
7.1 Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult Patients
The concomitant use of PRADAXA with P-gp inducers (e.g., rifampin) reduces exposure to dabigatran and should generally be avoided [see Clinical Pharmacology (12.3)].
P-gp inhibition and impaired renal function are the major independent factors that result in increased exposure to dabigatran [see Clinical Pharmacology (12.3)]. Concomitant use of P-gp inhibitors in patients with renal impairment is expected to produce increased exposure of dabigatran compared to that seen with either factor alone.
In patients with moderate renal impairment (CrCl 30-50 mL/min), reduce the dose of PRADAXA to 75 mg twice daily when administered concomitantly with the P-gp inhibitors dronedarone or systemic ketoconazole. The use of the P-gp inhibitors verapamil, amiodarone, quinidine, clarithromycin, and ticagrelor does not require a dose adjustment of PRADAXA. These results should not be extrapolated to other P-gp inhibitors [see Warnings and Precautions (5.5), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
The concomitant use of PRADAXA and P-gp inhibitors in patients with severe renal impairment (CrCl 15-30 mL/min) should be avoided [see Warnings and Precautions (5.5), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
7.2 Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
Avoid use of PRADAXA and P-gp inhibitors in patients with CrCl <50 mL/min [see Warnings and Precautions (5.5), Use in Specific Populations (8.6), and Clinical Pharmacology (12.3)].
7.3 Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism in Adult Patients Following Hip Replacement Surgery
In patients with CrCl ≥50 mL/min who have concomitant administration of P-gp inhibitors such as dronedarone or systemic ketoconazole, it may be helpful to separate the timing of administration of PRADAXA and the P-gp inhibitor by several hours. The concomitant use of PRADAXA and P-gp inhibitors in patients with CrCl <50 mL/min should be avoided [see Warnings and Precautions (5.5), Use in Specific Populations (8.6) and Clinical Pharmacology (12.2, 12.3)].
8. Use In Specific Populations
8.3 Females and Males of Reproductive Potential
Females of reproductive potential requiring anticoagulation should discuss pregnancy planning with their physician.
The risk of clinically significant uterine bleeding, potentially requiring gynecological surgical interventions, identified with oral anticoagulants including PRADAXA should be assessed in females of reproductive potential and those with abnormal uterine bleeding.
8.4 Pediatric Use
The safety and effectiveness of PRADAXA Capsules for the treatment and the reduction in risk of recurrence of venous thromboembolism have been established in pediatric patients 8 to less than 18 years of age. Use of PRADAXA for this indication is supported by evidence from adequate and well-controlled studies in pediatric patients. These studies included an open-label, randomized, parallel-group study and an open-label, single-arm safety study [see Adverse Reactions (6.1) and Clinical Studies (14.4, 14.5)]. Other age-appropriate pediatric dosage forms of dabigatran etexilate are available for pediatric patients less than 8 years of age for these indications.
Safety and effectiveness of PRADAXA Capsules have not been established in pediatric patients with non-valvular atrial fibrillation or those who have undergone hip replacement surgery.
8.5 Geriatric Use
Of the total number of patients in the RE-LY study, 82% were 65 and over, while 40% were 75 and over. The risk of stroke and bleeding increases with age, but the risk-benefit profile is favorable in all age groups [see Warnings and Precautions (5), Adverse Reactions (6.1), and Clinical Studies (14.1)].
10. Overdosage
Accidental overdose may lead to hemorrhagic complications. In the event of hemorrhagic complications, initiate appropriate clinical support, discontinue treatment with PRADAXA, and investigate the source of bleeding. A specific reversal agent (idarucizumab) is available for adult patients.
Dabigatran is primarily eliminated by the kidneys with a low plasma protein binding of approximately 35%. Hemodialysis can remove dabigatran; however, data supporting this approach are limited. Using a high-flux dialyzer, blood flow rate of 200 mL/min, and dialysate flow rate of 700 mL/min, approximately 49% of total dabigatran can be cleared from plasma over 4 hours. At the same dialysate flow rate, approximately 57% can be cleared using a dialyzer blood flow rate of 300 mL/min, with no appreciable increase in clearance observed at higher blood flow rates. Upon cessation of hemodialysis, a redistribution effect of approximately 7% to 15% is seen. The effect of dialysis on dabigatran's plasma concentration would be expected to vary based on patient specific characteristics. Measurement of aPTT or ECT may help guide therapy [see Warnings and Precautions (5.2) and Clinical Pharmacology (12.2)].
11. Pradaxa Description
The chemical name for dabigatran etexilate mesylate, a direct thrombin inhibitor, is β-Alanine, N-[[2-[[[4-[[[(hexyloxy)carbonyl]amino]iminomethyl] phenyl]amino]methyl]-1-methyl-1H-benzimidazol-5-yl]carbonyl]-N-2-pyridinyl-,ethyl ester, methanesulfonate. The empirical formula is C34H41N7O5 ∙ CH4O3S and the molecular weight is 723.86 (mesylate salt), 627.75 (free base). The structural formula is:
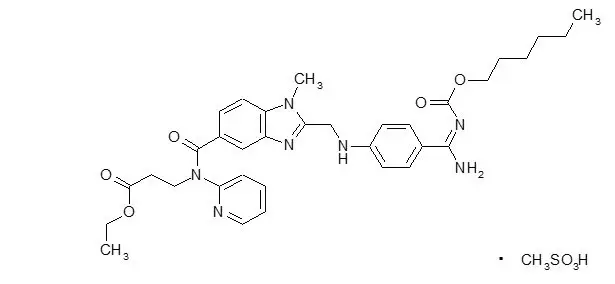
Dabigatran etexilate mesylate is a yellow-white to yellow powder. A saturated solution in pure water has a solubility of 1.8 mg/mL. It is freely soluble in methanol, slightly soluble in ethanol, and sparingly soluble in isopropanol.
PRADAXA Capsules are supplied in 75 mg, 110 mg, and 150 mg strengths for oral administration. Each capsule contains dabigatran etexilate mesylate as the active ingredient: 150 mg dabigatran etexilate (equivalent to 172.95 mg dabigatran etexilate mesylate), 110 mg dabigatran etexilate (equivalent to 126.83 mg dabigatran etexilate mesylate), or 75 mg dabigatran etexilate (equivalent to 86.48 mg dabigatran etexilate mesylate) along with the following inactive ingredients: acacia, dimethicone, hypromellose, hydroxypropyl cellulose, talc, and tartaric acid. The capsule shell is composed of carrageenan, hypromellose, potassium chloride, titanium dioxide, black edible ink, and FD&C Blue No. 2 (150 mg and 110 mg capsules only).
12. Pradaxa - Clinical Pharmacology
12.1 Mechanism of Action
Dabigatran and its acyl glucuronides are competitive, direct thrombin inhibitors. Because thrombin (serine protease) enables the conversion of fibrinogen into fibrin during the coagulation cascade, its inhibition prevents the development of a thrombus. Both free and clot-bound thrombin, and thrombin-induced platelet aggregation are inhibited by the active moieties.
12.2 Pharmacodynamics
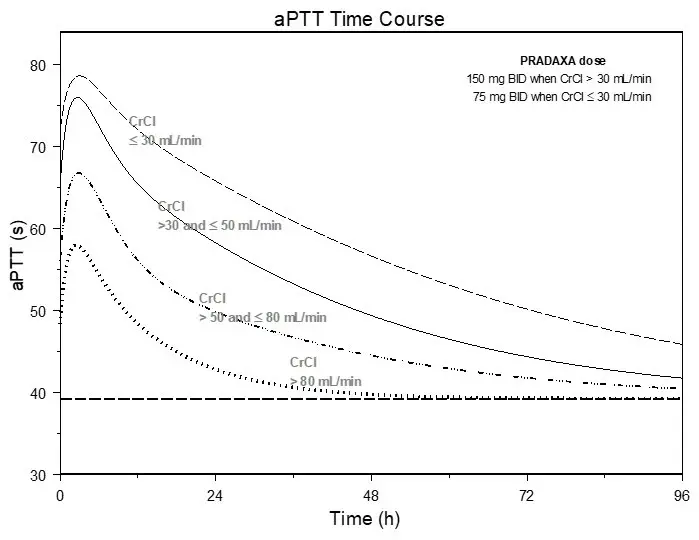
At recommended therapeutic doses, dabigatran etexilate prolongs the coagulation markers such as aPTT, ECT, TT, and dTT. INR is relatively insensitive to the exposure to dabigatran and cannot be interpreted the same way as used for warfarin monitoring.
12.3 Pharmacokinetics
Dabigatran etexilate mesylate is absorbed as the dabigatran etexilate ester. The ester is then hydrolyzed, forming dabigatran, the active moiety. Dabigatran is metabolized to four different acyl glucuronides and both the glucuronides and dabigatran have similar pharmacological activity. Pharmacokinetics described here refer to the sum of dabigatran and its glucuronides. Dabigatran displays dose-proportional pharmacokinetics in healthy adult subjects and adult patients in the range of doses from 10 to 400 mg. Given twice daily, dabigatran's accumulation factor in adults and pediatrics is approximately two.
Renal Impairment
An open, parallel-group, single-center study compared dabigatran pharmacokinetics in healthy adult subjects and adult patients with mild to moderate renal impairment receiving a single dose of PRADAXA Capsules 150 mg. Exposure to dabigatran increases with severity of renal function impairment (Table 10). Similar findings were observed in the RE-LY, RE-COVER and RE-NOVATE II trials.
| Renal Function | CrCl (mL/min) | Increase in AUC | Increase in Cmax | t1/2
(h) |
|---|---|---|---|---|
| +Patients with severe renal impairment were not studied in RE-LY, RE-COVER and RE-NOVATE II. Dosing recommendations in subjects with severe renal impairment are based on pharmacokinetic modeling [see Dosage and Administration (2.2, 2.4) and Use in Specific Populations (8.6)]. | ||||
| Normal | ≥ 80 | 1× | 1× | 13 |
| Mild | 50-80 | 1.5× | 1.1× | 15 |
| Moderate | 30-50 | 3.2× | 1.7× | 18 |
| Severe+ | 15-30 | 6.3× | 2.1× | 27 |
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Dabigatran was not carcinogenic when administered by oral gavage to mice and rats for up to 2 years. The highest doses tested (200 mg/kg/day) in mice and rats were approximately 3.6 and 6 times, respectively, the human exposure at MRHD of 300 mg/day based on AUC comparisons.
Dabigatran was not mutagenic in in vitro tests, including bacterial reversion tests, mouse lymphoma assay and chromosomal aberration assay in human lymphocytes, and the in vivo micronucleus assay in rats.
In the rat fertility study with oral gavage doses of 15, 70, and 200 mg/kg, males were treated for 29 days prior to mating, during mating up to scheduled termination, and females were treated 15 days prior to mating through gestation Day 6. No adverse effects on male or female fertility were observed at 200 mg/kg or 9 to 12 times the human exposure at MRHD of 300 mg/day based on AUC comparisons. However, the number of implantations decreased in females receiving 70 mg/kg, or 3 times the human exposure at MRHD based on AUC comparisons.
14. Clinical Studies
14.1 Reduction of Risk of Stroke and Systemic Embolism in Non-valvular Atrial Fibrillation in Adult Patients
The clinical evidence for the efficacy of PRADAXA Capsules was derived from RE-LY (Randomized Evaluation of Long-term Anticoagulant Therapy), a multi-center, multi-national, randomized, parallel group trial comparing two blinded doses of PRADAXA Capsules (110 mg twice daily and 150 mg twice daily) with open-label warfarin (dosed to target INR of 2 to 3) in patients with non-valvular, persistent, paroxysmal, or permanent atrial fibrillation and one or more of the following additional risk factors:
- Previous stroke, transient ischemic attack (TIA), or systemic embolism
- Left ventricular ejection fraction <40%
- Symptomatic heart failure, ≥ New York Heart Association Class 2
- Age ≥75 years
- Age ≥65 years and one of the following: diabetes mellitus, coronary artery disease (CAD), or hypertension
The primary objective of this study was to determine if PRADAXA Capsules was non-inferior to warfarin in reducing the occurrence of the composite endpoint, stroke (ischemic and hemorrhagic) and systemic embolism. The study was designed to ensure that PRADAXA Capsules preserved more than 50% of warfarin's effect as established by previous randomized, placebo-controlled trials of warfarin in atrial fibrillation. Statistical superiority was also analyzed.
A total of 18,113 patients were randomized and followed for a median of 2 years. The patients' mean age was 71.5 years and the mean CHADS2 score was 2.1. The patient population was 64% male, 70% Caucasian, 16% Asian, and 1% black. Twenty percent of patients had a history of a stroke or TIA and 50% were vitamin K antagonist (VKA) naïve, defined as less than 2 months total lifetime exposure to a VKA. Thirty-two percent of the population had never been exposed to a VKA. Concomitant diseases of patients in this trial included hypertension 79%, diabetes 23%, and CAD 28%. At baseline, 40% of patients were on aspirin and 6% were on clopidogrel. For patients randomized to warfarin, the mean percentage of time in therapeutic range (INR 2 to 3) was 64%.
Relative to warfarin and to PRADAXA Capsules 110 mg twice daily, PRADAXA Capsules 150 mg twice daily significantly reduced the primary composite endpoint of stroke and systemic embolism (see Table 11 and Figure 4).
| PRADAXA Capsules 150 mg twice daily | PRADAXA Capsules 110 mg twice daily | Warfarin | |
|---|---|---|---|
| * Randomized ITT | |||
| Patients randomized | 6076 | 6015 | 6022 |
| Patients (% per yr) with events | 135 (1.12%) | 183 (1.54%) | 203 (1.72%) |
| Hazard ratio vs warfarin (95% CI) | 0.65 (0.52, 0.81) | 0.89 (0.73, 1.09) | |
| P-value for superiority | 0.0001 | 0.27 | |
| Hazard ratio vs PRADAXA 110 mg (95% CI) | 0.72 (0.58, 0.91) | ||
| P-value for superiority | 0.005 | ||
Figure 4 Kaplan-Meier Curve Estimate of Time to First Stroke or Systemic Embolism
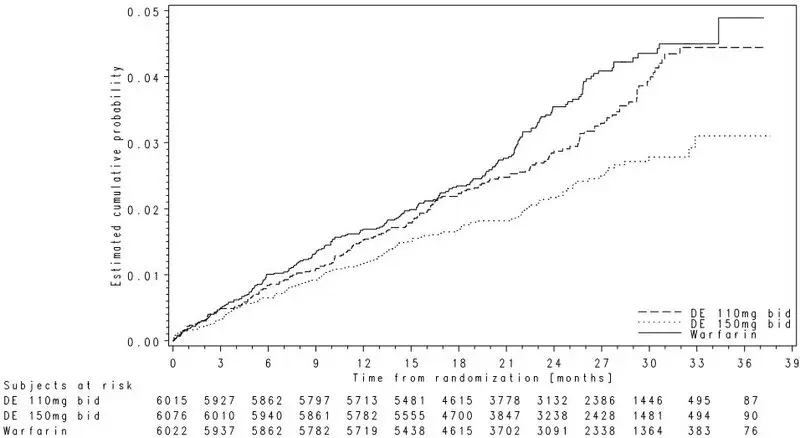
The contributions of the components of the composite endpoint, including stroke by subtype, are shown in Table 12. The treatment effect was primarily a reduction in stroke. PRADAXA Capsules 150 mg twice daily was superior in reducing ischemic and hemorrhagic strokes relative to warfarin.
| PRADAXA Capsules 150 mg twice daily | Warfarin | Hazard ratio vs warfarin (95% CI) |
|
|---|---|---|---|
| Patients randomized | 6076 | 6022 | |
| Stroke | 123 | 187 | 0.64 (0.51, 0.81) |
| Ischemic stroke | 104 | 134 | 0.76 (0.59, 0.98) |
| Hemorrhagic stroke | 12 | 45 | 0.26 (0.14, 0.49) |
| Systemic embolism | 13 | 21 | 0.61 (0.30, 1.21) |
In the RE-LY trial, the rate of all-cause mortality was lower on PRADAXA Capsules 150 mg than on warfarin (3.6% per year versus 4.1% per year). The rate of vascular death was lower on PRADAXA Capsules 150 mg compared to warfarin (2.3% per year versus 2.7% per year). Non-vascular death rates were similar in the treatment arms.
The efficacy of PRADAXA Capsules 150 mg twice daily was generally consistent across major subgroups (see Figure 5).
Figure 5 Stroke and Systemic Embolism Hazard Ratios by Baseline Characteristics*
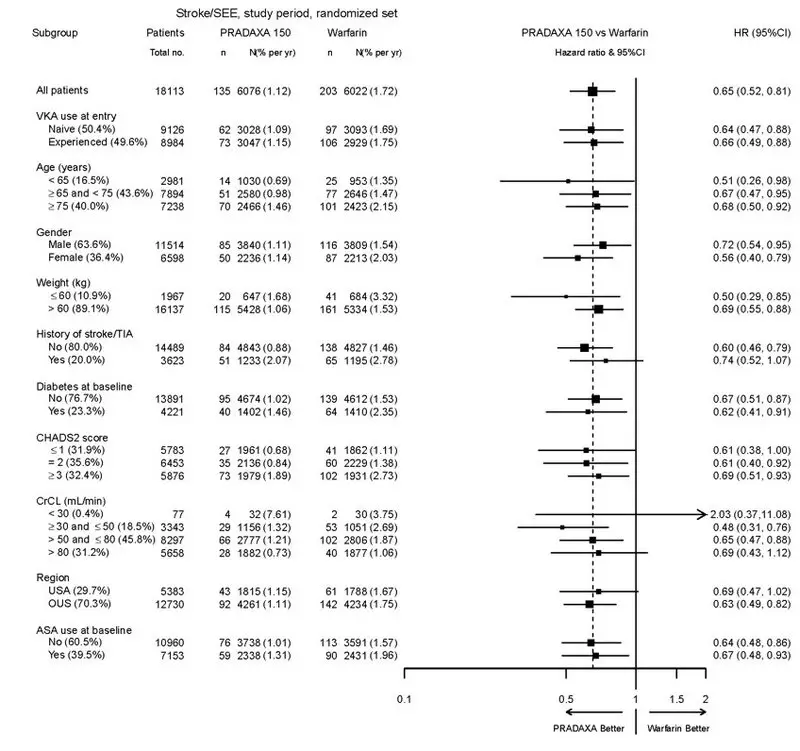
* Randomized ITT
Note: The figure above presents effects in various subgroups all of which are baseline characteristics and all of which were pre-specified. The 95% confidence limits that are shown do not take into account how many comparisons were made, nor do they reflect the effect of a particular factor after adjustment for all other factors. Apparent homogeneity or heterogeneity among groups should not be over-interpreted.
In RE-LY, a higher rate of clinical myocardial infarction was reported in patients who received PRADAXA Capsules (0.7 per 100 patient-years for 150 mg dose) than in those who received warfarin (0.6).
14.2 Treatment and Reduction in the Risk of Recurrence of Deep Venous Thrombosis and Pulmonary Embolism in Adult Patients
In the randomized, parallel group, double-blind trials, RE-COVER and RE-COVER II, patients with deep vein thrombosis and pulmonary embolism received PRADAXA Capsules 150 mg twice daily or warfarin (dosed to target INR of 2 to 3) following initial treatment with an approved parenteral anticoagulant for 5 to 10 days.
In RE-COVER, the median treatment duration during the oral only treatment period was 174 days. A total of 2539 patients (30.9% patients with symptomatic PE with or without DVT and 68.9% with symptomatic DVT only) were treated with a mean age of 54.7 years. The patient population was 58.4% male, 94.8% white, 2.6% Asian, and 2.6% black. The concomitant diseases of patients in this trial included hypertension (35.9%), diabetes mellitus (8.3%), coronary artery disease (6.5%), active cancer (4.8%), and gastric or duodenal ulcer (4.4%). Concomitant medications included agents acting on renin-angiotensin system (25.2%), vasodilators (28.4%), serum lipid-reducing agents (18.2%), NSAIDs (21%), beta-blockers (14.8%), calcium channel blockers (8.5%), ASA (8.6%), and platelet inhibitors excluding ASA (0.6%). Patients randomized to warfarin had a mean percentage of time in the INR target range of 2.0 to 3.0 of 60% in RE-COVER study.
In RE-COVER II, the median treatment duration during the oral only treatment period was 174 days. A total of 2568 patients (31.8% patients with symptomatic PE with or without DVT and 68.1% with symptomatic DVT only) were treated with a mean age of 54.9 years. The patient population was 60.6% male, 77.6% white, 20.9% Asian, and 1.5% black. The concomitant diseases of patients in this trial included hypertension (35.1%), diabetes mellitus (9.8%), coronary artery disease (7.1%), active cancer (3.9%), and gastric or duodenal ulcer (3.8%). Concomitant medications included agents acting on renin-angiotensin system (24.2%), vasodilators (28.6%), serum lipid-reducing agents (20.0%), NSAIDs (22.3%), beta-blockers (14.8%), calcium channel blockers (10.8%), ASA (9.8%), and platelet inhibitors excluding ASA (0.8%). Patients randomized to warfarin had a mean percentage of time in the INR target range of 2.0 to 3.0 of 57% in RE-COVER II study.
In studies RE-COVER and RE-COVER II, the protocol specified non-inferiority margin (2.75) for the hazard ratio was derived based on the upper limit of the 95% confidence interval of the historical warfarin effect. PRADAXA Capsules was demonstrated to be non-inferior to warfarin (dosed to target INR of 2 to 3) (Table 13) based on the primary composite endpoint (fatal PE or symptomatic non-fatal PE and/or DVT) and retains at least 66.9% (RE-COVER) and 63.9% (RE-COVER II) of the historical warfarin effect, respectively.
| PRADAXA Capsules 150 mg twice daily N (%) | Warfarin N (%) | Hazard ratio vs warfarin (95% CI) | |
|---|---|---|---|
| aModified ITT analyses population consists of all randomized patients who received at least one dose of study medication. bNumber of patients with one or more event. cNumber of events. For patients with multiple events each event is counted independently. |
|||
| RE-COVER | N=1274 | N=1265 | |
| Primary Composite Endpointb | 34 (2.7) | 32 (2.5) | 1.05 (0.65, 1.70) |
| Fatal PEc | 1 (0.1) | 3 (0.2) | |
| Symptomatic non-fatal PEc | 16 (1.3) | 8 (0.6) | |
| Symptomatic recurrent DVTc | 17 (1.3) | 23 (1.8) | |
| RE-COVER II | N=1279 | N=1289 | |
| Primary Composite Endpointb | 34 (2.7) | 30 (2.3) | 1.13 (0.69, 1.85) |
| Fatal PEc | 3 (0.2) | 0 | |
| Symptomatic non-fatal PEc | 9 (0.7) | 15 (1.2) | |
| Symptomatic recurrent DVTc | 30 (2.3) | 17 (1.3) | |
In the randomized, parallel-group, double-blind, pivotal trial, RE-MEDY, patients received PRADAXA Capsules 150 mg twice daily or warfarin (dosed to target INR of 2 to 3) following 3 to 12 months of treatment with anticoagulation therapy for an acute VTE. The median treatment duration during the treatment period was 534 days. A total of 2856 patients were treated with a mean age of 54.6 years. The patient population was 61% male, and 90.1% white, 7.9% Asian and 2.0% black. The concomitant diseases of patients in this trial included hypertension (38.6%), diabetes mellitus (9.0%), coronary artery disease (7.2%), active cancer (4.2%), and gastric or duodenal ulcer (3.8%). Concomitant medications included agents acting on renin-angiotensin system (27.9%), vasodilators (26.7%), serum lipid reducing agents (20.6%), NSAIDs (18.3%), beta-blockers (16.3%), calcium channel blockers (11.1%), aspirin (7.7%), and platelet inhibitors excluding ASA (0.9%). Patients randomized to warfarin had a mean percentage of time in the INR target range of 2.0 to 3.0 of 62% in the study.
In study RE-MEDY, the protocol specified non-inferiority margin (2.85) for the hazard ratio was derived based on the point estimate of the historical warfarin effect. PRADAXA Capsules was demonstrated to be non-inferior to warfarin (dosed to target INR of 2 to 3) (Table 14) based on the primary composite endpoint (fatal PE or symptomatic non-fatal PE and/or DVT) and retains at least 63.0% of the historical warfarin effect. If the non-inferiority margin was derived based on the 50% retention of the upper limit of the 95% confidence interval, PRADAXA Capsules was demonstrated to retain at least 33.4% of the historical warfarin effect based on the composite primary endpoint.
| PRADAXA Capsules 150 mg twice daily N=1430 N (%) | Warfarin N=1426 N (%) | Hazard ratio vs warfarin (95% CI) | |
|---|---|---|---|
| aModified ITT analyses population consists of all randomized patients who received at least one dose of study medication. bNumber of patients with one or more event. cNumber of events. For patients with multiple events each event is counted independently. |
|||
| Primary Composite Endpointb | 26 (1.8) | 18 (1.3) | 1.44 (0.78, 2.64) |
| Fatal PEc | 1 (0.07) | 1 (0.07) | |
| Symptomatic non-fatal PEc | 10 (0.7) | 5 (0.4) | |
| Symptomatic recurrent DVTc | 17 (1.2) | 13 (0.9) | |
In a randomized, parallel-group, double-blind, pivotal trial, RE-SONATE, patients received PRADAXA Capsules 150 mg twice daily or placebo following 6 to 18 months of treatment with anticoagulation therapy for an acute VTE. The median treatment duration was 182 days. A total of 1343 patients were treated with a mean age of 55.8 years. The patient population was 55.5% male, 89.0% white, 9.3% Asian, and 1.7% black. The concomitant diseases of patients in this trial included hypertension (38.8%), diabetes mellitus (8.0%), coronary artery disease (6.0%), history of cancer (6.0%), gastric or duodenal ulcer (4.5%), and heart failure (4.6%). Concomitant medications included agents acting on renin-angiotensin system (28.7%), vasodilators (19.4%), beta-blockers (18.5%), serum lipid reducing agents (17.9%), NSAIDs (12.1%), calcium channel blockers (8.9%), aspirin (8.3%), and platelet inhibitors excluding ASA (0.7%). Based on the outcome of the primary composite endpoint (fatal PE, unexplained death, or symptomatic non-fatal PE and/or DVT), PRADAXA was superior to placebo (Table 15).
| PRADAXA Capsules 150 mg twice daily N=681 N (%) | Placebo N=662 N (%) | Hazard ratio vs placebo (95% CI) | |
|---|---|---|---|
| aModified ITT analyses population consists of all randomized patients who received at least one dose of study medication. bNumber of patients with one or more events. cNumber of events. For patients with multiple events each event is counted independently. |
|||
| Primary Composite Endpointb | 3 (0.4) | 37 (5.6) | 0.08 (0.02, 0.25) p-value <0.0001 |
| Fatal PE and unexplained deathc | 0 | 2 (0.3) | |
| Symptomatic non-fatal PEc | 1 (0.1) | 14 (2.1) | |
| Symptomatic recurrent DVTc | 2 (0.3) | 23 (3.5) | |
14.3 Prophylaxis of Deep Vein Thrombosis and Pulmonary Embolism in Adult Patients Following Hip Replacement Surgery
In the randomized, parallel-group, double-blind, non-inferiority trials, RE-NOVATE and RE-NOVATE II patients received PRADAXA Capsules 75 mg orally 1-4 hours after surgery followed by 150 mg daily (RE-NOVATE), PRADAXA Capsules 110 mg orally 1-4 hours after surgery followed by 220 mg daily (RE-NOVATE and RE-NOVATE II) or subcutaneous enoxaparin 40 mg once daily initiated the evening before surgery (RE-NOVATE and RE-NOVATE II) for the prophylaxis of deep vein thrombosis and pulmonary embolism in patients who have undergone hip replacement surgery.
Overall, in RE-NOVATE and RE-NOVATE II, the median treatment duration was 33 days for PRADAXA Capsules and 33 days for enoxaparin. A total of 5428 patients were treated with a mean age of 63.2 years. The patient population was 45.3% male, 96.1% white, 3.6% Asian, and 0.4 % black. The concomitant diseases of patients in these trials included hypertension (46.1%), venous insufficiency (15.4%), coronary artery disease (8.2%), diabetes mellitus (7.9%), reduced renal function (5.3%), heart failure (3.4%), gastric or duodenal ulcer (3.0%), VTE (2.7%), and malignancy (0.1%). Concomitant medications included cardiac therapy (69.7%), NSAIDs (68%), vasoprotectives (29.7%), agents acting on renin-angiotensin system (29.1%), beta-blockers (21.5%), diuretics (20.8%), lipid modifying agents (18.2%), any antithrombin/anticoagulant (16.0%), calcium channel blockers (13.6%), low molecular weight heparin (7.8%), aspirin (7.0%), platelet inhibitors excluding ASA (6.9%), other antihypertensives (6.7%), and peripheral vasodilators (2.6%).
For efficacy evaluation all patients were to have bilateral venography of the lower extremities at 3 days after last dose of study drug unless an endpoint event had occurred earlier in the study. In the primary efficacy analysis, PRADAXA Capsules 110 mg orally 1-4 hours after surgery followed by 220 mg daily was non-inferior to enoxaparin 40 mg once daily in a composite endpoint of confirmed VTE (proximal or distal DVT on venogram, confirmed symptomatic DVT, or confirmed PE) and all cause death during the treatment period (Tables 16 and 17). In the studies 2628 (76.5%) patients in RE-NOVATE and 1572 (78.9%) patients in RE-NOVATE II had evaluable venograms at study completion.
| PRADAXA Capsules 220 mg N (%) | Enoxaparin N (%) |
|
|---|---|---|
| aFull Analysis Set (FAS): The FAS included all randomized patients who received at least one subcutaneous injection or one oral dose of study medication, underwent surgery and subjects for whom the presence or absence of an efficacy outcome at the end of the study was known, i.e., an evaluable negative venogram for both distal and proximal DVT in both legs or any of the following: positive venography in one or both legs, or confirmed symptomatic DVT, PE, or death during the treatment period. bVTE is defined as proximal DVT and PE |
||
| Number of Patientsa | N=880 | N= 897 |
| Primary Composite Endpoint | 53 (6.0) | 60 (6.7) |
| Risk difference (%) vs enoxaparin (95% CI) | -0.7 (-2.9, 1.6) | |
| Number of Patients | N=909 | N=917 |
| Composite endpoint of major VTEb and VTE related mortality | 28 (3.1) | 36 (3.9) |
| Number of Patients | N=905 | N=914 |
| Proximal DVT | 23 (2.5) | 33 (3.6) |
| Number of Patients | N=874 | N=894 |
| Total DVT | 46 (5.3) | 57 (6.4) |
| Number of Patients | N=1137 | N=1142 |
| Symptomatic DVT | 6 (0.5) | 1 (0.1) |
| PE | 5 (0.4) | 3 (0.3) |
| Death | 3 (0.3) | 0 |
| PRADAXA Capsules 220 mg N (%) | Enoxaparin N (%) |
|
|---|---|---|
| aFull Analysis Set (FAS): The FAS included all randomized patients who received at least one subcutaneous injection or one oral dose of study medication, underwent surgery and subjects for whom the presence or absence of an efficacy outcome at the end of the study was known, i.e., an evaluable negative venogram for both distal and proximal DVT in both legs or any of the following: positive venography in one or both legs, or confirmed symptomatic DVT, PE, or death during the treatment period. bVTE is defined as proximal DVT and PE |
||
| Number of Patientsa | N=792 | N= 786 |
| Primary Composite Endpoint | 61 (7.7) | 69 (8.8) |
| Risk difference (%) vs enoxaparin (95% CI) | -1.1 (-3.8, 1.6) | |
| Number of Patients | N=805 | N=795 |
| Composite endpoint of major VTEb and VTE related mortality | 18 (2.2) | 33 (4.2) |
| Number of Patients | N=804 | N=793 |
| Proximal DVT | 17 (2.1) | 31 (3.9) |
| Number of Patients | N=791 | N=784 |
| Total DVT | 60 (7.6) | 67 (8.5) |
| Number of Patients | N=1001 | N=992 |
| Symptomatic DVT | 0 | 4 (0.4) |
| PE | 1 (0.1) | 2 (0.2) |
| Death | 0 | 1 (0.1) |
14.4 Treatment of VTE in Pediatric Patients
The DIVERSITY study was conducted to demonstrate the efficacy and safety of PRADAXA compared to standard of care (SOC) for the treatment of venous thromboembolism (VTE) in pediatric patients from birth to less than 18 years of age. The study was designed as an open-label, randomized, parallel-group, non-inferiority study. Patients enrolled were randomized according to a 2:1 scheme to either an age-appropriate formulation (capsules, oral pellets, or oral solution) of PRADAXA (doses adjusted for age and weight) after at least 5 days and no longer than 21 days of treatment with a parenteral anticoagulant, or to SOC comprised of low molecular weight heparins (LMWH) or vitamin K antagonists (VKA) or fondaparinux. For patients on PRADAXA, drug concentration was determined prior to the 7th dose and a single titration was permitted to achieve drug target levels of 50-250 ng/mL. Inability to achieve target, after one up-titration, resulted in premature termination of study drug in 12 patients (6.8%).
The median treatment duration during the treatment period was 85 days. In total, 267 patients entered the study (leading index VTE was 64% deep vein thrombosis, 10% cerebral venous thrombosis or sinus thrombosis, and 9.0% pulmonary embolism), with 18% of patients having a central line-associated thrombosis. The patient population was 49.8% male, 91.8% white, 4.9% Asian, and 1.5% black; 168 patients were 12 to <18 years old, 64 patients 2 to <12 years, and 35 patients were younger than 2 years. The concomitant VTE-related risk factors of patients in this trial among study arms were as follows: inherited thrombophilia disorder (PRADAXA: 20%, SOC: 22%), congenital heart disease (PRADAXA: 12%, SOC: 30%), heart failure (PRADAXA: 3%, SOC: 18%), history of cancer (PRADAXA: 10%, SOC: 1%), CVL insertion (PRADAXA: 23%, SOC: 27%), immobility (PRADAXA: 13%, SOC: 10%) and significant infection (PRADAXA: 15%, SOC: 13%). The number of patients taking concomitant medications with hemostatic effects were similar in both treatment groups (PRADAXA: 15%, SOC: 16%).
The efficacy of PRADAXA was established based on a composite endpoint of patients with complete thrombus resolution, freedom from recurrent venous thromboembolic event, and freedom from mortality related to venous thromboembolic event (composite primary endpoint). Of the 267 randomized patients, 81 patients (45.8%) in the PRADAXA group and 38 patients (42.2%) in the SOC group met the criteria for the composite primary endpoint. The corresponding rate difference and 95% CI was -0.038 (-0.161, 0.086) and thus demonstrated non-inferiority of PRADAXA to SOC, since the upper bound of the 95% CI was lower than the predefined non-inferiority margin of 20% (see Table 18).
| PRADAXA | Standard of Care | |||
|---|---|---|---|---|
| 1 Mantel-Haenszel weighted difference with age group as stratification factor | ||||
| Number of patients randomized (%) | 177 (100.0) | 90 (100.0) | ||
| Complete thrombus resolution | 81 | (45.8) | 38 | (42.2) |
| Freedom from recurrent VTE | 170 | (96.0) | 83 | (92.2) |
| Freedom from mortality related to VTE | 177 | (100.0) | 89 | (98.9) |
| Composite endpoint met | 81 | (45.8) | 38 | (42.2) |
| Difference in rate (95% CI)1 | -0.038 (-0.161, 0.086) | |||
| p-value for non-inferiority | <0.0001 | |||
| p-value for superiority | 0.2739 | |||
Subgroup analyses showed that there were no outliers in the treatment effect for the subgroups by age, sex, region, and presence of certain risk factors (central venous line, congenital heart disease, malignant disease). For the 3 different age strata, the proportions of patients that met the efficacy endpoint in the PRADAXA and SOC groups, respectively, were 13/22 (59.1%) and 7/13 (53.8%) for patients from birth to < 2 years [Rate Difference -0.052; (95%CI: -0.393, 0.288)], 21/43 (48.8%) and 12/21 (57.1%) for patients aged 2 to < 12 years [Rate Difference 0.083; (95%CI: -0.176, 0.342)], and 47/112 (42.0%) and 19/56 (33.9%) for patients aged 12 to < 18 years [Rate Difference -0.080; (95%CI: -0.234, 0.074)].
14.5 Reduction in the Risk of Recurrence of VTE in Pediatric Patients
Study 2 was an open-label, single-arm safety study to assess the safety of PRADAXA for the prevention of recurrent VTE in pediatric patients from birth to <18 years. Patients who required further anticoagulation due to the presence of a clinical risk factor after completing the initial treatment for confirmed VTE (for at least 3 months) or after completing the DIVERSITY study were included in the study. Eligible patients received age- and weight adjusted doses of an age-appropriate formulation (capsules or oral pellets) of PRADAXA until the clinical risk factor resolved, or up to a maximum of 12 months. The primary endpoints of the study included the recurrence of VTE, major and minor bleeding events, and mortality (overall and related to thrombotic or thromboembolic events) at 6 and 12 months.
Of the 214 patients in the study, 162 patients were 12 to <18 years old, 43 patients were 2 to <12 years old, and 9 patients were aged 6 months to <2 years old.
The overall probability of being free from recurrence of VTE during the on-treatment period was 0.990 (95% CI: 0.960, 0.997) at 3 months, 0.984 (95% CI: 0.950, 0.995) at 6 months, and 0.984 (95% CI: 0.950, 0.995) at 12 months. The probability of being free from bleeding events during the on-treatment period was 0.849 (95% CI: 0.792, 0.891) at 3 months, 0.785 (95% CI: 0.718, 0.838) at 6 months, and 0.723 (95% CI: 0.645, 0.787) at 12 months. No on-treatment deaths occurred.
16. How is Pradaxa supplied
PRADAXA 75 mg capsules have a white opaque cap imprinted with the Boehringer Ingelheim company symbol and a white opaque body imprinted with "R75". The color of the imprinting is black. The capsules are supplied in the packages listed:
- NDC 0597-0355-09 Unit of use bottle of 60 capsules
- NDC 0597-0355-56 Blister package containing 60 capsules (10 × 6 capsule blister cards)
PRADAXA 110 mg capsules have a light blue opaque cap imprinted with the Boehringer Ingelheim company symbol and a light blue opaque body imprinted with "R110". The color of the imprinting is black. The capsules are supplied in the packages listed:
- NDC 0597-0108-54 Unit of use bottle of 60 capsules
- NDC 0597-0108-60 Blister package containing 60 capsules (10 × 6 capsule blister cards)
PRADAXA 150 mg capsules have a light blue opaque cap imprinted with the Boehringer Ingelheim company symbol and a white opaque body imprinted with "R150". The color of the imprinting is black. The capsules are supplied in the packages listed:
- NDC 0597-0360-55 Unit of use bottle of 60 capsules
- NDC 0597-0360-82 Blister package containing 60 capsules (10 × 6 capsule blister cards)
17. Patient Counseling Information
Advise the patient or caregiver to read the FDA-approved patient labeling (Medication Guide).
| This Medication Guide has been approved by the U.S. Food and Drug Administration. | Revised: June 2021 | |||
| MEDICATION GUIDE PRADAXA (pra dax a) (dabigatran etexilate) Capsules |
||||
| This Medication Guide is for PRADAXA Capsules. If your healthcare provider prescribes PRADAXA Oral Pellets for you, read the Medication Guide that comes with your medicine. Read this Medication Guide before you start taking PRADAXA Capsules and each time you get a refill. There may be new information. This Medication Guide does not take the place of talking with your healthcare provider about your medical condition or your treatment. |
||||
What is the most important information I should know about PRADAXA?
|
||||
| What is PRADAXA?
PRADAXA is a prescription medicine that is used to:
|
||||
Do not take PRADAXA if you:
|
||||
Before taking PRADAXA, tell your healthcare provider about all of your medical conditions, including if you:
Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins, and herbal supplements. Some of your other medicines may affect the way PRADAXA works. Certain medicines may increase your risk of bleeding. See "What is the most important information I should know about PRADAXA?" Especially tell your healthcare provider if you take a medicine that contains rifampin. Know the medicines you take. Keep a list of them and show it to your healthcare provider and pharmacist when you get a new medicine. |
||||
How should I take PRADAXA Capsules?
|
||||
| What are the possible side effects of PRADAXA?
PRADAXA can cause serious side effects. See "What is the most important information I should know about PRADAXA?"
|
||||
|
|
| ||
|
||||
|
| |||
Common side effects of PRADAXA in adults and children include:
In children, common side effects also include:
These are not all of the possible side effects of PRADAXA. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088. |
||||
How should I store PRADAXA Capsules?
|
||||
| General information about the safe and effective use of PRADAXA
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not use PRADAXA Capsules for a condition for which it was not prescribed. Do not give PRADAXA Capsules to other people, even if they have the same symptoms that you have. It may harm them. This Medication Guide summarizes the most important information about PRADAXA. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about PRADAXA that is written for health professionals. |
||||
| What are the ingredients in PRADAXA Capsules?
Active ingredient: dabigatran etexilate mesylate Inactive ingredients: acacia, dimethicone, hypromellose, hydroxypropyl cellulose, talc, and tartaric acid. The capsule shell is composed of carrageenan, hypromellose, potassium chloride, titanium dioxide, black edible ink, and FD&C Blue No. 2 (150 mg and 110 mg capsules only). Distributed by: Boehringer Ingelheim Pharmaceuticals, Inc. Ridgefield, CT 06877 USA For more information about PRADAXA, including current prescribing information and Medication Guide, go to www.pradaxa.com or call Boehringer Ingelheim Pharmaceuticals, Inc. at 1-800-542-6257 or scan the code to go to www.pradaxa.com.
Copyright © 2021 Boehringer Ingelheim Pharmaceuticals, Inc. ALL RIGHTS RESERVED COL8774CF252021 |
||||
| PRADAXA
dabigatran etexilate mesylate capsule |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| PRADAXA
dabigatran etexilate mesylate capsule |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| PRADAXA
dabigatran etexilate mesylate capsule |
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||||||||||||
| Labeler - Boehringer Ingelheim Pharmaceuticals Inc. (603175944) |
| Registrant - Boehringer Ingelheim Pharmaceuticals Inc. (603175944) |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| West-Ward Columbus Inc. | 058839929 | PACK(0597-0108, 0597-0355, 0597-0360) , LABEL(0597-0108, 0597-0355, 0597-0360) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Boehringer Ingelheim Pharma GmbH and Co. KG | 551147440 | ANALYSIS(0597-0108, 0597-0355, 0597-0360) , MANUFACTURE(0597-0108, 0597-0355, 0597-0360) , API MANUFACTURE(0597-0108, 0597-0355, 0597-0360) , PACK(0597-0108, 0597-0355, 0597-0360) , LABEL(0597-0108, 0597-0355, 0597-0360) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Bidachem S.p.a. | 429232812 | ANALYSIS(0597-0108, 0597-0355, 0597-0360) , API MANUFACTURE(0597-0108, 0597-0355, 0597-0360) | |
| Establishment | |||
| Name | Address | ID/FEI | Business Operations |
|---|---|---|---|
| Sixarp, LLC - Praxis Packaging Solutions | 016329513 | PACK(0597-0108, 0597-0355, 0597-0360) , LABEL(0597-0108, 0597-0355, 0597-0360) | |