Drug Detail:Rasuvo (injection) (Methotrexate (injection) [ meth-oh-trex-ate ])
Drug Class: Antimetabolites Antipsoriatics Antirheumatics Other immunosuppressants
Highlights of Prescribing Information
RASUVO (methotrexate) injection, for subcutaneous use
Initial U.S. Approval: 1953
WARNING: SEVERE TOXIC REACTIONS, INCLUDING EMBRYO- FETAL TOXICITY AND DEATH
See full prescribing information for complete boxed warning.
- Serious toxic reactions and death have been reported with the use of methotrexate. Patients should be closely monitored for bone marrow, liver, lung, skin, and kidney toxicities (5.1).
- Methotrexate can cause embryo-fetal toxicity, including fetal death. Use is contraindicated during pregnancy (4). Advise females and males of reproductive potential to use effective contraception during and after treatment with methotrexate. (5.2, 8.1, 8.3).
- Unexpectedly severe (sometimes fatal) bone marrow suppression, aplastic anemia, and gastrointestinal toxicity have been reported with concomitant administration of methotrexate (usually in high dosage) along with some nonsteroidal anti-inflammatory drugs (NSAIDs) (5.1).
- Hepatotoxicity, fibrosis, and cirrhosis may occur after prolonged use (5.1).
- Methotrexate may cause interstitial pneumonitis at any time during therapy and has been reported at low doses. Pulmonary symptoms (especially a dry, nonproductive cough) may require interruption of treatment and careful investigation (5.1).
- Diarrhea, ulcerative stomatitis, hemorrhagic enteritis, and death from intestinal perforation may occur (5.1).
- Severe, occasionally fatal, skin reactions have been reported (5.1).
- Potentially fatal opportunistic infections may occur (5.1).
Indications and Usage for Rasuvo Injection
Rasuvo is a folate analog metabolic inhibitor indicated for the:
- Management of patients with severe, active rheumatoid arthritis (RA) and polyarticular juvenile idiopathic arthritis (pJIA), who are intolerant of or had an inadequate response to first-line therapy (1.1)
- Symptomatic control of severe, recalcitrant, disabling psoriasis in adults who are not adequately responsive to other forms of therapy (1.2)
Limitation of Use
Rasuvo is not indicated for the treatment of neoplastic diseases (1.3).
Rasuvo Injection Dosage and Administration
- Rasuvo is for once weekly subcutaneous use only.
- Administer Rasuvo in the abdomen or thigh. (2.1)
- Use another formulation of methotrexate for patients requiring oral, intramuscular, intravenous, intra-arterial, or intrathecal dosing, doses less than 7.5 mg per week, doses above 30 mg per week, high-dose regimens, or dose adjustments of less than 2.5 mg increments (2.1)
- Starting doses of methotrexate:
- RA: 7.5 mg once weekly of an oral or subcutaneous formulation (2.2)
- pJIA: 10 mg/m2 once weekly (2.2)
- Psoriasis: 10 to 25 mg once weekly of an oral, intramuscular, subcutaneous, or intravenous formulation (2.3)
- Adjust dose gradually to achieve an optimal response (2.2, 2.3)
Dosage Forms and Strengths
Injection: Single-dose manually-triggered auto-injector delivering methotrexate in the following dosage strengths: 7.5 mg, 10 mg, 12.5 mg, 15 mg, 17.5 mg, 20 mg, 22.5 mg, 25 mg, 27.5 mg, and 30 mg (3).
Contraindications
- Pregnancy (4)
- Alcoholism or liver disease (4)
- Immunodeficiency syndromes (4)
- Preexisting blood dyscrasias (4)
- Hypersensitivity to methotrexate (4)
Warnings and Precautions
- Organ system toxicity: Potential for serious toxicity. Only for use by physicians experienced in antimetabolite therapy (5.1).
- Effects on reproduction: May cause impairment of fertility, oligospermia and menstrual dysfunction (5.3)
- Laboratory tests: Monitor complete blood counts, renal function and liver function tests (5.4).
- Risks from improper dosing: Mistaken daily use has led to fatal toxicity (5.5)
- Patients with impaired renal function, ascites, or pleural effusions: Elimination is reduced (5.6).
- Dizziness and fatigue: May impair ability to drive or operate machinery (5.7)
Adverse Reactions/Side Effects
Common adverse reactions are: nausea, abdominal pain, dyspepsia, stomatitis/mouth sores, rash, nasopharyngitis, diarrhea, liver function test abnormalities, vomiting, headache, bronchitis, thrombocytopenia, alopecia, leukopenia, pancytopenia, dizziness, photosensitivity, and "burning of skin lesions" (6).
To report SUSPECTED ADVERSE REACTIONS, contact Medexus at 1-855-336-3322 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Aspirin, NSAIDs, and steroids: concomitant use may elevate and prolong serum methotrexate levels and cause increased toxicity (7.1)
- Proton pump inhibitors: concomitant use may elevate and prolong serum methotrexate levels and cause increased toxicity (7.2)
Use In Specific Populations
- Pediatric use: Safety and efficacy of methotrexate, including Rasuvo, have not been established in pediatric patients with psoriasis. Safety and efficacy of Rasuvo have not been established in pediatric patients with malignancy (8.4)
- Geriatric use: Use caution in dose selection (8.5)
- Lactation: Advise women not to breastfeed (8.2)
See 17 for PATIENT COUNSELING INFORMATION.
Revised: 3/2020
Full Prescribing Information
WARNING: SEVERE TOXIC REACTIONS, INCLUDING EMBRYO-FETAL TOXICITY AND DEATH
Rasuvo should be used only by physicians whose knowledge and experience include the use of antimetabolite therapy. Because of the possibility of serious toxic reactions (which can be fatal), Rasuvo should be used only in patients with psoriasis or rheumatoid arthritis with severe, recalcitrant, disabling disease which is not adequately responsive to other forms of therapy. Deaths have been reported with the use of methotrexate in the treatment of malignancy, psoriasis, and rheumatoid arthritis. Patients should be closely monitored for bone marrow, liver, lung, skin, and kidney toxicities. Patients should be informed by their physician of the risks involved and be under a physician's care throughout therapy [see Warnings and Precautions (5.1)].
- 1.
- Methotrexate can cause embryo-fetal toxicity, including fetal death. Use is contraindicated during pregnancy. Verify the pregnancy status of females of reproductive potential prior to initiating therapy. Advise females and males of reproductive potential to use effective contraception during and after treatment with Rasuvo [see Warnings and Precautions (5.2), Contraindications (4), and Use in Specific Populations (8.1, 8.3)].
- 2.
- Methotrexate elimination is reduced in patients with impaired renal functions, ascites, or pleural effusions. Such patients require especially careful monitoring for toxicity, and require dose reduction or, in some cases, discontinuation of Rasuvo administration [see Warnings and Precautions (5.6)].
- 3.
- Unexpectedly severe (sometimes fatal) bone marrow suppression, aplastic anemia, and gastrointestinal toxicity have been reported with concomitant administration of methotrexate (usually in high dosage) along with some nonsteroidal anti-inflammatory drugs (NSAIDs) [see Warnings and Precautions (5.1) and Drug Interactions(7.1)].
- 4.
- Methotrexate causes hepatotoxicity, fibrosis and cirrhosis, but generally only after prolonged use. Acutely, liver enzyme elevations are frequently seen. These are usually transient and asymptomatic, and also do not appear predictive of subsequent hepatic disease. Liver biopsy after sustained use often shows histologic changes, and fibrosis and cirrhosis have been reported; these latter lesions may not be preceded by symptoms or abnormal liver function tests in the psoriasis population. For this reason, periodic liver biopsies are usually recommended for psoriatic patients who are under long-term treatment. Persistent abnormalities in liver function tests may precede appearance of fibrosis or cirrhosis in the rheumatoid arthritis population [see Warnings and Precautions (5.1)].
- 5.
- Methotrexate-induced lung disease, including acute or chronic interstitial pneumonitis, is a potentially dangerous lesion, which may occur acutely at any time during therapy and has been reported at low doses. It is not always fully reversible and fatalities have been reported. Pulmonary symptoms (especially a dry, nonproductive cough) may require interruption of treatment and careful investigation [see Warnings and Precautions (5.1)].
- 6.
- Diarrhea and ulcerative stomatitis require interruption of therapy: otherwise, hemorrhagic enteritis and death from intestinal perforation may occur [see Warnings and Precautions (5.1)].
- 7.
- Malignant lymphomas, which may regress following withdrawal of methotrexate, may occur in patients receiving low-dose methotrexate and, thus, may not require cytotoxic treatment. Discontinue Rasuvo first and, if the lymphoma does not regress, appropriate treatment should be instituted [see Warnings and Precautions (5.8)].
- 8.
- Like other cytotoxic drugs, methotrexate may induce "tumor lysis syndrome" in patients with rapidly growing tumors [see Warnings and Precautions (5.9)].
- 9.
- Severe, occasionally fatal, skin reactions have been reported following single or multiple doses of methotrexate. Reactions have occurred within days of oral, intramuscular, intravenous, or intrathecal methotrexate administration. Recovery has been reported with discontinuation of therapy [see Warnings and Precautions (5.1)].
- 10.
- Potentially fatal opportunistic infections, especially Pneumocystis jiroveci pneumonia, may occur with methotrexate therapy [see Warnings and Precautions (5.1)].
- 11.
- Methotrexate given concomitantly with radiotherapy may increase the risk of soft tissue necrosis and osteonecrosis [see Warnings and Precautions (5.10)].
1. Indications and Usage for Rasuvo Injection
1.1 Rheumatoid Arthritis including Polyarticular Juvenile Idiopathic Arthritis
Rasuvo is indicated in the management of selected adults with severe, active rheumatoid arthritis (RA) (ACR criteria), or children with active polyarticular juvenile idiopathic arthritis (pJIA), who have had an insufficient therapeutic response to, or are intolerant of, an adequate trial of first-line therapy including full dose non-steroidal anti-inflammatory agents (NSAIDs).
1.2 Psoriasis
Rasuvo is indicated in adults for the symptomatic control of severe, recalcitrant, disabling psoriasis that is not adequately responsive to other forms of therapy, but only when the diagnosis has been established, as by biopsy and/or after dermatologic consultation. It is important to ensure that a psoriasis "flare" is not due to an undiagnosed concomitant disease affecting immune responses.
2. Rasuvo Injection Dosage and Administration
2.1 Important Dosing Information
Rasuvo is a single-dose manually-triggered auto-injector for once-weekly subcutaneous use only [see Warnings and Precautions (5.5)]. Administer Rasuvo in the abdomen or the thigh. Rasuvo is only available in doses between 7.5 to 30 mg in 2.5 mg increments. Use another formulation of methotrexate for alternative dosing in patients who require oral, intramuscular, intravenous, intra-arterial, or intrathecal dosing, doses less than 7.5 mg per week, doses more than 30 mg per week, high-dose regimens, or dose adjustments of less than 2.5 mg increments.
2.2 Rheumatoid Arthritis including Polyarticular Juvenile Idiopathic Arthritis
Recommended starting dose of methotrexate:
Adult RA: 7.5 mg as a single oral or subcutaneous dose once weekly.
pJIA: 10 mg/m2 once weekly.
For patients switching from oral methotrexate to Rasuvo, consider any differences in bioavailability between oral and subcutaneously administered methotrexate [see Clinical Pharmacology (12.3)].
Dosages may be adjusted gradually to achieve an optimal response. Limited experience shows a significant increase in the incidence and severity of serious toxic reactions, especially bone marrow suppression, at doses greater than 20 mg/wk in adults. Although there is experience with doses up to 30 mg/m2/wk in children, there are too few published data to assess how doses over 20 mg/m2/wk might affect the risk of serious toxicity in children. Experience does suggest, however, that children receiving 20 to 30 mg/m2/wk (0.65 to 1.0 mg/kg/wk) may have better absorption and fewer gastrointestinal side effects if methotrexate is administered either intramuscularly or subcutaneously.
Therapeutic response usually begins within 3 to 6 weeks and the patient may continue to improve for another 12 weeks or more.
The optimal duration of therapy is unknown. Limited data available from long-term studies in adults indicate that the initial clinical improvement is maintained for at least two years with continued therapy. When methotrexate is discontinued, the arthritis usually worsens within 3 to 6 weeks.
The patient should be fully informed of the risks involved and should be under constant supervision of the physician. Assessment of hematologic, hepatic, renal, and pulmonary function should be made by history, physical examination, and laboratory tests before beginning, periodically during, and before reinstituting Rasuvo therapy [see Warnings and Precautions (5.4)]. Females of childbearing potential should not be started on Rasuvo until pregnancy is excluded [see Contraindications (4) and Warnings and Precautions (5.2)].
All schedules should be continually tailored to the individual patient. An initial test dose may be given prior to the regular dosing schedule to detect any extreme sensitivity to adverse effects.
Maximal myelosuppression usually occurs in seven to ten days.
2.3 Psoriasis
Recommended starting dose of methotrexate:
Psoriasis: 10-25 mg as a single oral, intramuscular, subcutaneous, or intravenous dose once weekly.
For patients switching from oral methotrexate to Rasuvo, consider any differences in bioavailability between oral and subcutaneously administered methotrexate [see Clinical Pharmacology (12.3)].
Dosage may be gradually adjusted to achieve optimal clinical response; 30 mg/week should not ordinarily be exceeded. Once optimal clinical response has been achieved, the dosage should be reduced to the lowest possible amount of drug and to the longest possible rest period. The use of Rasuvo may permit the return to conventional topical therapy, which should be encouraged.
2.4 Administration and Handling
Rasuvo is a manually-triggered auto-injector intended for subcutaneous use under the guidance and supervision of a physician.
Patients may self-inject with Rasuvo if a physician determines that it is appropriate, if they have received proper training in how to prepare and administer the correct dose, and if they receive medical follow-up, as necessary.
Rasuvo is injected once weekly. The patient must be explicitly informed about the once weekly dosing schedule. It is advisable to determine an appropriate fixed day of the week for the injection.
Visually inspect Rasuvo for particulate matter and discoloration prior to administration. Do not use Rasuvo if the seal is broken.
Handle and dispose of Rasuvo consistent with recommendations for handling and disposal of cytotoxic drugs1.
3. Dosage Forms and Strengths
Rasuvo is an injection containing methotrexate at a concentration of 50 mg/ml available as a manually-triggered auto-injector that administers a single dose of methotrexate solution in the following dosage strengths:
- 7.5 mg
- 10 mg
- 12.5 mg
- 15 mg
- 17.5 mg
- 20 mg
- 22.5 mg
- 25 mg
- 27.5 mg
- 30 mg
5. Warnings and Precautions
5.1 Organ System Toxicity
Rasuvo should be used only by physicians whose knowledge and experience include the use of antimetabolite therapy. Because of the possibility of serious toxic reactions (which can be fatal), Rasuvo should be used only in patients with psoriasis or rheumatoid arthritis with severe, recalcitrant, disabling disease which is not adequately responsive to other forms of therapy.
Deaths have been reported with the use of methotrexate in the treatment of malignancy, psoriasis, and rheumatoid arthritis. Patients should be closely monitored for bone marrow, liver, lung and kidney toxicities.
Rasuvo has the potential for serious toxicity. Toxic effects may be related in frequency and severity to dose or frequency of administration but have been seen at all doses. Because they can occur at any time during therapy, it is necessary to follow patients on Rasuvo closely. Most adverse reactions are reversible if detected early. When such reactions do occur, the drug should be reduced in dosage or discontinued and appropriate corrective measures should be taken. If necessary, this could include the use of leucovorin calcium and/or acute, intermittent hemodialysis with a high-flux dialyzer [see Overdosage (10)]. If Rasuvo therapy is reinstituted, it should be carried out with caution, with adequate consideration of further need for the drug and increased alertness as to possible recurrence of toxicity. The clinical pharmacology of methotrexate has not been well studied in older individuals. Due to diminished hepatic and renal function as well as decreased folate stores in this population, relatively low doses should be considered, and these patients should be closely monitored for early signs of toxicity [see Use in Specific Populations (8.5)].
5.2 Embryo-Fetal Toxicity
Based on published reports and methotrexate's mechanism of action, methotrexate can cause embryo-fetal toxicity, including fetal death when administered to a pregnant woman. In pregnant women Rasuvo is contraindicated. Verify the pregnancy status of females of reproductive potential prior to initiating Rasuvo. Advise females of reproductive potential to use effective contraception during treatment with Rasuvo and for 6 months after the final dose. Advise males of reproductive potential to use effective contraception during Rasuvo treatment and for 3 months after the final dose [see Contraindications (4), Use in Specific Populations (8.1, 8.3), Clinical Pharmacology (12.1)].
5.3 Effects on Reproduction
Based on published reports, methotrexate can cause impairment of fertility, oligospermia, and menstrual dysfunction. It is not known if the infertility may be reversible in affected patients. Discuss the risk of effects on reproduction with female and male patients of reproductive potential [see Use in Specific Populations (8.3)].
5.4 Laboratory Tests
Patients undergoing Rasuvo therapy should be closely monitored so that toxic effects are detected promptly. Baseline assessment should include a complete blood count with differential and platelet counts, hepatic enzymes, renal function tests and a chest X-ray.
During therapy, monitoring of these parameters is recommended: hematology at least monthly, renal function and liver function every 1 to 2 months [see Warnings and Precautions (5.1)].
During initial or changing doses, or during periods of increased risk of elevated methotrexate blood levels (e.g., dehydration), more frequent monitoring may also be indicated.
5.5 Risks from Improper Dosing
Both the physician and pharmacist should emphasize to the patient that Rasuvo is administered once weekly and that mistaken daily use has led to fatal toxicity [see Dosage and Administration (2)].
5.6 Patients with Impaired Renal Function, Ascites, or Pleural Effusions
Methotrexate elimination is reduced in patients with impaired renal function, ascites, or pleural effusions. Such patients require especially careful monitoring for toxicity and require dose reduction or, in some cases, discontinuation of Rasuvo administration.
5.7 Dizziness and Fatigue
Adverse reactions, such as dizziness and fatigue, may affect the ability to drive or operate machinery.
5.8 Malignant Lymphomas
Non-Hodgkin's lymphoma and other tumors have been reported in patients receiving low-dose oral methotrexate. However, there have been instances of malignant lymphoma arising during treatment with low-dose oral methotrexate, which have regressed completely following withdrawal of methotrexate, without requiring active anti-lymphoma treatment. Discontinue Rasuvo first and, if the lymphoma does not regress, appropriate treatment should be instituted.
6. Adverse Reactions/Side Effects
The following adverse reactions are discussed in more detail in other sections of the labeling.
- Organ System Toxicity [see Warnings and Precautions (5.1)]
- Embryo-Fetal Toxicity [see Warnings and Precautions (5.2)]
- Effects on Reproduction [see Warnings and Precautions (5.3)]
- Malignant Lymphomas [see Warnings and Precautions (5.8)]
The most frequently reported adverse reactions include ulcerative stomatitis, leukopenia, nausea, and abdominal distress. Other frequently reported adverse reactions are malaise, undue fatigue, chills and fever, dizziness and decreased resistance to infection.
6.1 Clinical Trials Experience
This section provides a summary of adverse reactions reported in subjects in clinical studies conducted with Rasuvo as well as with methotrexate injection and oral methotrexate.
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug, and may not reflect the rates observed in practice.
6.2 Other Adverse Reactions
Other adverse reactions that have been reported with methotrexate in oncology, RA, pJIA, and psoriasis patients are listed below by organ system.
Alimentary System: gingivitis, pharyngitis, stomatitis, anorexia, nausea, vomiting, diarrhea, hematemesis, melena, gastrointestinal ulceration and bleeding, enteritis, pancreatitis.
Blood and Lymphatic System Disorders: suppressed hematopoiesis, anemia, aplastic anemia, pancytopenia, leukopenia, neutropenia, thrombocytopenia, agranulocytosis, eosinophilia, lymphadenopathy and lymphoproliferative disorders (including reversible). Hypogammaglobulinemia has been reported rarely.
Cardiovascular: pericarditis, pericardial effusion, hypotension, and thromboembolic events (including arterial thrombosis, cerebral thrombosis, deep vein thrombosis, retinal vein thrombosis, thrombophlebitis, and pulmonary embolus).
Central Nervous System: headaches, drowsiness, blurred vision, transient blindness, speech impairment including dysarthria and aphasia, hemiparesis, paresis and convulsions have also occurred following administration of methotrexate. Following low doses, there have been occasional reports of transient subtle cognitive dysfunction, mood alteration or unusual cranial sensations, leukoencephalopathy, or encephalopathy.
Hepatobiliary Disorders: hepatotoxicity, acute hepatitis, chronic fibrosis and cirrhosis, hepatic failure, decrease in serum albumin, liver enzyme elevations.
Infection: There have been case reports of sometimes fatal opportunistic infections in patients receiving methotrexate therapy for neoplastic and non-neoplastic diseases. Pneumocystis jiroveci pneumonia was the most common opportunistic infection. There have also been reports of infections, pneumonia, Cytomegalovirus infection, including cytomegaloviral pneumonia, sepsis, fatal sepsis, nocardiosis, histoplasmosis, cryptococcosis, Herpes zoster, Herpes simplex hepatitis, and disseminated Herpes simplex.
Musculoskeletal System: stress fracture.
Ophthalmic: conjunctivitis, serious visual changes of unknown etiology.
Pulmonary System: respiratory fibrosis, respiratory failure, alveolitis, interstitial pneumonitis deaths have been reported, and chronic interstitial obstructive pulmonary disease has occasionally occurred.
Skin: erythematous rashes, pruritus, urticaria, photosensitivity, pigmentary changes, alopecia, ecchymosis, telangiectasia, acne, furunculosis, erythema multiforme, toxic epidermal necrolysis, Stevens-Johnson syndrome, skin necrosis, skin ulceration and exfoliative dermatitis.
Urogenital System: severe nephropathy or renal failure, azotemia, cystitis, hematuria, proteinuria; defective oogenesis or spermatogenesis, transient oligospermia, menstrual dysfunction, vaginal discharge, and gynecomastia; infertility, abortion, fetal death, fetal defects.
Other rarer reactions related to or attributed to the use of methotrexate such as nodulosis, vasculitis, arthralgia/myalgia, loss of libido/impotence, diabetes, osteoporosis, sudden death, lymphoma, including reversible lymphomas, tumor lysis syndrome, soft tissue necrosis and osteonecrosis. Anaphylactoid reactions have been reported.
7. Drug Interactions
7.1 Aspirin, Nonsteroidal Anti-Inflammatory Drugs, and Steroids
Nonsteroidal anti-inflammatory drugs (NSAIDs) should not be administered prior to or concomitantly with the high doses of methotrexate, such as used in the treatment of osteosarcoma. Concomitant administration of some NSAIDs with high dose methotrexate therapy has been reported to elevate and prolong serum methotrexate levels, resulting in deaths from severe hematologic and gastrointestinal toxicity [see Warnings and Precautions (5.1)].
Caution should be used when NSAIDs and salicylates are administered concomitantly with lower doses of methotrexate, including Rasuvo. These drugs have been reported to reduce the tubular secretion of methotrexate in an animal model and may enhance its toxicity.
Despite the potential interactions, studies of methotrexate in patients with rheumatoid arthritis have usually included concurrent use of constant dosage regimens of NSAIDs, without apparent problems. It should be appreciated, however, that the doses used in rheumatoid arthritis (7.5 to 15 mg/week) are somewhat lower than those used in psoriasis and that larger doses could lead to unexpected toxicity. Aspirin, NSAIDs, and/or low dose steroids may be continued, although the possibility of increased toxicity with concomitant use of NSAIDs including salicylates has not been fully explored. Steroids may be reduced gradually in patients who respond to methotrexate.
7.2 Proton Pump Inhibitors (PPIs) and H2 Blockers
Use caution if high-dose methotrexate is administered to patients receiving proton pump inhibitor (PPI) therapy. Case reports and published population pharmacokinetic studies suggest that concomitant use of some PPIs, such as omeprazole, esomeprazole, and pantoprazole, with methotrexate (primarily at high dose), may elevate and prolong serum levels of methotrexate and/or its metabolite hydroxymethotrexate, possibly leading to methotrexate toxicities. In two of these cases, delayed methotrexate elimination was observed when high-dose methotrexate was co-administered with PPIs, but was not observed when methotrexate was co-administered with ranitidine. However, no formal drug interaction studies of methotrexate with ranitidine have been conducted.
7.3 Oral Antibiotics
Oral antibiotics such as tetracycline, chloramphenicol, and nonabsorbable broad spectrum antibiotics, may decrease intestinal absorption of methotrexate or interfere with the enterohepatic circulation by inhibiting bowel flora and suppressing metabolism of the drug by bacteria.
Penicillins may reduce the renal clearance of methotrexate; increased serum concentrations of methotrexate with concomitant hematologic and gastrointestinal toxicity have been observed with high and low dose methotrexate. Use of Rasuvo with penicillins should be carefully monitored.
Trimethoprim/sulfamethoxazole has been reported rarely to increase bone marrow suppression in patients receiving methotrexate, probably by decreased tubular secretion and/or an additive antifolate effect.
7.4 Hepatotoxins
The potential for increased hepatotoxicity when methotrexate is administered with other hepatotoxic agents has not been evaluated. However, hepatotoxicity has been reported in such cases. Therefore, patients receiving concomitant therapy with Rasuvo and other potential hepatotoxins (e.g., azathioprine, retinoids, and sulfasalazine) should be closely monitored for possible increased risk of hepatotoxicity.
7.5 Theophylline
Methotrexate may decrease the clearance of theophylline; theophylline levels should be monitored when used concurrently with Rasuvo.
7.6 Folic Acid and Antifolates
Vitamin preparations containing folic acid or its derivatives may decrease responses to systemically administered methotrexate. Preliminary animal and human studies have shown that small quantities of intravenously administered leucovorin enter the CSF primarily as 5-methyltetrahydrofolate and, in humans, remain 1 to 3 orders of magnitude lower than the usual methotrexate concentrations following intrathecal administration. However, high doses of leucovorin may reduce the efficacy of intrathecally administered methotrexate. Folate deficiency states may increase methotrexate toxicity.
Trimethoprim/sulfamethoxazole has been reported rarely to increase bone marrow suppression in patients receiving methotrexate, probably by decreased tubular secretion and/or an additive antifolate effect.
7.7 Mercaptopurine
Methotrexate increases the plasma levels of mercaptopurine. The combination of Rasuvo and mercaptopurine may therefore require dose adjustment.
7.8 Nitrous oxide
The use of nitrous oxide anesthesia potentiates the effect of methotrexate on folate dependent metabolic pathways, resulting in the potential for increased toxicity. Avoid the simultaneous use of nitrous oxide and methotrexate.
7.9 Other Drugs
Methotrexate is partially bound to serum albumin, and toxicity may be increased because of displacement by certain drugs, such as salicylates, phenylbutazone, phenytoin, and sulfonamides.
Renal tubular transport is also diminished by probenecid; use of Rasuvo with this drug should be carefully monitored.
Combined use of methotrexate with gold, penicillamine, hydroxychloroquine, sulfasalazine, or cytotoxic agents, has not been studied and may increase the incidence of adverse effects.
8. Use In Specific Populations
8.4 Pediatric Use
The safety and effectiveness of methotrexate, including Rasuvo, have not been established in pediatric patients with psoriasis.
The safety and effectiveness of Rasuvo have not been established in pediatric patients with neoplastic diseases.
The safety and effectiveness of methotrexate have been established in pediatric patients with polyarticular juvenile idiopathic arthritis [see Clinical Studies (14.2)].
Published clinical studies evaluating the use of methotrexate in children and adolescents (i.e., patients 2 to 16 years of age) with pJIA demonstrated safety comparable to that observed in adults with rheumatoid arthritis [see Adverse Reactions (6.1)].
Rasuvo does not contain a preservative. However, methotrexate injectable formulations containing the preservative benzyl alcohol are not recommended for use in neonates. There have been reports of fatal 'gasping syndrome' in neonates (children less than one month of age) following the administrations of intravenous solutions containing the preservative benzyl alcohol. Symptoms include a striking onset of gasping respiration, hypotension, bradycardia, and cardiovascular collapse.
Serious neurotoxicity, frequently manifested as generalized or focal seizures, has been reported with unexpectedly increased frequency among pediatric patients with acute lymphoblastic leukemia who were treated with intermediate-dose intravenous methotrexate (1 gm/m2) [see Warnings and Precautions (5.1)].
8.5 Geriatric Use
Clinical studies of methotrexate did not include sufficient numbers of subjects age 65 and over to determine whether they respond differently from younger subjects. In general, dose selection for an elderly patient should be cautious reflecting the greater frequency of decreased hepatic and renal function, decreased folate stores, concomitant disease or other drug therapy (i.e., that interfere with renal function, methotrexate or folate metabolism) in this population [see Warnings and Precautions (5.1), Drug Interactions (7.7) and Use in Specific Populations (8.6)]. Since decline in renal function may be associated with increases in adverse reactions and serum creatinine measurements may over estimate renal function in the elderly, more accurate methods (i.e., creatinine clearance) should be considered. Serum methotrexate levels may also be helpful. Elderly patients should be closely monitored for early signs of hepatic, bone marrow and renal toxicity. In chronic use situations, certain toxicities may be reduced by folate supplementation.
Post-marketing experience suggests that the occurrence of bone marrow suppression, thrombocytopenia, and pneumonitis may increase with age [see Warnings and Precautions (5.1)].
8.6 Renal Impairment
Methotrexate elimination is reduced in patients with impaired renal function. Such patients require especially careful monitoring for toxicity and require dose reduction or, in some cases, discontinuation of Rasuvo administration.
8.7 Hepatic Impairment
The effect of hepatic impairment on methotrexate pharmacokinetics has not been studied. Rasuvo is contraindicated in patients with alcoholic liver disease or other chronic liver disease. Patients with obesity, diabetes, hepatic fibrosis or steatohepatitis are at increased risk for hepatic injury and fibrosis secondary to methotrexate, and should be monitored closely [see Warnings and Precautions (5.1)].
10. Overdosage
Leucovorin is indicated to diminish the toxicity and counteract the effect of inadvertently administered overdosages of methotrexate. Leucovorin administration should begin as promptly as possible. As the time interval between methotrexate administration and leucovorin initiation increases, the effectiveness of leucovorin in counteracting toxicity decreases. Monitoring of the serum methotrexate concentration is essential in determining the optimal dose and duration of treatment with leucovorin.
In cases of massive overdosage, hydration and urinary alkalinization may be necessary to prevent the precipitation of methotrexate and/or its metabolites in the renal tubules. Generally speaking, neither hemodialysis nor peritoneal dialysis has been shown to improve methotrexate elimination. However, effective clearance of methotrexate has been reported with acute, intermittent hemodialysis using a high-flux dialyzer (Wall, SM et al: Am J Kidney Dis 28 (6): 846-854, 1996).
Accidental intrathecal overdosage may require intensive systemic support, high-dose systemic leucovorin, alkaline diuresis and rapid CSF drainage and ventriculolumbar perfusion.
In postmarketing experience, overdose with methotrexate has generally occurred with oral and intrathecal administration, although intravenous and intramuscular overdose have also been reported.
Reports of oral overdose often indicate accidental daily administration instead of weekly (single or divided doses). Symptoms commonly reported following oral overdose include those symptoms and signs reported at pharmacologic doses, particularly hematologic and gastrointestinal reaction. For example, leukopenia, thrombocytopenia, anemia, pancytopenia, bone marrow suppression, mucositis, stomatitis, oral ulceration, nausea, vomiting, gastrointestinal ulceration, gastrointestinal bleeding. In some cases, no symptoms were reported.
There have been reports of death following overdose. In these cases, events such as sepsis or septic shock, renal failure, and aplastic anemia were also reported.
Symptoms of intrathecal overdose are generally central nervous system (CNS) symptoms, including headache, nausea and vomiting, seizure or convulsion, and acute toxic encephalopathy. In some cases, no symptoms were reported. There have been reports of death following intrathecal overdose. In these cases, cerebellar herniation associated with increased intracranial pressure, and acute toxic encephalopathy have also been reported.
There are published case reports of intravenous and intrathecal carboxypeptidase G2 treatment to hasten clearance of methotrexate in cases of overdose.
11. Rasuvo Injection Description
Rasuvo contains methotrexate, a folate analog metabolic inhibitor.
Chemically, methotrexate is [N-[4-[[(2,4-diamino-6-pteridinyl)methyl]methylamino]benzoyl]-Lglutamic acid. The structural formula is:
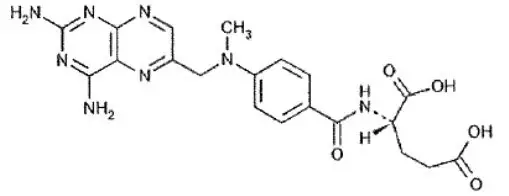
C20H22N8O5 M.W.= 454.45
Rasuvo contains methotrexate in a sterile, preservative-free, non-pyrogenic solution for a single subcutaneous injection. Rasuvo is an isotonic, clear, yellow to brown solution.
Rasuvo contains the following inactive ingredients: sodium chloride 0.4% w/v; water for injections, sodium hydroxide and, if necessary, hydrochloric acid are added to adjust the pH to approximately 8.5.
12. Rasuvo Injection - Clinical Pharmacology
12.1 Mechanism of Action
Methotrexate inhibits dihydrofolic acid reductase. Dihydrofolates must be reduced to tetrahydrofolates by this enzyme before they can be utilized as carriers of one-carbon groups in the synthesis of purine nucleotides and thymidylate. Therefore, methotrexate interferes with DNA synthesis, repair, and cellular replication. Actively proliferating tissues such as malignant cells, bone marrow, fetal cells, buccal and intestinal mucosa, and cells of the urinary bladder are in general more sensitive to this effect of methotrexate.
The mechanism of action in rheumatoid arthritis is unknown; it may affect immune function.
12.2 Pharmacodynamics
Two reports describe in vitro methotrexate inhibition of DNA precursor uptake by stimulated mononuclear cells, and another describes in animal polyarthritis partial correction by methotrexate of spleen cell hyporesponsiveness and suppressed IL 2 production. Other laboratories, however, have been unable to demonstrate similar effects. Clarification of methotrexate's effect on immune activity and its relation to rheumatoid immunopathogenesis await further studies.
In psoriasis, the rate of production of epithelial cells in the skin is greatly increased over normal skin. This differential in proliferation rates is the basis for the use of methotrexate to control the psoriatic process.
Methotrexate in high doses, followed by leucovorin rescue, is used as a part of the treatment of patients with non- metastatic osteosarcoma. The original rationale for high dose methotrexate therapy was based on the concept of selective rescue of normal tissues by leucovorin. More recent evidence suggests that high dose methotrexate may also overcome methotrexate resistance caused by impaired active transport, decreased affinity of dihydrofolic acid reductase for methotrexate, increased levels of dihydrofolic acid reductase resulting from gene amplification, or decreased polyglutamation of methotrexate. The actual mechanism of action is unknown.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Methotrexate has been evaluated in a number of animal studies for carcinogenic potential with inconclusive results. Although there is evidence that methotrexate causes chromosomal damage to animal somatic cells and human bone marrow cells, the clinical significance remains uncertain.
Data are available regarding the risks for pregnancy and for fertility in humans [see Use in Specific Populations (8.1 and 8.3)].
14. Clinical Studies
14.1 Rheumatoid Arthritis
Clinical trials in patients with rheumatoid arthritis were performed using other formulations of methotrexate.
In patients with rheumatoid arthritis, effects of methotrexate on articular swelling and tenderness can be seen as early as 3 to 6 weeks.
Most studies of methotrexate in patients with rheumatoid arthritis are relatively short term (3 to 6 months). Limited data from long-term studies indicate that an initial clinical improvement is maintained for at least two years with continued therapy.
14.2 Polyarticular Juvenile Idiopathic Arthritis
Clinical trials in patients with polyarticular juvenile idiopathic arthritis were performed using other formulations of methotrexate.
In a 6-month double-blind, placebo-controlled trial of 127 pediatric patients with pJIA (mean age, 10.1 years; age range, 2.5 to 18 years; mean duration of disease, 5.1 years) on background nonsteroidal anti-inflammatory drugs and/or prednisone, methotrexate given weekly at an oral dose of 10 mg/m2 provided significant clinical improvement compared to placebo as measured by either the physician's global assessment, or by a patient composite (25% reduction in the articular-severity score plus improvement in parent and physician global assessments of disease activity). Over two-thirds of the patients in this trial had polyarticular-course JIA, and the numerically greatest response was seen in this subgroup treated with 10 mg/m2/wk methotrexate.
The overwhelming majority of the remaining patients had systemic-course JIA. All patients were unresponsive to NSAIDs; approximately one-third were using low dose corticosteroids.
Weekly methotrexate at a dose of 5 mg/m2 was not significantly more effective than placebo in this trial.
16. How is Rasuvo Injection supplied
Rasuvo contains methotrexate in a preservative-free sterile solution for a single subcutaneous injection in the following configurations.
| Strength | Pack Configuration* | NDC |
|---|---|---|
|
||
| 7.5 mg per 0.15 mL | 1 | 59137-505-01 |
| 4 | 59137-505-04 | |
| 10 mg per 0.20 mL | 1 | 59137-510-01 |
| 4 | 59137-510-04 | |
| 12.5 mg per 0.25 mL | 1 | 59137-515-01 |
| 4 | 59137-515-04 | |
| 15 mg per 0.30 mL | 1 | 59137-520-01 |
| 4 | 59137-520-04 | |
| 17.5 mg per 0.35 mL | 1 | 59137-525-01 |
| 4 | 59137-525-04 | |
| 20 mg per 0.40 mL | 1 | 59137-530-01 |
| 4 | 59137-530-04 | |
| 22.5 mg per 0.45 mL | 1 | 59137-535-01 |
| 4 | 59137-535-04 | |
| 25 mg per 0.50 mL | 1 | 59137-540-01 |
| 4 | 59137-540-04 | |
| 27.5 mg per 0.55 mL | 1 | 59137-545-01 |
| 4 | 59137-545-04 | |
| 30 mg per 0.60 mL | 1 | 59137-550-01 |
| 4 | 59137-550-04 | |
Not all pack sizes may be marketed.
| RASUVO
methotrexate injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| RASUVO
methotrexate injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| RASUVO
methotrexate injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| RASUVO
methotrexate injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| RASUVO
methotrexate injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| RASUVO
methotrexate injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| RASUVO
methotrexate injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| RASUVO
methotrexate injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| RASUVO
methotrexate injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| Labeler - Medexus Pharma Inc. (078811131) |